Abstract
Kidney disease is a common complication in patients with multiple myeloma. Traditionally, patients with active multiple myeloma and end-stage renal disease have been excluded from kidney transplantation due to the risk of malignancy progression. The introduction of bortezomib-based therapy for patients with multiple myeloma and renal impairment has significantly improved survival in this population. In this report, we present 2 cases of patients with active and controlled multiple myeloma who underwent successful kidney transplantation without progression of their underlying malignancy. In patients with active multiple myeloma controlled with bortezomib, kidney transplantation should be considered a valid option for patients with end-stage kidney disease.
Kidney involvement is a common clinical manifestation of multiple myeloma. It has been estimated that over 50% of patients develop some form renal impairment during their disease, with more than 12% requiring renal replacement therapy.1-3 The presence of renal disease in multiple myeloma is a poor prognostic indicator, especially among those requiring dialysis.4,5
Advancements in the treatment of multiple myeloma have resulted in an increase in median survival of greater than 5 years after the initial diagnosis of multiple myeloma. Patients with end-stage renal disease with multiple myeloma have typically been excluded from kidney transplantation due to concerns of disease progression in the presence of chronic immunosuppression.6 The prebortezomib literature for patients with multiple myeloma and kidney transplantation has been limited to case reports and case series in patients who were in remission before transplantation and have demonstrated very poor outcomes with a high rate of progressive myeloma and patient death.7-11 Herein we present 2 successful cases of kidney transplantation with ongoing multiple myeloma and stable light chain disease maintained on bortezomib before and after kidney transplantation.
CASE REPORT
Case 1
The patient is a 67-year-old man with a medical history notable for hypertension, ulcerative colitis requiring colectomy with ostomy placement at age 58 years, and left renal cell carcinoma postlaproscopic nephrectomy at age 59 years, and was started on maintenance hemodialysis at age 66 years. The cause of his renal disease was attributed to his longstanding hypertension and reduced nephron mass after nephrectomy. Histology of the renal cell carcinoma showed a mass of 4.8 cm with clear margins and clear cell pathology. The patient was monitored for several years with no evidence of recurrent disease.
After referral for kidney transplantation, he was noted to have an M spike of 0.9 g/dL on serum protein electrophoresis. Analysis of the serum light chains demonstrated markedly elevated serum κ light chains at 3461 mg/L (reference, 5.7-26.3 mg/L) and a mild elevation in λ chains at 86 mg/L was also present (reference, 3.3-19.4 mg/L), which was thought to be compatible with kidney failure. A bone survey was unremarkable, and the patient underwent a bone marrow biopsy showing 25% plasma cell involvement, consistent with multiple myeloma. Given his severe renal impairment, he was started on dexamethasone and bortezomib maintenance therapy, which he was maintained on for 1 year before kidney transplantation. The patient responded well to therapy with a reduction in his κ light chains to 300 to 500 mg/L (reference, 5.7-26.3 mg/L), and the λ light chains remained elevated at 80 to 90 mg/L. A repeat bone marrow biopsy showed no evidence of plasma cell dyscrasia.
The patient subsequently underwent a living unrelated kidney transplant as part of a paired exchange, with his wife as his exchange donor. The patient has a donor-specific antibody to his wife, and direct donation was not possible. The import donor was in his 60s and had a donation creatinine of 1.1 mg/dL. The patient was unsensitized at the time of transplant with a panel reactive assay of 0% and received basiliximab for induction. He was discharged from the hospital on postoperative day 4 with a creatinine of 1.9 mg/dL.
Posttransplantation, he was maintained on bortezomib every 3 weeks. Both his κ and λ light chains decreased to the normal reference range and have remained so 2 years postkidney transplantation (Figure 1A). His transplant course had otherwise been complicated by tremors requiring a switch from tacrolimus to cyclosporine and BK viremia 5 months posttransplant with discontinuation of mycophenolate mofetil. He was maintained on dual therapy with prednisone and cyclosporine with a baseline creatinine between 1.8 and 2.0 mg/dL with no proteinuria. A protocol biopsy at 1 year demonstrated no evidence of multiple myeloma or rejection within the kidney transplant. The patient had no evidence of donor-specific antibodies on testing at 6, 12, and 24 months posttransplantation by single antigen beads (Luminex). He remains on bortezomib therapy with stable allograft function 25 months after kidney transplantation, with a serum creatinine of 2.0 mg/dL.
FIGURE 1.
