Abstract
Background:
This study was done to evaluate the relationship between the time of endoscopy in patients with upper gastrointestinal bleeding with morbidity and mortality rates of patients at the Al Zahra Hospital emergency room.
Materials and Methods:
In a cohort study, 1152 patients at 2014 and 2015 have been hospitalized due to gastrointestinal bleeding in Al Zahra Hospital, were selected and demographic and clinical information and day and time of endoscopy and hospital mortality and fewer deaths than a month after discharge were studied, and prognosis was analyzed in terms of day and time of endoscopy.
Results:
Nine hundred and seventy-three cases (84.5%) of endoscopy were performed during the working days and 179 (15.5%) were performed on holidays. Moreover, 801 cases (69.5%) of endoscopy were done in the morning and 351 cases (30.5%) were performed in the evening and night shifts. The day and time of endoscopy had no significant effect on mortality in hospital and less than a month after but hospital death in whom underwent endoscopy by fellowship was significantly higher (P = 0.004).
Conclusion:
Endoscopy in nonholiday and holiday days and the time of endoscopy has no significant effect on hospital mortality 1 month after discharge. However, other factors such as endoscopy by attendant or fellowship, time between admission to endoscopy, age and sex of the patients, etc., were significantly effective on in-hospital mortality and death 1 months after discharge. Also faster and sooner endoscopy cannot reduce rate of blood transfusions or reduce the length of hospital stay but faster endoscopy of patients can reduce the risk of in-hospital death.
Keywords: Endoscopy, gastrointestinal bleeding, mortality
Introduction
Upper gastrointestinal bleeding (UGIB) is blood loss with gastrointestinal bleeding origin above the ligament of Treitz and the peptic ulcer disease is said to be the most common cause of it.[1] The annual incidence of hospital admissions due to UGIB is almost 1.0% and the mortality rate is about 5%–10%.
There are several therapeutic procedures to control bleeding of upper gastrointestinal that endoscopy is one of the most effective and most cost-effective method.[1,2,3,4] Endoscopic treatment of bleeding can be an early and urgent action or it can be done after the patient's hemodynamic stability and recovery.[5,6] Many studies have been mentioned that different medical conditions, hospital admission duration, and faster endoscopy of patients in hospital together can be predictive of disease outcome. Faster endoscopy is causing hemostasis faster in high risk patients and leads to earlier diagnosis and more appropriate treatment while preventing unnecessary hospitalization.[7,8] In some studies, it has been noted that patients’ admission during the week or weekend is independent factor for mortality. Endoscopy in patients with underlying serious problems such as heart disease until patient's hemodynamic stability must be delayed.[9] It seems that patients with nonvariceal gastrointestinal bleeding admitted at evening and night shifts or in weekends compared to patients who are hospitalized in the morning or during the week, have a longer time to endoscopy.[4,6] Some studies have suggested that patients’ admission during the week or weekends is not an independent predictor of in-hospital mortality[10] and it has been cited in other studies that compared with patients who are examined during the week, patients who are hospitalized over the weekend have a worse prognosis.[2,3,9]
Yet it seems more factors have indirect impact on the prognosis of disease and mortality of patients with gastrointestinal bleeding who are undergoing endoscopy depends to factors such as endoscopy skills, the severity of bleeding, and characteristics of individual patient and underlying disease, which can be will found at the time of endoscopy. Considering controversies in various studies on the impact of multiple factors in the prognosis of patients with gastrointestinal bleeding and the fact that no study has been done on the impact of these factors in Iran yet, the present study aimed to evaluate the effect of endoscopy time on morbidity and mortality rates in patients with UGIB patients.
