Abstract
Objective
To describe the change in colposcopy volume in light of recent guideline shifts, which target higher-risk women while limiting unnecessary procedures in low-risk women.
Methods
After institutional review board approval, colposcopy clinic visits at a large-volume referral center from January 2010 to December 2015 were reviewed. All women diagnosed with abnormal cervical cytology who were referred and subsequently underwent colposcopic evaluation were included. Mean monthly and annual clinic volumes were calculated. Return visit proportions were compared using chi-square test. Negative binomial regression analysis was used to examine trends.
Results
There were a total of 8722 colposcopy clinic visits between January 2010 and December 2015. Approximately 7395 visits (85%) were new patient visits, and 1327 visits (15%) were return visits. The percentage of return visits declined dramatically during the study period from 22.9% (2011) of total visits to 9.0% in 2015 (P < 0.001). Annual clinic volume ranged from 903 to 1884 with a mean monthly volume of 121.13 visits (SD, 42.1). Annual volume was highest in 2011 (n = 1884) and has since demonstrated a steady decline. In 2015, average monthly volume (75.3 visits) dropped to nearly one third of its peak 218 visits per month in July 2010.
Conclusions
In a large referral clinic that adheres to guideline-based screening and management recommendations, monthly colposcopy volume has declined dramatically with a reduction by two thirds compared with peak volume in 2010.
Keywords: colposcopy, screening guidelines
Our knowledge and implementation of cervical cancer screening and colposcopy have undergone significant advances since their introduction in the 1940s. Screening guidelines and colposcopy practices are adjusted as our knowledge of cervical pathology and the natural history of the human papillomavirus (HPV) continues to expand.1 Although screening continues to be recommended for all women older than 21 years, our increasing knowledge in this field has facilitated a shift in guidelines toward less screening with longer intervals in low-risk women in an effort to reduce unnecessary morbidity.2–5
Major updates to guidelines have included the 2006 recommendation for conservative management of low-grade cytology in adolescents and pregnant women.3 Furthermore, in 2009, cytologic screening was no longer recommended for women younger than 21 years, and the interval for screening increased to every 2 years.3,4 More recently, in 2012, the recommended screening interval increased to every 3 years in low-risk women ages 21 to 29 years and every 5 years in women older than 30 years with both normal cytology and negative high-risk HPV testing. Cotesting for high-risk HPV types was also added to routine screening in women older than 30 years.2 In 2013, fewer colposcopies were recommended for women aged 21 to 24 years with low-grade cervical cytology. Specifically, where previous guidelines recommended colposcopic evaluation for atypical squamous cells of undetermined significance and low-grade squamous intraepithelial lesion cytology in these young 21- to 24-year-old women, guidelines now recommend repeating cytology in 1 year.5 These ongoing changes since 2006 all affect the frequency of follow-up and, thus, are likely to affect the number of colposcopic visits in the United States.
As updates to guidelines are trending toward less screening of low-risk women with longer intervals, it is imperative that we assess its potential effect on colposcopic volume as a decline in volume may have implications for the future practice of colposcopy. We conducted a retrospective, observational study of women referred to a large-volume university clinic for colposcopic evaluation, with the objective to evaluate clinic volume trends after recent updates to cervical cancer screening and colposcopy practice guidelines.
Methods
This retrospective study was carried out in accordance with the standards of the institutional review board at the University of Alabama at Birmingham (UAB). The UAB colposcopy clinic was selected for this study as it is a high-volume academic referral center, in which patients are referred from the state's county health departments, which follow the US Preventive Services Task Force guidelines.5 Patients are managed strictly by evidence-based guidelines from the American Society for Colposcopy and Cervical Pathology. Changes to guidelines are implemented into clinical practice at our clinic immediately after their public release.
