Abstract
Background
Internet use is pervasive in many cultures. Little is known about the impact of Obsessive-Compulsive Personality Disorder (OCPD) symptoms on impulsive and compulsive psychopathologies in people who use the Internet.
Method
1323 adult Internet users completed an online questionnaire quantifying OCPD symptoms, likely occurrence of select mental disorders (OCD, ADHD, problematic Internet use, anxiety), and personality questionnaires of impulsivity (Barratt) and compulsivity (Padua). Predictors of presence of OCPD symptoms (endorsement of at least 4 of 8 DSM criteria) were identified using binary logistic regression.
Results
In regression (p<0.001, AUC 0.77), OCPD symptoms were significantly associated with (in order of decreasing effect size): lower non-planning impulsivity, higher ADHD symptoms, problematic Internet use, avoidant personality disorder, female gender, generalized anxiety disorder, and some types of compulsions (checking, dressing/washing).
Conclusions
These data suggest that OCPD symptoms, defined in terms of at least 4 of 8 DSM tick-list criteria being met, are common in Internet users. OCPD symptoms were associated with considerably higher levels of psychopathology relating to both impulsive (ADHD) and compulsive (OC-related and problematic Internet use) disorders. These data merit replication and extension using gold-standard in-person clinical assessments, as the current study relied on self-report over the Internet.
Keywords: anankastic, OCPD, compulsive, rigid, internet
Introduction
Despite constituting a relatively new technology, access to the Internet is now all-pervasive in many parts of the world. For example, around 90% of young adults use the Internet in Europe and the United States. The impact of Internet use on people with certain personality disorders has received very limited research attention. Individuals with obsessive-compulsive personality disorder (OCPD), also referred to as anankastic personality disorder, often have a rigid or ‘inflexible’ approach towards life, endorsing at least four of eight symptoms (Table 1) (1). Such a rigid cognitive style could theoretically pre-dispose towards habitual patterns of behavior, such as repetitive use of the Internet, which may in turn lead to problematic Internet use. OCPD was first recognized over 100 years ago (2), and has been included in the Diagnostic and Statistical Manual (DSM) since its inception and in each subsequent revision, including the latest, i.e. DSM-5 (3).
Table 1. Summary of individual OCPD symptoms, adapted from DSM-5 (1).
By current DSM-5 criteria, endorsement of four or more aspects is necessary for a diagnosis.
| • | Being preoccupied with rules or organization, to the point that the main aim of a given activity is lost |
| • | Being over-devoted to work or productivity |
| • | Inflexible approach to morality and ethics |
| • | Perfectionism that interferes with task completion |
| • | Difficulties throwing away worn out or worthless items with no sentimental value |
| • | Reluctance to delegate work to other people |
| • | Miserly spending towards self and/or others |
| • | Being rigid or stubborn |
Some evidence suggests that OCPD constitutes the most common personality disorder in the general population (4), with a lifetime prevalence of up to 7.9%, based on data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) (5, 6) [but see lower rates of 1.7-2.0% elsewhere (7, 8)]. In patients recruited from clinical sites, OCPD was associated with milder functional impairment than other personality disorders; but almost 90% reported being markedly impaired in at least one domain, suggesting that the disorder merits clinical and public health attention (9). The NESARC data also demonstrated that individuals with OCPD have higher rates of most psychiatric disorders compared to the general population, although the NESARC failed to screen for OCD (6). Surprisingly, in view of the arguably high prevalence rate and related problems, there has been relatively scant research into OCPD’s associations with comorbid mental disorders and other clinical features (3).
Two concepts that are of particular relevance when considering OCPD, in terms of its diagnostic classification and relationship with other disorders, are compulsivity and impulsivity. Compulsivity entails repetitive, habitual actions (or mental acts), which continue despite the original goal of the task being lost, and/or despite untoward longer term consequences (10, 11). Impulsivity, on the other hand, refers to behaviors that are risky, hasty, unduly thought out, or premature, which result in untoward longer term outcomes (12, 13). Compulsivity and impulsivity can be considered at the level of overt symptoms/behavior, or at the level of neurocognitive functioning. While OCPD is currently listed as a personality disorder, it may bear parallels with the ‘archetypal’ ‘compulsive’ disorder, namely obsessive-compulsive disorder (OCD), which is now listed in DSM-5 as an Obsessive-Compulsive and Related Disorder (1).
The relationship between OCPD and OCD has been the subject of considerable debate (14). OCD is characterized by obsessions (recurrent, intrusive thoughts) and/or compulsions (repetitive, unwanted behaviors), often revolving around key themes such as harm and uncertainty (14). It was traditionally thought that OCPD might lead to, or be causally implicated, in OCD (15). From the perspective of top-level symptoms, individuals with OCPD and those with OCD may show rigidity in terms of tendencies to get stuck within a particular behavioral routine (14). Co-occurrence of OCPD and OCD has been reported to be in the order 23-45%, using more recent DSM conceptualizations. In a sample of 238 treatment-seeking individuals with OCD, for example, 27% met criteria for comorbid OCPD (16). Another study, in 148 adults with OCD, found OCPD in 47.3% of the sample, which was associated with more prominent OCD symptoms (except for contamination and checking), and more distress (17). In 403 people with OCD, comorbid OCPD occurred in 34% of the cases (18). In a large cohort of participants in the Collaborative Longitudinal Personality Disorders Study, there was a significant association between OCPD and OCD (odds ratios of around 3), and relationships between OCPD and anxiety/mood disorders were not so strong (19). One review however found, based on OCD clinical samples, that the majority of individuals with OCD (75%) do not have OCPD. Similarly, results from personality disorder samples suggest that the majority of individuals with OCPD (80%) do not have OCD (20). Nevertheless, although not all studies agree on the high comorbidity rates, OCPD also appears to be more common in relatives of people with OCD than in control relatives, hinting at a familial and possibly genetic overlap with regards etiology (21).