Materials and Methods
This study is a case cohort study that was conducted in 2014 and 2015 in Al Zahra Hospital. The study population included people over 18 years from October 2014 to the end of September 2015, who had undergone endoscopy due to UGIB. Inclusion criteria for this study were patients ability for endoscopy, hemodynamically stable conditions (systolic blood pressure >10 mm Hg without orthostatic hypo-tension) or heart rate <100/min at 3 h of admission or hemodynamic stabilizing liquid treatment within 3 h of admission, absence of severe comorbidities and Rokal score <5, platelet more than 40000, lack of bleeding in the hospital, avoiding the use of anticoagulant,[1,7,10] and the patient agreed to participate in the study. Cancel endoscopes for various reasons, gastrointestinal bleeding caused by nonupper reason, age <18 years, lack of patients follow-up, and patients referred from other centers were considered as exclusion criteria.
The sample size required for this study using sample size formula for the prevalence studies and taking into account the 95% confidence level, the incidence of mortality in patients undergoing endoscopy due to the lack of similar studies was considered 5.0 and acceptance of 0.05% error rate, the initial sample size was set as 384, and according to hospital shifts, the overall sample size was estimated as 1152 person.
After approved of proposal in Ethical Committee of Isfahan University of Medical Sciences, at the beginning, public information was completed for all patients and treatment protocol for all patients was done based on the severity of bleeding and the presence of co morbidities. Hours and days of hospitalization, bleeding severity, endoscopy, and treatment time based on the results contained in patient records, endoscopy paper records in endoscopic check list was gathered and for an accurate record of mortality percentage; within 30 days, information were collected using phone calls. All endoscopies were done by Olympus machine (Q145, manufactured in Japan).
The adequate definition of UGIB is associated with vomiting, enough grand vomiting, vomiting containing light blood, melena, and presence of light blood in nasogastric tube.[8] The mean by endoscopy hours during the day was between 8 am and 14 compared with the next 18 h and the mean by days off a week was from Saturday to Thursday and Friday in the holidays. Moreover, the purpose of endoscopic treatment was an injection of epinephrine, argon plasma coagulation, band ligation, or combination therapy with hemoclips (a malleability mental instrument that using for ligation of blood vessel. The used hemostasis clip was Boston single use rotatable with length of 235 cm and diameter of 2.8 mm). Patients with active bleeding, visible veins, and deposits were transferred to the Intensive Care Unit and patients with flat spat or adherent clot were transferred to the section. Patients with clean wound or nonbleeding Mallory–Weiss or absence of findings on endoscopy were discharged.[11]
The aim of morbidity was the length of hospital stay, number of blood products was received, and the need for endoscopy. Rebleeding was defined as hemoglobin drop of more than 2 after stabilization of hemoglobin or hemodynamic instability after hemodynamic stabilization or out-breaks of reactive hematemesis.[7,9] The purpose of co morbidities was cardiovascular disease (dysrhythmias, acute syndrome after a corner, heart failure), liver disease (cirrhosis), pulmonary diseases (acute respiratory failure, chronic obstructive pulmonary disease), kidney disease (creatinine >4, patients on dialysis), neurological disorders (delirium, dementia, stroke within the last 6 months), and malignancy[2,5,7] and the mean by various reasons were gastrointestinal bleeding, angioectasia, the Dieulafoy lesion, and Mallory–Weiss.
All the information on the patient's clinical and hospital records collected by the data collection form and recorded. To determine the mortality and death less than a month and death of late, it was contacted with him. Her family in case of death, and the cause of death was questioned and recorded for each patient. Data entered into the computer at the end and analyzed by SPSS version 23 (manufactured by IBM company, NY, USA) using Chi-square, t-test, and one-way analysis of variance.
