Abstract
Patient: Female, 57
Final Diagnosis: Classic Kaposi sarcoma
Symptoms: Skin
Medication: —
Clinical Procedure: Biopsy
Specialty: Surgery
Objective:
Rare disease
Background:
Kaposi sarcoma is a malignancy commonly linked to HIV infection or immunosuppression. An association with human herpes virus 8 (HHV-8) infection has also been reported. We present a case of classic Kaposi sarcoma in a female Mediterranean patient.
Case Report:
A 57-year-old white female of Greek ethnicity, with no history of HIV infection or immunosuppression, presented to the Surgical Out-patient Department of our Center, with complaints of extensive discolored skin lesion on both legs, initially considered as chronic vein insufficiency. Histopathological findings from skin biopsies revealed Kaposi sarcoma.
Conclusions:
Non-HIV-related Kaposi sarcoma is an HHV-8-related, angioproliferating skin cancer that can cause pain, disfigurement, and limb dysfunction. High suspicion of this condition can lead to early treatment and delay progression.
MeSH Keywords: Immunosuppression; Sarcoma, Kaposi; Skin Abnormalities
Background
Kaposi sarcoma is a multifocal vascular angioproliferative neoplasm, with cutaneous and extracutaneous involvement. It was first described by Moritz Kaposi as an idiopathic, multifocal, pigmented skin sarcoma [1].
Kaposi sarcoma can be classified in the following 4 groups: classic (rare, mainly in older men of Mediterranean, eastern European, or Jewish origin), epidemic or HIV-related (20 000 times more common than in the general population), endemic or African (not typically associated with immune deficiency), and iatrogenic (probably due to immunosuppression, after solid organ transplantation) [2].
We present a rare case of classic, non-HIV-related Kaposi sarcoma with extensive appearance in both legs, in a Mediterranean woman treated in the Surgical Out-patient Department of our Center.
Case Report
A 57-year-old white female patient with morbid obesity and extensive, bilateral, protruding, pigmented lesions of the lower extremities was referred to our surgical team for consultation. The patient had no history of HIV infection or immune diseases, and she did not report taking any immunosuppressant drugs. The lesions had been ineffectively treated for a long time with gradient compression stockings and regular physical activity, as correlated with chronic vein insufficiency (Figures 1, 2).
Figure 1.

Bilateral skin lesions in the lower extremities, initially considered as a result of chronic vein insufficiency.
Figure 2.

Extensive brittle lesions with high pigmentation and hemorrhagic points.
On physical examination, the patient presented extensive lesions that were highly pigmentated, brittle, hemorrhagic, and sensitive to palpation. Complete blood count, markers of thrombosis, and full blood laboratory examination showed results within normal range. Due to the refractory nature of the lesions, and the lack of clinical improvement despite multiple attempts of treatment in other facilities, further investigation was performed and multiple skin and subcutaneous tissue biopsies were obtained.
Histopathology of the excised tissues revealed that the lesions were, in fact, a bilateral manifestation of Kaposi sarcoma (Figures 3, 4). After this diagnosis, although she did not mention any risk factors, she was tested for HIV infection, with negative results. Therefore, the patient was referred to the Oncology Department for further management. Unfortunately, no further follow-up was available, as the patient died of acute myocardial infarction 2 months after diagnosis.
Figure 3.
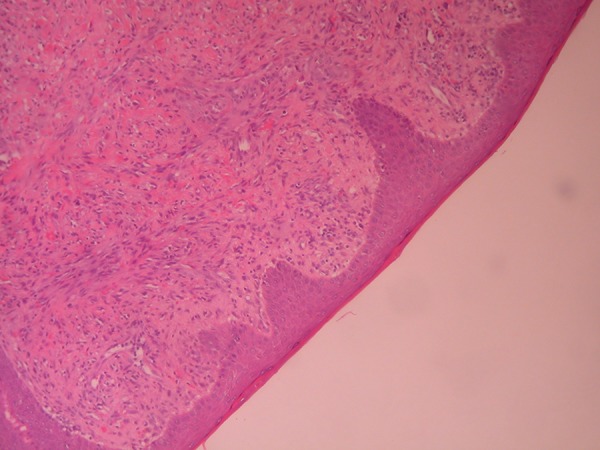
Dermal invasion of spindle cells and slit-like capillaries (H+E ×100).
