Abstract
Background
China uses both social health insurance (SHI) programs and a medical financial assistance (MFA) program to protect the poor from illness-induced financial risks. The MFA provides a dual benefit package targeting low-income families: subsidizing these families’ participation in SHI programs, and providing cash aid to protect them from catastrophic health expenditure (CHE). This study aims to investigate: (1) the association between MFA subvention for SHI enrollment and SHI enrollment; (2) the association between MFA cash aid and CHE; and (3) the association between SHI enrollment and CHE in low-income households in China.
Methods
Using nationally representative data from a comprehensive survey of low-income households in 2014, we construct an estimate of CHE based on out-of-pocket health spending data. Controlling for other covariates, we estimate the three associations using a three-level logistic model.
Results
The MFA program subsidizes 50.1% of low-income households to aid their enrollment in SHI programs and provides cash aid to 24.1% of these households. Multilevel logistic analysis reveals that MFA subvention has no significant association with low-income households’ SHI enrollment, that MFA cash aid has no significant association with CHE, and that full SHI enrollment is inversely associated with CHE status.
Conclusions
The MFA program is currently not an effective supplement to SHI programs in China in terms of promoting SHI enrollment and providing financial risk protection. The Chinese government needs to invest more funds to expand further low-income household enrollment in SHI programs and to widen the benefit package of MFA cash aid.
Electronic supplementary material
The online version of this article (doi:10.1186/s12939-017-0638-3) contains supplementary material, which is available to authorized users.
Keywords: China, Medical financial assistance, Cash aid, Social health insurance, Catastrophic health expenditure
Background
Poverty has been redefined as encompassing not only material deprivation but also low achievements in health, education, and so on [1]. There is a vicious cycle linking poverty and poor health, in that the poor are particularly vulnerable to financial risks caused by serious illness and high out-of-pocket expenditure (OPE) on health, which may further worsen their health [2, 3]. A common measure of the financial risks related to illness is catastrophic health expenditure (CHE) [4, 5]. CHE is defined as a household’s OPE exceeding a substantial fraction of the household’s total expenditure or capacity to pay [4–9]. Previous studies have found that the percentage of households with CHE in China was 9.9% in rural areas in 2001 [10], 12.9% in 2011 [9], and 13.0% in 2012 [11]. In addition, the percentage of households with CHE is region- and socio-demographic characteristic-specific. It is significantly higher in the central and western regions of China, such as Chongqing and Shaanxi Province, than in eastern regions like Shanghai and Shandong Province [10–14]. Undeveloped areas, rural families, households with older adults and chronically ill members, and low-income households are more likely to incur CHE and impoverishment due to health expenditure [12, 15, 16].
Investing in health services is a rational choice for health equity promotion and poverty reduction strategies in developing countries [17]. The World Health Organization (WHO) advocates “pro-poor” health policies and has launched global advocacy, regional initiatives, and direct support for developing countries implementing such health policies [18]. Countries have implemented various health policies to prevent poor families from falling into medical impoverishment, out of which social health insurance (SHI) and medical financial assistance (MFA) programs are most often adopted. SHI, as a financing approach for mobilizing funds and pooling risks, provides health insurance to contributing members and their dependents and often requires mandatory contributions [19, 20]. MFA provides financial aid to cover the poor’s medical spending directly or to assist them to participate in health insurance programs [21, 22]. Many low- and middle-income countries, such as Turkey, Indonesia, Colombia, and Mexico, have used SHI programs to provide mandatory health service coverage for vulnerable people [20, 23–26]. Countries, such as Georgia and many sub-Saharan African countries, have established MFA programs for the poor who have experienced serious illnesses [21, 22]. Other countries, such as India, Rwanda, Lao People’s Democratic Republic, Vietnam, and Senegal, have developed community-based health insurance to protect the enrollees from medical impoverishment [27–33]. The effects of SHI and MFA programs vary in these countries. SHI enrollment accompanies high OPE in Turkey [23], and reduces OPE in Indonesia, Colombia, and Mexico [24–26]. MFA significantly increases medical care utilization by the poor in Georgia [21], while it has low coverage of enrollment among the poor in sub-Saharan African countries [22].
China uses both SHI program and a MFA program to protect the poor from the financial risks of illness. The SHI system in China, introduced in the first decade of the twenty-first century, is targeted at all types of residents. It comprises three government-run schemes (see Table 1) and reached universal coverage at the beginning of the 2010s [34]. The MFA program in China, targeting low-income households, is used as a supplement to SHI programs and provides extra financial assistance to low-income households in addition to SHI. A low-income household in this study is defined as a household where income or assets are officially identified as lower than a certain county-specific criterion. It includes four types of households: households enrolled in the Minimum Living Standard Scheme (MLSS), extremely poor residents, households with a monthly income of between 100% and 120–150% of the local MLSS line, and other vulnerable persons identified by local county government [35–40].
Table 1.
Policy design of the MFA program and SHI programs in China
| Medical Financial Assistance (MFA) | Social Health Insurance (SHI) | |
|---|---|---|
| Policy implementation | 2003: The Ministry of Civil Affairs piloted the MFA in a few rural areas; 2005: The Ministry of Civil Affairs piloted the MFA in a few urban areas; 2009: The MFA reached universal coverage across the whole country; 2013: The Ministry of Finance and the Ministry of Civil Affairs required localities to coordinate the management of SHI programs and the MFA, aiming to provide one-time reimbursement to target households; 2014: The State Council enacted the Draft Decree on Social Assistance, legitimizing the MFA as an indispensable part of social assistance programs; 2015: The State Council ruled that the MFA gives priority to households with serious illnesses. |
1998: The State Council established the Urban Employee Basic Medical Insurance (UEBMI); 2003: The Ministry of Health, the Ministry of Finance, and the Ministry of Agriculture established the New Cooperative Medical Scheme (NCMS); 2007: The State Council established the Urban Resident Basic Medical Insurance (URBMI); 2009: The Communist Party of China Central Committee and the State Council launched a new health care reform; 2010: The three SHI programs reached universal coverage across the whole country. 2016: The State Council decided to integrate the URBMI with the NCMS. |
| Targets | (1) Households enrolling in the Minimum Living Standard Scheme (MLSS). The MLSS is a national social assistance program and targets the poorest households where monthly or yearly income is lower than a certain criterion. Unlike the national unified poverty line [2300 Chinese Yuan (USD372) in 2011 and 3000 Yuan (USD488) in 2016] that was regulated by the State Council Leading Group Office of Poverty Alleviation and Development to facilitate county-based poverty alleviation, the MLSS, run by the Ministry of Civil Affairs, is a household-based cash aid program. Its criterion of eligibility is county-specific in most areas and province-specific in some others. In 2016, the criterion in Shanghai was a monthly income per person of 880 Yuan (USD143) for a household, the highest in any province. An MLSS applicant must be reviewed through a complicated means-test of his/her household’s monetary income, basic living needs, and other household characteristics such as labor capacity and severe illnesses. The difference between the estimated income of an MLSS household and the local MLSS criterion is paid to the household. (2) Extremely poor residents (EPR, including: “Sanwu,” urban residents with no income, labor capacity, or caregivers; “Wubao,” rural residents with no income, labor capacity, or caregivers; “Tekun,” households defined as extremely poor by the Draft Decree on Social Assistance). (3) Low-income families not enrolled in the MLSS (LIF, identified by local government; the criterion is usually a monthly family income of between 100% and 120–150% of the local MLSS line). (4) Persons who are identified by county government. |