Results
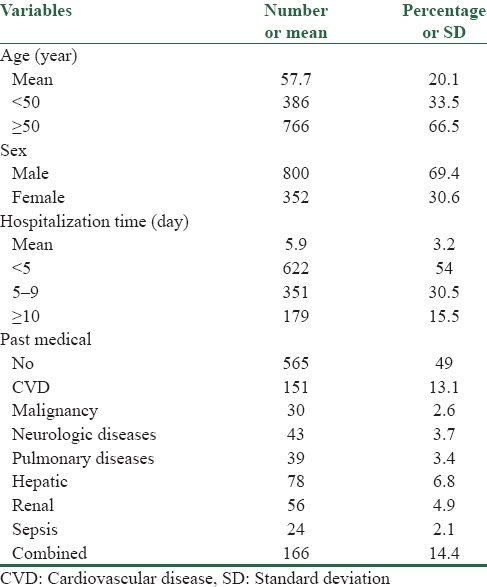
In this study, 1152 endoscopy were studied. The mean age of patients was 57.7 ± 20.1 years. Three hundred and eighty-six (33.5%) patients were aged <50 years and 766 cases (66.5%) were aged 50 years and older. Eight hundred patients (69.4%) were male and 352 cases (30.6%) were female. Five hundred and eighty-seven patients (51%) patients had underlying medical conditions that heart disease was the most common disease observed in these patients. Notably, hematemesis was the most common symptom referring. The patient's general demographic variables are shown in Table 1.
Table 1.
Frequency distribution of demographic data in the studied patients
Of 1152 patients, endoscopy in 803 patients (69.7%) were done by attendant and in 349 (30.3%) was done by the fellowship. The mean time from admission to perform endoscopy was 14.9 ± 11.1 h. About 384 patients (33.3%) in <12 h of admission undergone endoscopy, 717 patients (62.2%) in 12–24 h after admission, and 51 (4.4%) after 24 h of admission. Nine hundred and seventy-three cases (84.5%) of endoscopy performed during the working days and 179 (15.5%) were performed on holidays. Moreover, 801 cases (69.5%) of endoscopy were done in the morning and 351 cases (30.5%) were performed in the evening and night shifts [Figure 1].
Figure 1.
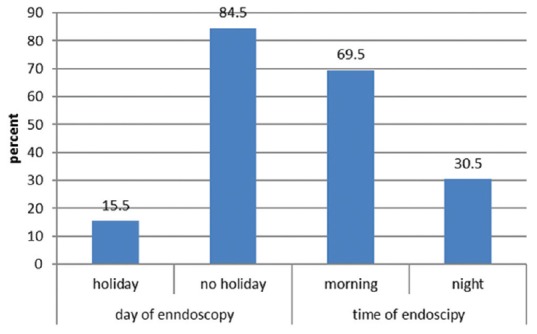
Frequency percentage of the time and day of endoscopy
Based on Figure 2, the most common source of bleeding in patients was multi-sources bleeding with a frequency of 239 cases (20.9%). In terms of clinical treatment, 33 (2.9%) patients were undergoing surgery, 633 cases (54.9%) had regular blood transfusions, and 274 cases (23.8%) underwent endoscopy [Table 2]. Notably, 13 (1.1%) of the patients died in the hospital and 28 patients (2.4%) died in less than a month after discharge. According to Table 3 and Figure 3, the day and time of endoscopy had no significant effect on mortality in hospital and less than a month after, but hospital death in whom underwent endoscopy by fellowship was significantly higher (P = 0.004) while for the death less than a month, there was no significant relationship with the physician endoscopist. The hospital mortality was not significantly different depending on the underlying disease, but for death less than a month, depending on the underlying disease mortality rate was significant (P < 0.001) [Table 4].
Figure 2.
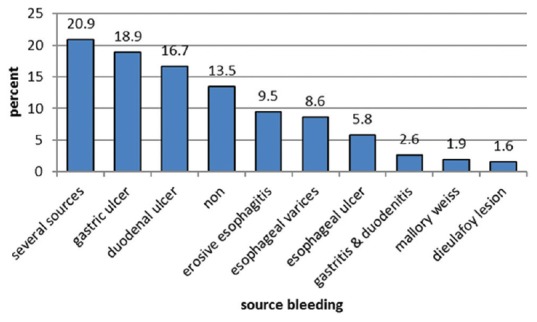
Frequency percentage of source bleeding in the patients
Table 2.