Subjects were identified through the UAB colposcopy clinic database, which includes all encounters at the colposcopy clinic. Eligible subjects included women with abnormal cervical cytology who were referred and subsequently underwent colposcopic evaluation between January 2010 and December 2015. This time frame was chosen to specifically evaluate the potential effects of new guidelines during this era, which extended screening intervals and allowed for conservative management of low-grade cytology in young women.2–5 Visits were queried and subdivided into new versus return patient visits. Mean monthly and annual clinic volumes were calculated. The proportions of yearly return visits were calculated. Comparisons were made using chi-square test. Initially, a Poisson regression model was constructed, with the number of patient visits as a dependent variable and the months and before and after guideline status as independent variables.6 Poisson regression model for patient volume was rejected in favor of a negative binomial regression model using Akaike information criterion values because of model-fit related to overdispersion. The Akaike information criterion value for the negative binomial (700.5) was lower than the Poisson model (996.9), indicating negative binomial is a better model. Figure 2 represents 2 trends: the 26-month period before and the 46-month period after the guideline release date (using March 2012 as a cutoff ).
Figure 2.
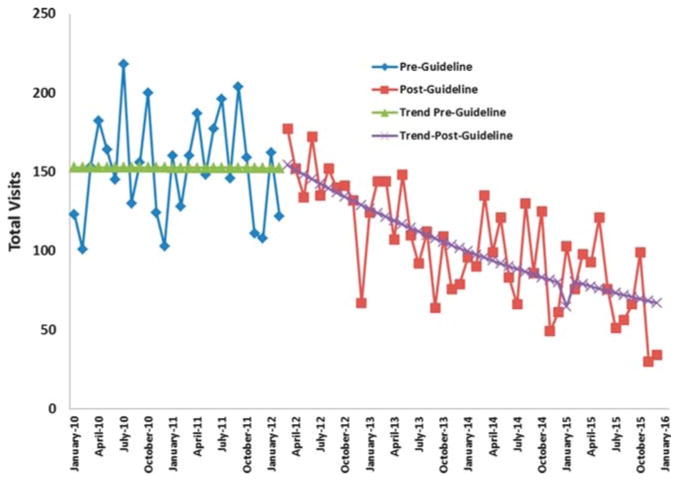
Monthly colposcopy clinic volume and trend, 2010 to 2015. Negative binomial regression trend line demonstrates observed decline in monthly volume before and after 2012 guideline implementation.
Data regarding the number of unattended, “no-show” appointments were also collected for each month, and annual appointment no-show rates were calculated. To address economic influences during this study period, annual average gasoline prices were obtained, and pricing trends were evaluated using Spearman correlation.7
Results
There were a total of 8722 colposcopy clinic visits between January 2010 and December 2015. Approximately 7395 visits (85%) were new patient visits, and 1327 visits (15%) were return visits (Figure 1). The proportion of new to return visits shifted significantly with the percentage of return visits, demonstrating a statistically significant decrease from 22.9% (2011) to 9.0% (2015; P < 0.001). Annual clinic volume ranged from 903 to 1884 visits with a mean monthly volume of 121.1 visits (SD, 42.1). The highest annual volume was demonstrated in 2011 with 1884 visits, and volume declined annually thereafter with an annual volume of 903 visits in 2015.
Figure 1.
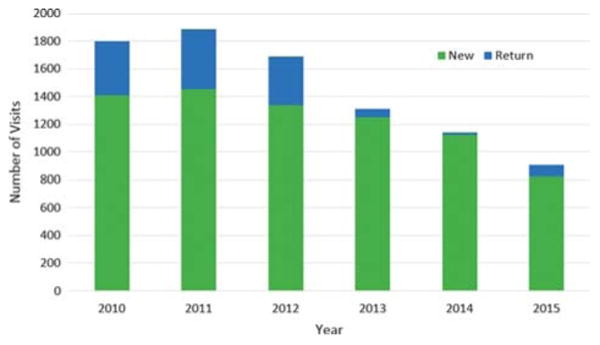
Annual colposcopy volume. Breakdown of annual volume by visit type, comparing new versus return visits. Significant decline in return volume noted from 2010 to 2015 (P < 0.001).