If the traditional suggestion that impulsivity and compulsivity represent polar opposites of a continuum (reflecting risk-seeking and risk-avoidance, respectively) is correct (22), one might expect people with OCPD to show low rates of impulsivity: their day-to-day symptoms suggest a rigid response style and wishing for things to be ‘perfect’ and ‘controlled’, rather than risky and hasty. The issue of impulsivity in OCPD has had limited scrutiny. In an early study, comprising a mix of individuals who were self-referred due to aggression problems (n=29), or who had been clinically-referred due to aggression problems (n=89), OCPD was evident in 24% of the sample, but antisocial personality was considerably higher at 52% (23). The authors argued for a compensatory theory for the development of OCPD, at least in some cases. Specifically, it was hypothesized that some individuals with disinhibition may adopt a structured personality style (OCPD, or features thereof), in order to sustain functioning in academic and social spheres. A similar argument could be suggested for ADHD: that people with ADHD could develop OCPD traits to maintain order in their lives. The issue of comorbid overlap between OCPD and ADHD symptoms has barely been studied as a specific topic. ADHD in adults shows high comorbidity with a range of personality disorders, including OCPD (24). While this may suggest an impulsive element to OCPD (in terms of higher than expected risk of comorbid ADHD) this could stem partly from diagnostic overlap or confusion. For example, an individual with OCPD could endorse being inattentive or hyperactive (e.g. feeling like they are “driven by a motor”), but as a consequence of a desire to achieve perfection or as a means of trying to maintain control. Similarly, reluctance to delegate or submit to others’ way of doing something could drive a type of behavior that appears “impulsive”.
Data elsewhere suggest lower rather than higher rates of impulsivity in OCPD, at least in terms of trait questionnaire and cognitive measures. In a study of 110 patients with OCD, patients with comorbid OCPD (20.9% of the sample) had lower non-planning impulsivity than non-comorbid cases, as indexed by the Barratt Impulsiveness Questionnaire (25). In other study, OCPD (n=25 patients) was associated with increased capacity to delay reward (i.e. less reward discounting impulsivity) compared to healthy controls (n=25), and patients with OCD (n=25) (26). Here, reward discounting was assessed using a questionnaire; OCPD patients with and without OCD did not differ significantly on this measure, suggesting that this measure of diminished impulsivity was associated with OCPD per se (26). In a small sample, OCD patients with and without OCPD had similar impulsivity on a neurocognitive task (Stop-signal task), but comorbid cases had significantly worse inflexibility on a set-shifting task, indicative of being less impulsive, or more compulsive (14).
Some discrepancies in the (admittedly scant) existing research exploring aspects of impulsivity and compulsivity in OCPD could stem from limited sample sizes, focusing on people recruited from clinical settings, and/or not accounting for the confounding influence between different variables. Psychopathological associations between Internet use and OCPD symptoms have barely been studied. Therefore, the aim of the current study was to explore OCPD symptoms and their relationship with impulsive and compulsive measures, in a large sample of Internet users, who completed an online survey. On the basis of the existing literature, we hypothesized that OCPD symptom would be associated with elevated obsessive-compulsive symptoms, and lower impulsivity as indexed by a personality questionnaire.
Methods
Participants and method of data collection
This was a multi-site study, with data collected in Chicago (USA) and Stellenbosch (South Africa) 2014-2015, using SurveyMonkey software. Advertisements were used to recruit people – these adverts asked people if they used the Internet, and if so, to consider doing the online questionnaire. The research study was approved by an Institutional Review Board at each site, and individuals provided consent prior to participation. On completion of the survey, participants were able to enroll in a prize draw, with prizes valued between $50 and $200 in the USA and between ZAR250 and ZAR750 in South Africa.
Contents of online survey
The online survey contained questions about each individual’s age, gender, race, and educational levels. OCPD symptom status was quantified using the eight-item tick list covering the DSM-5 criteria (Figure 1); endorsement of four or more items was necessary for confirmation of significant OCPD symptoms. Occurrence of the following mental disorders was also recorded using questions adapted from the Mini International Neuropsychiatric Interview (MINI) (27): OCD, generalized anxiety disorder, and panic disorder. The MINI was designed as a brief structured interview for the major Axis I psychiatric disorders in the DSM-IV and ICD-10. Avoidant personality disorder was measured using questions adapted from DSM-5 criteria. Internet Addiction symptoms were measured using Young’s Internet Addiction Test (IAT) (28). The IAT is comprised of 20 questions examining levels of problematic Internet use, and has good psychometric properties (Cronbach’s alpha ~ 0.9) (28). ADHD symptoms were assessed using the World Health Organization Adult ADHD Rating Scale (ASRS v1.1) Part A (29, 30); this instrument asks about difficulties finalizing projects, organizing things, remembering appointments/obligations, avoiding getting started on a task, squirming/fidgeting, and feeling overly active and compelled to do things. The ASRS Part A yields a total symptom score of range 0-24, and has fair to good psychometric properties (Cronbach’s alpha ~ 0.7) (30). In addition, we evaluated obsessive-compulsive symptoms using the Padua Inventory (PI) (31), and impulsive personality traits with the Barratt Impulsiveness Questionnaire (BIS, version 11) (32, 33). The Padua Inventory consists of 39 items describing common obsessional and compulsive behavior and allows investigation of the topography of such problems in normative and clinical contexts. The Padua Inventory yields sub-scores for five different domains of obsessive-compulsive type symptoms, and has good psychometric properties (Cronbach’s alpha ~ 0.9) (31). The BIS is a self-report questionnaire used to determine levels of impulsiveness in domains of attentional impulsivity, motor impulsivity, and non-planning impulsivity. Again, it has good psychometric properties (Cronbach’s alpha ~ 0.80) (32, 33).
