Abstract
Objective
Studies suggest that American Muslim women underutilize mammography. While religion has a strong influence upon Muslim health behaviors scant research has examined how religion-related beliefs inform Muslim women’s intention for mammography. Our study identifies and examines such beliefs.
Methods
Muslim women aged 40 and older sampled from mosques participated in focus groups and individual interviews. Drawing upon the Theory of Planned Behavior, interviews elicited salient behavioral, normative, and control beliefs regarding mammography and the influence of Islam upon screening intention.
Results
Fifty women participated in 6 focus groups and 19 in semi-structured interviews, with near-equal numbers of African American, South Asian, and Arab Muslims. Forty-two percent of participants had not had a mammogram within the past two years. Across differences in race/ethnicity and mammography status women voiced four religion-related salient beliefs that inform mammography intention: (1) the perceived duty to care for one’s health, (2) religious practices as methods of disease prevention, (3) fatalistic notions about health, and (4) comfort with gender concordant healthcare.
Conclusions
Religious beliefs influence decisions to pursue mammography across the ethnic/racial diversity of Muslim women. Notions about duty to God and the stewardship of one’s body appear to enhance mammography intention. Theocentric notions of cure and illness and varied views regarding personal agency also inform decisional frames that impact mammography intention. Given the salience of religion among our participants, religiously-tailored messages in interventions have the potential to enhance cancer screening.
Keywords: Islam, Breast Cancer Screening, Fatalism, Theory of Planned Behavior, Oncology, Cancer
Introduction
Regular screening mammography is an effective tool for breast cancer control as increased mammography utilization has contributed to the recent decline in cancer mortality [1–3]. Yet, despite these gains, a disproportionate burden of breast cancer mortality and low mammography rates persist among minorities [4, 5], including American Muslims [6–8].
American Muslims, number around 7 million persons [9–11] and comprise predominately of African Americans, Arabs, and South Asians [11, 12]. While nearly two-thirds are immigrants [13], 87% are English-literate [14]. Although the lack of religious affiliation captured in US census data and national health surveys precludes national estimates for Muslim mammography rates, community surveys report underutilization. Illustratively, a biennial mammography rate of 52% was reported in a study of 207 Muslim women recruited through Chicago community organizations [7], and our Muslim organization-based survey of 240 women in Chicago found that 37% of the sample had not had a mammogram within the past two years [15]. Similarly, a California-based survey of 226 Muslim women found 54% to have received a mammogram in the past two years [6]. The lower rates of mammography among American Muslims coupled with data that suggests that some Muslim ethnic groups present with breast cancer at a younger age, with more advanced disease, and with worse morphological features [8, 16–18], underscores the need for delineating and intervening upon barriers to mammography in this community.
Although knowledge-based and access-related barriers to mammography have been studied among Muslim women [19–22], the influence of religion-related beliefs upon cancer screening practices is not well understood. Several studies suggest that modesty concerns pose barriers to mammography uptake [19, 21–23], yet others suggest that religious beliefs such as the notion of stewardship of the body might promote cancer screening [21]. While informative, these small qualitative studies largely study Muslim women from a single ethnic group, and most often study immigrants, thereby challenging both the ability to separate religious influences from those of race/ethnicity and to describe experiences related to immigrant status separately from those related to religious identity. Consequently, we sought to identify, within a diverse Muslim sample, salient behavioral, normative, and control beliefs impacting mammography intention and among these beliefs closely examine those related to Islam.
Methods
Theoretical framework
The Theory of Planned Behavior (TPB) [24] provided conceptual frames for interview questions, data codebooks, and qualitative content analyses. TPB asserts that the most proximate and strongest predictor of behavior is intention. Behavioral intention is informed by: (1) one’s overall attitude toward the action, including his or her outcome expectations; (2) one’s belief that most of the people important to him or her believe that he or she should or should not perform the action (subjective norm) and beliefs about those norms; and (3) one’s perceived control regarding performance of the action [25]. This project sets Islam-related factors within the TPB framework as global beliefs and values that influence mammography intention through more specific behavioral, normative and control beliefs.
Study setting, design, and project team
Set in Greater Chicago, home to over 300,000 Muslims [26] with large numbers of Arab, South Asian and African members [9, 27] the study utilized a community-engaged approach and was approved by the University of Chicago Institutional Review Board. A Community Advisory Board (CAB) comprised of individuals who represent the Council of Islamic Organizations of Greater Chicago (CIOGC, a federation of over 60 mosques, Muslim community centers, and social service organizations), and two CIOGC member social service organizations: the Arab American Family Services, and the Muslim Women Resources Center, provided feedback on study objectives and design, facilitated data collection, and participated in dissemination activities. The academic team consisted of a physician-researcher with expertise in mixed-methods health disparities research and Islamic bioethics, a behavioral scientist, and clinician-researchers with expertise in culturally-tailored interventions.