Figure 4.
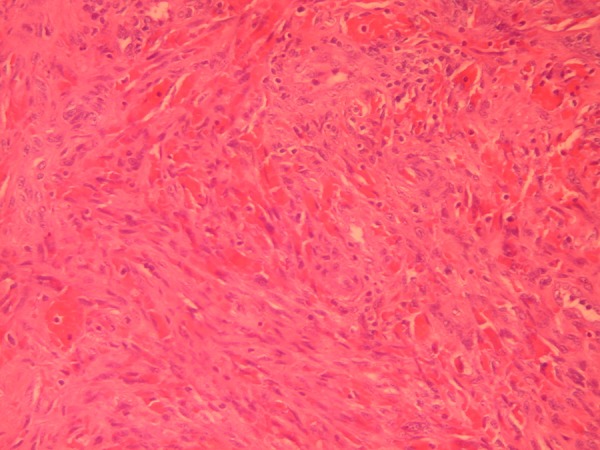
Spindle cells, slit-like capillaries, and red cell extravasation (H+E ×100).
Discussion
Skin lesions of classic Kaposi sarcoma commonly appear in the legs, face, and genitalia [3], as elliptical lesions with no pain or necrosis [2]. Dermatic lymphatic involvement [4] can also appear. Other than skin lesions and lymph nodes, Kaposi syndrome can present extracutaneous spread to the oral cavity and gastrointestinal tract, or present as lung injuries, even in patients with no HIV infection or other immune disorders [5].
Most of the cases of non-HIV-related Kaposi sarcoma occur in the fifth and sixth decade of life. In the USA and Europe, only 4–8% of the classic KS is observed in people under age 50 years [6]. This type appears in older persons (mean age over 70 years), especially in males (ratio 7: 1); according to recent studies, with a higher distribution people of white/American, Mediterranean, South American Hispanic, and black ethnicities, within the USA population [7]. Presentation in a younger female, as in our case, is very rare and can lead to problematic differential diagnosis.
The case that we report is a case of classic Kaposi sarcoma, not related to HIV infection, with no history of immunodeficiency due to medication or transplantation, and no other risk factors, which is rare. Cases that are not included in the 4 aforementioned recognized categories have also been reported [8], suggesting exposure to other environmental factors. Cross-sectional epidemiological studies have determined that seropositivity in HHV-8, now also called Kaposi Sarcoma-Associated Herpesvirus (KSHV), is strongly correlated with the risk of Kaposi sarcoma, and several longitudinal studies have shown that this virus precedes the onset of the disease. The presence of HHV-8 and any immune system imbalance are recognized factors that also promote the pathogenesis of this cancer [9,10], and a link to HPV infection has also been reported [11]. Immunosuppressant drugs are associated with the iatrogenic type of Kaposi sarcoma, especially in patients with kidney transplants, but they also seem to enhance the risk in other patients [12]. Hypertension has been correlated with poorer outcomes; plaque formation and more than 40 pack-years of smoking present a better progression-free survival [13]. Recently, the association of classic Kaposi sarcoma with miR-146a polymorphisms has been shown, but not with miR-149 [14].
Differential diagnosis can be difficult, especially in cases where risk factors are not present, as is our patient, who was HIV-negative, with good immune system and no risk factors. Her lesions were similar to those developed due to chronic venous insufficiency. Chronic venous insufficiency can create similar patches and plaques on the legs; therefore, for better differential diagnosis, skin biopsies and HHV-8 tests may be necessary, especially in cases that do not respond to conservative treatment [15]. The same lesions can also be misdiagnosed as cutaneous toxicities of BRAF inhibitors, such as dabrafenib, in cases treated for metastatic melanoma [16]. Diagnosis can be achieved through skin biopsies and polymerase-chain reaction (PCR) for HHV-8, or immunostaining for the HHV-8 antigen.
