Abstract
Objective:
To investigate the common thinking, as reinforced by the International Classification of Headache Disorders, 3rd edition (beta), that occipital headaches in children are rare and suggestive of serious intracranial pathology.
Methods:
We performed a retrospective chart review cohort study of all patients ≤18 years of age referred to a university child neurology clinic for headache in 2009. Patients were stratified by headache location: solely occipital, occipital plus other area(s) of head pain, or no occipital involvement. Children with abnormal neurologic examinations were excluded. We assessed location as a predictor of whether neuroimaging was ordered and whether intracranial pathology was found. Analyses were performed with cohort study tools in Stata/SE 13.0 (StataCorp, College Station, TX).
Results:
A total of 308 patients were included. Median age was 12 years (32 months–18 years), and 57% were female. Headaches were solely occipital in 7% and occipital-plus in 14%. Patients with occipital head pain were more likely to undergo neuroimaging than those without occipital involvement (solely occipital: 95%, relative risk [RR] 10.5, 95% confidence interval [CI] 1.4–77.3; occipital-plus: 88%, RR 3.7, 95% CI 1.5–9.2; no occipital pain: 63%, referent). Occipital pain alone or with other locations was not significantly associated with radiographic evidence of clinically significant intracranial pathology.
Conclusions:
Children with occipital headache are more likely to undergo neuroimaging. In the absence of concerning features on the history and in the setting of a normal neurologic examination, neuroimaging can be deferred in most pediatric patients when occipital pain is present.
With a pediatric migraine prevalence of 3.9% to 11%1–3 and a lifetime aggregate prevalence of 54.4%2 for all pediatric headaches, a rational approach to the use of costly diagnostic studies is needed. The American Academy of Neurology/Child Neurology Society practice parameter states that neuroimaging is not indicated in a child with recurrent headache and a normal neurologic examination.4 Nonetheless, 45% of children with nonacute recurrent headaches will receive at least one neuroimaging study without clinical benefit.5
The American Academy of Neurology/Child Neurology Society practice parameter supports the use of neuroimaging in patients with recurrent headaches and abnormal neurologic examination findings, seizures, or a history of recent-onset severe headache or recent changes in the nature of the headache.4 Multiple pediatric emergency department (ED) studies have tried to identify warning signs deserving further workup,6–10 and 2 of the studies suggested that an occipital headache location signified intracranial pathology.7,9 Other warning signs not addressed in the practice parameter included younger age, severe intensity, and an inability to describe the quality of the pain.11
The International Classification of Headache Disorders, 3rd edition (ICHD-3) (beta)12 perpetuates the notion that occipital headaches in children raise clinical concern, stating that “[o]ccipital headache in children is rare and calls for diagnostic caution.”12 However, in children with normal neurologic examinations who are experiencing recurrent headaches, it is unclear whether this warning has merit. In a recent study, occipital headache location was not predictive of intracranial pathology in children.13 In this study, we investigated whether occipital headaches in children warrant neuroimaging.
METHODS
Study design.
This was a retrospective review of the cohort of consecutive pediatric patients who were seen at an urban child neurology clinic for a complaint of headache.
Standard protocol approvals, registrations, and patient consents.
The study was approved by the Rainbow Babies and Children's Hospital Institutional Review Board. There was no study-related contact with the patients in this retrospective chart review, and a consent waiver was granted by the Institutional Review Board.
Study setting and population.
All patients presenting to the child neurology clinic with a complaint of headache between January 1 and December 31, 2009, were evaluated for inclusion in the study. Patients were identified by searching ICD-9 codes related to headache. Exclusion criteria included age <12 months or ≥19 years of age, a chief complaint other than headache, being seen for a second opinion, and a previous workup for the same headache symptoms before the study period or as an inpatient. Because the clinic uses paper charts, some patients were excluded as a result of missing or incomplete charting.
Data extraction.
All available charts identified by the electronic query were collected, reviewed, and evaluated for inclusion. If the patient met any of the exclusion criteria, the reason for exclusion was recorded. Otherwise, patient data were collected for analysis. The sources of information within the paper chart included the physician's clinic visit note; a standard multipage questionnaire given to all new patients that covers family, social, and medical history; and imaging reports. Extracted data included age at presentation to the clinic; sex; comorbidities; headache characteristics and associated symptoms, frequency, and duration; physical examination findings; and CT and MRI results.
