This analysis presents data on medical marijuana laws, cannabis use, and cannabis use disorders from 3 US national surveys conducted approximately 10 years apart.
Key Points
Question
Are US state medical marijuana laws one of the underlying factors for increases in risk for adult cannabis use and cannabis use disorders seen since the early 1990s?
Findings
In this analysis using US national survey data collected in 1991-1992, 2001-2002, and 2012-2013 from 118 497 participants, the risk for cannabis use and cannabis use disorders increased at a significantly greater rate in states that passed medical marijuana laws than in states that did not.
Meaning
Possible adverse consequences of illicit cannabis use due to more permissive state cannabis laws should receive consideration by voters, legislators, and policy and health care professionals, with appropriate health care planning as such laws change.
Abstract
Importance
Over the last 25 years, illicit cannabis use and cannabis use disorders have increased among US adults, and 28 states have passed medical marijuana laws (MML). Little is known about MML and adult illicit cannabis use or cannabis use disorders considered over time.
Objective
To present national data on state MML and degree of change in the prevalence of cannabis use and disorders.
Design, Participants, and Setting
Differences in the degree of change between those living in MML states and other states were examined using 3 cross-sectional US adult surveys: the National Longitudinal Alcohol Epidemiologic Survey (NLAES; 1991-1992), the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; 2001-2002), and the National Epidemiologic Survey on Alcohol and Related Conditions–III (NESARC-III; 2012-2013). Early-MML states passed MML between NLAES and NESARC (“earlier period”). Late-MML states passed MML between NESARC and NESARC-III (“later period”).
Main Outcomes and Measures
Past-year illicit cannabis use and DSM-IV cannabis use disorder.
Results
Overall, from 1991-1992 to 2012-2013, illicit cannabis use increased significantly more in states that passed MML than in other states (1.4–percentage point more; SE, 0.5; P = .004), as did cannabis use disorders (0.7–percentage point more; SE, 0.3; P = .03). In the earlier period, illicit cannabis use and disorders decreased similarly in non-MML states and in California (where prevalence was much higher to start with). In contrast, in remaining early-MML states, the prevalence of use and disorders increased. Remaining early-MML and non-MML states differed significantly for use (by 2.5 percentage points; SE, 0.9; P = .004) and disorder (1.1 percentage points; SE, 0.5; P = .02). In the later period, illicit use increased by the following percentage points: never-MML states, 3.5 (SE, 0.5); California, 5.3 (SE, 1.0); Colorado, 7.0 (SE, 1.6); other early-MML states, 2.6 (SE, 0.9); and late-MML states, 5.1 (SE, 0.8). Compared with never-MML states, increases in use were significantly greater in late-MML states (1.6–percentage point more; SE, 0.6; P = .01), California (1.8–percentage point more; SE, 0.9; P = .04), and Colorado (3.5–percentage point more; SE, 1.5; P = .03). Increases in cannabis use disorder, which was less prevalent, were smaller but followed similar patterns descriptively, with change greater than never-MML states in California (1.0–percentage point more; SE, 0.5; P = .06) and Colorado (1.6–percentage point more; SE, 0.8; P = .04).
Conclusions and Relevance
Medical marijuana laws appear to have contributed to increased prevalence of illicit cannabis use and cannabis use disorders. State-specific policy changes may also have played a role. While medical marijuana may help some, cannabis-related health consequences associated with changes in state marijuana laws should receive consideration by health care professionals and the public.
Introduction
Over the last 20 years, laws and attitudes regarding cannabis have changed. As of November 2016, 28 states have passed medical marijuana laws (MML). Many adults now favor legalizing recreational use, and fewer view cannabis as risky. Despite this view, while some can use cannabis without harm, potential consequences include impaired functioning, vehicle crashes, emergency department visits, psychiatric symptoms, and addiction. Over time, the prevalence of adult illicit use and related consequences has increased. Thus, identifying factors underlying increased adult illicit use is important. State MML may be one such factor.
Little is known about MML and adult cannabis outcomes. Two national studies showed greater use and DSM-IV–diagnosed disorders in MML states but did not examine differences before and after MML. One national study did so, finding increased post-MML cannabis use and cannabis disorders. However, this study only addressed 2004 to 2012, adults 20 years and older, and 10 states that changed MML status. To our knowledge, no study of differences before and after MML has used adult national data predating all MML, differentiated between earlier and more recent periods, or separately examined particular states. Differences between states that passed MML early vs late are important because the national normative context differed for early-MML states, when few such laws existed, and late-MML states, enacted when more states had MML. Also, earlier data can show if trends in cannabis use and disorder in late-passing states began prior to their MML. Further, California and Colorado warrant separate, secondary examination. In 1996, when California passed the first MML, its cannabis rates were higher than other states, and thus its MML may have had little additional effect. Colorado (MML passed in 2000) experienced unique policy changes in 2009-2010 (eAppendix 1 in the Supplement) followed by increases in medical user applications from 500 per month to greater than 10 000 per month and from no known dispensaries to greater than 900, potentially exerting additional impact on cannabis outcomes during the later period.
We examined MML, illicit cannabis use, and cannabis use disorders in 3 cross-sectional adult surveys: the 1991-1992 National Longitudinal Alcohol Epidemiologic Survey (NLAES), the 2001-2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), and the 2012-2013 National Epidemiologic Survey on Alcohol and Related Conditions–III (NESARC-III). Over this period, the national context for MML changed. In 1991-1992, no Americans lived in MML states; in 2001, 18.9% lived in MML states, and in 2012, more than one-third (34.3%) lived in MML states. We therefore addressed 3 questions. First, between 1991-1992 and 2012-2013 (the overall study period), were changes in the prevalence of illicit cannabis use and disorders greater in states that ever had MML vs never had MML? Second, between 1991-1992 and 2001-2002 (for convenience, termed the earlier period), did changes in prevalence differ between states that did and did not pass MML during this time, including and excluding California? Third, between 2001-2002 and 2012-2013 (for convenience, termed the later period), did changes in prevalence differ between never-MML states, states passing MML during the earlier period, and states passing MML during the later period? In investigating the later period, we again kept California separate and also separated Colorado, given its 2009-2010 changes.
Methods
Study Design and Participants
The NLAES, NESARC, and NESARC-III surveyed adults 18 years and older in households and group quarters, using similar multistage sampling designs. Sample weights were adjusted for selection probabilities and nonresponse. Field procedures were similar across surveys, except that the NLAES used paper-and-pencil interviews whereas the NESARC and NESARC-III used computer-assisted interviews. Because trained interviewers used similar procedures in all surveys, respondents were similarly exposed to interview questions, permitting examination of trends over time. Quality assurance included training, supervision, and callbacks to verify respondent data. The NLAES and NESARC protocols and consent procedures were approved by the institutional review boards at the US Bureau of the Census and the Office of Management and Budget; written consent was provided. The NESARC-III protocols and consent procedures were approved by institutional review boards at the National Institutes of Health and Westat; consent was verbal but recorded electronically, as approved by both institutional review boards. Overall response rates were 60% to 84%. Eleven states in which primary sampling units were not randomly selected in NESARC-III were excluded from analyses (Table 1), yielding 41 764 participants from the NLAES, 41 184 from the NESARC, and 35 549 from the NESARC-III, totaling 118 497 participants. Sample demographic characteristics are shown in eTable 1 in the Supplement.