Frequency distribution of treatment activities in the patients
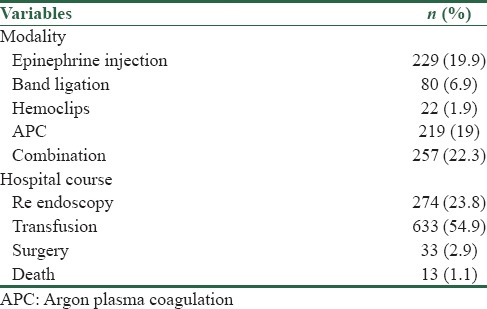
Table 3.
Frequency distribution of mortality based on demographic characteristics, time of endoscopy, endoscopist, and time of hospitalization to endoscopy
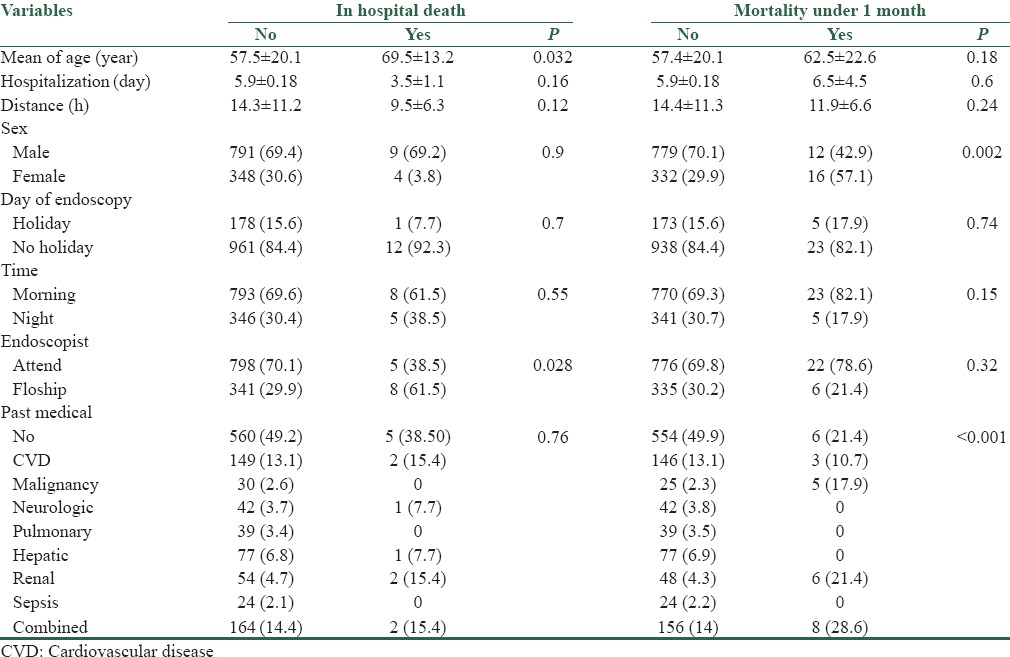
Figure 3.
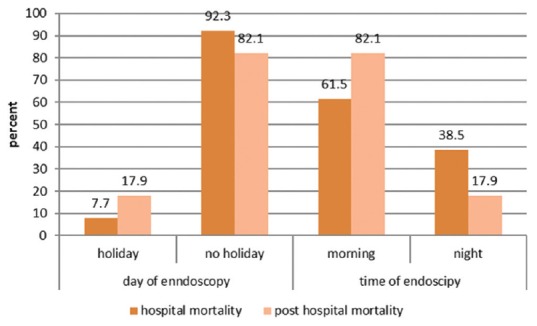
Frequency percentage of hospital mortality in the patients
Table 4.