Participant sampling and recruitment
Focus Group Interviews
We recruited self-identified Muslim, English-speaking women over the age of 40 from nine mosques between August 2013 and January 2014. Sites were purposively selected to achieve near-equal representation of Arabs, South Asians, and African Americans and recruitment primarily took place in-person via recruitment tables at events at mosques.
Semi-Structured Interviews
Between November 2014 and April 2015, women from the already recruited potential participant pool who did not participate in focus groups were offered the option of participating in interviews. Furthermore, using the same criteria for focus group participants, several additional women were recruited from the mosque sites so as to generate a diverse interviewee pool.
Data collection
Focus groups were held at the mosques, lasted 1.5–2 hours, were conducted in English, and moderated by a trained female research assistant. Semi-structured interviews lasted 45–90 minutes, were conducted in English by trained female research assistants and all but one interview was conducted via telephone.
Drawing upon TPB constructs, focus group questions captured mammography experiences and beliefs, with probes eliciting behavioral, normative, and control beliefs regarding mammography. Follow-up questions sought to clarify religious and communal aspects of these beliefs. Two additional domains of inquiry- cancer beliefs and preventive health practices—were also elicited through separate questions. The semi-structured interview guide added probes and questions to the focus group guide in order to discuss beliefs emerging from the focus groups in greater depth. Interview guides were initially reviewed by the investigative team to reduce redundancy and enhance clarity, and during data collection problematic questions were iteratively revised based on participant responses. Participant socio-demographic characteristics, mammography status,, and religiosity was obtained prior to focus groups, and at the conclusion of semi-structured interviews.
Data analysis
Interviews were audio-recorded and transcribed verbatim. Two research assistants created an initial codebook using TPB domains and emergent Islamic beliefs and values as tree nodes. Implementing a team-based and framework approach to qualitative coding and data analysis [28], four research assistants coded one focus group and coding disagreements were resolved through team-based discussion. Emergent themes were then added to the initial codebook as branch nodes of the TPB-based domains yielding a final codebook. Inter-rater reliability was measured by Cohen’s kappa coefficient (κ) and recoding was performed until the κ > 0.8 for each code. Thereafter, research assistants coded the remaining transcripts independently. During team meetings, interview summaries were reviewed by code, and codes were grouped into higher-order conceptual themes based on team consensus. NViVo 10 software was used to facilitate data analysis [29]. A particular belief was termed salient if it was discussed during three or more focus groups, and a theme was categorized as dominant when it was discussed by half or more participants in a focus group. A belief was defined as religion-related if participants mentioned that it was informed by God, religious texts, or religious teachings.
Results
Of the 122 individuals recruited, 77 confirmed availability to attend focus group sessions, but 50 participants eventually participated in 6 focus groups. Nineteen women participated in individual interviews. In total there was nearly equal numbers of Arab (19), South Asian (25) and African American (20) participants. Twenty-nine participants (42%) did not have a mammogram within the past 2 years. [See Tables 1 and 2]
Table 1.