Data coding.
The headache locations were recorded as being frontal, frontotemporal, temporal, occipital, top of head, or generalized; patients could choose more than one location if needed. For analysis, participants were stratified as solely occipital location of pain, occipital plus other area(s) of head pain, or no occipital involvement. Headache severity was recorded as the most severe headache described by the patient (mild, moderate, or severe). Symptom duration was recorded as the midpoint duration if the patient offered a range (e.g., 9 months if the patient said symptoms had been present for 6–12 months). The examination was recorded as abnormal if there were any focal neurologic deficits or abnormalities, general physical examination findings suggestive of a neurogenetic syndrome, or documentation of neurodevelopmental delay or disability noted on examination. Imaging findings were classified as clinically significant or not clinically significant by one of the authors (N.B.), a board-certified child neurologist. When the values for variables were not recorded on the clinic intake form or were not documented in the chart, the variable was treated as negative or normal for the statistical analysis.
Each participant was classified with the use of ICHD-3 (beta) as meeting criteria for migraine, probable migraine, or not migraine, with one exception: because the clinic intake form included the lower-limit duration distinctions of <1 hour and 1 to 6 hours, headaches lasting >1 hour, rather than 2, were included as meeting duration criteria for pediatric migraine diagnosis.
We assessed 2 outcome questions: whether occipital headache location predicted whether neuroimaging was obtained and, within the subset of patients for whom imaging was obtained, whether occipital headache location predicted intracranial pathology. We were particularly interested in intracranial pathology that would necessitate a change in clinical management, including further testing, urgent interventions, or close clinical monitoring, and these findings were categorized as serious intracranial pathology.
Data analysis.
All data were analyzed with Stata/SE 13.0 (StataCorp, College Station, TX). Relative risk calculations and their confidence intervals were calculated with the cohort study epitab features. Comparisons of proportions were made with the Pearson χ2 and Fisher exact tests as appropriate. A value of p ≤ 0.05 was considered statistically significant. When the confidence intervals of the relative risk suggested statistical significance (i.e., the interval did not cross the null hypothesis) yet the Fisher exact test yielded a value of p > 0.05, we reported the findings as statistically insignificant.
RESULTS
A total of 586 patients were seen for headache during the study period. Of these, 230 patients (39%) were excluded for predefined criteria (figure), leaving a study population of 356 patients. There were 3 patients without neurologic examination documentation; 41 patients were missing family history documentation; and 37 patients did not have a headache location described. Forty-eight patients had an abnormal neurologic examination. The most common abnormalities documented included cranial nerve abnormalities, blurred disc margins on funduscopic examination, macrocephaly or microcephaly, or brisk or asymmetric reflexes. After the exclusion of the 48 patients with an abnormal examination, 308 patients remained for the primary analyses. Charts were reviewed 12 months after the end of the study period, resulting in a follow-up time ranging from 12 to 24 months, depending on the timing of the patient's initial presentation.
Figure. Determination of eligible patients for inclusion.
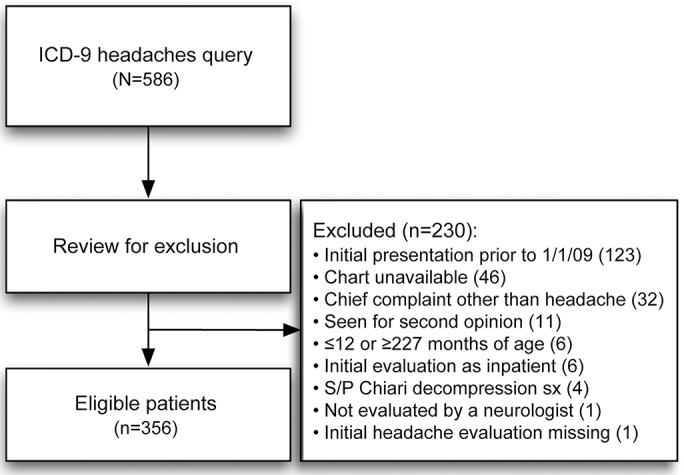
ICD-9 = International Classification of Diseases, 9th revision; S/P = status post; sx = symptoms.