Table 1. Difference in Predicted Prevalences of Past-Year Cannabis Use and DSM-IV Cannabis Use Disorder, 1991-1992 to 2012-2013: Never-MML States and Ever-MML States (Model 1).
| Outcome | Model 1, Prevalence (SE)a | |
|---|---|---|
| Never-MML Statesb (24 States) | Ever-MML Statesc (15 States) | |
| Cannabis use | ||
| 1991-1992 | 4.54 (0.39) | 5.55 (0.36) |
| 2012-2013 | 6.70 (0.39) | 9.15 (0.54) |
| Difference in prevalence | +2.17 (0.70)d | +3.60 (0.79)e |
| DiD (ever-MML vs never-MML states) | [Reference] | +1.43 (0.48)f |
| Cannabis use disorder | ||
| 1991-1992 | 1.35 (0.19) | 1.48 (0.19) |
| 2012-2013 | 2.30 (0.22) | 3.10 (0.34) |
| Difference in prevalence | +0.96 (0.38)g | +1.62 (0.47)h |
| DiD (ever-MML vs never-MML states) | [Reference] | +0.66 (0.30)i |
Abbreviations: DiD, difference-in-difference; MML, medical marijuana laws.
Prevalence based on participants in the 39 states included in all 3 surveys. States omitted: Alaska, Delaware, Hawaii, Idaho, Nebraska, New Hampshire, North Dakota, Rhode Island, South Dakota, West Virginia, and Wyoming. Prevalences back-transformed from marginal log-odds estimated from logistic regression interaction models (MML × survey) that included individual-level (sex, age, education, race/ethnicity, marital status, urbanicity, and poverty) and state-level (% male, % white, % <30 y, and % ≥25 y without a high school diploma) covariates. Predicted prevalences estimated by a model with a dichotomous MML variable (ever-MML states vs never-MML states).
Never-MML states (1996-2012): Alabama, Arkansas, Florida, Georgia, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Minnesota, Mississippi, Missouri, New York, North Carolina, Ohio, Oklahoma, Pennsylvania, South Carolina, Tennessee, Texas, Utah, Virginia, and Wisconsin.
Ever-MML states (1996-2012): Arizona, California, Colorado, Connecticut, Maine, Maryland, Massachusetts, Michigan, Montana, Nevada, New Jersey, New Mexico, Vermont, Oregon, and Washington.
P = .003; change in never-MML states between 1991-1992 and 2012-2013.
P < .001; change in ever-MML states between 1991-1992 and 2012-2013.
P = .004, change in never-MML states between 1991-1992 and 2012-2013.
P = .01; change in never-MML states between 1991-1992 and 2012-2013.
P = .001; change in ever-MML states between 1991-1992 and 2012-2013.
P = .03, change in never-MML states between 1991-1992 and 2012-2013.
Measures
The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS), a structured diagnostic interview, was used to assess substance use and DSM-IV substance use disorders. All 3 surveys included the same questions about illicit use in the prior 12 months, including cannabis. Illicit use was defined to participants as use without a prescription or other than prescribed, eg, to get high (eAppendix 2 in the Supplement). In the NLAES, information about cannabis was assessed only if participants used 12 or more times. For consistency with the NLAES, we analyzed cannabis use and disorders among NESARC and NESARC-III participants who used cannabis 12 or more times. Any illicit cannabis use in the past 12 months was analyzed, providing a consistent timeframe for use and disorders.
Participants with DSM-IV cannabis abuse or dependence in the past 12 months were coded positive for cannabis use disorder (abuse and dependence combined because their criteria reflect a single disorder). All AUDADIS versions included the same core questions covering cannabis disorder criteria. A minor difference between the NLAES and NESARC was that in the NLAES, criteria were assessed with 2 questions—1 on occurrence and 1 on recurrence—while in the NESARC and NESARC-III, single questions were used. Also, the NLAES but not the NESARC included 4 items assessing the “social impairment” and “use despite health problems” dependence criteria. Comparisons between DSM-IV cannabis diagnoses in the NLAES with and without these 4 questions yielded nearly identical prevalence (1.12% vs 1.06%, respectively) and near-perfect concordance (κ, 0.98), so these differences had little impact on results.
The NESARC and NESARC-III AUDADIS versions also had only minor differences. Four items were slightly reworded, 1 item was in the NESARC but not NESARC-III, and 1 item was in the NESARC-III but not NESARC. DSM-IV cannabis disorder diagnoses with and without these NESARC and NESARC-III items had near-identical prevalence and near-perfect concordance. Thus, these minor differences could not account for the substantial prevalence increases observed between surveys. Test-retest reliability and convergent validity of AUDADIS DSM-IV cannabis disorder diagnoses is documented extensively.
State-Level MML Variables
A team of legal scholars, policy analysts, and economists reviewed state policies to determine the year of MML passage. Three variables were then created (eTable 2 in the Supplement). One indicated participants in states passing MML between 1991 and 2012 (ever-MML states) vs others (never-MML states), 1 indicated participants in early-MML states vs non-early–MML states (ie, never-MML and late-MML states), and 1 indicated participants in early-MML states, late-MML states, and never-MML states. Early-MML states passed MML between 1991 and 2001 (in the earlier period). Late-MML states passed MML between 2002 and 2012 (in the later period). Never-MML states had no MML by 2012. Additional variables for secondary analyses represented California and Colorado separately.
Individual-Level and State-Level Control Covariates
Covariates included sex, age, education (less than high school vs others), race/ethnicity (Hispanic, non-Hispanic white, non-Hispanic black, and other; self-defined using US Census Bureau categories), marital status (unmarried vs others), urbanicity (metropolitan statistical areas vs others), and poverty (less than 100%, 100% to 200%, and greater than 200% of the federal poverty level). Following prior MML work, US Census data were used to define 4 state-level covariates: percent male, percent white, percent younger than 30 years, and percent 25 years and older without a high school diploma.
Statistical Analyses
We examined whether the degree of change between surveys differed in participants by state MML status using difference-in-difference (DiD) tests. By assuming that trends in non-MML states reflect what would have happened in MML states if they had not passed MML, DiD tests provide information about changes due to MML passage, with inferences strengthened if trends in MML and non-MML states did not differ before MML passage (ie, previous parallel paths). Difference-in-difference tests advantageously “difference out” fixed unmeasured factors and control for preexisting between-group differences that might bias results. By standardizing groups across time to the overall weighted distribution of model covariates, use of predicted marginal prevalences in the DiD approach additionally eliminates varying measured covariates as explanations of results.
The 3 survey data sets were concatenated, adding a variable indicating survey. Models included survey (NLAES, NESARC, and NESARC-III), MML indicators, survey by MML interaction terms, and covariates. Sample weights in multivariable logistic regression models generated weighted predicted marginal prevalence estimates (back-transformed from marginal log-odds) and SEs of cannabis outcomes in each survey within strata defined by MML variables. A first set of contrasts estimated between-survey change in predicted prevalences within MML strata. With a second set of contrasts, the DiD tests tested if these between-survey changes differed by MML strata. Difference-in-difference estimates differing significantly from 0 indicated differences in change between MML vs other states.
Separate models tested MML effects during the overall period (model 1), the earlier period (model 2), and the later period (model 3). In model 1 (1991-1992 vs 2012-2013), we evaluated MML effects by testing for differential changes between ever-MML states and never-MML states. In model 2 (1991-1992 vs 2001-2002), we evaluated early-MML effects by testing for differential changes in early-MML states vs remaining states (ie, late-MML and non-MML states), initially grouping California with other early-MML states (model 2A) and then examining California separately (model 2B). In model 3 (2001-2002 vs 2012-2013), we tested for differential changes between never-MML states (reference) and late-MML states, California, Colorado, and the other early-MML states.
We tested the parallel-path assumption of DiD estimators for late-MML states and Colorado by comparing their trends with non-MML states during the earlier period. Sensitivity analyses testing robustness of findings included (1) adding originally excluded NESARC and NESARC-III participants who only used cannabis 1 to 11 times to models 1, 2, and 3; (2) adding participants from all states included in each survey to models 1, 2, and 3; (3) recoding cannabis disorder to include withdrawal as a seventh criterion; and (4) omitting participants aged 18 and 19 years for consistency with earlier research. All analyses used SUDAAN version 11.0.1 (RTI International) and included survey weights and stratification variables to account for the complex survey design. Results were inspected for meaningful change from models 1, 2, and 3 if DiD tests gained or lost significance. All P values were 2-tailed, and significance was set at P < .05.