Frequency distribution of mortality based on the source of bleeding, clinical signs and endoscopy findings
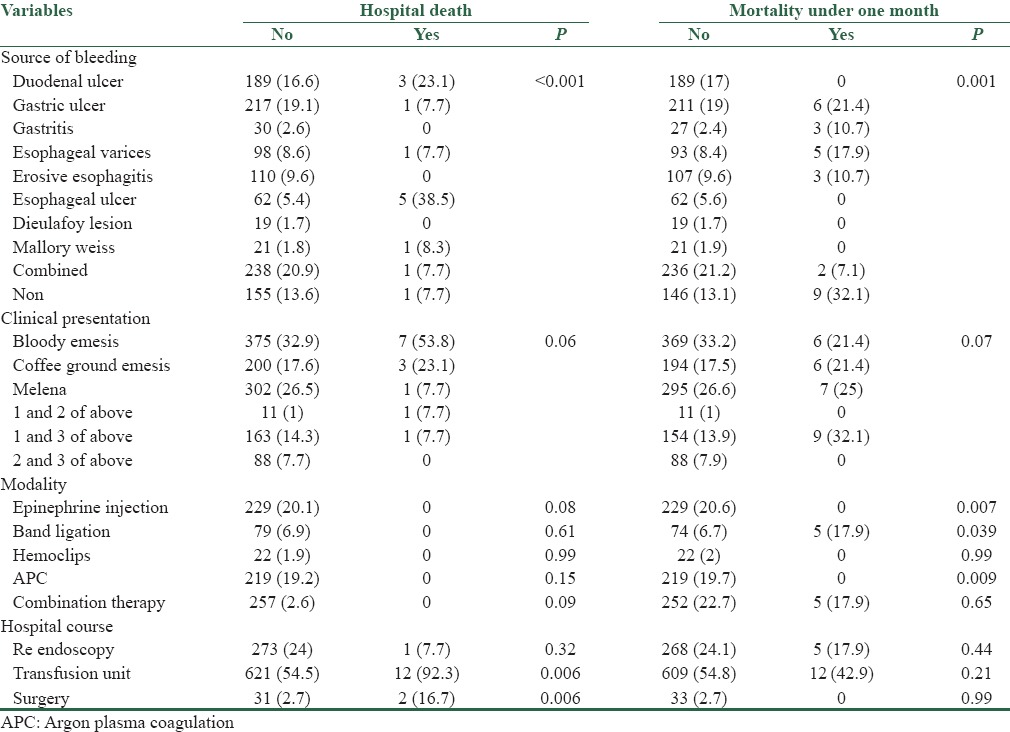
Logistic regression analysis on the above data showed that among the variables, the two variables, i.e., time of admission to endoscopy and endoscopic findings in hospital mortality had significant effect, so that the risk of death was 1.1 times more for each patient per hour distance (95% confidence interval [CI] = 1.004–1.24; P = 0.041). There is also a chance for active bleeding to the hospital death increased by 1.51 times (95%CI = 1.14–2.17; P = 0.005). There is also, risk of death increased from 1 month to the 1.13 for an underlying disease (95%CI = 1.02–1.25; P = 0.016).
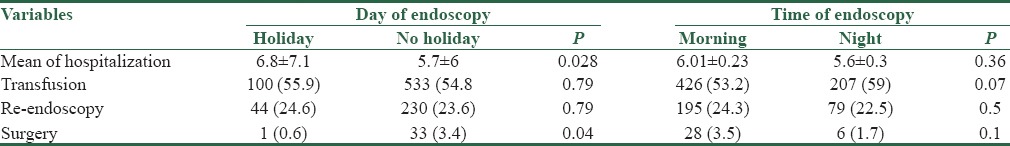
In Table 5, the frequency of findings related to the morbidity of patients in terms of day and time of endoscopy is shown. Based on these results, the mean duration of hospitalization in terms of holiday and nonholiday was significant, but there was no significant difference between morning and afternoon shifts. According to the table, blood transfusions and re-endoscopy were not significantly different in terms of day and time; however, a greater percentage of patients undergoing endoscopy was underwent surgery during the working days.
Table 5.