Demographics and pain distribution.
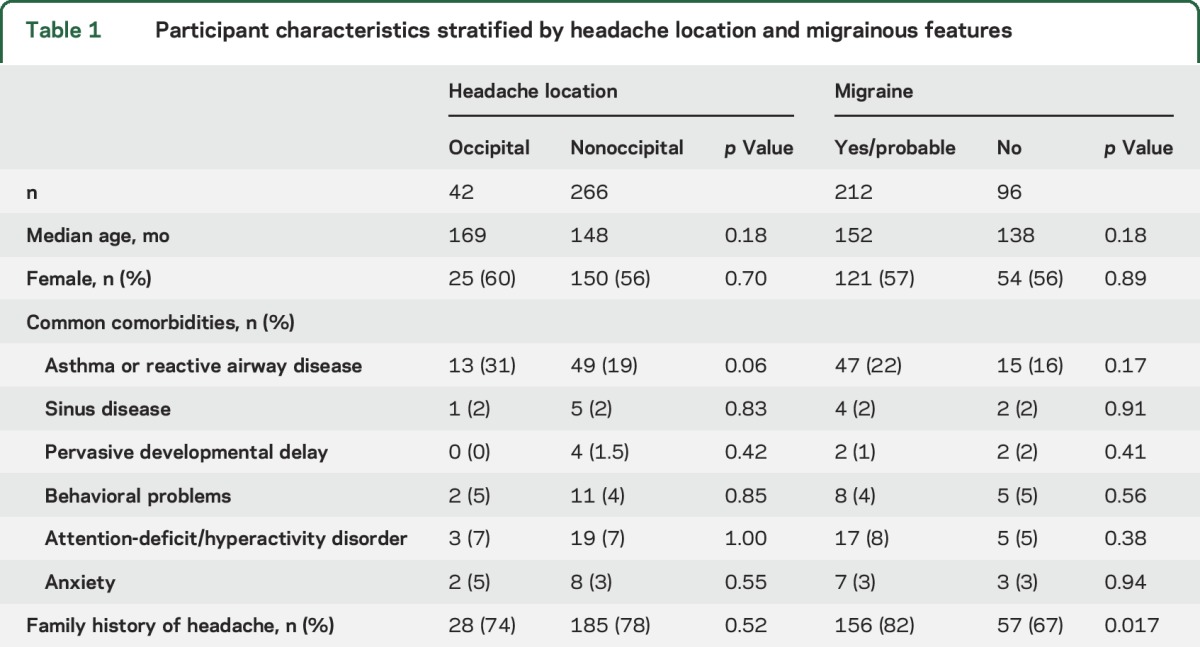
The median age of patients included in the study was 12 years (range 32 months–18 years), and 57% of patients were female. Headaches were solely occipital in 7% (n = 21), while a total of 14% (n = 42) of headaches included occipital pain. There was no association with an occipital location and age or sex (table 1).
Table 1.
Participant characteristics stratified by headache location and migrainous features
Headache features.
The characteristics of the patients' headaches, including location, duration of symptoms, severity, pain quality descriptions, and associated symptoms, are reported in table 2. One hundred twenty patients (34%) met criteria for migraine in children and an additional 120 patients met criteria for probable migraine for a total of 240 patients (67%). No association with age or sex was seen in patients with migraine or probable migraine vs no migraine, although the family history was more likely to be positive for headaches among patients meeting migraine or probable migraine criteria (table 1).