(1) The UEBMI provided mandatory coverage to urban employees. (2) The URBMI provided voluntary coverage to urban residents without formal employment. (3) The NCMS provided voluntary coverage to rural residents. |
| Benefit package | Dual benefit package: (1) Subvention for SHI enrollment. Target households are subsidized for their enrollment in SHI programs. (2) Cash aid. Members of target households can apply for MFA cash aid from the county Bureau of Civil Affairs if their OPE exceeds the thresholds of the MFA. If they are enrolled in a SHI scheme, MFA cash aid is provided as a proportion of their OPE; if not, the MFA cash subsidy is provided as a proportion of their total medical expenditure. |
Covers both outpatient and inpatient services and provides reimbursement to patients immediately or afterwards. |
| Funding sources | Raised from (1) government budget, (2) lottery welfare fund, and (3) society donations; County government normally sets up a special and independent MFA account within the SHI system, manages all funds uniformly, and takes full responsibility for its activities. |
Raised by a special SHI agency or taxation agencies by collecting premiums; Premium for the UEBMI is contributed by individual employees and employers; Premium for the URBMI and the NCMS is contributed by individual residents and the government. |
The MFA provides a dual benefit package for low-income families: subsidizing their enrollment in a SHI program (MFA subvention for SHI enrollment), and providing cash aid to eligible households to reimburse their medical expenditure (MFA cash aid) [41, 42]. The MFA pays part (partial MFA subvention, over 50% of premiums in most provinces) or all (full MFA subvention, 100% of premiums) of the premium (120 Chinese yuan [USD19.5] per household member in 2016) needed to enroll in a SHI for members of eligible low-income households. Those households obtaining partial MFA subvention must pay the remaining premium themselves. In rural areas, the MFA subsidizes eligible households’ enrollment in the New Cooperative Medical Scheme (NCMS), while in urban areas it subsidizes participation in the Urban Resident Basic Medical Insurance (URBMI). In practice, members in some households choose not to enroll in the two insurance programs after considering their affordability, health status, or employment conditions. As a result, low-income households may have all (full SHI enrollment), part (partial SHI enrollment), or none (no SHI enrollment) of their members enrolled in the insurance programs. Low-income households with a SHI enrollment may have most (more than 50% in practice) of their medical payments covered by SHI programs; if their OPE exceeds the thresholds regulated by the MFA, they can apply for cash aid from local authorities. A detailed chronology of policy design, targets, benefit packages, and funding sources for the MFA and SHI are presented in Table 1. During practical implementation, the policy design of the MFA (including thresholds, reimbursement rates, ceilings, and limitations on the eligibility for various illnesses and medical care services) varies across provinces and counties. For example, the thresholds for serious illnesses range from over USD100 to about USD5,000, while the cash aid for these illnesses accounts for 30–100% of OPE across provinces (see Additional file 1: Table S1).
The Chinese government launched the MFA to achieve two aims: (1) promoting SHI enrollment among the poor; and (2) improving the poor’s access to care and financial risk protection [36–38, 41]. Numerous studies have evaluated the performance of SHI programs in reducing CHE and medical impoverishment [8, 10, 16, 43–47]. Based on a small number of samples collected from a few counties, several studies have investigated the MFA program’s effect on poor families’ utilization of medical care services and their medical expenditure [39, 42, 48]. However, little empirical evidence has been generated on the role the MFA program plays in promoting SHI enrollment and reducing CHE. Given the rapid development and expansion of China’s MFA program, it is necessary and urgent to assess its role in promoting SHI enrollment and financial risk protection to provide evidence for evaluation and health policy development.
Using nationally representative data from a comprehensive survey of low-income households in 2014, this study investigated the role MFA subvention plays in promoting SHI enrollment and the association between MFA cash aid and CHE in China. We also examined the association between SHI enrollment and CHE. Figure 1 illustrates a conceptual framework for this study. To our knowledge, this study is the first policy study that uses a nationally representative dataset to investigate the MFA’s role in facilitating SHI enrollment and protecting low-income households from catastrophic health spending in China.
Fig. 1.
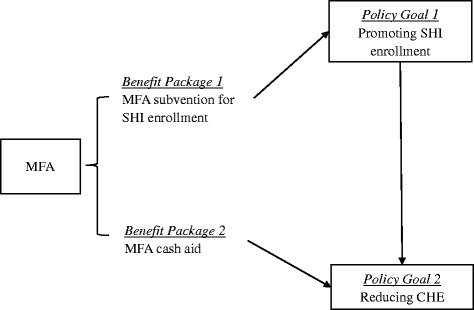
Conceptual framework
Methods
Data
The data were drawn from a nationally representative dataset collected for the study Evaluating Social Policy Supporting System for Vulnerable Families in Urban and Rural China (ESPSS) [49]. The Ministry of Civil Affairs of China launched the ESPSS in 2008 and undertook a program of annual surveys starting in 2012. The data used in this study were collected in 2014.
The ESPSS used a multistage cluster sampling method based on the sampling frame of the Sixth National Population Census of China in 2010. In the first stage, 1500 villages in rural areas and neighborhoods in urban areas were randomly drawn from 29 provinces (Xinjiang, Tibet, Hong Kong, and Macau were not included). In the second stage, seven low-income households were selected from each village and 12 from each neighborhood using quota sampling. Low-income families in the ESPSS data included households enrolled in the MLSS, extremely poor households, households that had made applications for the MLSS (including households that had dropped out of the MLSS), low-income families not enrolled in the MLSS (identified by local government in some provinces), and low-income immigrant households. An official letter about the survey was issued by the Ministry of Civil Affairs to local county-level Bureaus of Civil Affairs to facilitate the collection of information from vulnerable households with the help of local village or neighborhood committees. In 2014, a total of 14,179 low-income families were surveyed, with a response rate of 83%. This study used the information for 11,570 households (7290 urban households and 4280 rural households), excluding 2609 immigrant households.
To answer our study questions, we extracted three sets of subsamples: (1) the Q1 sample for estimating the association between MFA subvention and SHI enrollment. We only used data from households that were either fully enrolled in SHI or uninsured to identify the link; (2) the Q2 sample for examining the association between MFA cash aid and CHE. The MFA provides cash aid to low-income households where the OPE must exceed a county-specific threshold. We therefore only used data from households eligible for MFA cash aid. The detailed strategies on how the threshold was constructed in each county are in Additional file 1: Supplementary Text; and (3) the Q3 sample for estimating the association between SHI enrollment and CHE, which used data from all households in the ESPSS dataset. The final sample size was 9537 households for the Q1 sample, 1521 households for the Q2 sample, and 11,570 households for the Q3 sample.