Frequency distribution of morbidity based on the time and day of endoscopy
Discussion
Some studies and previous experience showed that the morbidity and mortality rates of patients with gastrointestinal bleeding admitted to hospital and subsequently underwent endoscopy are different in terms of time of admission; so this study was performed to determine the association of major bleeding in patients with UGIB endoscopy time with morbidity and mortality of patients in Al Zahra Hospital emergency. In this study, 1152 patients were underwent study and results showed that received blood transfusion products and re-endoscopy in patients who underwent endoscopy in holidays had no significant difference compared with patients who underwent endoscopy in working days. Moreover, significant difference in the morning shifts compared to the evening and night shifts was not observed. In a similar study which was conducted by the Chodari and Palmer, it was observed that the time of endoscopy cannot be a predictor for the need of a re-endoscopy or need to blood products.[1]
Marwan et al. study showed that compared with patients who were hospitalized during the week because of nonvariceal UGIB, patients admitted on weekends need to less re-endoscopy. Brennan mentioned that sooner endoscopy of patients cannot (can) decrease the need for blood products and endoscopy. That the difference between these studies may be due to increased study subjects in the above studies, which can affect the results. Surgery on maternal during the weekdays (4.3 compared to 6.0) but did not differ in the morning and evening shifts.[12]
Although various studies have shown that the surgery was more in the morning than the evening shift, they are different from ours due to the active presence and participation of surgeons residents of different surgical disciplines in the center that naturally this can be useful for timely therapeutic procedures in patients with gastrointestinal bleeding in order to prevent death.
In this study, duration of hospitalization in patients with endoscopy in holiday and weekends was 8.6 days that compared with the duration of hospitalization in patients with endoscopy on week days which was 7.5 days was significantly higher but this difference between morning and night shifts was not significant that the results of our study was closer to studies by Kelvin and Marwan.[12,13] In Marwan's study, the average length of stay in hospital among patients admitted during the week was 5.2 days and for patients admitted on a weekend was 5.3 days[12] but study by Saeed et al. and another study by Ming, having endoscopy was not an important factor affect the duration of hospitalization.[14]
Among the causes of increased time of hospitalization in patients who were admitted on weekends, the administrative rules relating to admission and discharge can be mentioned. In our study, no association between mortality of patients underwent endoscopy in holiday and nonholiday days and also in morning and afternoon shifts was not seen. This difference was not significant in patients followed after 1 month of endoscopy but logistic regression analysis of hospital risk of death was 1.1 times for each time interval that this may be due to an increased risk of side effects, including exacerbation of underlying disease, resulting in an increase in the risk of mortality by delaying be endoscopy. In studies conducted by Tai et al. and Bjorkman et al., also no significant statistical association was observed between mortality of patients and endoscopy in the holiday and nonholiday days.[15,16]
Although, our study had some of limitations such as the lack of gastrointestinal bleeding patients and incomplete of hospital records.
Conclusion
