Abstract
Purpose
The posterior subcapsular region of the prostate is often under-sampled by transrectal ultrasound (TRUS) guided biopsy. The close proximity of these lesions to the posterior capsular wall of the prostate makes them difficult to localize while increasing the need for early detection because of their increased risk for extracapsular extension. We retrospectively evaluated the multi-parametric MRI (mpMRI) features of subcapsular prostate cancers to make radiologists more aware of this condition.
Materials and Methods
Between January 2010 and July 2014 all patients referred for 3T mpMRI and subsequent MR-US Fusion guided biopsy (FgBx) and systematic 12-core sextant biopsy (SBx) under an IRB approved protocol, were reviewed and imaging confirmed subcapsular prostate cancers were identified. Subcapsular lesions were defined as thin lesions that were just inside the prostate capsule. Matching patient demographics and clinical findings including age, PSA, PSA density, whole prostate volume, history of prostate cancer, Gleason score, and clinical management were tabulated.
Results
Of 992 eligible patients, 33 patients had subcapsular lesions in the prostate detected by mpMRI. Mean age, PSA and prostate volume in this group were 63 years (range: 52–76 years), 8.4ng/mL (range: 1.22–65.20), and 53 mL (range: 12–125 mL), respectively. The combination biopsy (SBx + FgBx) confirmed prostate cancer in 24 of 33 patients (72.7%) and in 9 patients the biopsy was negative. Of the 24 cancers, 19 were confirmed on both FgBx and conventional biopsy; however 5 cancers were only detected on FgBx. In 4 of the 19 patients in which both biopsy methods were positive, the FgBx yielded a higher Gleason score.
Conclusion
Subcapsular lesions on mpMRI are relatively infrequent but are usually malignant. Although the majority are confirmed on conventional 12-core biopsies, about 20% of these lesions require FgBx for diagnosis and FgBx more accurately grades the lesions in another 20%. Thus, FgBx is of considerable benefit in confirming the diagnosis of subcapsular prostate cancer despite their proximity to the prostatic capsule.
Keywords: prostate cancer, subcapsular, MRI, fusion biopsy
Introduction
Prostate cancer is the second leading cause of cancer related death for men in the United States with an estimated 233,000 new diagnoses in 2014 [1]. Patients with elevated PSA and/or abnormal DRE findings, commonly undergo a standard-of-care systematic 12-core sextant biopsy (SBx). More recently, multiparametric magnetic resonance imaging (mpMRI) of the prostate has been employed for initial detection, staging and follow-up. A major benefit of mpMRI is that it more accurately localizes tumors prior to biopsy [2–4]. This has led to development of image-guided biopsies, most notably, MRI-transrectal ultrasound (TRUS) fusion guided biopsy (FgBx) [5]. Targeted biopsy permits more accurate sampling of regions of the prostate that are not routinely sampled during SBx, such as the very distal apical prostate and anterior transition zone [6–8]. Another challenging type of prostate lesion is one that grows along the posterior prostate capsule and tends to be long and thin [9]. These subcapsular lesions are found just deep to the prostate capsule and can be quite subtle and difficult to successfully biopsy because they are so thin and flat (Figure 1). During routine biopsy, the needle is placed within the prostatic parenchyma to avoid injury to periprostatic vessels and nerves. Thus, thin subcapsular lesions may be undersampled; however, to the best of our knowledge, there is no data in literature which reports on the undersampling of this specific area. These features make them easy to miss on mpMRI and SBx. In this study, we review our experience with such lesions and compare the utility of SBx and FgBx in this setting with the goal of increasing awareness of mpMRI features of posterior subcapsular prostate cancers.
Figure 1.