Measurement
Dependent variables
To evaluate the association between MFA subvention and household SHI enrollment, we used a dummy variable for household SHI enrollment (0 = no SHI enrollment; 1 = full SHI enrollment). To assess the association between MFA cash aid or SHI enrollment and household CHE, we measured CHE using households’ annual OPE data. The ESPSS asked each household to report annual OPE for all its members. It also included questions about households’ total spending, food spending, and household size in 2014. Using the WHO’s approach [4], this study defined a household as having CHE if its annual OPE exceeded 40% of its annual capacity to pay. We measured capacity to pay by subtracting spending on basic subsistence needs from total household expenditure. We calculated basic subsistence needs as the average annual food expenditure of households where food shares were in the 45th and 55th percentiles. We assigned the value “1″ to CHE if the ratio of a household’s annual total OPE to its capacity to pay was 0.4 or above, and “0″ otherwise.
Independent variables
To evaluate the association between MFA subvention and household SHI enrollment, we used two dummy variables: full MFA subvention (0 = no MFA subvention; 1 = full MFA subvention) and partial MFA subvention (0 = no MFA subvention; 1 = partial MFA subvention). To examine the association between MFA cash aid and CHE, we used a dummy variable for MFA cash aid (0 = no MFA cash aid; 1 = MFA cash aid). In addition, to assess the association between household SHI enrollment and CHE, we used two dummy variables: full SHI enrollment (0 = no SHI enrollment; 1 = full SHI enrollment) and partial SHI enrollment (0 = no SHI enrollment; 1 = partial SHI enrollment).
Other covariates
First, household total medical costs: according to the policy design of the MFA, cash aid is provided only if the OPE or total medical costs of a low-income household exceed the threshold of MFA cash aid, indicating that total medical costs affect the provision of MFA cash aid. In addition, high total medical costs increase the possibility of high OPE and CHE when there is a lack of protection from the social welfare system [50]. Second, health care needs: health care needs may confound the relationship between the MFA/SHI and CHE. We included the number of older adults (aged 65 and older) and the number of children (under five years old), the adjusted health score for household members, the number of people with chronic illnesses, the number of people with serious illnesses, and the number of people needing long-term care. The ESPSS asked the head of each household to report on each members’ health status using a 5-point Likert scale (1 = very good, 2 = good, 3 = normal, 4 = bad, and 5 = very bad). We constructed a variable representing a household’s health score by adding the points from all members in the household. We then regressed the household health score on household’s number of older adults, number of children, number of people with chronic illnesses, and number of people with serious illnesses [51]. We divided the predicted health score by household size to obtain the adjusted household health score. Third, socioeconomic strata variables: socioeconomic strata here involved three dimensions: income, education, and occupation. The ESPSS asked the head of each household to report total household income for the previous year. We used per capita household income, dividing total household income by household size [52]. We also used the number of unemployed and the number of household members with a high school education and above. Fourth, demographic variables: we included urban status (0 = living in rural areas; 1 = living in urban areas) and the number of male members. Summary statistics of these variables are presented in Table 2.
Table 2.
Summary statistics of variables used in the three multilevel logistic models
| Q1 sample | Q2 sample | Q3 sample | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | N | Mean | SD | |
| CHE | 9389 | 0.50 | 0.50 | 1502 | 0.69 | 0.46 | 11,386 | 0.49 | 0.50 |
| Household SHI enrollment | |||||||||
| No SHI enrollment | 9521 | 0.28 | 0.45 | - | - | - | 11,554 | 0.23 | 0.42 |
| Partial SHI enrollment | - | - | - | - | - | - | 11,554 | 0.18 | 0.38 |
| Full SHI enrollment | 9521 | 0.72 | 0.45 | - | - | - | 11,554 | 0.59 | 0.49 |
| MFA cash aid | 9525 | 0.23 | 0.42 | 1509 | 0.45 | 0.50 | - | - | - |
| MFA subvention for SHI enrollment | |||||||||
| No subvention | 8527 | 0.50 | 0.50 | - | - | - | - | - | - |
| Partial subvention | 8527 | 0.25 | 0.43 | - | - | - | - | - | - |
| Full subvention | 8527 | 0.25 | 0.43 | - | - | - | - | - | - |
| Log (total medical cost) | 8536 | 7.03 | 1.67 | 1521 | 8.19 | 1.08 | 10,442 | 7.08 | 1.68 |
| Urban | 9537 | 0.61 | 0.49 | 1521 | 0.63 | 0.48 | 11,570 | 0.63 | 0.48 |
| Number of males | 9537 | 1.47 | 0.91 | 1521 | 1.64 | 0.95 | 11,570 | 1.52 | 0.92 |
| Number of older adults | 9537 | 0.56 | 0.75 | 1521 | 0.65 | 0.82 | 11,570 | 0.56 | 0.75 |
| Number of children | 9537 | 0.08 | 0.31 | 1521 | 0.10 | 0.34 | 11,570 | 0.09 | 0.33 |
| Adjusted household health score | 9520 | 3.78 | 2.06 | 1519 | 3.92 | 1.93 | 11,551 | 3.59 | 1.96 |
| Number of people with chronic illness | 9525 | 0.76 | 0.82 | 1519 | 0.78 | 0.87 | 11,557 | 0.78 | 0.83 |
| Number of people with serious illness | 9530 | 0.28 | 0.52 | 1521 | 1.14 | 0.38 | 11,562 | 0.30 | 0.54 |
| Number of people needing long-term care | 9535 | 0.42 | 0.64 | 1521 | 0.70 | 0.71 | 11,568 | 0.44 | 0.65 |
| Number of people with high school education and above | 9537 | 0.52 | 0.83 | 1521 | 0.64 | 0.89 | 11,570 | 0.60 | 0.88 |
| Number of unemployed | 9537 | 0.78 | 0.82 | 1521 | 1.02 | 0.85 | 11,570 | 0.80 | 0.82 |
| Log (per capita household income) | 9537 | 4.11 | 8.29 | 1521 | 4.20 | 8.18 | 11,570 | 4.28 | 8.09 |
The Q1 sample was used to assess the association between MFA subvention for SHI enrollment and SHI enrollment (Eq. 1); the Q2 sample was used to examine the association between MFA cash aid and CHE after addressing self-selection bias (Eq. 2); and the Q3 sample was used to analyze the association between SHI enrollment and CHE (Eq. 3)
We converted the value of all expenditure- and cost-related items to the value of the Chinese yuan in 2014 [53]. Next, we transformed the unit of expenditures and costs from Chinese yuan to US dollars, using the 2014 exchange rate of 6.143 [54]. In addition, we took the logarithm on all expenditure- and cost-related variables to render positively skewed distributions normal and to increase the efficiency of the analysis. To families with no medical expenditure (medical expenditure = 0) we assigned an extremely small value, 10−10, to facilitate log transformation. Out of 11,570 observations, data for 0.90% of households’ expenditure, 2.43% of households’ food expenditure, and 0.30% of households’ income were missing. We used regression imputation to address the issue of missing data [55, 56]. We regressed these expenditure variables on all independent variables having high correlations with them in a correlation matrix and then replaced the missing values with predictive values.
