Graphical abstract
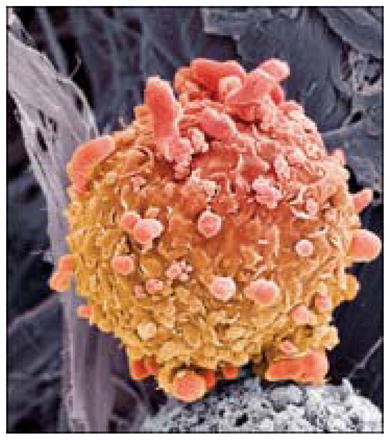
Steve Gschmeissner/Science Photo Library
Metastatic melanoma is driven by activation of the mitogen-activated protein kinase (MAPK) pathway in most patients. Mutations in BRAF, present in approximately 40–50% of patients’ tumors, are the most common activators of the MAPK pathway. NRAS, an upstream effector of RAF, MEK, and MAPK signaling, is the second most common molecular aberration, affecting approximately 20% of patients 1. In NRAS-driven cells, downstream inhibition of MEK should prevent ERK activation and lead to cell death. Indeed, in vitro studies show that most, but not all, NRAS-mutated melanoma cell lines are sensitive to MEK inhibition2.
Dummer and colleagues report the results of the NRAS melanoma and MEK inhibitor (NEMO) study which was the first randomized, phase 3 study for patients with NRAS mutant melanoma. Binimetinib, a MEK inhibitor, was associated with an improved progression free survival compared to dacarbazine (HR=0.62) although there was little apparent difference by 6 months and no detectable effect on overall survival. Binimetinib was also associated with a higher objective response rate (15.2%) compared to dacarbazine (6.8%). This response rate was consistent with the 20% response rate seen in a prior phase II trial in NRAS mutant melanoma of binimetinib 3.
While this study demonstrates the superiority of binimetinib over dacarbazine in NRAS mutant melanoma, the magnitude of the benefit was small providing fertile ground for future investigations. There are several possible reasons why most patients did not respond and why among those who did the median duration of response was limited at 6.9 months. One possibility is that MEK may not have been adequately blocked by binimetinib. The level of MEK inhibition was not measured and this dose and schedule was not well-tolerated; approximately 61% of patients required dose reduction and 20% of patients discontinued binimetinib due to drug-related toxicity. These rates of dose reduction may be higher than what could be expected in clinical practice since most dose modifications were due to asymptomatic events detected by frequent protocol mandated evaluations. Another potential barrier is that even if MEK is effectively inhibited, loss of negative feedback mechanisms will partially restore MAPK signaling4. Based on preclinical data, it has been proposed that an intermittent dosing schedule, rather than continuous daily dosing, might be a strategy to address the loss of negative feedback 5, 6. Thirdly, it is possible that non-responding tumors had additional molecular alterations such that MEK inhibition was insufficient for an antitumor effect 7.
On the other hand, four patients had a complete response to binimetinib. These patients appear to be extremely sensitive to MEK inhibition and require further study to understand the basis of this MEK dependence.
Although the response rate of binimetinib was statistically significantly higher than dacarbazine, this should be interpreted with caution as there was a high proportion of patients in both the dacarbazine arm (31%) and the binimetinib arm (15%) who were not assessable for response mostly either because they refused treatment assignment or did not have a valid post-treatment assessment. These patients were counted appropriately as non-responders but response rates may have been underestimated.
Binimetinib was associated with expected adverse drug events of MEK inhibitors. Due to the known ocular toxicities of MEK inhibitors, patients underwent ophthalmologic examinations every 3 weeks. Despite the frequency of reported ocular events, visual impairment only occurred in approximately 15% of patients and was usually reversible; no patients developed permanent blindness. The authors question, correctly in our opinion, the need for regularly scheduled ophthalmologic examinations in asymptomatic patients receiving MEK inhibitors. Other known side effects of MEK inhibitors are elevations in creatine phosphokinase (CPK) levels and decreased cardiac ejection fraction. CPK levels were elevated in 42% of patients and decreased ejection fraction was seen in 11% of patients. Both findings were of uncertain clinical consequence as it remains unclear whether this extensive monitoring and consequent dose modifications in asymptomatic patients are required. Despite the reported rates of decreased ejection fraction, the rate of symptomatic congestive heart failure remains unknown.
Overall, the NEMO study should be viewed as a success for the melanoma field which was able to conduct the first randomized trial in patients molecularly selected for NRAS mutations, an underserved patient population in need of novel therapeutics. After initial immunotherapy, MEK inhibition may ultimately have a role in treating NRAS-mutated melanoma. However, combining MEK inhibitors with other molecular inhibitors and immunotherapy will likely be necessary to firmly establish MEK inhibition in the treatment of NRAS mutant melanoma. Additional efforts to improve MEK inhibition through alternative dosing strategies and additional molecular studies to define patient populations most likely to benefit are needed.
References
- 1.Cancer Genome Atlas N. Genomic Classification of Cutaneous Melanoma. Cell. 2015;161(7):1681–96. doi: 10.1016/j.cell.2015.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joseph EW, Pratilas CA, Poulikakos PI, et al. The RAF inhibitor PLX4032 inhibits ERK signaling and tumor cell proliferation in a V600E BRAF-selective manner. Proc Natl Acad Sci U S A. 2010;107(33):14903–8. doi: 10.1073/pnas.1008990107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ascierto PA, Schadendorf D, Berking C, et al. MEK162 for patients with advanced melanoma harbouring NRAS or Val600 BRAF mutations: a non-randomised, open-label phase 2 study. The Lancet Oncology. 2013;14(3):249–56. doi: 10.1016/S1470-2045(13)70024-X. [DOI] [PubMed] [Google Scholar]
- 4.Dougherty MK, Muller J, Ritt DA, et al. Regulation of Raf-1 by direct feedback phosphorylation. Mol Cell. 2005;17(2):215–24. doi: 10.1016/j.molcel.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 5.Tate SC, Burke TF, Hartman D, Kulanthaivel P, Beckmann RP, Cronier DM. Optimising the combination dosing strategy of abemaciclib and vemurafenib in BRAF-mutated melanoma xenograft tumours. Br J Cancer. 2016;114(6):669–79. doi: 10.1038/bjc.2016.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Das Thakur M, Salangsang F, Landman AS, et al. Modelling vemurafenib resistance in melanoma reveals a strategy to forestall drug resistance. Nature. 2013;494(7436):251–5. doi: 10.1038/nature11814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kwong LN, Costello JC, Liu H, et al. Oncogenic NRAS signaling differentially regulates survival and proliferation in melanoma. Nat Med. 2012;18(10):1503–10. doi: 10.1038/nm.2941. [DOI] [PMC free article] [PubMed] [Google Scholar]