Figure 2 shows 2 separate negative binomial regression lines based on the guideline release date. The total visits trend clearly decreasing from the guideline implementation date. Observed trends in volume before and after guideline implementation were significantly different (P < 0.01). Specifically, average monthly volume in 2015 dropped to approximately one third of peak monthly volume in July 2010, with 75.3 visits per month and 218 visits per month, respectively. We investigated alternative reasons for the decrease in colposcopy volume including economic barriers as women typically had to drive long distances to this clinic. Annual average gasoline prices showed little change over the study period (2010—$2.74/gal, 2011—$3.48/gal, 2012— $3.55/gal, 2013—$3.44/gal, 2014—$3.30/gal, 2015—$2.36/gal) and were not associated with annual volume (Spearman correlation, r = 0.54; P > 0.2). The rate of “no-shows” remained consistent throughout the study period as well (52.9%–58.1%).
Discussion
A steady decline in total colposcopy clinic volume, average monthly volume, and proportion of return visits was noted from 2010 to 2015, as would be expected, given significant changes in practice guidelines during the same period.
The data were collected from a university-based clinic that follows the most recent evidence-based practice guidelines. The setting of this colposcopy clinic offered a unique opportunity to evaluate changes in volume related to guideline updates, as UAB provides substantial input on establishing statewide health department screening guidelines, which follow published guidelines from the US Preventive Services Task Force.5 The University of Alabama at Birmingham is also the primary referral center in the state for women with abnormal cervical cytology from the county health departments.
Although this study is strengthened by review of a large-volume referral clinic, managed strictly by the latest evidence-based guidelines, it is limited by the inherent biases associated with retrospective data collection, which include difficulty controlling for confounding variables and determining cause-effect relationships. Data regarding specific cytologic and pathologic diagnoses and patient age were not collected in this initial review, as we focused primarily on volume changes with this study. Future studies may be conducted to evaluate this further and may help identify whether more recent volume has shifted to include primarily high-grade disease in light of the newest guidelines.
We were unable to account for all factors that may have affected the decline in colposcopic volume. Factors which may affect a clinic's volume may include: vaccination impact and referral patterns. It should be noted that this clinic serves primarily uninsured or state funded patients. Although a nominal fee is requested no patient is turned away if they cannot afford the fee, and therefore, economic trends are unlikely to affect the number of visits. Moreover, annual average gasoline prices did not demonstrate an increase that corresponded with the declining volume in this study period.8 The rate of “no-shows” remained consistent throughout the study period as well (52.9%–58.1%), suggesting that the limitations associated with travel to our referral clinic were relatively consistent over time.
Clinic structure and statewide referral methods were reviewed, and we did not detect any changes in the clinic structure or referral patterns; the UAB Colposcopy Clinic remains the sole referral center for this patient population. Lastly, long-term effects of HPV vaccination are anticipated to lead to decreased rates of high-grade cervical dysplasia, although, given the low vaccination rates in the state of Alabama, vaccination against HPV is not likely to have contributed to the significant decline in volume discovered in this study.9
It is generally understood that increased volume translates into better patient outcomes. Multiple studies evaluating caseload and patient outcomes have confirmed this “practice makes perfect” hypothesis in cases of high-risk, complex surgery, cancer treatment, and management of critically ill patients by demonstrating improved patient outcomes with increased caseload.10–13 The colposcopy procedure is associated with considerable subjectivity and interobserver variability, which presents a challenge when it comes to providing a standardized service.14,15 Per current recommendations from the American Society for Colposcopy and Cervical Pathology, the performance of reliable colposcopy necessitates clinical insight and experience and should ideally be performed only after comprehensive didactic and clinical instruction is obtained.16 Studies evaluating the sensitivity and accuracy of colposcopy have demonstrated differences between more and less experienced colposcopists and improved sensitivity with an increased number of biopsies, although additional research to identify factors that influence the precision of colposcopic diagnosis is needed.17–20
Going forward, it is important that future colposcopists continue to receive adequate training in light of declining volume. The Council on Resident Education in Obstetrics and Gynecology requires Obstetrics and Gynecology residents to demonstrate competence in performing and interpreting these screening and diagnostic procedures for cervical intraepithelial neoplasia.21 As colposcopy volume at UAB's large-volume referral center has experienced a dramatic decline, we must assume colposcopy volume in other practices nationwide will also experience a similar decline in light of the most recent guideline changes. If a decline is noted on a national level, attention will need to be directed at developing minimum standards for training in colposcopy and ensure sufficient training to provide an acceptable standard of care. Future studies should be conducted to evaluate the accuracy of cervical dysplasia diagnosis with colposcopy as it relates to provider experience and training, as well as accuracy of cervical dysplasia diagnosis related to colposcopic technique; studies should also evaluate whether decline in colposcopy volume can be validated in other practices across the United States and evaluate how the generation of quality assurance standards have affected the performance of colposcopy in those countries with established standards. In response to the anticipated growing deficit in colposcopic volumes, training programs should consider the use of simulation models to supplement colposcopic education. Simulation models have already been widely adopted in the realm of gynecologic surgery and have been proven effective.22 Colposcopic training models have been developed and used by institutions worldwide with comparable success.23 Based on this evidence, we should work to establish a set of quality assurance standards for the practice of colposcopy in the United States. These data raise the question of whether we also need to develop a certification process for colposcopists and whether low-volume colposcopists are able to maintain adequate experience to continue performing the colposcopy procedure. Colposcopy standards have already been established in Europe, Canada, and Australia.24,25 With established standards in place, a system for continued audit of individual practice could be developed, with the goal of identifying areas of deficiency and implementing practice improvements.