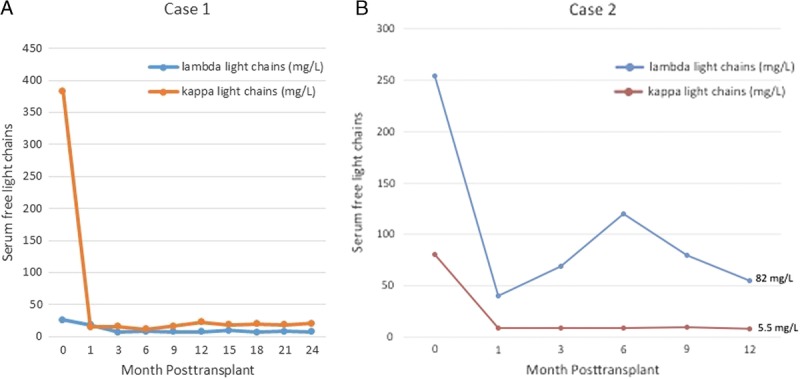
A, λ and κ Light chain trend after transplantation in patient 1. B, λ and κ Light chain trend after transplantation in patient 2.
Case 2
The patient is a 62-year-old woman with a medical history notable for multiple myeloma. She was initially diagnosed with multiple myeloma 4 years before she presented with profound anemia (Hg, 4 g/dL), markedly impaired renal function with a serum creatinine of 5.7 mg/dL, and nephrotic range proteinuria (7.4 g/g). A native kidney biopsy was performed and demonstrated myeloma cast nephropathy. A bone survey was negative, and a bone marrow biopsy showed plasma infiltrates of more than 30% within the bone marrow, consistent with multiple myeloma. She was initially treated with plasmapheresis, dexamethasone, and bortezomib with improvement in her renal function to a serum creatinine of 2.7 mg/dL. She developed a perforated duodenal ulcer with high-dose dexamethasone which required surgical repair.
She was maintained on bortezomib dosing every 2 weeks with stable elevations in her serum κ and λ light chains. Her serum κ light chains ranged from a value of 140 to 343 mg/L (reference, 5.7-26.3 mg/L), and the serum λ light chains ranged from a value of 69 to 80 mg/L (reference, 3.3-19.4 mg/L). Unfortunately, the patient's kidney disease progressed, and she was initiated on hemodialysis 2 years before kidney transplantation. A repeat bone marrow biopsy showed normal bone marrow.
The patient subsequently underwent a living unrelated kidney transplant as part of a paired exchange, with her daughter as her exchange donor. The import donor was in her 40s with a donation creatinine of 0.9 mg/dL. The patients were sensitized with a panel reactive assay of 57%, and she received basiliximab for induction given her active multiple myeloma. She was discharged on hospital day 4 with a serum creatinine of 0.9 mg/dL.
Posttransplantation, she was initially maintained on bortezomib every 2 weeks. Her κ light chains decreased to the normal reference range, and her λ light chains decreased to 40 to 60 mg/L. Six months posttransplant, her hematologists decreased her bortezomib dosing to every 3 weeks and her λ light chains increased to 120 mg/L. Her urine protein was measured at 0.11 mg/dL without Bence-Jones proteinuria on dilution. Her bortezomib was subsequently increased to every 2-week dosing and her λ chains decreased to 40 to 60 mg/L (Figure 1B).
Her posttransplant course has otherwise been uncomplicated. She was unable to tolerate mycophenolate mofetil or mycophenolic acid due to severe gastrointestinal side effects and has been maintained on dual therapy with prednisone and tacrolimus with a baseline creatinine between 0.9 and 1.1 mg/dL for the past year posttransplantation and her urine protein:creatinine ratio was less than 0.10. The patient had no evidence of donor-specific antibodies on testing at 6 and 12 months by single-antigen beads (Luminex). She refused a protocol biopsy at 1 year. She remains on bortezomib therapy with stable allograft function 13 months after kidney transplantation, with a serum creatinine of 1.0 mg/dL.