| Characteristic
|
Focus Group (N=50) |
Individual Interviews (N=19) |
|---|---|---|
| No. (%)
|
No. (%)
|
|
| I. Socio-demographic Information | ||
|
| ||
| Racial/Ethnic Background | N = 50 | N= 18 |
| African American/Black | 16(32.0) | 3 (16.7) |
| South Asian | 16(32.0) | 9 (50.0) |
| Arab/Arab American | 14(28.0) | 6 (33.3) |
|
| ||
| Age | N=50 | N=18 |
| 40–49 | 21(42.0) | 11 (61.1) |
| 50–74 | 28(56.0) | 7 (38.9) |
| Mean (range) | 51 (range: 40–75) | 45 (range: 41–67) |
|
| ||
| Marital Status | N=46 | N=19 |
| Married | 38(82.6) | 17 (89.5) |
|
| ||
| Highest Level of Education | N=45 | N=19 |
| High school/GED or Less | 8(17.8) | 4 (21.1) |
| Associates | 11(24.4) | 3 (15.8) |
| Bachelors | 18(40.0) | 7 (36.8) |
| Advanced degree (Masters or higher) | 8(17.8) | 5 (26.3) |
|
| ||
| Immigrant Status | N=50 | |
| Immigrated as Adult | 28(56.0) | |
| Born in the US | 15(30.0) | |
| Immigrated as Child | 7(14.0) | |
| Duration in the United States | N=19 | |
| Less than 15 years | 3 (15.8) | |
| 16–20 years | 3 (15.8) | |
| More than 20 years | 13 (68.4) | |
|
| ||
| Annual Household Income | N=44 | |
| Less than $50,000 | 18 (41.0) | |
| $50,001 – $100,000 | 14 (31.8) | |
| Over $100,001 | 7 (15.9) | |
| Annual Household Income | N=16 | |
| Less than $60,000 | 7(43.8) | |
| $60,000 – $90,000 | 6(37.5) | |
| Over $90,001 | 3 (18.8) | |
|
| ||
| II. Health Services Utilization | ||
|
| ||
| Have Primary Care Physician |
N=50 47(94.0) |
N=19 19 (100) |
|
| ||
| Have Had a Clinical Breast Exam | N=5042(84.0) |
N=19 18 (94.7) |
|
| ||
| Have Had a Mammogram Ever | N=50 | N=19 |
| 37(74.0) | 14 (73.7) | |
| Mammogram within the Last 2 years | 28(56.0) | 12 (63.2) |
|
| ||
| III. Religiosity | ||
|
| ||
| Islamic Affiliation | N=50 | N=19 |
|
| ||
| Sunni | 37(74.0) | 15 (78.9) |
| Rating of Religiosity (on 1–10 scale) | N=43 | N=18 |
| 5 (Somewhat Religious) | 6(14.0) | 2 (11.1) |
| 6 | 4(9.3) | 2 (11.1) |
| 7 | 4(9.3) | 7 (38.9) |
| 8 | 15(34.9) | 3 (16.7) |
| 9 | 5(11.6) | 1 (5.6) |
| 10 (Very Religious) | 8(18.6) | 3 (16.7) |
|
| ||
| Wear Hijab | N=46 | N=19 |
| Yes | 36(78.3) | 18 (94.7) |
Table 2.
Self-reported Ethnicity By Focus Group Location
| Focus Group | Number of Participants | Self-reported Ethnicity | |||
|---|---|---|---|---|---|
| African-American/Black | South Asian | Arab/Arab-American | Other | ||
| Islamic Foundation | 8 | 6 | 2 | ||
| Masjid Al-Ihsan | 7 | 7 | |||
| Orland Park Prayer Center | 8 | 8 | |||
| Mosque Foundation | 8 | 6 | 2 | ||
| Muslim Education Center | 10 | 10 | |||
| Nigerian Islamic Association | 9 | 9 | |||
Eighteen themes were classified as salient and 13 as dominant [see Figure 1 and Table 2–online supplement]. Four beliefs were religion-related: (1) the perceived duty to care for one’s health, (2) methods of disease prevention, (3) fatalistic notions about health, and (4) the comfort with gender concordant healthcare. [See Figure 1 and Table 3-online supplement]
Figure 1.
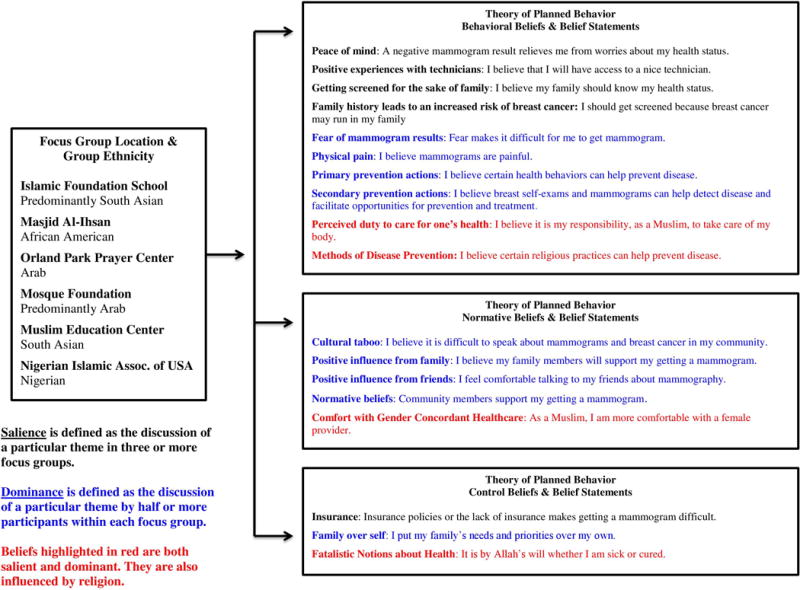
Qualitive Analysis Illustration
Perceived duty to care for one’s health
During discussions about preventative health and about mammography participants reported a religious duty to care for their body. A focus group participant noted “Allah says you have to take care of yourself,” and an interviewee explained “God gave us the responsibility of taking care of the body that He gave us.” Participants explained that they must demonstrate care for their body before they can expect God’s help as a focus group participant shared “God will not help you until you help yourself. So in order for God to do His work, you should do your work first.”