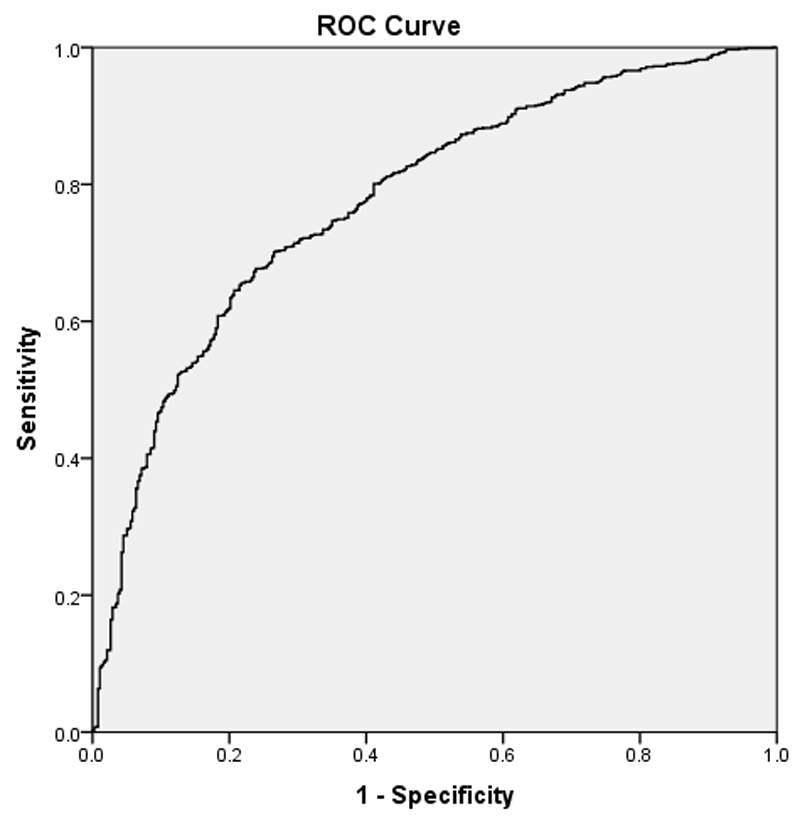
Figure 1. ROC Curve for binary regression model for identification of OCPD in the sample based on demographic and clinical variables listed in Table 3.
Our rationale for focusing on these disorders and symptoms specifically was that we believed they would be implicated in the occurrence of OCPD, balanced against the need to screen for a finite number of disorders to limit the length of the online questionnaire.
Data analysis
Only data from participants who completed the entirety of the online survey were included in the analyses. Occurrence of mental disorders and scores on personality measures were compared between individuals with and without OCPD symptoms using one-way analysis of variance (ANOVA) or suitable alternative non-parametric tests as indicated, with significance defined as p<0.05, two-tailed, Bonferroni corrected for the number of multiple comparisons. In order to identify variables that were significantly capable of classifying subjects as having OCPD symptoms at diagnostic threshold or not, binary logistic regression was used including all possibly predictive variables (all variables listed in Table 2). This statistical approach enabled variables significantly associated with OCPD symptoms at the diagnostic threshold to be identified, while controlling for variation in other measures. We did not exclude people endorsing 1-3 OCPD criteria from the reference group because we wished for our analysis to detect meaningful associations with symptoms that were likely clinically significant rather than sub-syndromal. The binary logistic regression used method ‘Enter’, with a model constant, classification cut-off 0.5, and maximum iterations 20. Model assumptions and fit were evaluated using inter alia Hosmer-Lemeshow goodness of fit, case-wise listing of residuals, and inspection of outliers. For the purposes of the binary logistic regression, statistical significance for individual predictors was defined as p<0.05, two-tailed, uncorrected. Our rationale for this is that multiplicity is controlled for at the level of the overall model significance – i.e. this approach first asks if a combination of variables can successfully classify participants; if so, it then asks what variables accounted for this. All data analyses were conducted using SPSS 22.
Table 2. Demographic and Clinical Characteristics of subjects with and without OCPD symptoms (endorsement of at least 4 of 8 diagnostic criteria).