Conclusions
As expected, recent changes to cervical cancer screening and colposcopy guidelines have resulted in a significant downward trend in colposcopy volume from 2010–2015, and we anticipate that this trend will be seen on a national level. This generates potential for negative implications with respect to training of future colposcopists and maintaining adequate experience for current providers. Moving forward, this serves as a call to action for professional organizations to carefully consider implications of this decline in colposcopy volume as well as opportunities for improvement of current training and credentialing practices.
Acknowledgments
None.
Footnotes
Oral presentation and winner of the “Best Scientific Paper” award at the American Society for Colposcopy and Cervical Pathology Biennial Scientific Meeting: April 9 to 12, 2014, Scottsdale, AZ.
The authors have declared they have no conflicts of interest.
IRB: Approved, Protocol X130930005.
Disclosures: Warner K. Huh serves as a member of the Merck Scientific Advisory Board.
References
- 1.Papanicolaou GN, Traut HF. The diagnostic value of vaginal smears in carcinoma of the uterus. 1941. Arch Pathol Lab Med. 1997;121:211–24. [PubMed] [Google Scholar]
- 2.Saslow D, Solomon D, Lawson HW, et al. American Cancer Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. Am J Clin Pathol. 2012;137:516–42. doi: 10.1309/AJCPTGD94EVRSJCG. [DOI] [PubMed] [Google Scholar]
- 3.Wright TC, Jr, Massad LS, Dunton CJ, et al. 2006 consensus guidelines for the management of women with abnormal cervical screening tests. J Low Genit Tract Dis. 2007;11:201–22. doi: 10.1097/LGT.0b013e3181585870. [DOI] [PubMed] [Google Scholar]
- 4.Bulletins—Gynecology ACoP. ACOG Practice Bulletin no. 109: Cervical cytology screening. Obstet Gynecol. 2009;114:1409–20. doi: 10.1097/AOG.0b013e3181c6f8a4. [DOI] [PubMed] [Google Scholar]
- 5.Massad LS, Einstein MH, Huh WK, et al. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2013;17(5 Suppl 1):S1–27. doi: 10.1097/LGT.0b013e318287d329. [DOI] [PubMed] [Google Scholar]
- 6.Long JS. Regression models for categorical and limited dependent variables. Thousand Oaks, CA: Sage Publications; 1997. [Google Scholar]
- 7.Daniel WW. Applied Nonparametric Statistics. 2nd. Boston, MA: Cengage Learning; 1990. [Google Scholar]
- 8.U.S. Department of Energy. U.S. Energy Information Administration, Independent Statistics & Analysis: Petroleum & Other Liquids. [Accessed February 20, 2015];2015 Available at: http://www.eia.gov/dnav/pet/pet_pri_gnd_dcus_r30_a.htm.