Treatment of the condition aims to reduce the lesions, delay the progression with subsequent alleviation of stress or other organ involvement and, finally, cure. Management involves local therapies (e.g., chemotherapy, radiotherapy, and alitretinoin), immunotherapy, and anti-HHV8 therapy [17]. Highly active antiretroviral therapy (HAART) is recommended for patients with simultaneous HIV infection.
As the disease is characterized by an indolent clinical behavior, close surveillance can be a valuable approach in selected cases [18]. Surgical excision and surveillance, when possible, can be curative in certain cases [19]. Lesions are highly radiosensitive, and the treatment is well tolerated and temporarily controls large localized lesions. Other conservative options include immunotherapy with interferon; chemotherapy with vinblastine, vincristine, bleomycin, or oral etoposide; or anthracyclines in more aggressive types. Valganciclovir can be effective in treating HHV-8 infection sarcoma [20]. Taxanes have also been reported to be effective against classic Kaposi sarcoma; however, a particular therapeutic strategy does not exist yet [21]. Thalidomide has also been used due to its antiangiogenic and immunomodulatory properties, but without promising results [22].
Patients with classic Kaposi sarcoma usually die of non-neoplastic conditions, or, uncommonly, of lymphoid malignancies [23]. Prognosis is considered relatively good, with 75% 5-year survival; therefore, early diagnosis and treatment are crucial [24].
Conclusions
Kaposi sarcoma is commonly related to HIV infection, but non-HIV-related cases are a distinct category and can occur with equivocal presentations. A high index of suspicion for these uncommon presentations should be maintained for prompt and correct diagnosis with early biopsy, followed by initiation of therapy if indicated.
Footnotes
Conflict of interest
None.
References:
- 1.Trujillo JM, Alves NR, Medeiros PM, et al. Clinical exuberance of classic Kaposi’s sarcoma and response to radiotherapy. An Bras Dermatol. 2015;90(6):883–86. doi: 10.1590/abd1806-4841.20153877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Phavixay L, Raynolds D, Simman R. Non AIDS Kaposi’s sarcoma leading to lower extremities wounds, case presentations and discussion. J Am Coll Clin Wound Spec. 2013;4(1):13–15. doi: 10.1016/j.jccw.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Attwa E, Gharib K, Albalat W, Amer A. Classical Kaposi sarcoma: Case reports with unusual presentation of the penis and scrotum. Int J Dermatol. 2016;55(10):e533–38. doi: 10.1111/ijd.13319. [DOI] [PubMed] [Google Scholar]
- 4.Gilani JA, Ullah Khan A, Shahid S, et al. Clinical presentation of non-HIV Kaposi sarcoma. J Coll Physicians Surg Pak. 2009;19(9):586–88. [PubMed] [Google Scholar]
- 5.Kodra A, Walczyszyn M, Grossman C, et al. Case report: Pulmonary Kaposi sarcoma in a non-HIV patient. F1000Res. 2015;4:1013. doi: 10.12688/f1000research.7137.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jan RA, Koul PA, Ahmed M, et al. Kaposi sarcoma in a non HIV patient. Int J Health Sci (Qassim) 2008;2(2):153–56. [PMC free article] [PubMed] [Google Scholar]
- 7.Hiatt KM, Nelson AM, Lichy JH, Fanburg-Smith JC. Classic Kaposi sarcoma in the United States over the last two decades: a clinicopathologic and molecular study of 438 non-HIV-reated Kaposi sarcoma patients with comparison to HIV-related Kaposi sarcoma. Mod Pathol. 2008;21(5):572–82. doi: 10.1038/modpathol.2008.15. [DOI] [PubMed] [Google Scholar]
- 8.Simonart T. Non-HIV related Kaposi’s sarcoma in former colonists/expatriates in Central Africa. J Travel Med. 2009;16(2):134–35. doi: 10.1111/j.1708-8305.2008.00289.x. [DOI] [PubMed] [Google Scholar]