Data are displayed as mean (standard deviation) or number, n, of cases [% of group].
| Controls (N=377) |
OCPD symptom group (N=946) |
F | Uncorrected P | Corrected Sig | |
|---|---|---|---|---|---|
| Age, years | 28.5 (13.0) | 26.2 (11.1) | 10.377 | 0.001 | * |
| Sex male, n [%] | 163 [43.2%] | 344 [36.4%] | @ | 0.0241 | n.s. |
| Ethnicity White, n [%] | 259 [68.7%] | 670 [70.8%] | @ | 0.464 | n.s. |
| Educational Level | 1.44 (1.90) | 1.03 (1.70) | 14.573 | <0.001 | ** |
| Generalized Anxiety Disorder, n [%] | 30 [8.0%] | 208 [22.0%] | @ | <0.0001 | ** |
| Social Anxiety Disorder, n [%] | 24 [6.4%] | 146 [15.4%] | @ | <0.0001 | ** |
| Avoidant Personality Disorder, n [%] | 119 [31.6%] | 495 [52.3%] | @ | <0.0001 | ** |
| OCD, n [%] | 22 [5.8%] | 125 [13.2%] | 16.063 | <0.001 | ** |
| Internet Addiction symptoms, IAT total score | 29.0 (9.6) | 32.6 (11.8) | 27.279 | <0.001 | ** |
| ADHD symptoms, ASRS total score | 16.2 (0.39) | 19.8 (0.25) | 62.951 | <0.001 | ** |
| BIS Attentional impulsivity | 18.9 (5.1) | 18.1 (4.8) | 7.558 | 0.006 | n.s. |
| BIS Motor impulsivity | 25.9 (6.9) | 24.0 (6.8) | 22.671 | <0.001 | ** |
| BIS Non-Planning impulsivity | 25.8 (4.8) | 23.5 (5.1) | 58.590 | <0.001 | ** |
| Padua Contamination Obsessions and Washing Compulsions | 6.8 (6.8) | 11.0 (8.4) | 72.255 | <0.001 | ** |
| Padua Dressing/Grooming Compulsions | 1.3 (2.0) | 2.6 (2.9) | 62.004 | <0.001 | ** |
| Padua Checking Compulsions | 7.6 (6.4) | 12.7 (8.5) | 110.317 | <0.001 | ** |
| Padua Thought of Harm to Self/Others | 3.2 (3.7) | 6.0 (5.3) | 87.753 | <0.001 | ** |
| Padua Impulses to Harm Self/Others | 2.2 (3.7) | 3.7 (5.2) | 25.199 | <0.001 | ** |
Statistical tests refer to ANOVA F, except where indicated c = chi-square test. IAT = Young’s Internet Addiction Diagnostic Questionnaire; BIS = Barratt Impulsiveness Questionnaire; Padua = obsessive-compulsive questionnaire; ASRS = Adult ADHD Rating Scale.
Corrected sig. refers to whether differences are statistically significant with Bonferroni correction: * <0.05, ** p<0.01, n.s. not significant.
Results
In the study sample, 946 people in the sample met criteria for OCPD symptoms (endorsing 4 or more of DSM criteria, out of 8), while 377 people did not. The mean (standard deviation) total number of OCPD criteria endorsed in the two groups were 5.8 (1.4) and 2.2 (0.9), respectively. Table 2 provides an overview of the demographic and clinical measures in the two groups, along with group statistical comparisons, for each variable considered independently. It can be seen that the OCPD symptom group – compared to non-OCPD symptom group – was significantly younger, and had lower mean educational level, but did not differ significantly in terms of race-ethnicity. There was a tendency towards there being a lower than expected proportion of females in the OCPD symptom group, but this finding was not significant with Bonferroni correction applied.
In terms of morbidity, the OCPD symptom group showed significantly higher occurrence of generalized anxiety disorder, social anxiety disorder, OCD, and avoidant personality disorder, compared to the control group. They also scored significantly higher in terms of Internet Addiction total scores, and ADHD symptom total scores. OCPD symptoms were also associated with lower impulsiveness scores on the Barratt (all three sub-scales, albeit differences only withstood Bonferroni correction for two of the sub-scales); and significantly higher Padua obsessive-compulsive scores (all five domains).
Binary regression identified a significant model (Chi-square = 257.031, df=18, p<0.001) that accounted for approximately 25.3% in the variance in occurrence of OCPD (as indexed by Nagelkerke R square). The model was an adequate fit according to the Hosmer and Lemeshow test. The overall percentage successful classification of the model was 75.2%. Model beta coefficients and p values are indicated in Table 3. It can be seen that presence of OCPD was significantly predicted by (in order of diminishing statistical significance): lower Barratt non-planning impulsivity, higher ADHD symptom scores, higher Internet addiction symptoms, presence of avoidant personality disorder, female gender, presence of generalized anxiety disorder, higher Padua checking compulsions, and higher Padua dressing/grooming compulsions. The constant term was significant (Wald 9.428, p=0.002) with beta value 2.085 (standard error 0.679). The Receiver Operating Characteristic (ROC) for the ability of the binary logistic model to identify OCPD in the sample is shown in Figure 1 below; total area under the curve was .78, indicating fair to good properties.
Table 3. Results of the binary logistic regression predicting presence of OCPD versus not.
Variables are listed in order of descending statistical significance.
