A 67-year-old man with a 45-pack-year smoking history presented with worsening dyspnea. His resting oxygen saturation was 94%, declining to 86% after walking for 60 meters. A pulmonary examination revealed inspiratory crackles at the bases and diminished breath sounds at the apices. A cardiovascular examination showed normal results, without peripheral edema. A chest x-ray showed hyperinflation and increased interstitial markings. Pulmonary function tests were obtained (Table; Figure).
Table.
Pulmonary Function Test Resultsa
| Patient’s Values | Predicted, % | LLN | ||
|---|---|---|---|---|
| Measured | Predicted | |||
| FVC, L | 3.84 | 5.02 | 76 | 4.01 |
| FEV1, L | 2.30 | 3.73 | 62 | 2.88 |
| FEV1/FVC ratio | 0.60 | 0.74 | 0.65 | |
| FEF25%–75%, L/s | 0.98 | 2.89 | 34 | 1.16 |
| TLC, L | 5.21 | 7.70 | 68 | 6.55 |
| RV, L | 1.22 | 2.67 | 46 | 2.00 |
| FRC, L | 3.17 | 3.85 | 82 | 2.87 |
| DLCO, mL/mm Hg/min | 8.9 | 30.16 | 30 | 23.24 |
| VA, L | 4.46 | 7.70 | 58 | 6.55 |
| DLCO/VA, mL/mm Hg/min/L | 1.99 | 3.92 | 51 | |
Abbreviations: DLCO/VA, carbon monoxide diffusing capacity ÷ alveolar volume; FEF25%–75%, forced expiratory flow 25%–75% of forced vital capacity; FEV1/FVC, ratio of forced expiratory volume in the first second of expiration to forced vital capacity; FRC, functional residual capacity; LLN, lower limit of normal; RV, residual volume; TLC, total lung capacity; VA, alveolar volume.
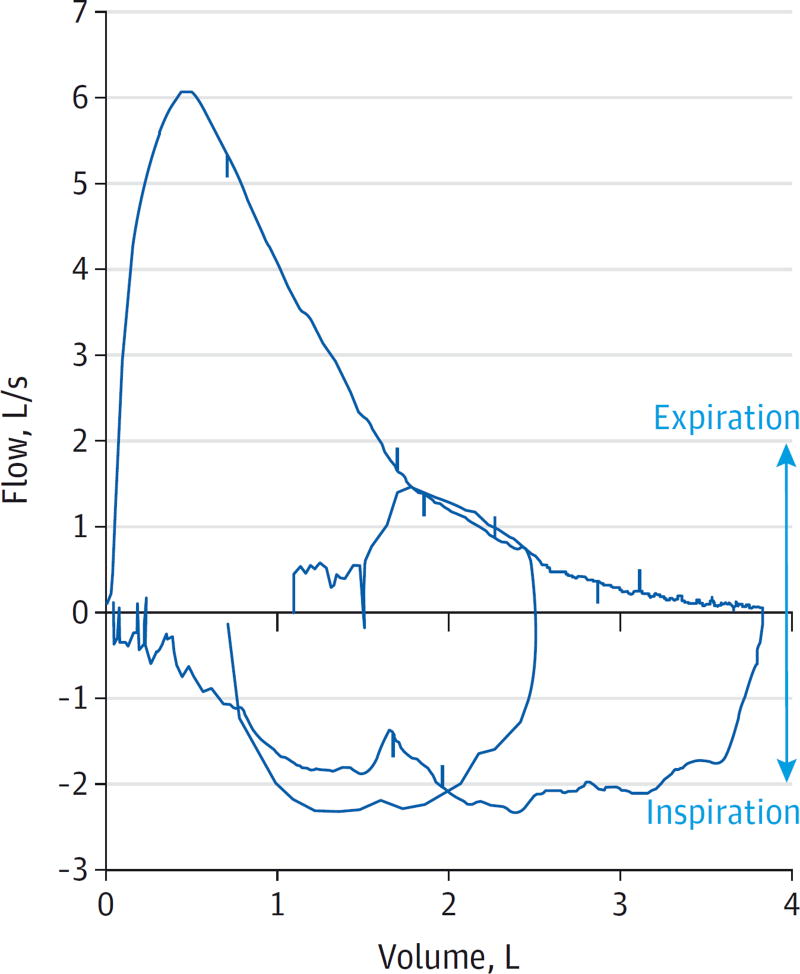
Figure.