Results
Descriptive Predicted Prevalences of Illicit Cannabis Use and Disorder
Between 1991-1992 and 2001-2002, illicit use decreased and disorder changed little. Between 2001-2002 and 2012-2013, use and disorder increased. eTable 3 in the Supplement presents predicted prevalences of use and disorder in the 39 states analyzed, by survey and MML status.
Change in Illicit Cannabis Use and Cannabis Use Disorder by State MML Status: 1991-1992 to 2012-2013 (Model 1)
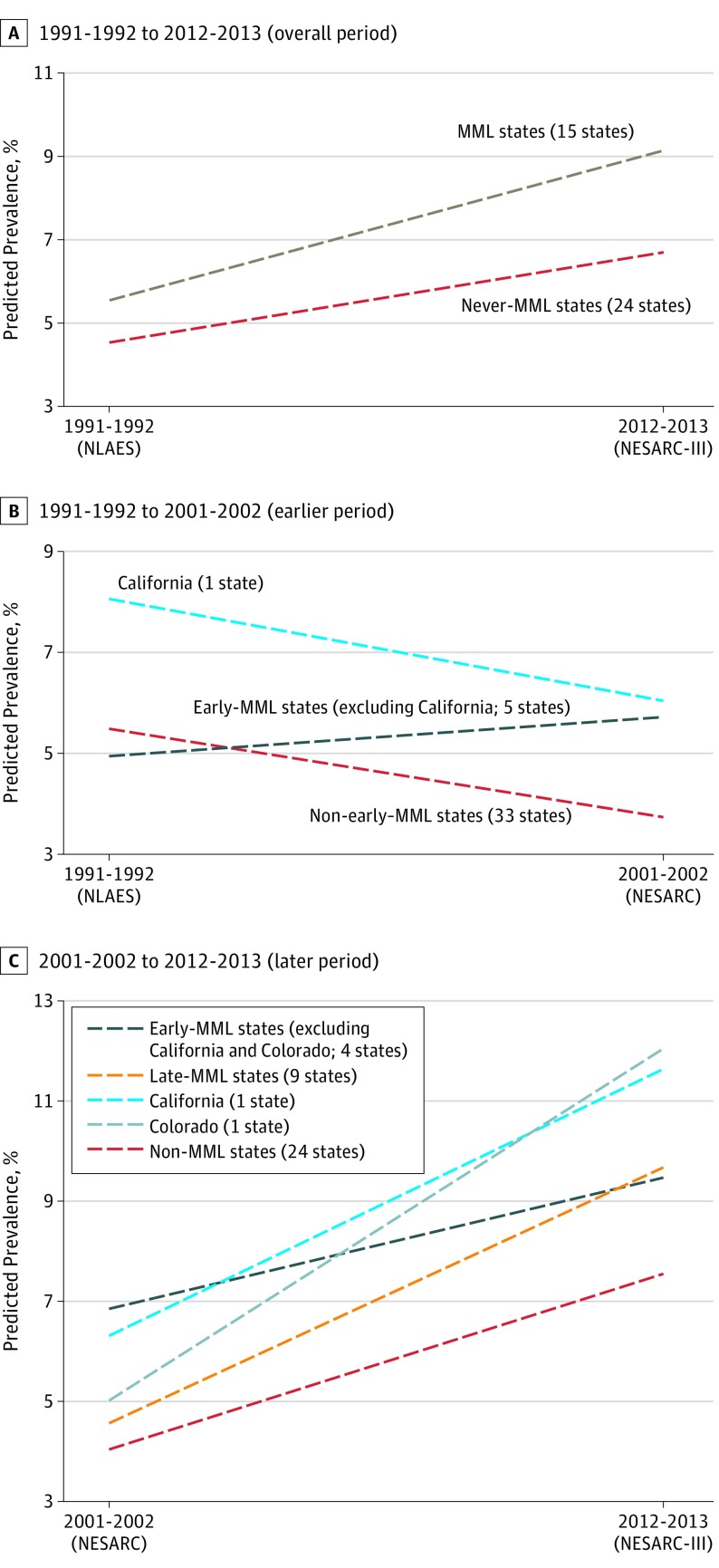
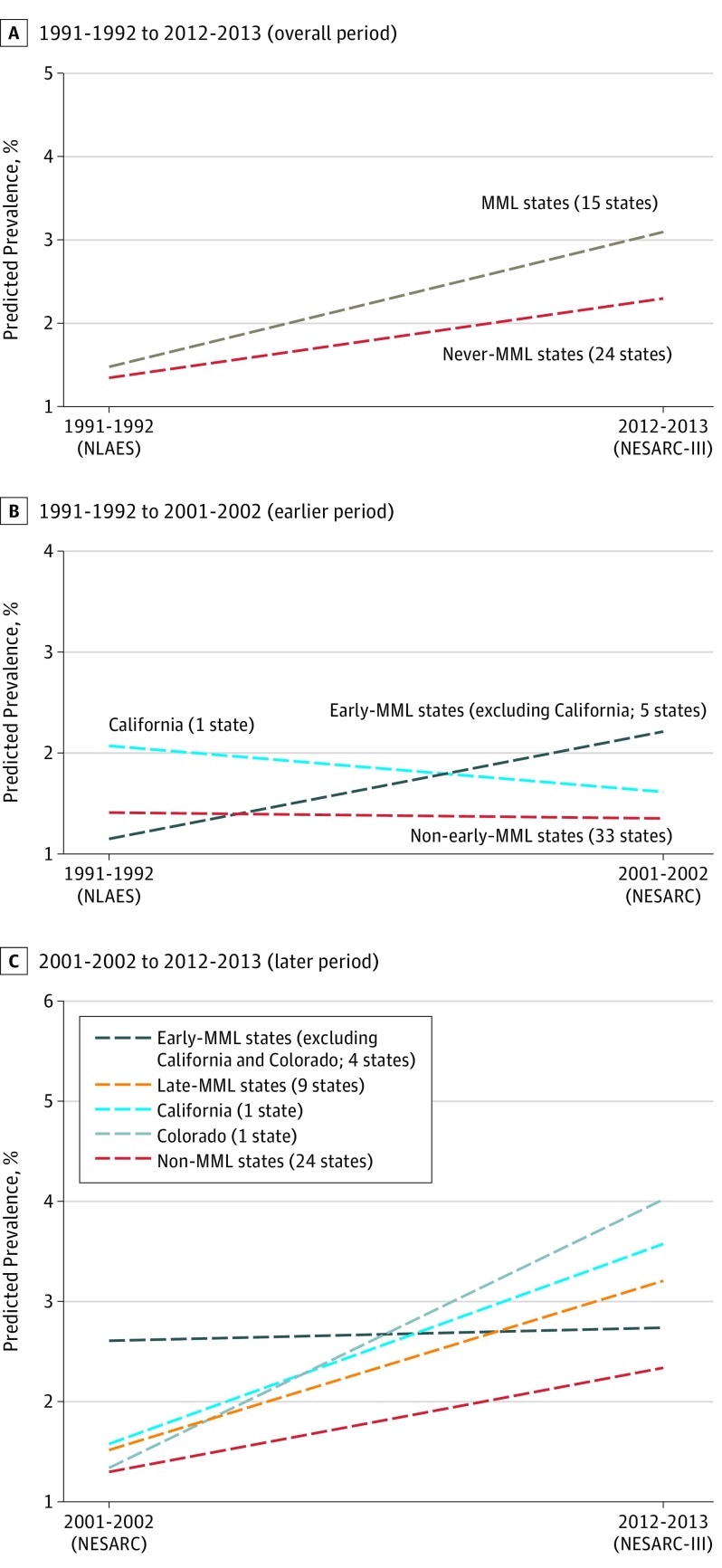
Between 1991-1992 and 2012-2013, the predicted prevalence of illicit use increased by 3.6 and 2.2 percentage points in ever-MML and never-MML states, respectively (Table 1) (Figure 1A), a significantly greater increase in ever-MML than never-MML states (P = .004). The predicted prevalence of cannabis disorder also increased (1.6 and 1.0 percentage points) in ever-MML and never-MML states (Figure 2A), also a significantly greater change in the ever-MML states (P = .03).