In explaining the duty towards bodily stewardship women utilized two interrelated concepts – the idea of the body as a loan from God and as a trust from God. As a focus group participant related “we should really be taking care of ourselves and our body because that’s – it’s a loan from Allah…we have to return it too.” An interviewee expounded “we are responsible for our bodies and if we don't take proper care of it, if we neglect it, if we abuse it, if we do things to harm it, then we will be accountable on the Day of Judgment.”
Participants also explained the obligation to care for their body through the idea that health is a trust from God. To describe this trust women referenced the concept of amana, an Islamic ethical concept sourced within many different Quranic verses (23:8, 4:58) and Prophetic narrations. As one focus group participant explained “it’s [in] the hadith (Prophetic statements) telling us to take care of ourselves.” Another focus group participant detailed, “Allah does not tell you not to take care of yourself. You know something we call amana which is… if someone gives you like a gift or something you take care of it. You don’t… just say, okay, I’m sitting here.” Another focus group participant succinctly stated “health is an amana.”
This belief that one is religiously obligated to care for the body appeared to motivate preventive health actions, including mammography. One interviewee explained “our religion always calls for awareness, taking care of yourself…you do [mammograms] for your body for you, for something good.”
Methods of disease prevention
Participants offered examples of behaviors to prevent illness and maintain health such as diet control, exercise, taking medication, as well as visiting the doctor to obtain referrals for or undergo screening tests, including mammography. In addition religious practices, such as prayer and fasting, were believed to be health promoting, illness preventing and even curative. “I pray regularly even if I go to the doctor, asking for good health – that’s one, number one in the list [of prevention actions]” stated one focus group participant. An interviewee discussed how the five obligatory daily prayers assist with health, “I feel it cleans my heart and it is a very good exercise.”
Another individual interviewee noted that before getting her mammogram, she turned to prayer as a means of prevention and comfort “I was just praying for myself that, please God, keep me healthy.” A focus group participant shared her belief that it was prayer that changed her fate, “[the] tests just came back negative, because I prayed on it.”
Fatalistic notions about health
A complex and variable picture of personal agency in the context of God’s decree resulting in disease and cure was shared by participants. At one end there was almost no perceived personal agency in light of God’s decree and individuals declined from pursuing preventative health activities such as mammography. Most participants spoke about this tendency among the community in a disapproving fashion. One focus group participant relayed, “[Other Muslims] put all their faith in God and feel that they don’t have to do anything,” and an individual interviewee shared that she debates with people who say “I don’t go [for screening tests]…it’s just with Allah whatever happens, happens. We are all going to die someday” by saying “we are all going to die, I agree…but the quality of life until you die, how is it going to be?” Other participants reflected that God’s control over disease impacted their own mammography decisions, as an interviewee said “God is not going to give you something that’s not written. So me not taking [mammograms] it is not going to prevent anything from happening because if it’s meant, then it’s meant to be.” An interviewee explained the reason why she did not get a mammogram saying “Allah will[s] what is destined will be…If I don’t have any reason to dig into anything, I’ll continue to pray for good health…if that’s [cancer] is His will then it will be.”
With respect to prayer influencing God’s decree regarding illness some participants noted that prayer was a legitimate means to access cure from God and others explained that prayer could forestall illness. Yet, in contrast the view that “[prayer] doesn't prevent you from getting sick because if God wants to get you sick, you're going to get sick” was also mentioned.
Seeking to balance notions of God’s decree and personal responsibility to obtain healthcare one interviewee shared “everything is in the hands of God…however we don’t know what His plans are and therefore we follow His rule which says to seek treatment.” Another interviewee explained that while “everything is preordained by God but He doesn’t choose for you. You choose for yourself but He just knows what you are going to choose,” and another interviewee expounded that one’s choices determine illness “it’s not because God from the beginning wanted you to get it, it might be your lifestyle.” Another interviewee shared that her decision to get a mammogram was also part of providential design explaining “it was Allah that steered me to have the test on whatever particular day and time in my life and in him I put my trust for whatever the outcome or the result will be…whatever Allah has decreed for you, he has decreed for you.” These sorts of understanding of God’s decree left room for personal agency and appeared to facilitate mammography screening.