| B | S.E. | Wald | Sig. | Estimated Odds Ratio | |
|---|---|---|---|---|---|
| Significant predictors in model | |||||
| Barratt Non-Planning Impulsivity | -0.117 | 0.017 | 45.832 | <0.001 | 0.890 |
| ADHD score, ASRS | 0.043 | 0.012 | 14.198 | <0.001 | 1.044 |
| Internet Addiction score, IAT | 0.027 | 0.009 | 9.407 | 0.002 | 1.027 |
| Avoidant Personality Disorder, present | 0.421 | 0.154 | 7.497 | 0.006 | 0.656 |
| Gender, male | -0.309 | 0.143 | 4.676 | 0.031 | 1.362 |
| Generalized Anxiety Disorder, present | 0.535 | 0.252 | 4.491 | 0.034 | 0.586 |
| Padua Checking Compulsions | 0.028 | 0.014 | 4.279 | 0.039 | 1.028 |
| Padua Dressing/Grooming Compulsions | 0.074 | 0.037 | 4.025 | 0.045 | 1.077 |
| Non-significant predictors in model | |||||
| Padua Contamination Obsessions and Washing Compulsions | 0.022 | 0.012 | 3.543 | 0.060 | 1.022 |
| Padua Thoughts of Harm to Self/Others | 0.024 | 0.024 | 1.018 | 0.313 | 1.024 |
| Barratt Motor Impulsivity | 0.010 | 0.018 | 0.328 | 0.567 | 1.010 |
| Age | -0.003 | 0.007 | 0.231 | 0.630 | 0.997 |
| Race, Caucasian | 0.072 | 0.152 | 0.226 | 0.635 | 0.930 |
| Barratt Attentional Impulsivity | -0.011 | 0.023 | 0.207 | 0.649 | 0.989 |
| Educational level | -0.009 | 0.069 | 0.017 | 0.897 | 0.991 |
| Presence of OCD | 0.016 | 0.285 | 0.003 | 0.956 | 0.984 |
| Social Anxiety Disorder, present | -0.011 | 0.285 | 0.001 | 0.970 | 1.011 |
| Padua Impulses of Harm to Self/Others | 0.000 | 0.021 | 0.000 | 0.990 | 1.000 |
IAT = Young’s Internet Addiction Diagnostic Questionnaire; ADHD = attention-deficit hyperactivity disorder; BIS = Barratt Impulsiveness Questionnaire; Padua = obsessive-compulsive questionnaire; ASRS = Adult ADHD Symptom Rating Scale. Sig. indicates uncorrected p value. All df = 1.
Discussion
In this study, we explored relationships between OCPD symptoms (endorsement of four or more DSM-5 criteria) and measures of impulsivity plus compulsivity, in a relatively large sample of Internet users. The main findings, robust in regression modelling, were that the OCPD symptom group, compared to controls, was less impulsive on a questionnaire measure, had more obsessive-compulsive symptoms (specifically checking, dressing, and grooming compulsions), and had more ADHD symptoms and problematic Internet use. OCPD symptoms were also associated with female gender, occurrence of generalized anxiety disorder, and occurrence of avoidant personality disorder.
The finding of a dissociation between impulsivity and compulsivity, whereby OCPD symptoms were characterized by less impulsivity on the Barratt non-planning subscale, but more compulsivity as indexed by Padua inventory sub-scores, has potentially quite profound broader implications for how we conceptualize impulsivity/compulsivity. In terms of impulsivity, our results are broadly consistent with a previous report of lower (rather than higher) reward discounting impulsivity (26), and lower non-planning impulsivity (25) in OCPD. These results may run counter to the suggestion that OCPD in general is a consequence of individuals with high trait impulsivity, in terms of personality, exerting rigid/controlling traits in order to maintain more optimal life functioning (23). These results also militate against the idea that questionnaire-based impulsive and compulsive features are underpinned by a common substrate. At the same time, we found that higher ADHD symptoms were associated with OCPD symptomatology; we suspect this may reflect overlap at the level of screening questions rather than contradicting the Barratt findings: the ASRS self-report scale for ADHD measures aspects including difficulty finalizing the details of projects, difficulty getting things in order, and fidgeting/squirming when having to sit still. Individuals could endorse such items due to OCPD related rigidity and perfectionism, rather than due to fundamental problems with hyperactivity, inattention, or impulsivity.
While OCPD by definition is functionally impairing, milder forms of some of the symptoms could be viewed as being potentially adaptive or useful. Notably we did not address the “functional impairment” aspect of OCPD, as we assessed OCPD symptoms rather than a formal diagnosis, using a tick-list for the 8 symptom types. For example, in many occupations, high productivity and perfectionism might indeed be valued by society at large (35). In the US National Epidemiologic Survey on Alcohol and Related Conditions (2001-2002), OCPD was not consistently related to higher occurrence of disability, unlike virtually all other personality disorders (5). The finding of an apparent ‘trade off’ or dissociation between Barratt Impulsiveness and Padua Compulsiveness may hint at such functional usefulness of aspects of OCPD, at least conceivably in milder forms. Future work could explore this by including measures of day-to-day functioning. Future research could also evaluate OCPD symptoms and their correlates longitudinally, because some studies suggest that OCPD is not temporally stable (36). Indeed, the long held notion that personality disorders in general are temporally stable is being increasingly challenged. The temporal stability of personality disorders may be much lower than for disorders such as schizophrenia (37). Thus, it may be better to conceptualize aberrant personality in terms of function or diathesis at a specific time point, rather than in categorical terms (38). Longitudinal exploration of OCPD could also help to address the interplay we observed here between OCPD and higher (rather than lower) apparent ADHD symptoms.
The finding that Internet addiction scores were higher in participants with OCPD symptoms, and also significantly predicted higher endorsement of OCPD items, is interesting in view of increasing interest in this putative psychiatric problem. The DSM-5 listed Internet Gaming Disorder as a condition in need of further study. If one accepts that OCPD traits likely develop before internet addiction, this may suggest that the rigid and maladaptive profile of OCPD predisposes towards habitual, potentially maladaptive use of the Internet. We did not assess other types of personality type and as such further work would be needed before concluding that OCPD has a particular or unique relationship with internet use problems, as compared to other types of personality disorder. In a cross-sectional study, using in-person assessments, Internet addiction was associated with significantly higher rates of personality disorders, especially with cluster C personality traits (which would include OCPD) in men (39). However, the group-level difference was not significant at the level of OCPD viewed separately, perhaps reflecting the low frequency of this category of disorder in the sample (39). In general, more research is needed regarding personality in Internet addiction, as data are negative or conflicting (40).