Figure 1. Medical Marijuana Laws (MML) and Marijuana Use in the Past 12 Months.
Prevalences predicted by logistic regression model 1 (A), model 2B (B), and model 3 (C). Models controlled for sex, age (18-29, 30-39, 40-49, and ≥50 years), education (<high school vs others), race/ethnicity (Hispanic, non-Hispanic white, non-Hispanic black, and other), marital status (unmarried vs others), urbanicity (metropolitan statistical areas vs others), and poverty (<100%, 100%-200%, and >200% of the federal poverty level). Early-MML states (1996-2001) include California, Colorado, Maine, Nevada, Oregon, and Washington. Late-MML states (2002-2012) include Arizona, Connecticut, Maryland, Massachusetts, Michigan, Montana, New Jersey, New Mexico, and Vermont. Trend lines are included for visual comparison; they do not imply that the trend was linearly changing over time. NESARC indicates the National Epidemiologic Survey on Alcohol and Related Conditions; NESARC-III, the National Epidemiologic Survey on Alcohol and Related Conditions–III; NLAES, the National Longitudinal Alcohol Epidemiologic Survey.
Figure 2. Medical Marijuana Laws (MML) and DSM-IV Cannabis Use Disorder in the Past 12 Months.
Prevalences predicted by logistic regression model 1 (A), model 2B (B), and model 3 (C). Models controlled for sex, age (18-29, 30-39, 40-49, and ≥50 years), education (<high school vs others), race/ethnicity (Hispanic, non-Hispanic white, non-Hispanic black, and other), marital status (unmarried vs others), urbanicity (metropolitan statistical areas vs others), and poverty (<100%, 100%-200%, and >200% of the federal poverty level). Early-MML states (1996-2001) include California, Colorado, Maine, Nevada, Oregon, and Washington. Late-MML states (2002-2012) include Arizona, Connecticut, Maryland, Massachusetts, Michigan, Montana, New Jersey, New Mexico, and Vermont. Trend lines are included for visual comparison; they do not imply that the trend was linearly changing over time. NESARC indicates the National Epidemiologic Survey on Alcohol and Related Conditions; NESARC-III, the National Epidemiologic Survey on Alcohol and Related Conditions–III; NLAES, the National Longitudinal Alcohol Epidemiologic Survey.
Change During the Earlier Period: 1991-1992 to 2001-2002 (Models 2A and 2B)
From 1991-1992 to 2001-2002, when grouping California with other early-MML states in model 2A, the predicted prevalence of illicit use did not change significantly in early-MML states and decreased by 1.7 percentage points in non-early–MML states, which was not a significant difference. For cannabis disorders, change in all early-MML and non-early–MML states also did not differ significantly (model 2A) (Table 2).
Table 2. Differences in Predicted Prevalences of Past-Year Cannabis Use and DSM-IV Cannabis Use Disorder, 1991-1992 to 2001-2002: Non-Early–MML States and Early-MML States (Models 2A and 2B).
| Outcome | Prevalencea (SE) | |||
|---|---|---|---|---|
| Model 2Ab | Model 2Bc | |||
| Non-Early–MML States (33 States)d | All Early-MML States (6 States)e | All Early-MML States but California (5 States) | California (1 State) | |
| Cannabis use | ||||
| 1991-1992 | 4.97 (0.44) | 6.34 (0.48) | 4.49 (0.53) | 7.59 (0.71) |
| 2001-2002 | 3.29 (0.14) | 5.24 (0.47) | 5.26 (0.71) | 5.58 (0.60) |
| Change in prevalence | −1.69 (0.42)f | −1.10 (0.59) | +0.77 (0.87) | −2.01 (0.74)g |
| DiD (early-MML states vs non-early–MML states) | [Reference] | +0.58 (0.62)h | +2.51 (0.85)i | −0.27 (0.80)j |
| Cannabis use disorder | ||||
| 1991-1992 | 1.43 (0.22) | 1.73 (0.23) | 1.15 (0.25) | 2.08 (0.33) |
| 2001-2002 | 1.36 (0.08) | 1.86 (0.28) | 2.22 (0.42) | 1.62 (0.28) |
| Change in prevalence | −0.07 (0.21) | +0.14 (0.33) | +1.07 (0.49)k | −0.46 (0.37) |
| DiD (early-MML states vs non-early–MML states) | [Reference] | +0.21 (0.35)l | +1.13 (0.47)m | −0.40 (0.40)n |
Abbreviations: DiD, difference-in-difference; MML, medical marijuana laws.
Prevalence based on participants in the 39 states included in all 3 surveys. States omitted: Alaska, Delaware, Hawaii, Idaho, Nebraska, New Hampshire, North Dakota, Rhode Island, South Dakota, West Virginia, and Wyoming. Prevalences back-transformed from marginal log-odds estimated from logistic regression interaction models (MML × survey) that included individual-level (sex, age, education, race/ethnicity, marital status, urbanicity, and poverty) and state-level (% male, % white, % <30 y, and % ≥25 y without a high school diploma) covariates. Predicted prevalences estimated by a model with a dichotomous MML variable (non-early–MML states vs early-MML states).
Predicted prevalences estimated by a model with a dichotomous MML variable (early-MML states vs non-early–MML states).
Predicted prevalences estimated by an identical model to model 2A, except California was specified as a separate group.
Non-early–MML states: Alabama, Arizona, Arkansas, Connecticut, Florida, Georgia, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, Montana, New Jersey, New Mexico, New York, North Carolina, Ohio, Oklahoma, Pennsylvania, South Carolina, Tennessee, Texas, Utah, Vermont, Virginia, and Wisconsin.
Early-MML states (1996-2001): California, Colorado, Maine, Nevada, Oregon, and Washington.
P < .001; change in non-early–MML states between 1991 and 2001.
P = .009; change in California between 1991 and 2001.
P = .35.
P = .004.
P = .74.
P = .03; change in all early-MML states but California between 1991 and 2001.
P = .55.
P = .02.
P = .33.
Separating California from the other early states produced very different results in model 2B (Table 2) (Figure 1B and Figure 2B). Note that in 1991-1992, predicted prevalences of use and disorder were higher in California than other early-MML states (use: 7.59% vs 4.49%; P = .001; disorder: 2.08% vs 1.15%; P = .02). Nevertheless, for use, decreases in California and non-early–MML states (−2.0 vs −1.7 percentage points) did not differ significantly, nor did the slight decreases in cannabis disorder.
In contrast, in the other 5 early-MML states, prevalences of use and disorder increased. The change in remaining early-MML states differed from non-MML states for use (by 2.5 percentage points; P = .004) and disorder (1.1 percentage points; P = .02).
Change During the Later Period: 2001-2002 to 2012-2013 (Model 3)
From 2001-2002 to 2012-2013, predicted prevalences of illicit cannabis use and cannabis disorder increased by the following percentage points: never-MML states, 3.5 and 1.0, respectively; California, 5.3 and 2.0; Colorado, 7.0 and 2.7; other early-MML states, 2.6 and 0.1; and late-MML states, 5.1 and 1.7. Compared with change in never-MML states, increases in use were significantly greater in late-MML states (P = .01), California (P = .04), and Colorado (P = .03) (Table 3) (Figure 1C). Comparing increases in prevalence of cannabis disorder with never-MML states (the reference group), change in late-MML states was not significant (P = .12) but was greater at a trend level in California (P = .06) and significantly greater in Colorado (P = .04) (Table 3) (Figure 2C).