DISCUSSION
Kidney transplantation is the preferred therapy for patients with end-stage kidney disease. However, the necessity of immunosuppression in kidney transplantation can exacerbate preexisting malignancy. General guidelines recommend a period of remission for most malignancies and avoidance of transplantation in patients with active multiple myeloma.12,13
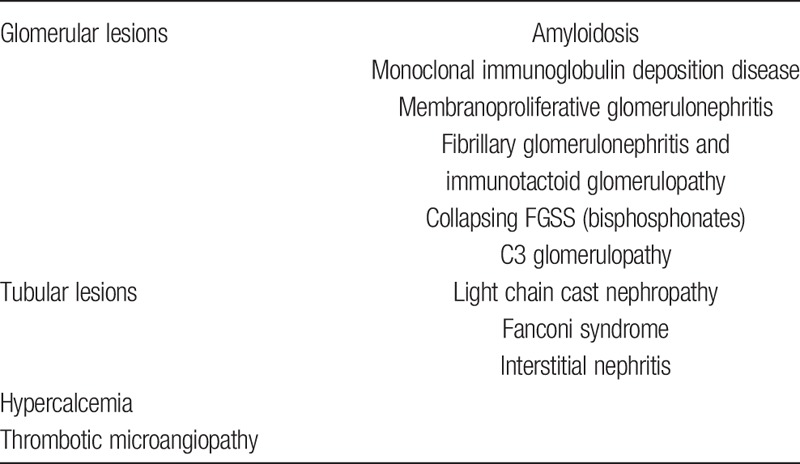
However, kidney disease is a common complication of multiple myeloma. Over 50% of patients develop some form of renal impairment during their disease, with 20% to 50% presenting with renal impairment at the time of diagnosis. Although the overproduction of immunoglobulins by clonal plasma cells is the underlying cause of kidney disease, various clinical manifestations exist (Table 1). Many patients present with acute kidney injury, which is reversible. However, more than 12% may develop chronic kidney disease, requiring renal replacement therapy. The presence of renal disease in multiple myeloma is a poor prognostic indicator, especially among those requiring dialysis, with a survival rate of 45% at 1 year compared with 80% for patients with a serum creatinine less than 1.5 mg/dL with traditional therapy.14,15
TABLE 1.
Renal manifestations of multiple myeloma
A whole host of new drugs has become available for the treatment of multiple myeloma in the past 10 to 15 years including thalidomide, lenalidomide, pomalidomide, bortezomib, carfilzomib, and more recently 2 monoclonal antibodies, daratumumab and elotumumab. First-line therapy of myeloma today typically consists of 1 or more of the newer agents plus a steroid. High-dose chemotherapy and autologous stem cell transplant (ASCT) after induction treatment is still considered standard of care. Studies in patients with renal impairment show improved clinical outcomes with effective control and reduction in light chains comparable to patients without renal impairment.16 These advancements have resulted in a marked increase in survival in patients with multiple myeloma, with median survival now approaching 5 years. The incidence of multiple myeloma as the cause of end-stage renal disease has decreased in the past decade, and mortality has improved significantly, meaning more patients are living longer on dialysis and multiple myeloma.
Kidney transplantation of patient with active multiple myeloma has generally been avoided due to risks of accelerated malignancy. Le et al17 reported on 4 patients who underwent kidney transplantation after ASCT and hematological remission. Time from remission to transplantation ranged from 20 to 66 months. Two patients continued bortezomib posttransplantation with developing progression of myeloma at 6 months posttransplantation. With a larger cohort of individual with AL amyloidosis, Herrmann et al18 also demonstrated successful kidney transplantation in patients with AL amyloidosis with complete response with or without ASCT in a larger cohort of 19 patients. Both case series demonstrate that kidney transplantation after complete hematological remission of myeloma with or without autologous stem cell transplantation is feasible with reasonable short-term outcomes.
To our knowledge, these are the first cases of patients who underwent kidney transplantation with active multiple myeloma and partial hematological response to chemotherapy at the time of transplantation. Both patients continue to have partial remission and are maintained on maintenance bortezomib therapy. The primary limitations of our report are the short follow-up time postkidney transplantation from 13 to 25 months posttransplantation and the small number of participants (n = 2).
However, we demonstrate a potential template for transplantation in carefully selected individuals with multiple myeloma in partial remission on bortezomib who have not undergone ASCT. Ensuring that patients achieve at least a partial remission as determined by measurement of serum and urine paraproteins and bone marrow analysis would appear to be critical for long-term success. Both patients underwent paired exchange because of preexisting donor-specific antibodies to their original donor. This allowed induction with basiliximab and avoidance of ATG to minimize the risk of exacerbating her underlying malignancy. However, ATG may have some antiplasma cell activity and could be considered.19 In addition, close monitoring while on continuous treatment with bortezomib was another important facet of our patients' management. One caveat to this is that immune modulating therapies should be avoided, as we have previously reported precipitation of acute rejection with these compounds.20
CONCLUSIONS
A new generation of therapeutic agents to treat multiple myeloma has dramatically improved outcomes in patients with significant renal impairment. Emerging data suggest that kidney transplantation in patients with a history of multiple myeloma with complete response with or without ASCT should be considered. However, complete response cannot be achieved by every patient. Patients with a good partial response and low light chain burden on maintenance chemotherapy may also benefit from kidney transplantation. Careful selection of patients with a history of multiple myeloma is essential in assessing which patients should undergo kidney transplantation, but a history of multiple myeloma should no longer be considered an absolute contraindication.
Footnotes
Published online 21 July, 2017.
The authors declare no funding or conflicts of interest.
E.L.L., N.K., T.P., G.D., S.B. participated in writing of the article. E.L.L. and T.P. did the figures.