In summary, many ideas emerged from the participants relating God’s decree, personal agency and healthcare decisions. For some participants mammography was unnecessary in light of God’s decree, others noted that one could petition God (through prayer) such that cancer was not fated for that person, others felt motivated to obtain screening based on their understanding of duty to God, while some participants voiced multiple perspectives at the same time.
Comfort with gender concordant healthcare
Many women discussed their preference for female healthcare providers including doctors and mammography technicians. A focus group participant said, “Well, if somebody is going to do a breast exam on me I’d really prefer a female…” Another focus group participant noted that gender concordance informs all her healthcare seeking actions, including mammography saying “If I went in there and I found out it was going to be male physician, I’ll probably just walk right back out or I’ll stay there until they find me somebody who’s going to be a [lady].”
The preference for gender concordant care resulted from ideas of physical and social comfort as well as adhering to religious notions of modesty. One focus group participant stated, “If I had a male doctor, I couldn’t talk to him. If he’s a gynecologist and he asks me certain questions, I’m not comfortable talking about it. Probably if it was a female, I would open up and tell everything.” An interviewee shared “yes, because I’m Muslim. They have to be female.” Indeed, modesty is a significant Islamic ethic impacting behavior, dress, speech, and one’s interaction with God that is sourced within many Quranic verses (e.g. 24:30–31) and Prophetic statements [33]. Importantly the loss of modesty was mentioned as a risk or harm related to clinical breast exams.
Discussion
Our study into the salient behavioral, normative and control mammography-related beliefs of Muslim women provides critical insight into religious beliefs that influence their cancer screening behaviors. Through focus groups and interviews, and across differences in race/ethnicity and mammography status, participants described (1) a perceived duty to care for one’s body, and by extension one’s health, because the body represents an entrusted loan from God enhanced women’s intention for mammography, the beliefs that (2) religious practices are a credible means of preventing illness and (3) that God’s decree results in illness and cure, both variably influenced mammography intention as participants shared multiple perspectives regarding the utility of petitioning God to remain disease-free and the usefulness of cancer screening, and (4) comfort with gender concordant healthcare providers due to modesty norms influenced decisions to obtain mammograms. These themes extend findings from previous studies and have significant implications for interventions seeking to increase mammography rates among Muslims.
Our work builds upon the scant literature describing religious influences upon mammography utilization among American Muslims. Shirazi and colleagues studied the breast cancer knowledge of 53 non-English speaking, Muslim Afghan immigrants and report that women viewed “their body as a gift ‘they should take care of’” and that viewed “themselves responsible for…seeking medical care and treatment” in light of this trust [21]. While Shirazi and colleagues’ sample held that God’s decree determined illness and cure they did not voice “religious fatalism regarding health” whereby preventive health measures were seen as unnecessary [21]. Al-Amoudi and colleagues interview of 14 Somali Muslim women echoes Shirazi et. al’s findings [19]. Our study corroborates these notions of body stewardship and God’s decree as salient and dominant, and extends these findings to English-speaking Muslim women from diverse backgrounds. Yet, unlike these studies, some of our participants rationalized their disinclination to seek mammograms on the basis of religious fatalism [30]. On the other hand, our prior surveys in this same community found no association between measures of religious health fatalism and cancer screening rates [15, 31]. Hence our data suggests that Muslim views on God’s decree and personal agency do not fully map onto operative definitions of religious fatalism commonly used in the health literature, and that more nuanced measures are needed to assess Islamic notions of fatalism. Nonetheless, since God-centric views of health and illness and bodily stewardship were linked to positive intention for mammography, interventions that frame preventive health measures within theologically-appropriate religious frameworks may be effective.
Similar to qualitative studies of Somali [19], Asian [23], Afghani [21] and other Muslims’ [22] attitudes towards breast cancer screening our study finds gender concordance and modesty preservation to be highly valued. These beliefs are normative in that they emerge from religious teachings that emphasize the maintaining modesty and detail norms of dress and cross-gender interaction [32] but may also influence control beliefs where women forgo mammograms if they cannot assure same-sex providers. Community-based interventions should highlight that many mammography centers are staffed by women in order to allay modesty concerns and overcome a perceived barrier for some Muslims. At the same time, programs that that sensitize healthcare providers to the critical role modesty and gender concordance play upon Muslim healthcare-seeking patterns, and enhance cross-cultural communication skills can also promote higher quality healthcare experiences and dispel communal narratives of religious discrimination. A two-pronged approach may particularly be important in Chicago since we previously found perceived religious discrimination in healthcare to be negatively associated with Muslim mammography rates [15].