Table 3. Differences in Predicted Prevalences of Past-Year Cannabis Use and DSM-IV Cannabis Use Disorder, 2001-2002 to 2012-2013: Never-MML States, Early-MML States, and Late-MML States (Model 3)a.
| Outcome | Model 3, Prevalenceb (SE) | ||||
|---|---|---|---|---|---|
| Never-MML States (24 States)c | All Early-MML States but California and Colorado (4 States)d | All Late-MML States (9 States)e | California (1 State) | Colorado (1 State) | |
| Cannabis use | |||||
| 2001-2002 | 3.12 (0.15) | 5.93 (0.81) | 3.64 (0.31) | 5.39 (0.59) | 4.10 (0.62) |
| 2012-2013 | 6.62 (0.41) | 8.55 (0.69) | 8.74 (0.74) | 10.72 (0.98) | 11.13 (1.64) |
| Change in prevalence | +3.50 (0.47)f | +2.62 (0.93)g | +5.11 (0.75)h | +5.33 (0.95)i | +7.03 (1.62)j |
| DiD (ever-MML vs never-MML states) | [Reference] | −0.87 (0.89)k | +1.61 (0.63)l | +1.83 (0.89)m | +3.53 (1.54)n |
| Cannabis use disorder | |||||
| 2001-2002 | 1.29 (0.09) | 2.61 (0.48) | 1.51 (0.20) | 1.57 (0.28) | 1.34 (0.47) |
| 2012-2013 | 2.33 (0.24) | 2.74 (0.49) | 3.21 (0.47) | 3.58 (0.55) | 4.02 (0.81) |
| Change in prevalence | +1.04 (0.28)o | +0.13 (0.61) | +1.70 (0.49)p | +2.00 (0.54)q | +2.68 (0.84)r |
| DiD (ever-MML vs never-MML states) | [Reference] | −0.91 (0.61)s | +0.65 (0.42)t | +0.96 (0.49)u | +1.64 (0.77)v |
Abbreviations: DiD, difference-in-difference; MML, medical marijuana laws.
States included were the 39 with data in all 3 surveys. States omitted: Alaska, Delaware, Hawaii, Idaho, Nebraska, New Hampshire, North Dakota, Rhode Island, South Dakota, West Virginia, and Wyoming. The predicted prevalences from the later period were estimated by a model with a trichotomous MML variable (early-MML states vs late-MML states vs never-MML states).
Predicted prevalences estimated by a model with a 5-level MML variable (early-MML states vs late-MML states vs California vs Colorado vs never-MML states). Prevalences back-transformed from marginal log-odds estimated from logistic regression interaction models (MML × survey) that included individual-level (sex, age, education, race/ethnicity, marital status, urbanicity, and poverty) and state-level (% male, % white, % <30 y, and % ≥25 y without a high school diploma) covariates.
Never-MML states (1996-2012): Alabama, Arkansas, Florida, Georgia, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Minnesota, Mississippi, Missouri, New York, North Carolina, Ohio, Oklahoma, Pennsylvania, South Carolina, Tennessee, Texas, Utah, Virginia, and Wisconsin.
Early-MML states (except California and Colorado) (1996-2001): Maine, Nevada, Oregon, and Washington.
Late-MML states (2002-2012): Arizona, Connecticut, Maryland, Massachusetts, Michigan, Montana, New Jersey, New Mexico, and Vermont.
P < .001; change in never-MML states between 2001 and 2012.
P < .001; change in all early-MML states (except California) between 2001 and 2012.
P < .001; change in all late-MML states between 2001 and 2012.
P < .001; change in California only between 2001 and 2012.
P < .001; change in Colorado only between 2001 and 2012.
P = .33.
P = .01.
P = .04.
P = .03.
P < .001; change in never-MML states between 2001 and 2012.
P = .001; change in all late-MML states between 2001 and 2012.
P < .001; change in California only between 2001 and 2012.
P = .002; change in Colorado only between 2001 and 2012.
P = .14.
P = .12.
P = .06.
P = .04.
Parallel Paths Sensitivity Analyses
The pre-MML parallel-path assumption was supported by a lack of difference during the earlier period in changes between non-MML states and late-MML states (eTable 4 in the Supplement) as well as non-MML states and Colorado (eTable 4 and eFigures 1 and 2 in the Supplement). Sensitivity analyses (eTable 5 in the Supplement) did not change results meaningfully, indicating robust main findings.
Discussion
In 3 cross-sectional national surveys spanning 20 years, we investigated whether increases in US adult illicit cannabis use and cannabis use disorders followed implementation of MML. Over the entire period, predicted prevalences of illicit use and disorders increased to a greater degree in states that passed MML than in other states. Holding population size and demographic distributions constant from 1991 to 2012, an additional 1.1 million adult illicit cannabis users and an additional 500 000 adults with a DSM-IV–diagnosed cannabis disorder may be attributable to medical marijuana law passage. Given the potential consequences of use and persistent disability associated with cannabis use disorders, this represents a serious public health problem.
During the earlier period (1991-1992 to 2001-2002), prevalences in the 5 early-MML states (excluding California) increased in contrast to decreases in non-MML states and California. In 1991-1992, the sharply higher rates of cannabis use and disorder in California than in other states (use, 69% higher; disorder, 80% higher) suggest that California, a bellwether state, differed from other states from the start, consistent with 1995 findings of higher cannabis use in California communities than elsewhere. Therefore, an already permissive environment in California may have overridden further MML effects. However, in other early-MML states, MML contributed to increased illicit use and disorder, contrary to a nationally decreasing trend.
During the later period (2001-2002 to 2012-2013), illicit use increased significantly more in late-MML states than in never-MML states. (The lack of significant differences in early-MML states could be due to absence of strong lagged effects, waning MML effects over time, or local factors.) Our inference that MML contributed to increased illicit use in late-MML states is strengthened by the lack of such differences in late-MML states during the earlier period (eTable 4 in the Supplement). Further, greater increases in cannabis use and disorder in Colorado than in never-MML states suggests that well-documented 2009-2010 policy changes and dispensary proliferation (eAppendix 1 in the Supplement) contributed to increases in use and disorder, particularly because similar increases did not occur there during the earlier period (eTable 4 and eFigures 1 and 2 in the Supplement). Substantial increases also occurred in California during the later period, consistent with qualitative observations of marijuana dispensary proliferation, although centralized California dispensary documentation is lacking. Additional research is needed on late MML and cannabis use disorder and how major policy changes and their implementation relate to public health consequences in MML states.
Increases in cannabis use associated with MML may have resulted from increasing availability, potency, perceived safety/acceptability, generally permissive attitudes (because other substance use and disorders also increased), greater use for coping with depression and anxiety (A.L.S., M.M.W., K.M.K., M.C., D.S.H.; unpublished data; 2017), or diminished economic opportunities. Future studies should investigate such mechanisms.
The previous study of pre-post MML changes in adults also found post-MML increases in cannabis use and disorder, supporting our results. However, while this study had an important advantage in that consecutive years of survey data were analyzed, only 8 years were included, changes in only 10 MML states were examined, early-MML vs late-MML effects were not addressed, and the survey did not differentiate between medical and illicit users, so medical use may have been included in its estimates. Finally, the diagnostic measure used in that study may have low sensitivity and validity. Thus, our examination of MML effects on adult illicit (ie, nonmedical) cannabis use contributes important new information.
To our knowledge, studies using DiD methods have not shown post-MML increases in adolescent cannabis use. The reasons MML differentially affect adolescents and adults merit investigation.
Since 2012, 8 states have legalized recreational cannabis use. Research is needed on the effects of these laws, which may differ from MML.