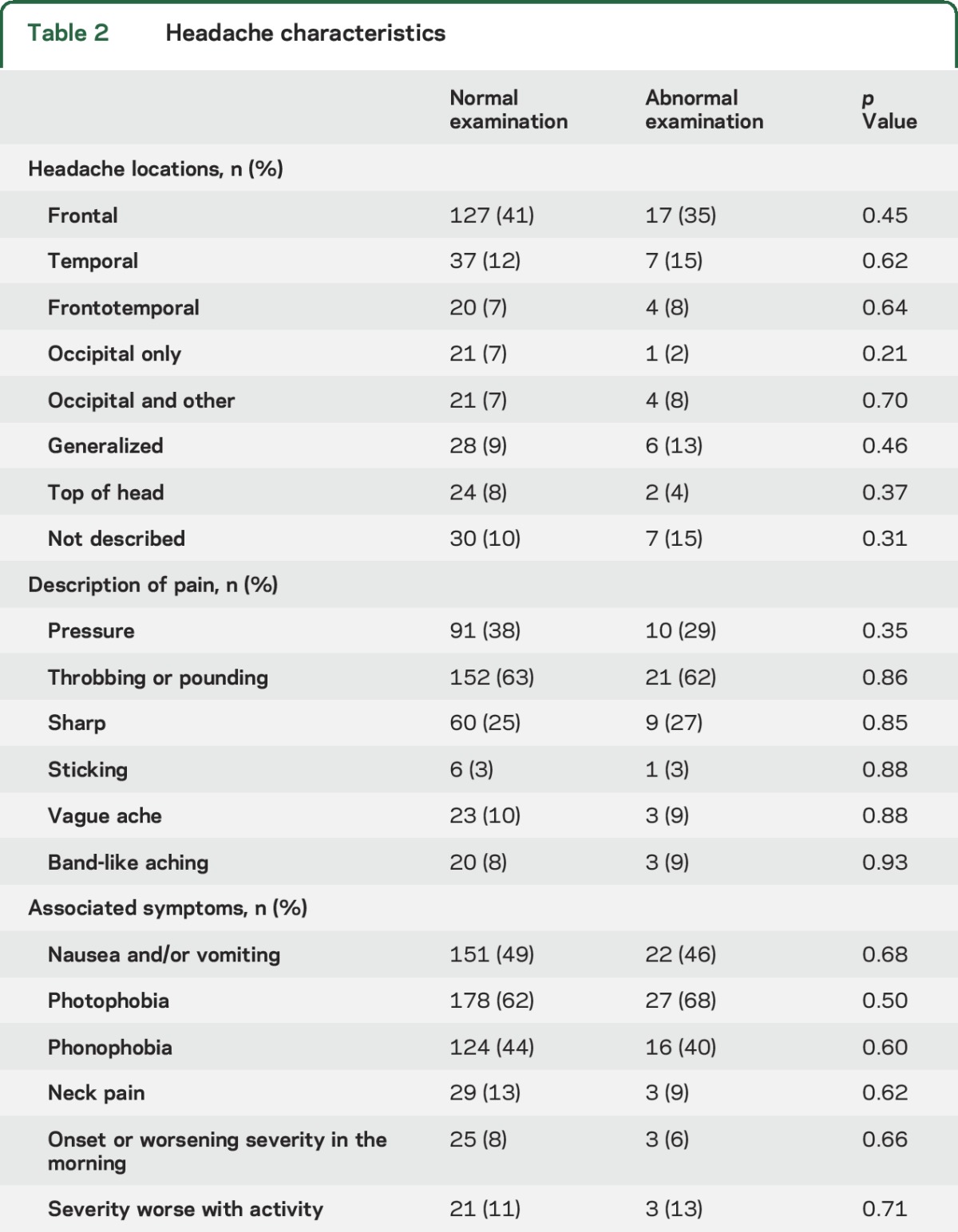
Table 2.
Headache characteristics
Neuroimaging.
Among the 308 patients with normal neurologic examinations and recurrent headaches, 205 had neuroimaging studies performed. Results were normal in 179 patients (87%), while 26 patients (13%) had abnormal findings. Fifty-four patients had a head CT; 132 patients had a head MRI; and 19 patients had both. Individuals who described occipital head pain were more likely to undergo neuroimaging than those without occipital involvement (table 3).
Table 3.