Statistical analysis
Using the full sample, we first reported on the percentage of low-income households enrolled in SHI programs and those receiving the MFA subvention, respectively in rural and urban areas. We then described the percentage of households with CHE by household MFA cash aid and SHI enrollment status, respectively across provinces. We also demonstrated the percentage of households receiving MFA cash aid in rural and urban areas.
A multilevel random intercepts model was used to control for potential clustering effects at provincial and county levels [57]. Three log binominal regressions were fitted for the two binary dependent variables, household SHI enrollment and household CHE status, as follows:
| 1 |
| 2 |
| 3 |
where Logit(SHIenrol ijk) represents the probability of full enrollment in SHI programs by all household members of the ith household in the jth county and kth province; Logit(CHE ijk) represents the probability of CHE for the ith household in the jth county and kth province; FullMFAsub ijk, PartMFAsub ijk, MFAcash ijk , FullSHIenrol ijk, and PartSHIenrol ijk represent, respectively, full MFA subvention for SHI enrollment, partial MFA subvention for SHI enrollment, MFA cash aid, full SHI enrollment, and partial SHI enrollment for the ith household in the jth county and kth province; β 13, β 22, and β 33 are vectors of the coefficients for X ijk, which is a vector of covariates on household characteristics for the ith household in the jth county and kth province; and ν 10k/ ν 20k/ ν 30k and μ 10jk/ μ 20jk/ μ 30jk represent between-province random variation and between-county/within-province random variation, respectively.
Total medical cost was controlled for in Eqs 2 and 3 because it may be correlated with SHI enrollment, eligibility for MFA cash aid, and CHE status. It was not included in Eq. 1. In addition, Eq. 1 was estimated with the Q1 sample, the Q2 sample was used for estimating Eq. 2, and the Q3 sample, for Eq. 3.
To test the sensitivity of the results, we used propensity score matching to analyze whether the two groups – the treatment group (receiving MFA cash aid) and control group (not receiving MFA cash aid) – differed significantly in the likelihood of CHE (see Additional file 1: Table S5) [58]. To capture the different scenarios between urban and rural areas, we conducted additional analyses on all descriptive and inferential statistics for urban and rural samples, respectively (see Additional file 1: Tables S2, S3, and S4). Given the high regional variation in economic development found in China, we also explored the impact of region (eastern, central, western, and northeastern regions) on the associations between MFA subvention and SHI enrollment, SHI enrollment and CHE, and MFA cash aid and CHE by including an interaction between region and main independent variables in various models (see Additional file 1: Tables S6 and S7).
Results
The role of MFA subvention for SHI enrollment
Figure 2 presents SHI enrollment and MFA subvention among low-income households in China. It shows that 23.4% of low-income households (22.0% of rural households and 24.3% of urban households) reported no family members enrolled in SHI programs; 49.9% of low-income households (55.6% of rural households and 46.2% of urban households) received no MFA subvention for SHI enrollment, despite being eligible.
Fig. 2.
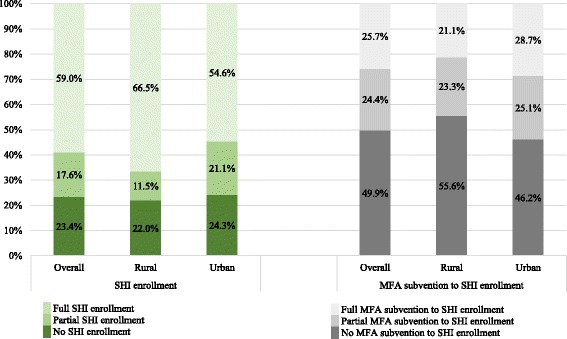
SHI enrollment and MFA subvention for SHI enrollment among low-income households in China
Table 3 shows the association between MFA subvention for SHI enrollment and household SHI enrollment using the Q1 sample. The model fit the data well, with Wald chi2 equal to 258.82 (p < 0.001). The results show that MFA subvention for SHI enrollment had no significant association with household SHI enrollment (for partial subvention, OR = 1.015, 95% CI = 0.756–1.364; for full subvention, OR = 1.174, 95% CI = 0.990–1.392). Among other covariates, a household with more members with chronic or serious illnesses and a higher household income was more likely to participate in SHI programs than one with fewer members with chronic or serious conditions and a lower household income. Additional file 1: Table S3 shows that MFA subvention for SHI enrollment had no significant association with household SHI enrollment in either rural or urban areas, except for a significantly positive association between full MFA subvention for SHI enrollment and SHI enrollment in rural areas. Additional file 1: Table S7 indicates no significant association between MFA subvention for SHI enrollment and SHI enrollment across all regions, except for a significantly positive association between full MFA subvention for SHI enrollment and SHI enrollment in the northeastern region.
Table 3.
Results of multilevel logistic analysis using the Q1 sample: MFA subvention for SHI enrollment and SHI enrollment
| Household SHI enrollment (1 = all enrolled; 0 = none enrolled) | Q1 sample (N = 8498; Province Group = 29; County Group = 159) | |
|---|---|---|
| OR | 95% CI | |
| MFA subvention for SHI enrollment | ||
| No subvention (reference) | reference | |
| Partial subvention | 1.015 | (0.756, 1.364) |
| Full subvention | 1.174 | (0.990, 1.392) |
| Urban | 0.911 | (0.601, 1.382) |
| Number of males | 0.959 | (0.819, 1.123) |
| Number of older adults | 1.134 | (0.979, 1.315) |
| Number of children | 0.951 | (0.712, 1.270) |
| Adjusted household health score | 0.997 | (0.957, 1.040) |
| Number of people with chronic illnesses | 1.470*** | (1.278, 1.690) |
| Number of people with serious illnesses | 1.265* | (1.049, 1.526) |
| Number of people needing long-term care | 0.999 | (0.856, 1.164) |
| Number of people with high school education and above | 1.051 | (0.930, 1.188) |
| Number of unemployed | 0.905 | (0.793, 1.033) |
| Log (per capita household income) | 1.025*** | (1.014, 1.037) |
OR odds ratio, CI confidence interval, SHI social health insurance, MFA Medical Financial Assistance; * = p < 0.05; ** = p < 0.01; *** = p < 0.001
The role of MFA cash aid and SHI enrollment
Figure 3 shows the percentage of low-income households with CHE in 2014. Overall, 49.3% of low-income households had CHE status. CHE was more likely to occur among low-income households receiving MFA cash aid (62.7%) and those with full SHI enrollment (51.9%). Additional file 1: Fig. S1 shows the distribution of CHE in urban and rural areas. In general, more rural low-income households had CHE than urban households.
Fig. 3.