Limitations and Strengths
Study limitations are noted. Measures were self-reported. Diminished underreporting as cannabis gained acceptability could have influenced observed increases between the NESARC and NESARC-III, as could other methodological issues. However, numerous other cannabis-related consequences also increased over this period, supporting the validity of NESARC to NESARC-III comparisons. In any case, there is no reason to expect that such methodological issues would have influenced potential differences between medical marijuana states and other locations. Also, the early and later periods were defined by dates of the surveys. Exploring other definitions of early and later in suitable data could contribute useful information, eg, before and after major policy changes. The treatment of California and Colorado is termed as secondary. While these results contribute important information, further research is needed on these states relative to the national context if suitable data can be found. Ideally, all 3 surveys would have included all 50 states. However, approximately equal proportions of ever-MML and never-MML states were excluded, and analyses suggested that omitted states would not have changed the results. Additionally, we used data sets from only 3 periods, precluding formal testing of the prior parallel-path assumption for the early-MML states. However, 2 smaller surveys conducted in 1984 and 1990 suggest descriptively that early-MML states other than California did not begin their sharp increase prior to MML passage (eTable 6 and eFigure 3 in the Supplement; written personal communication, William Kerr, PhD, February 2017). Study strengths include that results contribute knowledge from more than 100 000 participants in 39 states across 2 decades. Topics for future research include whether other outcomes (eg, cannabis use frequency and other substance use) were affected by MML and whether individual or state characteristics modify MML effects.
Conclusions
This study suggests that MML contributed to increasing US adult illicit cannabis use and cannabis disorders. Policy and clinical professionals should recognize that cannabis disorders can be severe, treatment needs are increasing, and treatment can be effective. Medical marijuana laws may benefit some with medical problems. However, changing state laws (medical or recreational) may also have adverse public health consequences. A prudent interpretation of our results is that professionals and the public should be educated on risks of cannabis use and benefits of treatment, and prevention/intervention services for cannabis disorders should be provided.
eAppendix 1. Justification for testing change in Colorado as a single state relative to never-MML states in the analysis of the later period (2001-2002 to 2012-2013).
eAppendix 2. Interviewer statement preceding AUDADIS questions about drug use in NLAES, NESARC and NESARC-III.
eTable 1. Demographic characteristics of NLAES, NESARC, and NESARC-III samples, with participants in the 11 states not common to the 3 surveys excluded.
eTable 2. Years that medical marijuana laws (MML) were enacted for the 50 US states up to 2012 and how participants in these states were coded in Models 1-3.
eTable 3. Predicted US prevalence of past-year illicit cannabis use and past-year DSM-IV cannabis use disorder: overall and by medical marijuana law (MML) status.
eTable 4. Testing the parallel paths assumption for Colorado and the late-MML states: differences in predicted prevalences of past-year cannabis use and DSM-IV cannabis use disorder during the earlier period, 1991-1992 to 2001-2002.
eTable 5. Difference-in-difference (DiD) results of sensitivity analyses for models 1-3.
eTable 6. Difference in prevalences of past-year cannabis use, 1984 to 1990: data from Alcohol Research Group National Surveys 7 and 8 of adults 18 years and older, grouped as California, other early-MML states, and non-early–MML states.
eFigure 1. Medical marijuana laws (MML) and cannabis use, past 12 months, during the earlier period (1991-1992 to 2001-2002): test of “parallel paths” assumption for late states and Colorado.
eFigure 2. Medical marijuana laws (MML) and DSM-IV cannabis use disorder, past 12 months, during the earlier period (1991-1992 to 2001-2002): test of “parallel paths” assumption for late states and Colorado.
eFigure 3. Past-year cannabis use, 1984 and 1990, from the National Alcohol Surveys of adults 18 years and older conducted by the Alcohol Research Group.
References
- 1.Gallup. Majority continues to support pot legalization in US. http://www.gallup.com/poll/179195/majority-continues-support-pot-legalization.aspx. Accessed June 8, 2015.
- 2.Pacek LR, Mauro PM, Martins SS. Perceived risk of regular cannabis use in the United States from 2002 to 2012: differences by sex, age, and race/ethnicity. Drug Alcohol Depend. 2015;149:232-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hasin DS, Kerridge BT, Saha TD, et al. . Prevalence and correlates of DSM-5 cannabis use disorder, 2012-2013: findings from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Am J Psychiatry. 2016;173(6):588-599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fergusson DM, Boden JM, Horwood LJ. Psychosocial sequelae of cannabis use and implications for policy: findings from the Christchurch Health and Development Study. Soc Psychiatry Psychiatr Epidemiol. 2015;50(9):1317-1326. [DOI] [PubMed] [Google Scholar]
- 5.Lev-Ran S, Imtiaz S, Taylor BJ, Shield KD, Rehm J, Le Foll B. Gender differences in health-related quality of life among cannabis users: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2012;123(1-3):190-200. [DOI] [PubMed] [Google Scholar]
- 6.Compton WM, Gfroerer J, Conway KP, Finger MS. Unemployment and substance outcomes in the United States 2002-2010. Drug Alcohol Depend. 2014;142:350-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kalousova L, Burgard SA. Unemployment, measured and perceived decline of economic resources: contrasting three measures of recessionary hardships and their implications for adopting negative health behaviors. Soc Sci Med. 2014;106:28-34. [DOI] [PubMed] [Google Scholar]
- 8.Lenné MG, Dietze PM, Triggs TJ, Walmsley S, Murphy B, Redman JR. The effects of cannabis and alcohol on simulated arterial driving: influences of driving experience and task demand. Accid Anal Prev. 2010;42(3):859-866. [DOI] [PubMed] [Google Scholar]
- 9.Hartman RL, Huestis MA. Cannabis effects on driving skills. Clin Chem. 2013;59(3):478-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brady JE, Li G. Trends in alcohol and other drugs detected in fatally injured drivers in the United States, 1999-2010. Am J Epidemiol. 2014;179(6):692-699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramaekers JG, Berghaus G, van Laar M, Drummer OH. Dose related risk of motor vehicle crashes after cannabis use. Drug Alcohol Depend. 2004;73(2):109-119. [DOI] [PubMed] [Google Scholar]
- 12.Zhu H, Wu LT. Trends and correlates of cannabis-involved emergency department visits: 2004 to 2011. J Addict Med. 2016;10(6):429-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis GP, Compton MT, Wang S, Levin FR, Blanco C. Association between cannabis use, psychosis, and schizotypal personality disorder: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Schizophr Res. 2013;151(1-3):197-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Di Forti M, Marconi A, Carra E, et al. . Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: a case-control study. Lancet Psychiatry. 2015;2(3):233-238. [DOI] [PubMed] [Google Scholar]
- 15.Danielsson AK, Lundin A, Allebeck P, Agardh E. Cannabis use and psychological distress: an 8-year prospective population-based study among Swedish men and women. Addict Behav. 2016;59:18-23. [DOI] [PubMed] [Google Scholar]
- 16.Blanco C, Hasin DS, Wall MM, et al. . Cannabis use and risk of psychiatric disorders: prospective evidence from a US national longitudinal study. JAMA Psychiatry. 2016;73(4):388-395. [DOI] [PubMed] [Google Scholar]