Imaging findings in children with normal physical examinations and occipital headaches, both exclusively occipital and any headaches including occipital pain, compared to those without occipital pain
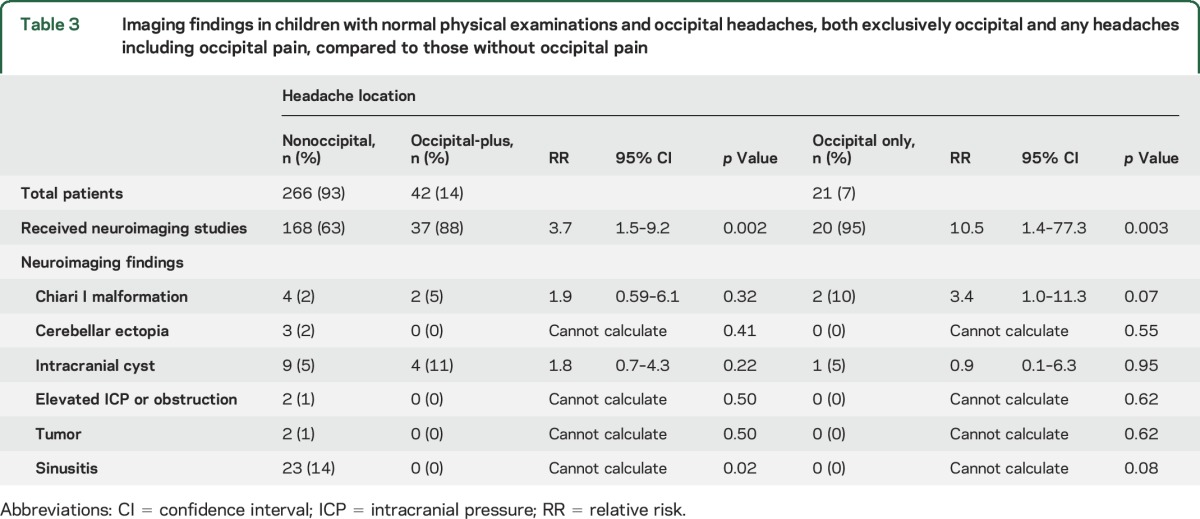
Among patients who underwent neuroimaging, the most common findings included sinusitis (n = 23), likely benign cyst (n = 13), Chiari 1 malformation (n = 6), and cerebellar ectopia (n = 3). A tumor was identified in 2 patients, 1 with a pituitary mass and 1 with a tectal glioma. There was no evidence of increased intracranial pressure from the tectal glioma. Two patients had imaging evidence of increased intracranial pressure, described in one patient as “optic disc and pituitary changes concerning for pseudotumor” and in the other as ventriculomegaly with flattening of the pituitary. Occipital pain was not associated with any intracranial pathology, whether the reported pain was solely occipital or occipital pain associated with other locations (table 3). There was a statistically significant inverse relationship between occipital pain and imaging evidence of sinusitis, with none of the 23 patients with sinusitis reporting occipital pain.
Migraine as a predictor.
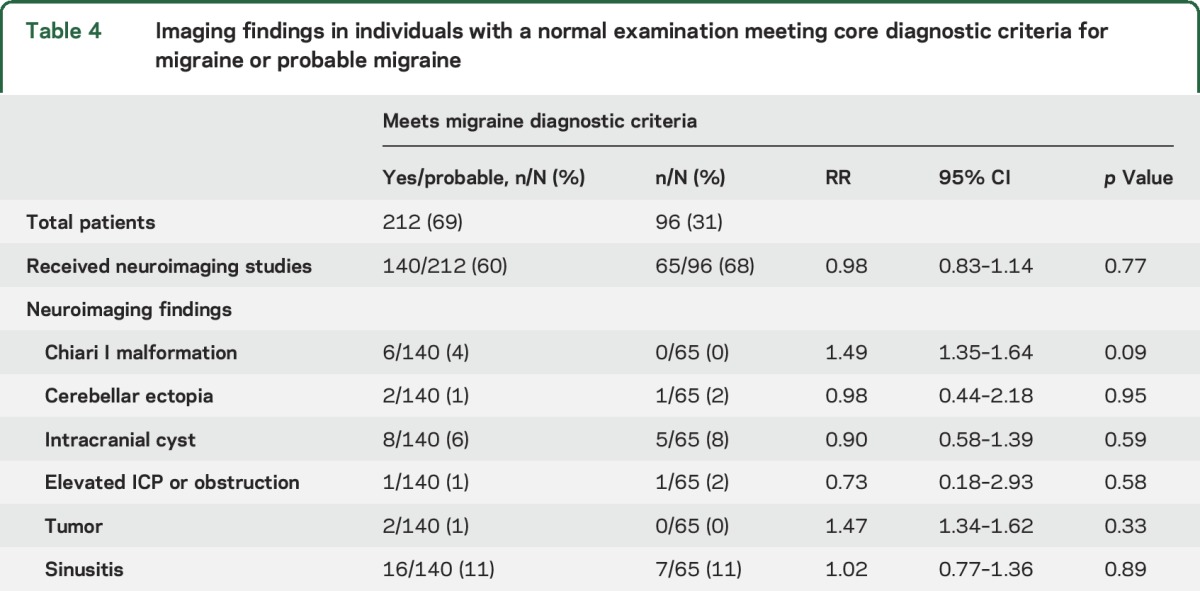
In post hoc analyses, we examined whether meeting criteria for a diagnosis of migraine could help predict the presence of serious intracranial pathology. However, the presence of migraine diagnostic criteria did not differentiate patients with and without intracranial pathology (table 4) even when the serious intracranial pathologies (tumor or elevated intracranial pressure) were grouped together for analysis.