According to the results of this study and other researches, it can be concluded that endoscopy in nonholiday and holiday days and the time of endoscopy has no significant effect on hospital mortality 1 month after discharge. However, other factors such as endoscopy by attendant or fellowship, time between admission to endoscopy, age and sex of the patients, underlying disease cause gastrointestinal bleeding, endoscopic findings, and modalities of hospital were significantly effective on in-hospital mortality and death 1 month after discharge. Moreover, faster and sooner endoscopy cannot reduce the rate of blood transfusions or reduce the length of hospital stay but faster endoscopy of patients can reduce the risk of in-hospital death.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chodari CP, Palmer KR. Timing of endoscopy for severe peptic ulcer hemorrhage: Out of hours emergency endoscopy is unnecessary. Gastroenterology. 1993;104:A55. [Google Scholar]
- 2.Lin HJ, Wang K, Perng CL, Chua RT, Lee FY, Lee CH, et al. Early or delayed endoscopy for patients with peptic ulcer bleeding. A prospective randomized study. J Clin Gastroenterol. 1996;22:267–71. doi: 10.1097/00004836-199606000-00005. [DOI] [PubMed] [Google Scholar]
- 3.ASGE Standars of Practice Committee. ASGE Guideline: The role of endoscopy in acute non-variceal upper-GI hemorrhage. Gastrointest Endosc. 2004;60:497–504. doi: 10.1016/s0016-5107(04)01568-8. [DOI] [PubMed] [Google Scholar]
- 4.Lee YC, Wang HP, Wu MS, Yang CS, Chang YT, Lin JT. Urgent bedside endoscopy for clinically significant upper gastrointestinal hemorrhage after admission to the intensive care unit. Intensive Care Med. 2003;29:1723–8. doi: 10.1007/s00134-003-1921-x. [DOI] [PubMed] [Google Scholar]
- 5.Spiegel BM, Vakil NB, Ofman JJ. Endoscopy for acute nonvariceal upper gastrointestinal tract hemorrhage: Is sooner better? A systematic review. Arch Intern Med. 2001;161:1393–404. doi: 10.1001/archinte.161.11.1393. [DOI] [PubMed] [Google Scholar]
- 6.Rockall TA, Logan RF, Devlin HB, Northfield TC. Incidence of and mortality from acute upper gastrointestinal haemorrhage in the United Kingdom. Steering committee and members of the National Audit of acute upper gastrointestinal haemorrhage. BMJ. 1995;311:222–6. doi: 10.1136/bmj.311.6999.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Laine L. Treatment of nonvariceal upper GI hemorrhage: What's happening in the real world. Am J Gastroenterol. 2004;99:1247–9. doi: 10.1111/j.1572-0241.2004.40252.x. [DOI] [PubMed] [Google Scholar]
- 8.Choudari CP, Rajgopal C, Elton RA, Palmer KR. Failures of endoscopic therapy for bleeding peptic ulcer: An analysis of risk factors. Am J Gastroenterol. 1994;89:1968–72. [PubMed] [Google Scholar]
- 9.Johnston JH. Endoscopic risk factors for bleeding peptic ulcer. Gastrointest Endosc. 1990;36(5 Suppl):S16–20. [PubMed] [Google Scholar]
- 10.Lau JY, Chung SC, Leung JW, Lo KK, Yung MY, Li AK. The evolution of stigmata of hemorrhage in bleeding peptic ulcers: A sequential endoscopic study. Endoscopy. 1998;30:513–8. doi: 10.1055/s-2007-1001336. [DOI] [PubMed] [Google Scholar]
- 11.Spiegel BM, Ofman JJ, Woods K, Vakil NB. Minimizing recurrent peptic ulcer hemorrhage after endoscopic hemostasis: The cost-effectiveness of competing strategies. Am J Gastroenterol. 2003;98:86–97. doi: 10.1111/j.1572-0241.2003.07163.x. [DOI] [PubMed] [Google Scholar]
- 12.Abougergi MS, Travis AC, Saltzman JR. Impact of day of admission on mortality and other outcomes in upper GI hemorrhage: A nationwide analysis. Gastrointest Endosc. 2014;80:228–35. doi: 10.1016/j.gie.2014.01.043. [DOI] [PubMed] [Google Scholar]
- 13.Tsoi KK, Ma TK, Sung JJ. Endoscopy for upper gastrointestinal bleeding: How urgent is it? Nat Rev Gastroenterol Hepatol. 2009;6:463–9. doi: 10.1038/nrgastro.2009.108. [DOI] [PubMed] [Google Scholar]
- 14.Saeed ZA, Cole RA, Ramirez FC, Schneider FE, Hepps KS, Graham DY. Endoscopic retreatment after successful initial hemostasis prevents ulcer rebleeding: A prospective randomized trial. Endoscopy. 1996;28:288–94. doi: 10.1055/s-2007-1005455. [DOI] [PubMed] [Google Scholar]
- 15.Tai CM, Huang SP, Wang HP, Lee TC, Chang CY, Tu CH, et al. High-risk ED patients with nonvariceal upper gastrointestinal hemorrhage undergoing emergency or urgent endoscopy: A retrospective analysis. Am J Emerg Med. 2007;25:273–8. doi: 10.1016/j.ajem.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 16.Bjorkman DJ, Zaman A, Fennerty MB, Lieberman D, Disario JA, Guest-Warnick G. Urgent vs.elective endoscopy for acute non-variceal upper-GI bleeding: An effectiveness study. Gastrointest Endosc. 2004;60:1–8. doi: 10.1016/s0016-5107(04)01287-8. [DOI] [PubMed] [Google Scholar]