Our participants did not voice several themes found by other researchers. Rajaram and colleagues reported that patriarchal beliefs about familial decision-making negatively impacted cancer screening among Asian Muslim women [23], while Shirazi reported similar views in their Afghan sample [21]. Within focus group discussions none of our participants reported an inability to obtain a mammogram because male relatives controlled decision-making, and even after probes were inserted into the semi-structured interview guides asking women to comment on such notions, interviewees rejected this view. We hypothesize that participants within our study might not have experienced similar controlling influences over cancer screening in part because of acculturation. In other words, as individuals of both genders acculturate to the individualistic nature of American society, patriarchal notions that possibly inform healthcare seeking decisions might wane and women no longer perceive a lack of control over their own cancer screening decisions. Indeed our participants on average had lived in the United States longer than the participants in the two aforementioned studies. It is also possible that such controlling influences are not the norm, as larger studies of Arab women living in Qatar and the UAE find that only a very small minority report male relatives objecting to breast cancer screening. [33–34]
While our findings are strengthened by a mosque-community based approach to recruitment, sampling from multiple segments of the Muslim community, involvement of a community-advisory board, and a team-based approach to qualitative content analysis, our methodology may limit generalizability. The recruitment strategy introduces selection bias towards Muslims for whom religious influences upon health behaviors are more prominent. Similarly, restricting participants to those who are English-proficient biases our sample against non-English speaking populations. However, since nearly 50% of American Muslims (inclusive of men and women) attend mosque once a week [14], and 87% of American Muslims (inclusive of men and women) are English-literate [14], we believe that our work legitimately represents the voices of a large cross-section of American Muslim women. Our interview guides did not elicit personal immigration histories nor delved into political circumstances informing health choices, further research is needed to assess the relative weight of these and other beliefs and factors that impact cancer screening among Muslims.
Given the salience of religion among our diverse Muslim participants, and that previous studies have also noted similar religious influences to inform screening practices among different racial/ethnic subgroups of Muslims, incorporating religiously-tailored messages in cancer screening interventions has the potential for broad impact. As described above complex theocentric notions of illness were juxtaposed with varied views on personal agency as related to cancer prevention, and discussions about duty to God and stewardship of one’s body dovetailed into conversations about the utility of religious practices for prevention. These ideas must be engaged with in order to enhance cancer screening in this community. Successfully addressing these beliefs requires partnering with Islamic scholars and Imams in a two-way dialogue where behavioral interventionalists come to understand Islamic doctrine and ethics while religious leaders gain literacy in the theory and practice of health behavior change. Other faith communities have successfully initiated such cooperative intervention programs [35]. Muslim groups should adapt these models utilize our research upon Muslim women’s cancer screening behaviors and the role of Imams in community health as foundational to such efforts [15, 31, 36].
Supplementary Material
Acknowledgments
A Mentored Research Scholar Grant(MRSG-14-032-01-CPPB) to AIP, in addition to an Institutional Research Grant (#58-004) from the American Cancer Society (ACS) provided project funds and supported the time-effort of AIP, HM, FM, SM and MV. A National Cancer Institute Cancer Center Support Grant (#P30 CA14599) provided additional project funds. We acknowledge the critical assistance of community partners: Mohammad Kaiseruddin from the Council of Islamic Organizations of Greater Chicago, Itedal Shelabi from Arab American Family Services, Sima Qureshi from Muslim Women’s Resource Center, Sahira Rahman from Islamic Foundation School, Imam Madyun and Tahira Madyun from Masjid Al-Ihsan, Ali Tai and Tayyaba Ahmad from Muslim Education Center, Aisheh Said from Mosque Foundation, Ghada Rafati from Orland Park Prayer Center, Rukiyat Lawal and Shaffdeen A. Amuwo from the Nigerian Islamic Association. We also thank our research interns Caitlin Ajax, Alia Azmat, Tasmiha Khan, Hinasahar Muneerudin for their work.