Table 4.
Imaging findings in individuals with a normal examination meeting core diagnostic criteria for migraine or probable migraine
DISCUSSION
In this study, we examined the traditional thinking that occipital pain in children is rare and cause for concern. In our retrospective cohort study of pediatric patients in an outpatient child neurology office, 7% of headaches were solely occipital, and a total of 14% of headaches included occipital pain, making it less common than frontal headaches but similar in prevalence to all other headache locations. Thus, we propose that occipital headaches in children might be less rare than previously suspected. Furthermore, we did not find an association between occipital headaches and serious intracranial pathology. This was true whether the reported headaches were solely occipital or involved the occipital location along with other pain locations. In fact, among the 4 patients in our cohort with serious intracranial pathology, none reported occipital pain.
In our post hoc analysis, the fact that both patients with a tumor and one of the patients with elevated intracranial pressure met criteria for definite or probable migraine was notable but was not a statistically significant finding. In the patient with the pituitary mass, elements of the history might have led to imaging anyway, including headache typically occurring in the morning and waking the patient from sleep. The second patient had a nonobstructive tectal glioma, which could have been an incidental discovery in a patient with migraine.
The original studies that suggested occipital headache might be cause for concern, leading to a cautionary statement in the ICHD-3 (beta), were performed in the pediatric ED setting.7,9 In one study, only 2 of 150 patients identified occipital pain, and both patients had brain tumors; however, both also had abnormal neurologic examinations.9 In the other study, occipital headaches were identified as a risk factor for serious intracranial pathology, but the analysis combined children with occipital headaches with those who were unable to identify the pain location.7 Another important distinction and reason for caution when extrapolating from the ED to the outpatient clinic is the difference in acuity; children in the ED might have a first acute headache or a more severe presentation of their headache, while those seen in a neurologist's clinic are more likely to have recurrent headaches. Furthermore, and perhaps most relevant to the outpatient practitioner, all children in both studies who had serious intracranial pathology also had abnormal neurologic examinations. On the basis of our findings and a review of the original literature, we propose that without a worrying history and with a normal examination, neuroimaging can be deferred in most pediatric patients when occipital pain is present.
The correlation between occipital-only headaches and the neuroimaging finding of a Chiari I malformation approached significance, and our study might have been underpowered to identify an association. This finding was not seen in another study examining occipital head pain in children.13 While the radiologists at the study site typically use the definition of a Chiari I malformation as extension of the cerebellar tonsils ≥5 mm through the foramen magnum, we did not review the imaging directly for this study. We cannot exclude the possibility that this definition was inconsistently followed and that the clinical history of occipital head pain biased the radiologic interpretation. We therefore interpret this finding cautiously and adhere to the ICHD-3 (beta) description of headaches attributable to Chiari I malformations, which states that they are “usually occipital or suboccipital, of short duration (less than 5 minutes) and provoked by cough or other Valsalva-like manoeuvres.”12
Limitations of this study stem from its retrospective nature, including missing data for some of the patients, a lack of control over which patients did and did not receive neuroimaging studies, and the possibility that clinical decisions were based on information that was not recorded in the medical record. As mentioned, the imaging studies were not independently reviewed for this study, and a bias could have existed in the radiologic interpretations based either on the rationale listed for the study or on differences in measurement by the radiologists.