REFERENCES
- 1.Kyle RA, Gertz MA, Witzig TE, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc. 2003;78:21–33. [DOI] [PubMed] [Google Scholar]
- 2.Torra R, Bladé J, Cases A, et al. Patients with multiple myeloma requiring long-term dialysis: presenting features, response to therapy, and outcome in a series of 20 cases. Br J Haematol. 1995;91:854–859. [DOI] [PubMed] [Google Scholar]
- 3.Sakhuja V, Jha V, Varma S, et al. Renal involvement in multiple myeloma: a 10-year study. Ren Fail. 2000;22:465–477. [DOI] [PubMed] [Google Scholar]
- 4.Reule S, Sexton DJ, Solid CA, et al. ESRD due to multiple myeloma in the United States, 2001–2010. J Am Soc Nephrol. 2016;27:1487–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knudsen LM, Hjorth M, Hippe E. Renal failure in multiple myeloma: reversibility and impact on the prognosis. Nordic Myeloma Study Group. Eur J Haematol. 2000;65:175–181. [DOI] [PubMed] [Google Scholar]
- 6.Knoll G, Cockfield S, Blydt-Hansen T, et al. Canadian Society of Transplantation: consensus guidelines on eligibility for kidney transplantation. CMAJ. 2005;173:S1–S25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dagher F, Sammett D, Abbi R, et al. Renal transplantation in multiple myeloma. Case report and review of the literature. Transplantation. 1996;62:1577–1580. [DOI] [PubMed] [Google Scholar]
- 8.Leung N, Lager DJ, Gertz MA, et al. Long-term outcome of renal transplantation in light-chain deposition disease. Am J Kidney Dis. 2004;43:147–153. [DOI] [PubMed] [Google Scholar]
- 9.Heher EC, Spitzer TR, Goes NB. Light chains: heavy burden in kidney transplantation. Transplantation. 2009;87:947–952. [DOI] [PubMed] [Google Scholar]
- 10.Heher EC, Spitzer TR. Hematopoietic stem cell transplantation in patients with chronic kidney disease. Semin Nephrol. 2010;30:602–614. [DOI] [PubMed] [Google Scholar]
- 11.Spitzer TR, Sykes M, Tolkoff-Rubin N, et al. Long-term follow-up of recipients of combined human leukocyte antigen-matched bone marrow and kidney transplantation for multiple myeloma with end-stage renal disease. Transplantation. 2011;91:672–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abramowicz D, Cochat P, Claas FH, et al. European Renal Best Practice Guideline on kidney donor and recipient evaluation and perioperative care. Nephrol Dial Transplant. 2015;30:1790–1797. [DOI] [PubMed] [Google Scholar]
- 13.Bansal T, Garg A, Snowden JA, et al. Defining the role of renal transplantation in the modern management of multiple myeloma and other plasma cell dyscrasias. Nephron Clin Pract. 2012;120:c228–c235. [DOI] [PubMed] [Google Scholar]
- 14.Korzets A, Tam F, Russell G, et al. The role of continuous ambulatory peritoneal dialysis in end-stage renal failure due to multiple myeloma. Am J Kidney Dis. 1990;16:216–223. [DOI] [PubMed] [Google Scholar]
- 15.Sharland A, Snowdon L, Joshua DE, et al. Hemodialysis: an appropriate therapy in myeloma-induced renal failure. Am J Kidney Dis. 1997;30:786–792. [DOI] [PubMed] [Google Scholar]
- 16.Kaygusuz I, Toptas T, Aydin F, et al. Bortezomib in patients with renal impairment. Hematology. 2011;16:200–208. [DOI] [PubMed] [Google Scholar]
- 17.Le TX, Wolf JL, Peralta CA, et al. Kidney transplantation for kidney failure due to multiple myeloma: case reports. Am J Kidney Dis. 2017;69:858–862. [DOI] [PubMed] [Google Scholar]
- 18.Herrmann SM, Gertz MA, Stegall MD, et al. Long-term outcomes of patients with light chain amyloidosis (AL) after renal transplantation with or without stem cell transplantation. Nephrol Dial Transplant. 2011;26:2032–2036. [DOI] [PubMed] [Google Scholar]
- 19.Timm MM, Kimlinger TK, Haug JL, et al. Thymoglobulin targets multiple plasma cell antigens and has in vitro and in vivo activity in multiple myeloma. Leukemia. 2006;20:1863–1869. [DOI] [PubMed] [Google Scholar]
- 20.Lum EL, Huang E, Bunnapradist S, et al. Acute kidney allograft rejection precipitated by lenalidomide treatment for multiple myeloma. Am J Kidney Dis. 2017;69:701–704. [DOI] [PubMed] [Google Scholar]