References
- 1.American Cancer Society. American Cancer Society Guidelines for the Early Detection of Cancer [Internet] 2014 Available from: http://www.cancer.org/healthy/findcancerearly/cancerscreeningguidelines/american-cancer-society-guidelines-for-the-early-detection-of-cancer [Accessed January 12, 2016]
- 2.Nelson HD, Tyne K, Naik A, Bougatsos C, Chan BK, Humphrey L. Screening for breast cancer: An update for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2009 doi: 10.1059/0003-4819-151-10-200911170-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pace LE, Keating NL. A systematic assessment of benefits and risks to guide breast cancer screening decisions. JAMA [Internet] 2014;311(13):1327–35. doi: 10.1001/jama.2014.1398. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2469160810.1001/jama.2014.1398. [DOI] [PubMed] [Google Scholar]
- 4.Peek ME, Han JH. Disparities in screening mammography: Current status, interventions, and implications. Journal of General Internal Medicine. 2004 doi: 10.1111/j.1525-1497.2004.30254.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller JW, King JB, Joseph DA, Richardson LC. Breast cancer screening among adult women–Behavioral Risk Factor Surveillance System, United States, 2010. MMWR Morb Mortal Wkly Rep [Internet] 2012;61(Suppl):46–50. pii. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=22695463su6102a8. [PubMed] [Google Scholar]
- 6.Shaheen MA, Galal OM, Salahi L, Aman Y. Utilization of mammography among Muslim women in Southern California [abstract] [Internet] 2005 Available from: https://apha.confex.com/apha/133am/techprogram/paper_106236.htm.
- 7.Hasnain M, Menon U, Ferrans CE, Szalacha L. Breast Cancer Screening Practices Among First-Generation Immigrant Muslim Women. J Women’s Heal [Internet] 2014;23(7):602–12. doi: 10.1089/jwh.2013.4569. Available from: http://online.liebertpub.com/doi/abs/10.1089/jwh.2013.456910.1089/jwh.2013.4569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hensley Alford S, Schwartz K, Soliman A, Johnson CC, Gruber SB, Merajver SD. Breast cancer characteristics at diagnosis and survival among Arab-American women compared to European- and African-American women. Breast Cancer Res Treat. 2009;114(2):339–46. doi: 10.1007/s10549-008-9999-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ba-Yunus I. East-West Review. Chicago: Muslims of Illinois: A Demographic Report; p. 1997. [Google Scholar]
- 10.Smith TW. The Muslim Population of the United States: The Methodology of Estimates. Public Opin Q [Internet] 2002;66(3):404–17. Available from: http://www.jstor.org/stable/307876910.1086/341669. [Google Scholar]
- 11.Muslim American Demographic Facts [Internet] [cited 2009 Jul 10]. Available from: http://www.allied-media.com/AM/
- 12.Gallup, Inc. Muslim Americans: A National Portrait - An In-depth Analysis of America’s Most Diverse Religious Community. Washington D.C: 2009. Available from: http://www.themosqueinmorgantown.com/pdfs/GallupAmericanMuslimReport.pdf. [Google Scholar]
- 13.Pew Research Center. Muslim Americans: Middle Class and Mostly Mainstream. Washington, DC: 2007. Available from: http://www.pewresearch.org/files/old-assets/pdf/muslim-americans.pdf. [Google Scholar]
- 14.Pew Research Center. Muslim Americans: No Signs of Growth in Alienation or Support for Extremism. Washington D.C: 2011. Available from: http://www.people-press.org/files/legacy-pdf/Muslim%20American%20Report%2010-02-12%20fix.pdf. [Google Scholar]
- 15.Padela AI, Murrar S, Adviento B, Liao C, Hosseinian Z, Peek M, et al. Associations Between Religion-Related Factors and Breast Cancer Screening Among American Muslims. Journal of Immigrant and Minority Health. 2014 doi: 10.1007/s10903-014-0014-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kakarala M, Rozek L, Cote M, Liyanage S, Brenner DE. Breast cancer histology and receptor status characterization in Asian Indian and Pakistani women in the U.S.–a SEER analysis. BMC Cancer. 2010 doi: 10.1186/1471-2407-10-191. 10:191.10.1186/1471-2407-10-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nasseri K, Moulton LH. Patterns of death in the first and second generation immigrants from selected middle eastern countries in California. J Immigr Minor Heal. 2011;13(2):361–70. doi: 10.1007/s10903-009-9270-7. [DOI] [PubMed] [Google Scholar]
