Question
A 73-year-old woman experienced 2 episodes of hematochezia 2 weeks before her admission. She had been treated for mild hypertension, and had a history of cholecystectomy, appendectomy, 2 C-sections, and unspecified pancreatic surgery 17 years prior. At presentation, her laboratory examinations showed a mild anemia (hemoglobin, 10.7 g/dL; hematocrit, 33.5%) and a slight increase of alkaline phosphatase (169 U/L; normal range, 45–129). She underwent colonoscopy at an outside hospital, which demonstrated an ulcerated partially obstructing large mass in the right colon. A contrast-enhanced computed tomography (CT) scan was subsequently requested in our hospital. Contrast-enhanced CT scan showed an 18.0 × 17.0-cm large pancreatic multilobulated cystic mass in the head of the pancreas with innumerable central calcifications (Figure A). CT images also demonstrated that the mass was composed of numinous central small cysts and some peripheral larger cysts (Figures A, white asterisks). The pancreatic mass was associated with pancreatic atrophy, biliary and pancreatic ducts dilatation (Figures A, black asterisks), encased the superior mesenteric vein (Figure A, black arrow), and displaced the duodenum (Figure A, white arrows). The pancreatic mass also infiltrated and protruded into the right colon lumen (Figure A, dashed arrows).
Figure A.
What is the diagnosis?
Look on page 000 for the answer and see the Gastroenterology website (www.gastrojournal.org) for more information on submitting your favorite image to Clinical Challenges and images in GI.
Answer to: Image 1 (page ■ ■ ■): Giant Serous Cystadenoma of the Pancreas Infiltrating the Colonic Wall
CT and magnetic resonance imaging studies obtained at the time of the patient described 17 years prior pancreatic surgery were obtained. These demonstrated an 8.5 × 8.0-cm typical serous cystadenoma with a honeycomb appearance on T2-weighted imaging (Figure B) and encasing the superior mesenteric vein (Figure C, black arrow). The operating room report back then described that the resection of the pancreatic lesion was not possible owing to adhesion to the superior mesenteric vein. The patient underwent right hemicolectomy and debulking of the serous cystadenoma because its complete resection was not possible. Pathology confirmed the diagnosis of serous cystadenoma infiltrating the colonic wall (Figure D). Microscopy showed variably sized small cysts lined by cuboidal cells with small hyperchromatic nuclei and subepithelial capillaries (Figure E; stain: hematoxylin and eosin; original magnification, ×100).
Figure B.

Figure C.
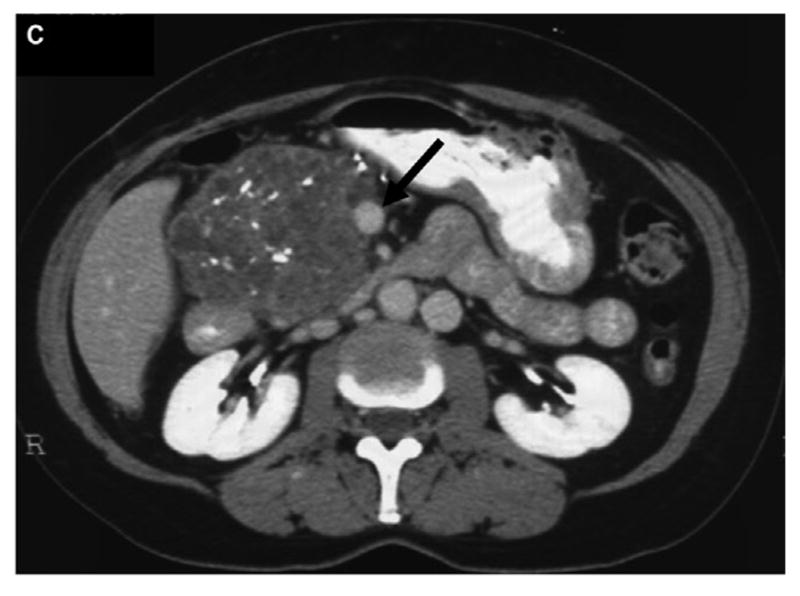
Figure D.

Figure E.

Pancreatic serous cystadenoma is a benign neoplasm which accounts for 1%–2% of all primary pancreatic neoplasms and 10%–15% of cystic pancreatic lesions.1 However, giant pancreatic serous cystadenomas (GPSC), defined as lesions measuring ≥10 cm, are very rare with only some sporadic cases reported in the literature.2 Liu et al2 in a recent review demonstrated that GPSC was more common in women (76%), with a mean age of 65.5 years and slightly more frequent in the head of the pancreas (59%). GPSC tend to adhere, compress, encase, or even infiltrate adjacent structures. Therefore, symptoms are more frequent, occurring in around 70% of cases, such as abdominal pain, nausea, vomiting, and abdominal mass. The microcystic appearance is more frequent (59%), followed by the macrocystic (35%) and mixed type (6%). Some surgeons advocate surgical resection for serous cystadenomas measuring ≥4 cm owing to rapid growth and potential complications, including obstructive pancreatitis, infiltration of surrounding structures, and malignant transformation.3 Curative resection is the treatment of choice for GPSC, when feasible.
Acknowledgments
Funding
This work was supported by the MSK Cancer Center Support Grant/Core Grant P30 CA008748.
Footnotes
Conflicts of interest
The authors disclose no conflicts.
References
- 1.Bosman FT, Carneiro F, Hruban RH, et al. WHO classification of tumours of the digestive system. Geneva: World Health Organization; 2010. [Google Scholar]
- 2.Liu QY, Zhou J, Zeng YR, et al. Giant serous cystadenoma of the pancreas (≥ 10 cm): the clinical features and CT findings. Gastroenterol Res Pract. 2016;2016:8454823. doi: 10.1155/2016/8454823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Horvat N, Monti S, Mannelli L. Unusual liver tumors. Gastroenterology. 2017;152:1287–1288. doi: 10.1053/j.gastro.2016.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]