- 9.Brotherton JM, Fridman M, May CL, et al. Early effect of the HPV vaccination programme on cervical abnormalities in Victoria, Australia: an ecological study. Lancet. 2011;377:2085–92. doi: 10.1016/S0140-6736(11)60551-5. [DOI] [PubMed] [Google Scholar]
- 10.Lee MS, Tsai SJ, Lee CC, et al. Higher caseload improves cervical cancer survival in patients treated with brachytherapy. Radiat Oncol. 2014;9:234. doi: 10.1186/s13014-014-0234-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang CM, Huang KY, Hsu TW, et al. Multivariate analyses to assess the effects of surgeon and hospital volume on cancer survival rates: a nationwide population-based study in Taiwan. PLoS One. 2012;7:e40590. doi: 10.1371/journal.pone.0040590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee CC, Huang TT, Lee MS, et al. Survival rate in nasopharyngeal carcinoma improved by high caseload volume: a nationwide population-based study in Taiwan. Radiat Oncol. 2011;6:92. doi: 10.1186/1748-717X-6-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walkey AJ, Wiener RS. Hospital case volume and outcomes among patients hospitalized with severe sepsis. Am J Respir Crit Care Med. 2014;189:548–55. doi: 10.1164/rccm.201311-1967OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hopman EH, Kenemans P, Helmerhorst TJ. Positive predictive rate of colposcopic examination of the cervix uteri: an overview of literature. Obstet Gynecol Surv. 1998;53:97–106. doi: 10.1097/00006254-199802000-00021. [DOI] [PubMed] [Google Scholar]
- 15.Sideri M, Spolti N, Spinaci L, et al. Interobserver variability of colposcopic interpretations and consistency with final histologic results. J Low Genit Tract Dis. 2004;8:212–6. doi: 10.1097/00128360-200407000-00009. [DOI] [PubMed] [Google Scholar]
- 16.American Society for Colposcopy and Cervical Pathology. Colposcopy: Basic components of the colposcopic exam. [Accessed March 31, 2014];2014 Available at: http://www.asccp.org/Members/Practice-Management-Full-Access/Cervix/Colposcopy.
- 17.Huh WK, Sideri M, Stoler M, et al. Relevance of random biopsy at the transformation zone when colposcopy is negative. Obstet Gynecol. 2014;124:670–8. doi: 10.1097/AOG.0000000000000458. [DOI] [PubMed] [Google Scholar]
- 18.Bekkers RL, van de Nieuwenhof HP, Neesham DE, et al. Does experience in colposcopy improve identification of high grade abnormalities? Eur J Obstet Gynecol Reprod Biol. 2008;141:75–8. doi: 10.1016/j.ejogrb.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 19.Gage JC, Hanson VW, Abbey K, et al. Number of cervical biopsies and sensitivity of colposcopy. Obstet Gynecol. 2006;108:264–72. doi: 10.1097/01.AOG.0000220505.18525.85. [DOI] [PubMed] [Google Scholar]
- 20.Jeronimo J, Schiffman M. Colposcopy at a crossroads. Am J Obstet Gynecol. 2006;195:349–53. doi: 10.1016/j.ajog.2006.01.091. [DOI] [PubMed] [Google Scholar]
- 21.The American Congress of Obstetricians and Gynecologists. [Accessed August 25, 2016];CREOG Educational Objectives. (10th). Available at: https://www.acog.org/-/media/Departments/Members-Only/CREOG/CREOGEducationalObjectives.pdf.
- 22.Selzer DJ, Dunnington GL. Surgical skills simulation: a shift in the conversation. Ann Surg. 2013;257:594–5. doi: 10.1097/SLA.0b013e3182894756. [DOI] [PubMed] [Google Scholar]
- 23.Ferris DG, Waxman AG, Miller MD. Colposcopy and cervical biopsy educational training models. Fam Med. 1994;26:30–5. [PubMed] [Google Scholar]
- 24.Bentley J Society of Canadian C. Colposcopic management of abnormal cervical cytology and histology. J Obstet Gynaecol Can. 2012;34:1188–206. doi: 10.1016/S1701-2163(16)35468-8. [DOI] [PubMed] [Google Scholar]
- 25.National Health Service Cervical Screening Programme. Colposcopy and programme management: guidelines for the NHS Cervical Screening Programme. 2nd. Sheffield, England: NHS Cancer Screening Programmes—Fullwood House; 2010. pp. 1–88. [Google Scholar]