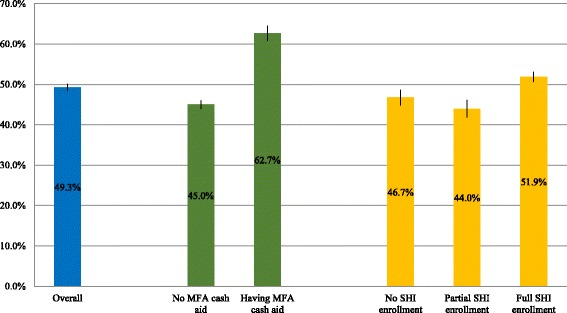
Percentage of low-income households with CHE, by MFA cash aid status and SHI enrollment status
Figure 4 shows CHE across China’s provinces in 2014. Heilongjiang, Jilin, Hebei, Henan, Shandong, Chongqing, Hunan, Yunnan, and Qinghai had the highest percentages of low-income households with CHE at over 54.0%.
Fig. 4.
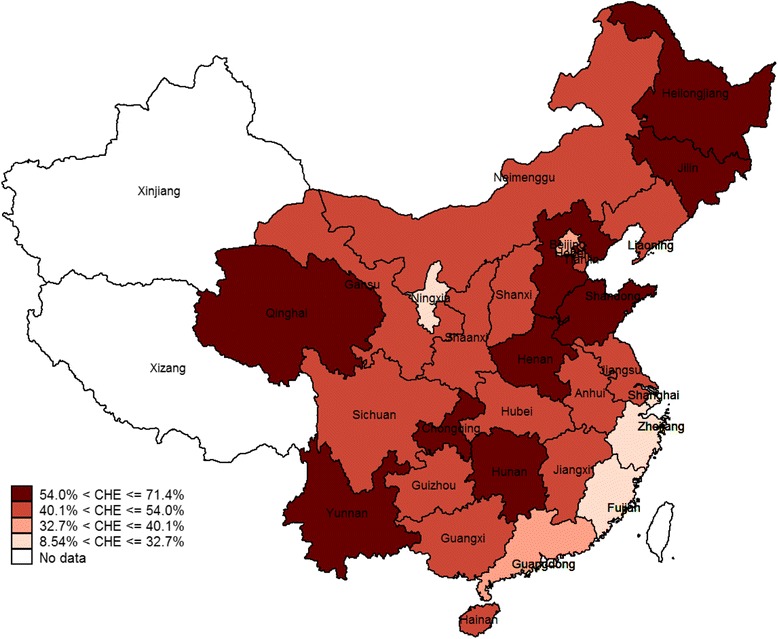
Percentage of low-income households with CHE across provinces in China
Figure 5 shows the data relating to MFA cash aid: 24.1% of low-income households received cash aid, with no significant difference between rural (23.8%) and urban (24.2%) areas.
Fig. 5.
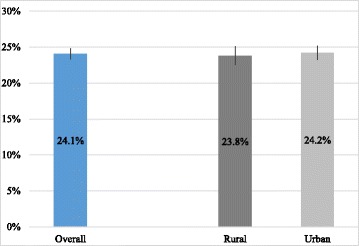
Percentage of low-income households receiving MFA cash aid in rural and urban China
Table 4 presents the associations between between MFA cash aid and CHE, and household SHI enrollment and CHE. Both models fit the data well, with Wald chi2 equal to 787.51 (p < 0.001) for the MFA cash aid model and 3402.95 (Prob > chi2 = 0.000) for the SHI enrollment model.
Table 4.
Results of multilevel logistic analysis: MFA cash aid and CHE using the Q2 sample; SHI enrollment and CHE using the Q3 sample
| CHE (1 = with CHE; 0 = no CHE) | Q2 sample (N = 1490; Province Group = 28; County Group = 135) | Q3 sample (N = 10,344; Province Group = 29; County Group = 158) | ||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Household SHI enrollment | ||||
| No participation | - | reference | ||
| Partial participation | - | 0.843 | (0.693, 1.025) | |
| Full participation | - | 0.760** | (0.626, 0.924) | |
| MFA cash aid | 1.009 | (0.744, 1.367) | - | |
| Log (total medical cost) | 2.774*** | (2.364, 3.256) | 2.172*** | (2.026, 2.328) |
| Urban | 0.723 | (0.449, 1.163) | 0.620*** | (0.474, 0.811) |
| Number of males | 0.942 | (0.808, 1.099) | 0.969 | (0.910, 1.031) |
| Number of older adults | 0.896 | (0.737, 1.088) | 1.173*** | (1.077, 1.276) |
| Number of children | 0.655** | (0.484, 0.886) | 0.806*** | (0.718, 0.905) |
| Adjusted household health score | 1.217** | (1.065, 1.392) | 1.358*** | (1.310, 1.407) |
| Number of people with chronic illnesses | 0.827* | (0.692, 0.988) | 0.864** | (0.791, 0.945) |
| Number of people with serious illnesses | 1.201 | (0.909, 1.587) | 0.925 | (0.813, 1.053) |
| Number of people needing long-term care | 0.916 | (0.741, 1.133) | 0.989 | (0.924, 1.060) |
| Number of people with high school education and above | 0.725** | (0.598, 0.878) | 0.660*** | (0.610, 0.714) |
| Number of unemployed | 1.253** | (1.070, 1.467) | 1.291*** | (1.184, 1.406) |
| Log (per capita household income) | 0.984 | (0.966, 1.003) | 0.986** | (0.977, 0.996) |
OR odds ratio, CI confidence interval, SHI social health insurance, MFA Medical Financial Assistance, CHE catastrophic health expenditure; * = p < 0.05; ** = p < 0.01; *** = p < 0.001
We detected no significant association between MFA cash aid and CHE (OR = 1.009; 95% CI = 0.744–1.367). Among the covariates, higher total medical costs, worse health status, and the number of unemployed household members were significantly associated with a higher likelihood of CHE. Having more children, more members with chronic conditions, and more members with a high school education and above were inversely associated with the likelihood of CHE. Comparable results were obtained when testing the sensitivity of the results using the propensity score matching model, where the association between MFA cash aid and CHE was also statistically insignificant (see Additional file 1: Table S5). Additional file 1: Table S4 shows that no significant association was found between MFA cash aid and CHE in either rural or urban areas. Additional file 1: Table S7 shows no significant association between MFA cash aid and CHE in any of the four regions.
Regarding the association between SHI enrollment and CHE, when controlling for total medical costs and other covariates, full SHI enrollment was significantly associated with lower likelihood of CHE (OR = 0.760, 95% CI = 0.626–0.924). A household with all members enrolled in SHI programs was 24.0% less likely to have CHE. Among other covariates, the likelihood of CHE increased with total medical cost, the number of older adults, worse health status, and the number of unemployed members; and decreased with living in urban areas, the number of children, the number of members with chronic illnesses, the number of members with high school education and above, and higher household income. Additional file 1: Table S4 shows that SHI enrollment had no significant association with CHE in rural areas, but had a significantly negative association with CHE in urban areas. Additional file 1: Table S7 shows that full SHI enrollment had a significantly negative association with CHE in eastern and central regions.