GLOSSARY
- ED
emergency department
- ICD-9
International Classification of Diseases, 9th revision
- ICHD-3
International Classification of Headache Disorders, 3rd edition
AUTHOR CONTRIBUTIONS
Joshua Bear: study concept and design, acquisition of data, analysis and interpretation of data, statistical analysis, manuscript preparation. Amy Gelfand and Peter Goadsby: critical revision of manuscript for intellectual content. Nancy Bass: study concept and design, critical revision of manuscript for intellectual content, study supervision.
STUDY FUNDING
No targeted funding reported.
DISCLOSURE
J. Bear reports no disclosures relevant to the manuscript. A. Gelfand receives grant support from NIH/National Center for Advancing Translational Sciences (8KL2TR000143-09), the Migraine Research Foundation, and the University of California, San Francisco Center for Translational Science Institute. She has received honoraria from Journal Watch Neurology, personal compensation for legal consulting, and consulting fees from Eli Lilly, eNeura, and Zosano, as well as travel expenses from Teva. P. Goadsby reports personal fees from Allergan, Amgen, and Eli-Lilly and Co; personal fees from Akita Biomedical, Alder Biopharmaceuticals, Autonomic Technologies Inc, Avanir Pharma, Cipla Ltd, Colucid Pharmaceuticals, Ltd, Dr Reddy's Laboratories, eNeura, Electrocore LLC, Novartis, Pfizer Inc, Promius Pharma, Quest Diagnostics, Scion, Teva Pharmaceuticals, Trigemina Inc, and Scion; and personal fees from MedicoLegal work, Journal Watch, Up-to-Date, and Oxford University Press. In addition, Dr. Goadsby has a patent magnetic stimulation for headache pending assigned to eNeura. N. Bass reports no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Bille BS. Migraine in school children: a study of the incidence and short-term prognosis, and a clinical, psychological and electroencephalographic comparison between children with migraine and matched controls. Acta Paediatr Suppl 1962;136:1–151. [PubMed] [Google Scholar]
- 2.Wöber-Bingöl C. Epidemiology of migraine and headache in children and adolescents. Curr Pain Headache Rep 2013;17:341. [DOI] [PubMed] [Google Scholar]
- 3.Abu-Arefeh I, Russell G. Prevalence of headache and migraine in schoolchildren. BMJ 1994;309:765–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lewis DW, Ashwal S, Dahl G, et al. Practice parameter: evaluation of children and adolescents with recurrent headaches: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 2002;59:490–498. [DOI] [PubMed] [Google Scholar]
- 5.Graf WD, Kayyali HR, Alexander JJ, Simon SD, Morriss MC. Neuroimaging-use trends in nonacute pediatric headache before and after clinical practice parameters. Pediatrics 2008;122:e1001–e1005. [DOI] [PubMed] [Google Scholar]
- 6.Burton LJ, Quinn B, Pratt-Cheney JL, Pourani M. Headache etiology in a pediatric emergency department. Pediatr Emerg Care 1997;13:1–4. [DOI] [PubMed] [Google Scholar]
- 7.Conicella E, Raucci U, Vanacore N, et al. The child with headache in a pediatric emergency department. Headache 2008;48:1005–1011. [DOI] [PubMed] [Google Scholar]
- 8.Lewis DW. Headache in the pediatric emergency department. Semin Pediatr Neurol 2001;8:46–51. [DOI] [PubMed] [Google Scholar]
- 9.Lewis DW, Qureshi F. Acute headache in children and adolescents presenting to the emergency department. Headache 2000;40:200–203. [DOI] [PubMed] [Google Scholar]
- 10.Scagni P, Pagliero R. Headache in an Italian pediatric emergency department. J Headache Pain 2008;9:83–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lewis DW. Red flags in children who present with headache: how to recognize a serious problem. Nat Clin Pract Neurol 2008;4:412–413. [DOI] [PubMed] [Google Scholar]
- 12.Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013;33:629–808. [DOI] [PubMed] [Google Scholar]
- 13.Eidlitz-Markus T, Zeharia A, Haimi-Cohen Y, Konen O. Occipital and craniocervical pain and brain MRI in children with migraine. Pediatr Neurol 2014;50:347–352. [DOI] [PubMed] [Google Scholar]