- 18.Moran MS, Gonsalves L, Goss DM, Ma S. Breast cancers in U.S. residing Indian-Pakistani versus non-Hispanic White women: Comparative analysis of clinical-pathologic features, treatment, and survival. Breast Cancer Res Treat. 2011;128(2):543–51. doi: 10.1007/s10549-011-1362-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al-Amoudi S, Cañas J, Hohl SD, Distelhorst SR, Thompson B. Breaking the Silence: Breast Cancer Knowledge and Beliefs Among Somali Muslim Women in Seattle. Washington: Health Care Women Int; 2013. pp. 37–41. Internet. April 2014. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2435106210.1080/07399332.2013.857323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salman KF. Health Beliefs and Practices Related to Cancer Screening Among Arab Muslim Women in an Urban Community. Health Care for Women International. 2012 doi: 10.1080/07399332.2011.610536. [DOI] [PubMed] [Google Scholar]
- 21.Shirazi M, Bloom J, Shirazi A, Popal R. Afghan immigrant women’s knowledge and behaviors around breast cancer screening. Psycho-Oncology. 2013 doi: 10.1002/pon.3216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Underwood SM, Shaikha L, Bakr D. Veiled yet vulnerable: Breast cancer screening and the Muslim way of life. Cancer Pract. 1999;7(6):285–90. doi: 10.1046/j.1523-5394.1999.76004.x. [DOI] [PubMed] [Google Scholar]
- 23.Rajaram SS, Rashidi A. Asian-Islamic women and breast cancer screening: a socio-cultural analysis. Women Health. 1999;28(3):45–58. doi: 10.1300/J013v28n03_04. [DOI] [PubMed] [Google Scholar]
- 24.Ajzen I. Behavioral Interventions: Design and Evaluation Guided by the Theory of Planned Behavior. In: Mark MM, Donaldson SI, Campbell B, editors. Social Psychology and Evaluation. 2011. pp. 74–101. [Google Scholar]
- 25.Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991 doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 26.Chicago Muslims: Deep Roots, Many Branches IIP Digital. 2014 Available from: http://iipdigital.usembassy.gov/st/english/publication/2013/11/20131104285728.html#axzz3atiKpc7e. [Date of access: January 12, 2016]
- 27.Logan JR. America’s Newcomers. 2003 [Internet]. Available from: http://mumford.albany.edu/census/NewComersReport/NewComer01.htm [Date of access: January 12, 2016[
- 28.MacQueen KM, McLellan E, Kay K, Milstein B. Codebook Development for Team-Based Qualitative Analysis. Field Methods. 1998 doi: 10.1177/1525822X980100020301. [DOI] [Google Scholar]
- 29.Ltd QIP. NVivo Qualitative Data Analysis Software. 2012 [Google Scholar]
- 30.Franklin MD, Schlundt DG, Wallston KA. Development and validation of a religious health fatalism measure for the African-American faith community. J Health Psychol. 2008;13(3):323–35. doi: 10.1177/1359105307088137. [DOI] [PubMed] [Google Scholar]
- 31.Padela AI, Peek ME, Johnson-Agbakwu CE, Hosseinian Z, Curlin F. Associations between religion-related factors and cervical cancer screening among Muslims in greater chicago. J Low Genit Tract Dis. 2014;18(4):326–32. doi: 10.1097/LGT.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Padela AI, Rodríguez del Pozo P. Muslim patients and cross-gender interactions in medicine: an Islamic bioethical perspective. J Med Ethics. 2011;37(1):40–4. doi: 10.1136/jme.2010.037614. [DOI] [PubMed] [Google Scholar]
- 33.Bener A, El Ayoubi HR, Moore MA, Basha B, Joseph S, Chouchane L. Do we need to maximise the breast cancer screening awareness? Experience with an endogamous society with high fertility. Asian Pac J Cancer Prev. 2009 Oct-Dec;10(4):599–604. [PubMed] [Google Scholar]
- 34.Bener A, Alwash R, Miller CJ, Denic S, Dunn EV. Knowledge, attitudes, and practices related to breast cancer screening: a survey of Arabic women. J Cancer Educ. 2001 Winter;16(4):215–20. doi: 10.1080/08858190109528776. [DOI] [PubMed] [Google Scholar]
- 35.Erwin DO, Spatz TS, Turturro CL. Development of an African-American role model intervention to increase breast self-examination and mammography. J Cancer Educ. 1992;7(4):311–9. doi: 10.1080/08858199209528188. [DOI] [PubMed] [Google Scholar]
- 36.Padela AI, Killawi A, Heisler M, Demonner S, Fetters MD. The role of imams in American Muslim health: perspectives of Muslim community leaders in Southeast Michigan. Journal of religion and health. 2011;50(2):359–73. doi: 10.1007/s10943-010-9428-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