Flow volume loop
Test Characteristics
Pulmonary function tests are essential for diagnosing and assessing severity of many pulmonary disorders (eTable in the Supplement). Spirometry measures forced vital capacity (FVC; the total exhaled volume) and the forced expiratory volume in the first second of expiration (FEV1) during a rapid and complete exhalation after maximal inspiration.1
A reduced FEV1/FVC ratio indicates airflow obstruction, while a normal ratio suggests normal spirometry or restrictive impairment. Mild airflow obstruction may exist with a normal FEV1/FVC ratio and is suggested by diminished forced expiratory flow (FEF25%–75%) in the middle half of the FVC and concave shape of the expiratory limb of the flow-volume loop (FVL).2 Restriction is suggested by reduced FVC and FEV1 with a normal or elevated FEV1/FVC ratio, but must be confirmed by measuring lung volumes. Bronchodilator testing compares spirometry before and after an inhaled short-acting bronchodilator. Complete reversibility of airflow obstruction after bronchodilator inhalation suggests asthma rather than chronic obstructive pulmonary disease, although a lack of response does not exclude asthma or exclude benefit from bronchodilator therapy.2 An FVL is a graphical representation of flow rate vs volume during a maximal exhalation and inhalation. FVL patterns can suggest poor-quality spirometry, restriction, diffuse airflow obstruction, or a central airway–obstructing lesion (see examples2).
Lung volume measurements, ideally obtained by plethysmography, estimate the volume of the lungs at maximal inhalation (total lung capacity [TLC]), relaxed exhalation (functional residual capacity [FRC]), and maximal exhalation (residual volume [RV]).3 A low TLC indicates restriction, while elevation of TLC and RV suggest hyperinflation and air trapping respectively, indicating obstruction. Pseudo-restriction is defined as an elevated RV due to prominent air trapping with a normal or slightly increased TLC, thereby reducing the FVC.
The carbon monoxide diffusing capacity (DLCO), measured using a test gas with a small amount of carbon monoxide, reflects the ability of the lungs to exchange gas into the bloodstream; it is diminished in emphysema, interstitial lung disease, pulmonary vascular disease, and anemia.4 Dividing the DLCO by the alveolar volume(VA) attempts to distinguish between a low DLCO due to abnormal gas exchange and a low DLCO due to reduced lung volume, although this is not a perfect correction.5 Medicare reimbursement ranges from $36.18 for spirometry to $168.73 for complete pulmonary function testing (eTable in the Supplement).6
Pulmonary function test results depend on patient effort. Normal ranges are related to the patient’s sex, age, race, and body size. Interpretation requires patient-appropriate reference equations that allow calculation of individualized predicted values and lower limits of normal.2 Although an FEV1/FVC ratio (<0.70) has been used to define airflow limitation,7 the ratio declines with age and current recommendations favor defining a low ratio as below the lower limit of normal.2
Application of Test Results to This Patient
The FVL demonstrates a smooth expiratory flow, which suggests good patient effort. The concave upward expiratory limb suggests obstructive lung disease but does not exclude coexisting restriction. The patient’s FEV1/FVC ratio is below the lower limit of normal. When airflow obstruction is present, severity is graded by FEV1 as a percentage of the predicted value. This patient’s FEV1 of 62% indicates moderate airflow obstruction.2
Along with a reduced FEV1/FVC ratio, the patient has a FVC below the lower limit of normal, suggesting either a mixed obstructive and restrictive deficit or pseudorestriction. The patient described in this article has a TLC below the lower limit of normal, indicating true restriction.