- 9.Galleu A, Fozza C, Simula MP, et al. CD4+ and CD8+ T-cell skewness in classic Kaposi sarcoma. Neoplasia. 2012;14(60):487–94. doi: 10.1596/neo.11646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fonseca Aizpuru EM, Arias Miranda I, García-Alcalde ML, Nuño Mateo FJ. [A 28 year-old woman non-HIV with Kaposi’s sarcoma, thrombocytopenic purpura and hypogammaglobulinemia.] An Med Interna. 2008;25(2):100. doi: 10.4321/s0212-71992008000200013. [in Spanish] [DOI] [PubMed] [Google Scholar]
- 11.Gill K, Shah J. Unusual wounds: Kaposi sarcoma in patients with diabetes. Adv Skin Wound Care. 2006;19(4):198–201. doi: 10.1097/00129334-200605000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Wani GM, Ahmad SM, Qayoom S, et al. Corticosteroid induced, HHV-8 positive Kaposi’s sarcoma in a non-HIV elderly patient. J IMA. 2012;44(1) doi: 10.5915/44-1-9317. pii: 44-1-9317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sen F, Tambas M, Ciftci R, et al. Factors affecting progression-free survival in non-HIV-related Kaposi sarcoma. J Dermatolog Treat. 2016;27(3):275–77. doi: 10.3109/09546634.2015.1094177. [DOI] [PubMed] [Google Scholar]
- 14.Yang H, Lu QL, Wu XJ, et al. Association of genetic variations in miR-146a rs2910164 and miR-149 rs11614913 with the development of classic Kaposi sarcoma. Genet Mol Res. 2016;15(4) doi: 10.4238/gmr15048855. [DOI] [PubMed] [Google Scholar]
- 15.Que SK, DeFelice T, Abdulla FR, et al. Non-HIV-related Kaposi sarcoma in 2 Hispanic patients arising in the setting of chronic venous insufficiency. Cutis. 2015;95(6):E30–33. [PubMed] [Google Scholar]
- 16.Parakh S, Goh M, Andrews MC. Non-HIV-associated Kaposi sarcoma in an immunosuppressed melanoma patient treated with dabrafenib. J Clin Pharm Ther. 2016;41(3):354–56. doi: 10.1111/jcpt.12366. [DOI] [PubMed] [Google Scholar]
- 17.Akasbi Y, Awada A, Arifi S, et al. Non-HIV Kaposi’s sarcoma: A review and therapeutic perspectives. Bull Cancer. 2012;99(10):92–99. doi: 10.1684/bdc.2012.1636. [DOI] [PubMed] [Google Scholar]
- 18.Vincenzi B, D’Onofrio L, Frezza AM, et al. Classic Kaposi Sarcoma: To treat or not to treat? BMC Res Notes. 2015;8:138. doi: 10.1186/s13104-015-1076-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schmid BM, Holmes CM. Classic solitary Kaposi sarcoma of the foot in an immunocompetent patient: A case report. Wounds. 2016;28(9):E35–40. [PubMed] [Google Scholar]
- 20.Yun JJ, Preda V, Frankum B. Chronic human herpes virus 8 infection successfully treated with valganciclovir. World Allergy Organ J. 2009;2(7):128–29. doi: 10.1097/WOX.0b013e3181abe7b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Denis D, Régnier-Rosencher E, Kramkimel N, et al. First-line treatment with paclitaxel for non-HIV-related Kaposi sarcoma: experience in 10 cases. Br J Dermatol. 2016;174(4):905–8. doi: 10.1111/bjd.14237. [DOI] [PubMed] [Google Scholar]
- 22.Ben M’barek L, Fardet L, Mebazaa A, et al. A retrospective analysis of thalidomide therapy in non-HIV-related Kaposi’s sarcoma. Dermatology. 2007;215(3):202–5. doi: 10.1159/000106576. [DOI] [PubMed] [Google Scholar]
- 23.Ascoli V, Minelli G, Kanieff M, et al. Cause-specific mortality in classic Kaposi’s sarcoma: A population-based study in Italy (1995–2002) Br J Cancer. 2009;101(7):1085–90. doi: 10.1038/sj.bjc.6605265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stiller CA, Trama A, Brewster DH, et al. Descriptive epidemiology of Kaposi sarcoma in Europe. Report from the RARECARE project. Cancer Epidemiol. 2014;38(6):670–78. doi: 10.1016/j.canep.2014.09.009. [DOI] [PubMed] [Google Scholar]