Discussion
Using data from a 2014 nationally representative database, this study found that about one quarter of low-income households were not enrolled in SHI programs and nearly half of those households did not receive MFA subventions for SHI enrollment. In addition, over half of the low-income households suffered from catastrophic health spending, while only a quarter of them received MFA cash aid. A three-level logistic analysis revealed that MFA subvention had no significant association with SHI enrollment in low-income households, that MFA cash aid had no significant association with the CHE status of low-income households, and that household SHI enrollment played an important role in reducing households’ catastrophic health spending.
The findings reveal the limited role of the MFA subsidy in encouraging low-income households to enroll in SHI programs and mitigating the financial risks of illness. The findings agree with previous studies that have found no significant association between a special MFA benefit package and the presence of substantial medical debt in rural areas of Chongqing Municipality [39], low coverage of enrollment and benefit levels of the MFA in four counties in Hubei Province and Sichuan Province [42], and a minor relationship between MFA cash aid and the financial burden of urban low-income households in the three counties of Hebei Province, Hubei Province, and Chongqing Municipality [48].
The non-significant association between MFA subvention and SHI enrollment could be due to limited eligibility and funding for a MFA subvention. As Additional file 1: Table S1 shows, in many localities, a MFA subvention for SHI enrollment is only provided to the extremely poor. Even if a poor household receives a MFA subvention for SHI enrollment, it may choose not to participate in SHI programs if the subvention funds cannot cover the total cost of the SHI premium. In addition, the MFA subvention for SHI enrollment is provided to households in cash, which allows them to use it for other purposes, such as buying food. This may be a key reason that a quarter of low-income households were not enrolled in SHI programs.
We have observed no significant association between MFA cash aid and CHE. There are two plausible explanations. First, the cash aid is mainly funded by local government and its threshold and ceiling of reimbursement are directly impacted by the local governments’ fiscal capacity. If a local government has a restricted budget, the MFA cash aid may have high thresholds and low ceilings for reimbursement. This may also explain why only a quarter of low-income households received MFA cash aid. Taking Shandong Province as an example, the threshold for MFA cash aid was USD163 for outpatient services (see Additional file 1: Table S1). The average cost of outpatient services was USD35 per visit in 2014, suggesting a large gap between the threshold of the MFA and the average cost of medical services [59]. Second, in many areas, MFA cash aid covers the cost of limited kinds of serious illnesses, as shown in Additional file 1: Table S1.
This study advocates the establishment of a “pro-poor” medical financial assistance policy in China that can respond to the international trend of investing in health as a major avenue towards poverty alleviation [60]. China has made remarkable progress in enacting and legislating the MFA program, extending coverage, and improving funding management [40, 41]. Further efforts should be devoted to at least two aspects: (1) ensuring low-income households’ enrollment in SHI programs. In this study, SHI has been found to be an efficient institution for mitigating catastrophe. The government may consider free SHI enrollment for all types of low-income households, rather than just providing subsidies for enrollment; (2) increasing the benefit package of MFA cash aid by reducing its threshold and expanding coverage to more serious diseases. At present, it is too small to alleviate catastrophic health spending in low-income households. Increasing funds for MFA cash aid could construct an effective safety net for the poor.
Our study has the following limitations. Firstly, the data in this study was extracted from one cross-sectional survey, with the result that is not possible to assess causal relationships. Secondly, the health spending data used were collected through a self-reported survey, that may not accurately reflect medical costs.
As the MFA, together with SHI programs, will continue to be major measures for financial risk protection in low-income households, future studies should focus on examining the causal effects of various policy components of MFA subvention and cash aid, respectively on SHI enrollment and financial risk protection using longitudinal data. For example, this study identified no significant association between MFA cash aid and CHE. Could this lack of a significant association be caused by high thresholds, low cash aid, or low ceilings for the cash aid? Future studies on this question may enable policy makers to make accurate adjustments to MFA benefit packages.
Conclusions
This study suggests that the MFA is not currently an effective supplement in terms of either subsidizing SHI enrollment or preventing financial risks through providing cash aid. As a result, it is neither a useful buffer in the cycle between poverty and poor health, nor a “pro-poor” health policy in the model advocated by the World Health Organization [18]. Compared with the poor performance of the MFA, SHI programs, with nearly nationwide coverage, play an important role in alleviating the health spending-related impoverishment experienced by low-income households.
Acknowledgements
None.
Funding
This study was supported by the National Social Science Foundation of China (16CSH032). The funding body had no role in the design or conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Availability of data and materials
The dataset supporting the conclusions of this article was acquired from the Ministry of Civil Affairs of China on the agreement that it be used prudently.
Abbreviations
- CHE
Catastrophic health expenditure
- CI
Confidence Interval
- ESPSS
Evaluating social policy supporting system for vulnerable families in Urban and Rural China
- MFA
Medical Financial Assistance
- N
Sample size
- OPE
Out-of-pocket health expenditure
- OR
Odds ratio
- SHI
Social Health Insurance
- WHO
World Health Organization
Additional file
Table S1. Eligibility and benefit package of the Medical Financial Assistance program across provinces in China. Supplementary Text. Fig. S1 Percentage of low-income households having the CHE, by urban/rural, MFA cash aid status and SHI status. Table S2 Summary of variables used in the three multilevel logistical models in rural and urban areas. Table S3 Results of multilevel logistic analysis in rural and urban areas: MFA subvention and SHI enrollment using the Q1 sample. Table S4 Results of multilevel logistic analysis by rural and urban areas: MFA cash aid and the CHE; and SHI enrollment and the CHE. Table S5 Results of propensity score matching analysis using the Q2 sample: Average treatment effects on the treated (ATT) for treatment of CHE. Table S6 Summary of variables used in multilevel logistic models including the interaction between main independent variables and regions. Table S7 Results of multilevel logistic models including the interaction between main independent variables and regions. (DOCX 64 kb)
Authors’ contributions
KL conceived and oversaw the study. JY analyzed the data under KL and CL’s supervision. KL and JY wrote the first draft of the paper. All authors were involved with data interpretation and manuscript writing, and approved the final version.
Ethics approval and consent to participate
The Ethics Committee of Renmin University of China approved this study’s protocol and analytical tools. The data used in this study were from a secondary dataset the ESPSS, which had acquired the consent of all individuals who participated in the survey process.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1186/s12939-017-0638-3) contains supplementary material, which is available to authorized users.
Contributor Information
Kai Liu, Phone: 86-10-61510320, Email: liuk@ruc.edu.cn.
Jing Yang, Email: jyang8711@gmail.com.
Chunling Lu, Email: chunling_lu@hms.harvard.edu.
References
- 1.The World Bank. World development report 2000/2001: attacking poverty. Oxford: Oxford University Press; 2001.