Our data may help to resolve the issue as to how OCPD and OCD symptoms overlap from a symptomatic perspective. As outlined previously, these conditions show very high comorbidity at the level of full disorder (20), and this comorbidity appears to influence how these disorders manifest (such as in terms of age at onset, or types of symptoms found – albeit with inconsistent results between studies) (16–19). Accounting for other variables, OCPD symptoms were not significantly predicted by presence of OCD itself in our study, but it was predicted by higher scores on Padua scales for checking compulsions and for dressing/grooming compulsions. The Padua measure for checking compulsions contains items such as returning to check switches/doors/taps, checking documents, checking that matches/cigarettes are properly extinguished, recounting money, checking letters before posting them, and re-reading work. The Padua dressing/grooming measure asks about following a particular order when washing/dressing/undressing, doing things in a certain order before sleep, and folding clothes in a particular way. Endorsements for these types of question can readily be expected in people who are rigid and have a particular perfectionistic approach to life, as in OCPD, rather than constituting ‘OCD within OCPD’. We interpret these findings to suggest that the overlap between OCPD and OCD symptoms observed in the literature might stem from overlapping symptom endorsements, for different reasons, rather than being due to common psychopathological mechanisms.
We believe this study fills a void in the literature, in view of its large sample size and inclusion of both impulsive and compulsive measures; nonetheless, there are several major limitations that should be considered. While participants were asked about the eight symptom domains for OCPD, this being an Internet survey, we were unable to assess whether full diagnostic criteria were met. In particular, we did not ask whether symptoms were pervasive, impairing, consistent over time, and present in a variety of contexts. Had we asked about these areas, the validity of this information would have been questionable as well, in the absence of face-to-face, structured, assessments by a healthcare professional. The validity and reliability of online version of the DSM OCPD checklist is not established. The rate of OCPD symptoms was unusually high in our sample, which may indicate that this approach lead to over-endorsement; or, in the alternative, this could truly reflect high rates of OCPD in Internet users who complete online surveys. Nonetheless we feel our results may be informative for the field, indicating associations between OCPD symptoms and other impulsive/compulsive clinical features in Internet users, which merit more rigorous scientific scrutiny. There are several limitations inherent in the use of online questionnaires, including recall and other bias, and limitations in the types of measures that could be collected (due to our desire to avoid excessive subject burden and data attrition). Because multiplicity in the regression model is effectively controlled for at the level of the overall model significance, we did not adjust for multiple comparisons at the level of individual variables within this model. Such an approach is typical in the field, and in our view justified, but this approach does run the risk of potential false positives. As such, replication is warranted before firm conclusions are drawn, especially for significant variables in the model whose p values were close to 0.05. Lastly, future work would benefit from including online neuropsychological tests as well as self-report questionnaires. For example, this could be useful to help ensure that people endorsing ADHD symptoms in such an online survey also present with cognitive impairments consistent with inattention and impulsivity (relative to controls).
In summary, OCPD symptoms, defined using a threshold of endorsement of at least 4 of 8 DSM criteria, was associated with multiple forms of psychopathology including ADHD, certain OCD symptoms, and more problematic Internet use itself. We suggest that OCPD – previously almost entirely neglected in neurobiological research of mental disorders – might be a valuable model for exploring impulsivity, compulsivity, and the interplay between these processes, both at the level of top-level symptoms/personality, and in terms of neurobiology. Confirmation of these associations between OCPD symptoms and different forms of impulsive and compulsive psychopathologies merits validation using gold-standard in-person assessments, in Internet users and in the wider background population.
Funding
This research was supported by a Grant from the Academy of Medical Sciences (UK) and by a Wellcome Trust Clinical Fellowship (110049/Z/15/Z) to Dr Chamberlain.