- 17.Bonn-Miller MO, Harris AH, Trafton JA. Prevalence of cannabis use disorder diagnoses among veterans in 2002, 2008, and 2009. Psychol Serv. 2012;9(4):404-416. [DOI] [PubMed] [Google Scholar]
- 18.Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219-2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gubatan J, Staller K, Barshop K, Kuo B. Cannabis abuse is increasing and associated with increased emergency department utilization in gastroenterology patients. Dig Dis Sci. 2016;61(7):1844-1852. [DOI] [PubMed] [Google Scholar]
- 20.Hasin DS, Saha TD, Kerridge BT, et al. . Prevalence of marijuana use disorders in the United States between 2001-2002 and 2012-2013. JAMA Psychiatry. 2015;72(12):1235-1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carliner H, Mauro PM, Brown QL, et al. . The widening gender gap in marijuana use prevalence in the US during a period of economic change, 2002-2014. Drug Alcohol Depend. 2017;170:51-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Substance Abuse and Mental Health Services Administration Drug Abuse Warning Network, 2011: National Estimates of Drug-Related Emergency Department Visits. HHS Publication No. (SMA) 13-4760. DAWN Series D-39. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 23.Compton WM, Han B, Jones CM, Blanco C, Hughes A. Marijuana use and use disorders in adults in the USA, 2002-14: analysis of annual cross-sectional surveys. Lancet Psychiatry. 2016;3(10):954-964. [DOI] [PubMed] [Google Scholar]
- 24.Charilaou P, Agnihotri K, Garcia P, Badheka A, Frenia D, Yegneswaran B. Trends of cannabis use disorder in the inpatient: 2002 to 2011 [published online February 2, 2017]. Am J Med. [DOI] [PubMed] [Google Scholar]
- 25.McKay MP, Groff L. 23 years of toxicology testing fatally injured pilots: implications for aviation and other modes of transportation. Accid Anal Prev. 2016;90:108-117. [DOI] [PubMed] [Google Scholar]
- 26.Vin-Raviv N, Akinyemiju T, Meng Q, Sakhuja S, Hayward R. Marijuana use and inpatient outcomes among hospitalized patients: analysis of the nationwide inpatient sample database. Cancer Med. 2017;6(1):320-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cerdá M, Wall M, Keyes KM, Galea S, Hasin D. Medical marijuana laws in 50 states: investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug Alcohol Depend. 2012;120(1-3):22-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wen H, Hockenberry JM, Cummings JR. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. J Health Econ. 2015;42:64-80. [DOI] [PubMed] [Google Scholar]
- 29.Khatapoush S, Hallfors D. “Sending the wrong message”: did medical marijuana legalization in California change attitudes about and use of marijuana? J Drug Issues. 2004;34(4):751-770. doi: 10.1177/002204260403400402 [DOI] [Google Scholar]
- 30.Schuermeyer J, Salomonsen-Sautel S, Price RK, et al. . Temporal trends in marijuana attitudes, availability and use in Colorado compared to non-medical marijuana states: 2003-11. Drug Alcohol Depend. 2014;140:145-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Davis JM, Mendelson B, Berkes JJ, Suleta K, Corsi KF, Booth RE. Public health effects of medical marijuana legalization in Colorado. Am J Prev Med. 2016;50(3):373-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maxwell JC, Mendelson B. What do we know now about the impact of the laws related to marijuana? J Addict Med. 2016;10(1):3-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fairman BJ. Trends in registered medical marijuana participation across 13 US states and District of Columbia. Drug Alcohol Depend. 2016;159:72-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Salomonsen-Sautel S, Min SJ, Sakai JT, Thurstone C, Hopfer C. Trends in fatal motor vehicle crashes before and after marijuana commercialization in Colorado. Drug Alcohol Depend. 2014;140:137-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sznitman SR, Zolotov Y. Cannabis for therapeutic purposes and public health and safety: a systematic and critical review. Int J Drug Policy. 2015;26(1):20-29. [DOI] [PubMed] [Google Scholar]
- 36.Grant BF, Harford TC, Dawson DA, Chou SP, Dufour M, Pickering RP. Prevalence of DSM-IV alcohol abuse and dependence: United States, 1992. Alcohol Health Res World. 1992;18(3):243-248. [PMC free article] [PubMed] [Google Scholar]
- 37.Hasin DS, Grant BF. Major depression in 6050 former drinkers: association with past alcohol dependence. Arch Gen Psychiatry. 2002;59(9):794-800. [DOI] [PubMed] [Google Scholar]
- 38.Grant BF, Stinson FS, Dawson DA, et al. . Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(8):807-816. [DOI] [PubMed] [Google Scholar]
- 39.Grant BF, Moore TC, Kaplan K. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- 40.Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(4):361-368. [DOI] [PubMed] [Google Scholar]
- 41.Grant BF, Chu A, Sigman R, et al. . Source and Accuracy Statement: National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2014. [Google Scholar]
- 42.Grant BF, Goldstein RB, Saha TD, et al. . Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72(8):757-766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.US Census Bureau Intercensal estimates of the resident population for the United States, regions, states, and Puerto Rico: April 1, 2000 to July 1, 2010. https://www.census.gov/data/tables/time-series/demo/popest/intercensal-2000-2010-state.html. Accessed March 21, 2017.
- 44.US Census Bureau Annual estimates of the resident population: April 1, 2010 to July 1, 2012 December 2012. https://www.census.gov/data/tables/2015/demo/popest/state-total.html. Accessed March 21, 2017.
- 45.Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991-1992 and 2001-2002. JAMA. 2004;291(17):2114-2121. [DOI] [PubMed] [Google Scholar]
- 46.Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991-1992 and 2001-2002. Drug Alcohol Depend. 2004;74(3):223-234. [DOI] [PubMed] [Google Scholar]
- 47.Martins SS, Keyes KM, Storr CL, Zhu H, Grucza RA. Birth-cohort trends in lifetime and past-year prescription opioid-use disorder resulting from nonmedical use: results from two national surveys. J Stud Alcohol Drugs. 2010;71(4):480-487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hasin DS, O’Brien CP, Auriacombe M, et al. . DSM-5 criteria for substance use disorders: recommendations and rationale. Am J Psychiatry. 2013;170(8):834-851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Canino G, Bravo M, Ramírez R, et al. . The Spanish Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability and concordance with clinical diagnoses in a Hispanic population. J Stud Alcohol. 1999;60(6):790-799. [DOI] [PubMed] [Google Scholar]
- 50.Chatterji S, Saunders JB, Vrasti R, Grant BF, Hasin D, Mager D. Reliability of the alcohol and drug modules of the Alcohol Use Disorder and Associated Disabilities Interview Schedule–Alcohol/Drug-Revised (AUDADIS-ADR): an international comparison. Drug Alcohol Depend. 1997;47(3):171-185. [DOI] [PubMed] [Google Scholar]
- 51.Cottler LB, Grant BF, Blaine J, et al. . Concordance of DSM-IV alcohol and drug use disorder criteria and diagnoses as measured by AUDADIS-ADR, CIDI and SCAN. Drug Alcohol Depend. 1997;47(3):195-205. [DOI] [PubMed] [Google Scholar]
- 52.Grant BF. DSM-IV, DSM-III-R, and ICD-10 alcohol and drug abuse/harmful use and dependence, United States, 1992: a nosological comparison. Alcohol Clin Exp Res. 1996;20(8):1481-1488. [DOI] [PubMed] [Google Scholar]
- 53.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71(1):7-16. [DOI] [PubMed] [Google Scholar]
- 54.Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39(1):37-44. [DOI] [PubMed] [Google Scholar]
- 55.Pull CB, Saunders JB, Mavreas V, et al. . Concordance between ICD-10 alcohol and drug use disorder criteria and diagnoses as measured by the AUDADIS-ADR, CIDI and SCAN: results of a cross-national study. Drug Alcohol Depend. 1997;47(3):207-216. [DOI] [PubMed] [Google Scholar]
- 56.Ustün B, Compton W, Mager D, et al. . WHO Study on the reliability and validity of the alcohol and drug use disorder instruments: overview of methods and results. Drug Alcohol Depend. 1997;47(3):161-169. [DOI] [PubMed] [Google Scholar]