- 2.The World Health Organization. The world health report 2010. Health systems financing: the path to universal coverage. Geneva: The World Health Organization; 2010. [DOI] [PMC free article] [PubMed]
- 3.Wagstaff A. Poverty and health sector inequalities. B World Health Organ. 2002;80(2):97–105. [PMC free article] [PubMed] [Google Scholar]
- 4.Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJ. Household catastrophic health expenditure: a multicounty analysis. Lancet. 2003;362(9378):111–117. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- 5.Xu K, Evans DB, Carrin G, et al. Protecting households from catastrophic health spending. Health Aff (Millwood) 2007;26(4):972–983. doi: 10.1377/hlthaff.26.4.972. [DOI] [PubMed] [Google Scholar]
- 6.Wagstaff A, Van Doorslaer E. Catastrophe and impoverishment in paying for health care: with applications to Vietnam 1993–1998. J Health Econ. 2003;12(11):921–933. doi: 10.1002/hec.776. [DOI] [PubMed] [Google Scholar]
- 7.Van Doorslaer E, O’Donnell O, Rannan-Eliya RP, et al. Catastrophic payments for health care in Asia. J Health Econ. 2007;16(11):1159–1184. doi: 10.1002/hec.1209. [DOI] [PubMed] [Google Scholar]
- 8.Wagstaff A, Lindelow M. Can insurance increase financial risk? The curious case of health insurance in China. J Health Econ. 2008;27(4):990–1005. doi: 10.1016/j.jhealeco.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Meng Q, Xu L, Zhang Y, et al. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet. 2012;379(9818):805–814. doi: 10.1016/S0140-6736(12)60278-5. [DOI] [PubMed] [Google Scholar]
- 10.Lu C, Liu Y, Shen J. Does China’s rural cooperative medical system achieve its goals? Evidence from the China health surveillance baseline survey in 2001. Contemp Econ Policy. 2012;30(1):93–112. doi: 10.1111/j.1465-7287.2011.00252.x. [DOI] [Google Scholar]
- 11.Li Y, Wu Q, Ling X, et al. Factors affecting catastrophic health expenditure and impoverishment from medical expenses in China: policy implications of universal health insurance. B World Health Organ. 2012;90(9):664–671. doi: 10.2471/BLT.12.102178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shi W, Chongsuvivatwong V, Geater A, et al. Effect of household and village characteristics on financial catastrophe and impoverishment due to health care spending in western and central rural China: a multilevel analysis. Health Res Policy Syst. 2011;9(1):16. doi: 10.1186/1478-4505-9-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sun X, Jackson S, Carmichael G, et al. Catastrophic medical payment and financial protection in rural China: evidence from the new cooperative medical scheme in medical scheme in Shandong province. Health Econ. 2009;18(1):103–119. doi: 10.1002/hec.1346. [DOI] [PubMed] [Google Scholar]
- 14.Ma J, Xu J, Zhang Z, Wang J. New cooperative medical scheme decreased financial burden but expanded the gap of income-related inequity: evidence from three provinces in rural China. Int J Equity Health. 2016;15:72. doi: 10.1186/s12939-016-0361-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu Y, Rao K, Hsiao WC. Medical expenditure and rural impoverishment in China. J Health Popul Nutr. 2003;21(3):216–222. [PubMed] [Google Scholar]
- 16.Zhang L, Cheng X, Tolhurst R, Tang S, Liu X. How effectively can the new cooperative medical scheme reduce catastrophic health expenditure for the poor and non-poor in rural China? Tropical Med Int Health. 2010;15(4):468–475. doi: 10.1111/j.1365-3156.2010.02469.x. [DOI] [PubMed] [Google Scholar]
- 17.Suhrcke M, McKee M, Rocco L. Health investment benefits economic development. Lancet. 2007;370(9597):1467–1468. doi: 10.1016/S0140-6736(07)61616-X. [DOI] [PubMed] [Google Scholar]
- 18.The World Health Organization. Health and development. http://www.who.int/hdp/poverty/en/. Accessed 4 May 2016.
- 19.Normand C, Weber A. Social health insurance: a guidebook for planning. 2. Geneva: World Health Organization; 2009. [Google Scholar]
- 20.Hsiao WC, Shaw RP. Introduction, context, and theory. In: Hsiao WC, Shaw RP, editors. Social health insurance for developing nations. Washington, DC: The World Bank; 2007. pp. 1–20. [Google Scholar]
- 21.Hou X, Chao S. An evaluation of the initial impact of the medical assistance program in Georgia. Washington DC: The World Bank; 2008. [Google Scholar]
- 22.Stierle F, Kaddar M, Tchicaya A, Schmidt-Ehry B. Indigence and access to health care in sub-Saharan Africa. Int J Health Plann Manag. 1999;14(2):81–105. doi: 10.1002/(SICI)1099-1751(199904/06)14:2<81::AID-HPM543>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 23.Erus B, Yakut-Cakar B, Cali S, Adaman F. Health policy for the poor: an exploration on the take-up of means-tested health benefits in Turkey. Soc Sci Med. 2015;130:99–106. doi: 10.1016/j.socscimed.2015.02.015. [DOI] [PubMed] [Google Scholar]
- 24.Quayyum Z, Nadjib M, Ensor T, Sucahya PK. Expenditure on obstetric care and the protective effect of insurance on the poor: lessons from two Indonesian districts. Health Policy Plan. 2010;25(3):237–247. doi: 10.1093/heapol/czp060. [DOI] [PubMed] [Google Scholar]
- 25.Trujillo AJ, Portillo JE, Vernon JA. The impact of subsidized health insurance for the poor evaluating the Colombian experience using propensity score matching. Int J Health Care Finance Econ. 2005;5(3):211–239. doi: 10.1007/s10754-005-1792-5. [DOI] [PubMed] [Google Scholar]
- 26.Knaul FM, Arreola-Ornelas H, Mendez-Carniado O, et al. Evidence is good for your health system policy reform to remedy catastrophic and impoverishing health spending in Mexico. Lancet. 2006;368(9549):1828–1841. doi: 10.1016/S0140-6736(06)69565-2. [DOI] [PubMed] [Google Scholar]
- 27.Habib SS, Pervee S, Khuwaja HMA. The role of micro health insurance in providing financial risk protection. BMC Public Health. 2016;16:281. doi: 10.1186/s12889-016-2937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ranson MK. Reduction of catastrophic health care expenditures by a community-based health insurance scheme in Gujarat, India: current experiences and challenges. B World Health Organ. 2002;80(8):613–621. [PMC free article] [PubMed] [Google Scholar]
- 29.Devadasan N, Seshadri T, Trivedi M, Criel B. Promoting universal financial protection: evidence from the Rashtriya Swasthya Bima Yojana (RSBY) in Gujarat, India. Health Res Policy Syst. 2013;11:29. doi: 10.1186/1478-4505-11-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lu C, Chin B, Lewandowski JL, et al. Towards university health coverage: an evaluation of Rwanda Mutuelles in its first eight years. PLoS One. 2012;7:e39282. doi: 10.1371/journal.pone.0039282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alkenbrack S, Lindelow M. The impact of community-based health insurance on utilization and out-of-pocket expenditures in Lao People’s Democratic Republic. Health Econ. 2015;24(4):379–399. doi: 10.1002/hec.3023. [DOI] [PubMed] [Google Scholar]
- 32.Axelson H, Bales S, Minh PD, Ekman B, Gerdtham U. Health financing for the poor produces promising short-term effects on utilization and out-of-pocket expenditure in Vietnam. Int J Equity Health. 2009;8:20. doi: 10.1186/1475-9276-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jutting JP. Do community-based health insurance schemes improve poor people’s access to health care evidence from rural Senegal. World Dev. 2004;32(2):273–288. doi: 10.1016/j.worlddev.2003.10.001. [DOI] [Google Scholar]
- 34.Yip WC, Hsiao WC, Chen W, Hu S, Ma J, Maynard A. Early appraisal of China’s huge and complex health-care reforms. Lancet. 2012;379(9818):833–842. doi: 10.1016/S0140-6736(11)61880-1. [DOI] [PubMed] [Google Scholar]
- 35.Ngok K. Social assistance policy and its impact on social development in China: the case of the minimum living standard scheme. China Soc Work. 2010;3(1):35–52. doi: 10.1080/17525090903560606. [DOI] [Google Scholar]
- 36.The State Council General Office of China. Notification on forwarding the Ministry of Civil Affairs’ opinions on improving the Medical Financial Assistance Scheme for serious illness. Beijing: The State Council General Office of China; 2015. http://www.gov.cn/zhengce/content/2015-04/30/content_9683.htm (in Chinese). Accessed 4 May 2016.