Footnotes
Disclosure(s): Dr Chamberlain consults for Cambridge Cognition. Dr Grant has received research Grants from the National Center for Responsible Gaming, and Forest and Roche Pharmaceuticals. Dr Grant receives yearly compensation from Springer Publishing for acting as Editor-in-Chief of the Journal of Gambling Studies and has received royalties from Oxford University Press, American Psychiatric Publishing, Inc., Norton Press, and McGraw Hill. The other authors report no potential conflicts of interest or funding declarations
References
- 1.Association AP. Diagnostic and statistical manual of mental disorders (DSM-5) 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 2.Janet P. Les obsessions et al psychasthenie. Paris: Bailliere; 1904. [Google Scholar]
- 3.Diedrich A, Voderholzer U. Obsessive-compulsive personality disorder: a current review. Current psychiatry reports. 2015;17(2):2. doi: 10.1007/s11920-014-0547-8. Epub 2015/01/27. [DOI] [PubMed] [Google Scholar]
- 4.de Reus RJ, Emmelkamp PM. Obsessive–compulsive personality disorder: a review of current empirical findings. Personality and Mental Health. 2012;6(1):1–21. [Google Scholar]
- 5.Grant BF, Hasin DS, Stinson FS, Dawson DA, Chou SP, Ruan WJ, et al. Prevalence, correlates, and disability of personality disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. The Journal of clinical psychiatry. 2004;65(7):948–58. doi: 10.4088/jcp.v65n0711. Epub 2004/08/05. [DOI] [PubMed] [Google Scholar]
- 6.Grant JE, Mooney ME, Kushner MG. Prevalence, correlates, and comorbidity of DSM-IV obsessive-compulsive personality disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of psychiatric research. 2012;46(4):469–75. doi: 10.1016/j.jpsychires.2012.01.009. Epub 2012/01/20. [DOI] [PubMed] [Google Scholar]
- 7.Nestadt G, Romanoski AJ, Brown CH, Chahal R, Merchant A, Folstein MF, et al. DSM-III compulsive personality disorder: an epidemiological survey. Psychological medicine. 1991;21(2):461–71. doi: 10.1017/s0033291700020572. [DOI] [PubMed] [Google Scholar]
- 8.Torgersen S, Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Archives of general psychiatry. 2001;58(6):590–6. doi: 10.1001/archpsyc.58.6.590. Epub 2001/06/29. [DOI] [PubMed] [Google Scholar]
- 9.Skodol AE, Gunderson JG, McGlashan TH, Dyck IR, Stout RL, Bender DS, et al. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiatry. 2002;159(2):276–83. doi: 10.1176/appi.ajp.159.2.276. [DOI] [PubMed] [Google Scholar]
- 10.van den Heuvel OA, van Wingen G, Soriano-Mas C, Alonso P, Chamberlain SR, Nakamae T, et al. Brain circuitry of compulsivity. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology. 2015 doi: 10.1016/j.euroneuro.2015.12.005. Epub 2015/12/30. [DOI] [PubMed] [Google Scholar]
- 11.Gillan CM, Robbins TW, Sahakian BJ, van den Heuvel OA, van Wingen G. The role of habit in compulsivity. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology. 2015 doi: 10.1016/j.euroneuro.2015.12.033. Epub 2016/01/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chamberlain SR, Sahakian BJ. The neuropsychiatry of impulsivity. Current opinion in psychiatry. 2007;20(3):255–61. doi: 10.1097/YCO.0b013e3280ba4989. [DOI] [PubMed] [Google Scholar]
- 13.Daruna JH, Barnes PA. A neurodevelopmental view of impulsivity. In: M WG, Johnson JL, Shure MB, editors. The impulsive client: theory, research and treatment. Washington, D. C.: American Psychological Association; 1993. [Google Scholar]
- 14.Fineberg NA, Sharma P, Sivakumaran T, Sahakian B, Chamberlain SR. Does obsessive-compulsive personality disorder belong within the obsessive-compulsive spectrum? CNS spectrums. 2007;12(6):467–82. doi: 10.1017/s1092852900015340. [DOI] [PubMed] [Google Scholar]
- 15.Gordon OM, Salkovskis PM, Oldfield VB, Carter N. The association between obsessive compulsive disorder and obsessive compulsive personality disorder: prevalence and clinical presentation. The British journal of clinical psychology / the British Psychological Society. 2013;52(3):300–15. doi: 10.1111/bjc.12016. Epub 2013/07/20. [DOI] [PubMed] [Google Scholar]
- 16.Coles ME, Pinto A, Mancebo MC, Rasmussen SA, Eisen JL. OCD with comorbid OCPD: a subtype of OCD? Journal of psychiatric research. 2008;42(4):289–96. doi: 10.1016/j.jpsychires.2006.12.009. Epub 2007/03/27. [DOI] [PubMed] [Google Scholar]
- 17.Starcevic V, Berle D, Brakoulias V, Sammut P, Moses K, Milicevic D, et al. Obsessive-compulsive personality disorder co-occurring with obsessive-compulsive disorder: Conceptual and clinical implications. The Australian and New Zealand journal of psychiatry. 2013;47(1):65–73. doi: 10.1177/0004867412450645. Epub 2012/06/13. [DOI] [PubMed] [Google Scholar]
- 18.Lochner C, Serebro P, van der Merwe L, Hemmings S, Kinnear C, Seedat S, et al. Comorbid obsessive-compulsive personality disorder in obsessive-compulsive disorder (OCD): a marker of severity. Progress in neuro-psychopharmacology & biological psychiatry. 2011;35(4):1087–92. doi: 10.1016/j.pnpbp.2011.03.006. Epub 2011/03/18. [DOI] [PubMed] [Google Scholar]
- 19.Eisen JL, Coles ME, Shea MT, Pagano ME, Stout RL, Yen S, et al. Clarifying the convergence between obsessive compulsive personality disorder criteria and obsessive compulsive disorder. J Personal Disord. 2006;20(3):294–305. doi: 10.1521/pedi.2006.20.3.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mancebo MC, Eisen JL, Grant JE, Rasmussen SA. Obsessive compulsive personality disorder and obsessive compulsive disorder: clinical characteristics, diagnostic difficulties, and treatment. Annals of clinical psychiatry : official journal of the American Academy of Clinical Psychiatrists. 2005;17(4):197–204. doi: 10.1080/10401230500295305. Epub 2006/01/13. [DOI] [PubMed] [Google Scholar]