- 57.Vrasti R, Grant BF, Chatterji S, et al. . Reliability of the Romanian version of the alcohol module of the WHO alcohol use disorder and associated disabilities: interview schedule–alcohol/drug-revised. Eur Addict Res. 1998;4(4):144-149. [DOI] [PubMed] [Google Scholar]
- 58.Pacula RL, Hunt P, Boustead A. Words can be deceiving: a review of variation among legally effective medical marijuana laws in the United States. J Drug Policy Anal. 2014;7(1):1-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hasin DS, Wall M, Keyes KM, et al. . Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross-sectional surveys. Lancet Psychiatry. 2015;2(7):601-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thompson RG Jr, Alonzo D, Hu MC, Hasin DS. Substance use disorders and poverty as prospective predictors of adult first-time suicide ideation or attempt in the United States. Community Ment Health J. 2017;53(3):324-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cerdá M, Wall M, Feng T, et al. . Association of state recreational marijuana laws with adolescent marijuana use. JAMA Pediatr. 2017;171(2):142-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Keyes KM, Wall M, Cerdá M, et al. . How does state marijuana policy affect US youth? medical marijuana laws, marijuana use and perceived harmfulness: 1991-2014. Addiction. 2016;111(12):2187-2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Imbens GW, Wooldridge JM. Recent developments in the econometrics of program evaluation. J Econ Lit. 2009;47(1):5-86. doi: 10.3386/w14251 [DOI] [Google Scholar]
- 64.Angrist JD, Pischke JS. Mostly Harmless Econometrics: An Empiricist’s Companion. Vol 1 Princeton, NJ: Princeton University Press; 2009. [Google Scholar]
- 65.Angrist J, Krueger AB. Empirical strategies in labor economics In: Ashenfelter O, Card D, eds. Handbook of Labor Economics. Vol 3A Amsterdam, the Netherlands: Elsevier; 1999:1277-1366. [Google Scholar]
- 66.Hunt PE, Miles J. The impact of legalizing and regulating weed: issues with study design and emerging findings in the USA [published online December 31, 2015]. Curr Top Behav Neurosci. [DOI] [PubMed] [Google Scholar]
- 67.Research Triangle Institute SUDAAN Language Manual, Release 11.0. Research Triangle Park, NC: Research Triangle Institute; 2012. [Google Scholar]
- 68.Rubio JM, Olfson M, Villegas L, Pérez-Fuentes G, Wang S, Blanco C. Quality of life following remission of mental disorders: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2013;74(5):e445-e450. [DOI] [PubMed] [Google Scholar]
- 69.Freisthler B, Kepple NJ, Sims R, Martin SE. Evaluating medical marijuana dispensary policies: spatial methods for the study of environmentally-based interventions. Am J Community Psychol. 2013;51(1-2):278-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pacula RL, Powell D, Heaton P, Sevigny EL. Assessing the effects of medical marijuana laws on marijuana use: the devil is in the details. J Policy Anal Manage. 2015;34(1):7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.ElSohly MA, Mehmedic Z, Foster S, Gon C, Chandra S, Church JC. Changes in cannabis potency over the last 2 decades (1995–2014): analysis of current data in the United States. Biol Psychiatry. 2016;79(7):613-619. doi: 10.1016/j.biopsych.2016.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Saha TD, Kerridge BT, Goldstein RB, et al. . Nonmedical prescription opioid use and DSM-5 nonmedical prescription opioid use disorder in the United States. J Clin Psychiatry. 2016;77(6):772-780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Martins SS, Sarvet A, Santaella-Tenorio J, Saha T, Grant BF, Hasin DS. Changes in US lifetime heroin use and heroin use disorder: prevalence from the 2001-2002 to 2012-2013 National Epidemiologic Survey on Alcohol and Related Conditions [published online March 29, 2017]. JAMA Psychiatry. doi: 10.1001/jamapsychiatry.2017.0113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jordan BK, Karg RS, Batts KR, Epstein JF, Wiesen C. A clinical validation of the National Survey on Drug Use and Health assessment of substance use disorders. Addict Behav. 2008;33(6):782-798. [DOI] [PubMed] [Google Scholar]
- 75.Hasin DS, Grant B. NESARC findings on increased prevalence of marijuana use disorders—consistent with other sources of information. JAMA Psychiatry. 2016;73(5):532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lynne-Landsman SD, Livingston MD, Wagenaar AC. Effects of state medical marijuana laws on adolescent marijuana use. Am J Public Health. 2013;103(8):1500-1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Choo EK, Benz M, Zaller N, Warren O, Rising KL, McConnell KJ. The impact of state medical marijuana legislation on adolescent marijuana use. J Adolesc Health. 2014;55(2):160-166. [DOI] [PubMed] [Google Scholar]
- 78.Anderson DM, Hansen B, Rees DI. Medical marijuana laws and teen marijuana use. Am Law Econ Rev. 2015;17(2):495-528. doi: 10.3386/w20332 [DOI] [Google Scholar]
- 79.Grucza RA, Agrawal A, Bierut LJ. NESARC findings on increased prevalence of marijuana use disorders—reply: consistent with other sources of information. JAMA Psychiatry. 2016;73(5):532-533. [DOI] [PubMed] [Google Scholar]
- 80.Grucza RA, Agrawal A, Krauss MJ, Cavazos-Rehg PA, Bierut LJ. Recent trends in the prevalence of marijuana use and associated disorders in the United States. JAMA Psychiatry. 2016;73(3):300-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Polcin DL, Korcha R, Greenfield TK, Bond J, Kerr W. Twenty-one-year trends and correlates of pressure to change drinking. Alcohol Clin Exp Res. 2012;36(4):705-715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Compton WM, Baler R. The epidemiology of DSM-5 cannabis use disorders among US adults: science to inform clinicians working in a shifting social landscape. Am J Psychiatry. 2016;173(6):551-553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry. 2008;165(2):179-187. [DOI] [PubMed] [Google Scholar]
- 84.Danovitch I, Gorelick DA. State of the art treatments for cannabis dependence. Psychiatr Clin North Am. 2012;35(2):309-326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Marshall K, Gowing L, Ali R, Le Foll B. Pharmacotherapies for cannabis dependence. Cochrane Database Syst Rev. 2014;12(12):CD008940. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Justification for testing change in Colorado as a single state relative to never-MML states in the analysis of the later period (2001-2002 to 2012-2013).
eAppendix 2. Interviewer statement preceding AUDADIS questions about drug use in NLAES, NESARC and NESARC-III.
eTable 1. Demographic characteristics of NLAES, NESARC, and NESARC-III samples, with participants in the 11 states not common to the 3 surveys excluded.
eTable 2. Years that medical marijuana laws (MML) were enacted for the 50 US states up to 2012 and how participants in these states were coded in Models 1-3.
eTable 3. Predicted US prevalence of past-year illicit cannabis use and past-year DSM-IV cannabis use disorder: overall and by medical marijuana law (MML) status.
eTable 4. Testing the parallel paths assumption for Colorado and the late-MML states: differences in predicted prevalences of past-year cannabis use and DSM-IV cannabis use disorder during the earlier period, 1991-1992 to 2001-2002.
eTable 5. Difference-in-difference (DiD) results of sensitivity analyses for models 1-3.
eTable 6. Difference in prevalences of past-year cannabis use, 1984 to 1990: data from Alcohol Research Group National Surveys 7 and 8 of adults 18 years and older, grouped as California, other early-MML states, and non-early–MML states.
eFigure 1. Medical marijuana laws (MML) and cannabis use, past 12 months, during the earlier period (1991-1992 to 2001-2002): test of “parallel paths” assumption for late states and Colorado.
eFigure 2. Medical marijuana laws (MML) and DSM-IV cannabis use disorder, past 12 months, during the earlier period (1991-1992 to 2001-2002): test of “parallel paths” assumption for late states and Colorado.
eFigure 3. Past-year cannabis use, 1984 and 1990, from the National Alcohol Surveys of adults 18 years and older conducted by the Alcohol Research Group.