- 37.The Ministry of Civil Affairs, The Ministry of Health, and The Ministry of Finance. Opinions on implementing rural Medical Financial Assistance. Beijing: The Ministry of Civil Affairs, The Ministry of Health, The Ministry of Finance; 2003. http://www.gov.cn/gongbao/content/2004/content_62870.htm (in Chinese). Accessed 4 May 2016.
- 38.The State Council General Office of China. Opinions on establishing pilots of urban Medical Financial Assistance Scheme. Beijing: The State Council General Office of China; 2005. http://www.gov.cn/gongbao/content/2005/content_63211.htm (in Chinese). Accessed 4 May 2016.
- 39.Hao Y, Wu Q, Zhang Z, et al. The impact of different benefit packages of medical financial assistance scheme on health service utilization of poor population in rural China. BMC Health Serv Res. 2010;10:170. doi: 10.1186/1472-6963-10-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.The State Council of China. Draft decree on the Social Assistance. Beijing: The State Council of China; 2014. http://www.gov.cn/flfg/2014-02/27/content_2624221.htm (in Chinese). Accessed 4 May 2016.
- 41.The Ministry of Finance and The Ministry of Civil Affairs. Decree on the fund management of urban and rural Medical Financial Assistance. Beijing: The Ministry of Finance, The Ministry of Civil Affairs; 2014. http://www.gov.cn/gzdt/2014-02/17/content_2610863.htm (in Chinese). Accessed 4 May 2016.
- 42.Ma X, Zhang J, Meessen B, Decoster K. Social health assistance schemes the case of medical financial assistance for the rural poor in four counties of China. Int J Equity Health. 2011;10:44. doi: 10.1186/1475-9276-10-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Filipski MJ, Zhang Y, Chen KZ. Making health insurance pro-poor: evidence from a household panel in rural China. BMC Health Serv Res. 2015;15:210. doi: 10.1186/s12913-015-0871-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu K, Wu Q, Liu J. Examining the association between social health insurance participation and patients’ out-of-pocket payments in China. Soc Sci Med. 2014;113:95–103. doi: 10.1016/j.socscimed.2014.05.011. [DOI] [PubMed] [Google Scholar]
- 45.Shi W, Chongsuvivatwong V, Geater A, Zhang J, Zhang H, Brombal D. The influence of the rural health security schemes on health utilization and household impoverishment in rural China: data from a household survey of western and central China. Int J Equity Health. 2010;9:7–17. doi: 10.1186/1475-9276-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang L, Sun X, Sleigh AC, Carmichael GA, Jackson S. Health payment-induced poverty under China's new cooperative medical scheme in rural Shandong. Health Policy Plan. 2010;25(5):419–426. doi: 10.1093/heapol/czq010. [DOI] [PubMed] [Google Scholar]
- 47.Yip W, Hsiao WC. Non-evidence-based policy: how effective is China's new cooperative medical scheme in reducing medical impoverishment? Soc Sci Med. 2009;68(2):201–209. doi: 10.1016/j.socscimed.2008.09.066. [DOI] [PubMed] [Google Scholar]
- 48.Fang LM, Qiao DP. The effect of the urban medical security system on the health care on the urban poor: based on the survey of the urban poor households in Bazhou, Chibi and Hechuan of China. J Financ Econ. 2012;38(11):103–113. [Google Scholar]
- 49.The Ministry of Civil Affairs Center of Policy Research . Evaluating social policy supporting system for vulnerable families in urban and rural China report. Beijing: China Society Press; 2011. [Google Scholar]
- 50.The World Health Organization. The world health report 2000. Health systems: improving performance. Geneva: The World Health Organization; 2000. http://www.who.int/whr/2000/en/whr00_en.pdf?ua=1. Accessed 4 May 2016.
- 51.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. doi: 10.2307/2955359. [DOI] [PubMed] [Google Scholar]
- 52.Stewart J. The MacArthur scale of social environment notebook. 2009. [Google Scholar]
- 53.The National Bureau of Statistics of China. China statistical yearbook 2014. Beijing: The National Bureau of Statistics of China; 2015. http://data.stats.gov.cn/easyquery.htm?cn=C01 (in Chinese). Accessed 20 Oct 2016.
- 54.The World Bank. Official exchange rate. Washington DC: The World Bank; 2014. http://data.worldbank.org/indicator/PA.NUS.FCRF?locations=CN&year_high_desc=false. Accessed 20 Oct 2016.
- 55.Royston P. Multiple imputation of missing values. Stata J. 2004;4(3):227–241. [Google Scholar]
- 56.Saunders J, Morrow-Howell N, Spitznagel E, Dork P, Proctor EK, Pescarino R. Imputing missing data: a comparison of methods for social work researchers. Soc Work Res. 2006;30(1):19–31. doi: 10.1093/swr/30.1.19. [DOI] [Google Scholar]
- 57.Goldstein H. Multilevel statistical models. 3. London: Arnold; 2003. [Google Scholar]
- 58.Guo S, Fraser WM. Propensity score analysis: statistical methods and applications. Thousand Oaks, CA: Sage Publications; 2014. [Google Scholar]
- 59.The Health and Family Planning Commission of Shandong Province. The Health and Family Planning Statistical Bulletin of Shandong Province 2014. http://www.sdwsjs.gov.cn/xwzx/ywsd/201508/t20150810_58723.html (in Chinese). Accessed 4 May 2016.
- 60.The World Health Organization. The world health report 1999. Making a difference. Geneva: The World Health Organization; 1999.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this article was acquired from the Ministry of Civil Affairs of China on the agreement that it be used prudently.