- 21.Samuels J, Nestadt G, Bienvenu OJ, Costa PT, Jr, Riddle MA, Liang KY, et al. Personality disorders and normal personality dimensions in obsessive-compulsive disorder. The British journal of psychiatry : the journal of mental science. 2000;177:457–62. doi: 10.1192/bjp.177.5.457. [DOI] [PubMed] [Google Scholar]
- 22.Stein DJ, Hollander E. Obsessive-compulsive spectrum disorders. The Journal of clinical psychiatry. 1995;56(6):265–6. [PubMed] [Google Scholar]
- 23.Villemarette-Pittman NR, Stanford MS, Greve KW, Houston RJ, Mathias CW. Obsessive-compulsive personality disorder and behavioral disinhibition. The Journal of psychology. 2004;138(1):5–22. doi: 10.3200/JRLP.138.1.5-22. Epub 2004/04/22. [DOI] [PubMed] [Google Scholar]
- 24.Irastorza Eguskiza LJ, Bellon JM, Mora M. Comorbidity of personality disorders and attention-deficit hyperactivity disorder in adults. Revista de psiquiatria y salud mental. 2016 doi: 10.1016/j.rpsm.2016.01.009. Epub 2016/03/13. Comorbilidad de trastornos de personalidad y trastorno por deficit de atencion e hiperactividad en adultos. [DOI] [PubMed] [Google Scholar]
- 25.Melca IA, Yucel M, Mendlowicz MV, de Oliveira-Souza R, Fontenelle LF. The correlates of obsessive-compulsive, schizotypal, and borderline personality disorders in obsessive-compulsive disorder. Journal of anxiety disorders. 2015;33:15–24. doi: 10.1016/j.janxdis.2015.04.004. Epub 2015/05/10. [DOI] [PubMed] [Google Scholar]
- 26.Pinto A, Steinglass JE, Greene AL, Weber EU, Simpson HB. Capacity to delay reward differentiates obsessive-compulsive disorder and obsessive-compulsive personality disorder. Biol Psychiatry. 2014;75(8):653–9. doi: 10.1016/j.biopsych.2013.09.007. Epub 2013/11/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of clinical psychiatry. 1998;59(Suppl 20):22–33. quiz 4-57. [PubMed] [Google Scholar]
- 28.Young KS. Caught in the net: how to recognize the signs of internet addiction – and a winning strategy for recovery. New York: Wiley; 1998. [Google Scholar]
- 29.Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychological medicine. 2005;35(2):245–56. doi: 10.1017/s0033291704002892. Epub 2005/04/22. [DOI] [PubMed] [Google Scholar]
- 30.Kessler RC, Adler LA, Gruber MJ, Sarawate CA, Spencer T, Van Brunt DL. Validity of the World Health Organization Adult ADHD Self-Report Scale (ASRS) Screener in a representative sample of health plan members. International journal of methods in psychiatric research. 2007;16(2):52–65. doi: 10.1002/mpr.208. Epub 2007/07/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burns GL, Keortge SG, Formea GM, Sternberger LG. Revision of the Padua Inventory of obsessive compulsive disorder symptoms: distinctions between worry, obsessions, and compulsions. Behaviour research and therapy. 1996;34(2):163–73. doi: 10.1016/0005-7967(95)00035-6. [DOI] [PubMed] [Google Scholar]
- 32.Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51(6):768–74. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 33.Barratt ES. Factor analysis of some psychometric measures of impulsiveness and anxiety. Psychological reports. 1965;16:547–54. doi: 10.2466/pr0.1965.16.2.547. [DOI] [PubMed] [Google Scholar]
- 34.Grassi G, Pallanti S, Righi L, Figee M, Mantione M, Denys D, et al. Think twice: Impulsivity and decision making in obsessive-compulsive disorder. J Behav Addict. 2015;4(4):263–72. doi: 10.1556/2006.4.2015.039. Epub 2015/12/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Paykel ES, Prusoff BA. Relationships between personality dimensions: neuroticism and extraversion against obsessive, hysterical and oral personality. The British journal of social and clinical psychology. 1973;12(3):309–18. doi: 10.1111/j.2044-8260.1973.tb00073.x. Epub 1973/09/01. [DOI] [PubMed] [Google Scholar]
- 36.Shea MT, Stout R, Gunderson J, Morey LC, Grilo CM, McGlashan T, et al. Short-term diagnostic stability of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. Am J Psychiatry. 2002;159(12):2036–41. doi: 10.1176/appi.ajp.159.12.2036. [DOI] [PubMed] [Google Scholar]
- 37.Baca-Garcia E, Perez-Rodriguez MM, Basurte-Villamor I, Fernandez del Moral AL, Jimenez-Arriero MA, Gonzalez de Rivera JL, et al. Diagnostic stability of psychiatric disorders in clinical practice. The British journal of psychiatry : the journal of mental science. 2007;190:210–6. doi: 10.1192/bjp.bp.106.024026. Epub 2007/03/03. [DOI] [PubMed] [Google Scholar]
- 38.Tyrer P, Coombs N, Ibrahimi F, Mathilakath A, Bajaj P, Ranger M, et al. Critical developments in the assessment of personality disorder. The British journal of psychiatry Supplement. 2007;49:s51–9. doi: 10.1192/bjp.190.5.s51. Epub 2007/05/02. [DOI] [PubMed] [Google Scholar]
- 39.Zadra S, Bischof G, Besser B, Bischof A, Meyer C, John U, Rumpf HJ. The association between Internet addiction and personality disorders in a general population-based sample. J Behav Addict. 2016 Dec;5(4):691–699. doi: 10.1556/2006.5.2016.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Byun S, Ruffini C, Mills JE, Douglas AC, Niang M, Stepchenkova S, Lee SK, Loutfi J, Lee JK, Atallah M, Blanton M. Internet addiction: metasynthesis of 1996-2006 quantitative research. Cyberpsychol Behav. 2009 Apr;12(2):203–7. doi: 10.1089/cpb.2008.0102. [DOI] [PubMed] [Google Scholar]