The cause of a reduced DLCO is best determined together with spirometry and lung volume measurement. This patient’s severely reduced DLCO, and DLCO/VA, accompanied by airflow obstruction (suggesting emphysema) and restriction (suggesting interstitial lung disease), suggests a combination of these processes.
What Are Alternative Diagnostic Testing Approaches?
Pulmonary function testing is the criterion standard for diagnosing obstructive and restrictive abnormalities. Gas exchange can be investigated with oximetry testing and arterial blood gas analysis; however, diffusing capacity detects more subtle changes.
Patient Outcome
Computed tomographic imaging confirmed emphysema and interstitial fibrosis, consistent with the pulmonary function tests. Ultimately, idiopathic pulmonary fibrosis was diagnosed. Catheterization of the right heart showed pulmonary hypertension, a likely contributor to the reduced DLCO. The patient was offered evaluation for lung transplantation.
Supplementary Material
HOW DO YOU INTERPRET THESE TEST RESULTS?
Primarily restrictive abnormality
Obstructive abnormality with pseudorestriction
Mixed obstructive and restrictive abnormality
Spirometry cannot be used to evaluate for obstruction in the setting of a restrictive abnormality
Answer
C. Mixed obstructive and restrictive abnormality
Clinical Bottom Line: Pulmonary Function Tests.
Pulmonary function tests are interpreted using published reference formulas based on a patient’s age, sex, race, and anthropomorphic characteristics.
Spirometry may demonstrate airflow obstruction and may suggest restrictive ventilatory impairment. Lung volumes confirm and quantify physiologic abnormalities.
Reduced gas exchange (DLCO) is nonspecific and may indicate parenchymal lung disease, pulmonary vascular disease, or anemia.
Acknowledgments
Funding/Support: Dr Heckman reports receipt of financial support from the National Institutes of Health grant T32 GM86308.
Footnotes
Quiz and Supplemental content at jama.com
Conflict of Interest Disclosures: Both authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Disclaimer: Dr O’Connor, JAMA Associater Editor, was not involved in the review of or decision to publish this article.
Additional Contribution: We thank the patient for sharing his experience and for granting permission to publish it.
References
- 1.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 2.Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–968. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- 3.Wanger J, Clausen JL, Coates A, et al. Standardisation of the measurement of lung volumes. Eur Respir J. 2005;26(3):511–522. doi: 10.1183/09031936.05.00035005. [DOI] [PubMed] [Google Scholar]
- 4.Macintyre N, Crapo RO, Viegi G, et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J. 2005;26(4):720–735. doi: 10.1183/09031936.05.00034905. [DOI] [PubMed] [Google Scholar]
- 5.Hughes JM, Pride NB. Examination of the carbon monoxide diffusing capacity (DL(CO)) in relation to its KCO and VA components. Am J Respir Crit Care Med. 2012;186(2):132–139. doi: 10.1164/rccm.201112-2160CI. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Medicare and Medicaid Services. [Accessed December 30, 2014];Physician fee schedule search: 2014. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/index.html?redirect=/PhysicianFeeSched/
- 7.Global Initiative for Chronic Obstructive Lung Disease. [Accessed March 23, 2015];Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2015. http://www.goldcopd.org.
- 8.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159(1):179–187. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- 9.Quanjer PH, Tammeling GJ, Cotes JE, et al. Lung volumes and forced ventilatory flows. Eur Respir J Suppl. 1993;16(suppl 16):5–40. doi: 10.1183/09041950.005s1693. [DOI] [PubMed] [Google Scholar]
- 10.Cotes JE, Chinn DJ, Quanjer PH, et al. Standardization of the measurement of transfer factor (diffusing capacity) Eur Respir J Suppl. 1993;16(suppl 16):41–52. doi: 10.1183/09041950.041s1693. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.