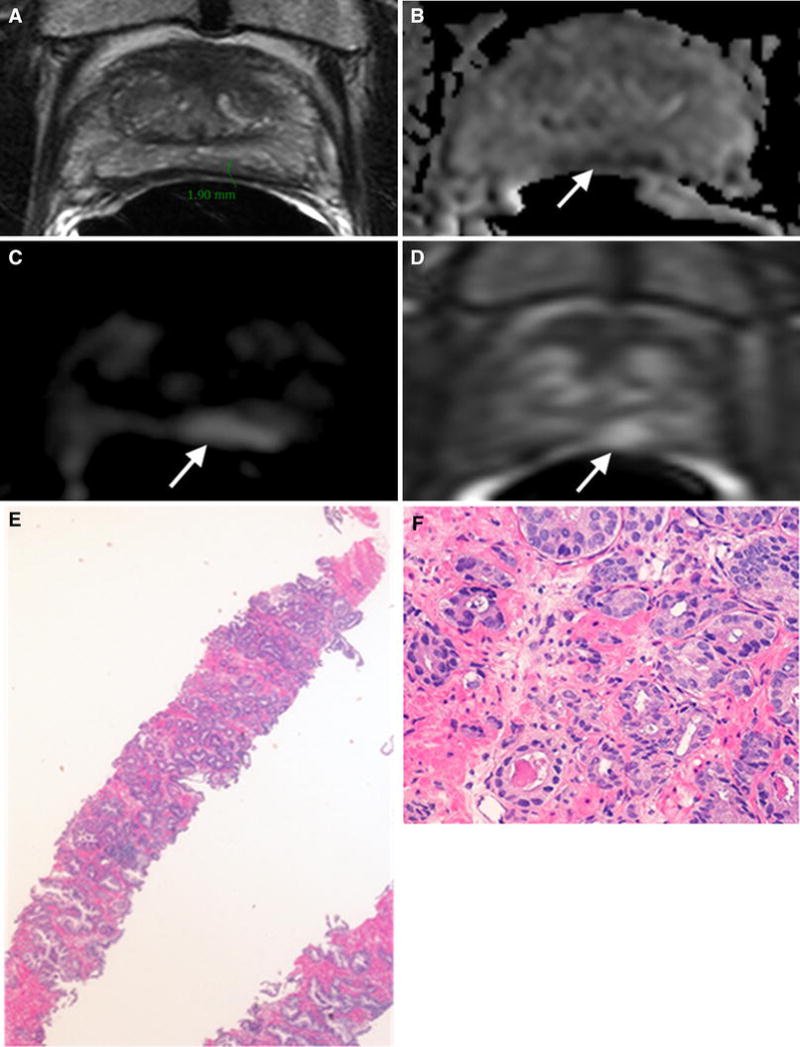
A 55 year old patient, with a PSA of 8.34 ng/mL, and history of one previous negative 12 core sextant biopsy Axial T2W MRI shows a poorly defined lesion in the left mid posterior peripheral zone, determined to be ‘subcapsular’ (1a). Axial diffusion weighted image shows a hypointense lesion in the corresponding left mid posterior peripheral zone (1b). Axial high b-value DWI (b=2000) is hyperintense in the left mid subcapsular peripheral zone (1c). Axial dynamic contrast enhanced image shows strong early hyper-enhancement in the left mid peripheral zone (1d). Subcapsular lesion was targeted by MRI/TRUS fusion guided biopsy. The needle biopsy specimen shows a clinically significant adenocarcinoma of the prostate at low power (1e), and high power (1f). Gleason score of 7 (4+3), involving 60% of 1 core. The patient became a candidate for active treatment (robotic assisted surgical prostatectomy vs. radiation therapy).
Materials and Methods
Study Design and Patient Population
This single-institution retrospective study was approved by the local institutional review board (IRB) and was compliant with the Health Insurance Portability and Accountability Act. From January 2010 to July 2014, 992 consecutive patients underwent an initial multi-parametric MRI scan with an endorectal coil at 3 Tesla. Based on the findings of the mpMRI all patients went on to both SBx and FgBx to confirm or rule-out cancer. A subcapsular lesion was defined as one that conformed to the inner margin of the posterior prostate capsule within the peripheral zone (Figure 1). Similar lesions in the anterior prostate were considered transition zone tumors and were excluded from this analysis.
Multiparametric MRI Evaluation of Subcapsular Lesions
Multiparametric MRI (mpMRI) scans were acquired using a 3 Tesla scanner (Achieva, Philips Healthcare, Best, The Netherlands). An endorectal coil (BPX-30, Medrad, Pittsburgh, Pennsylvania, USA) tuned to 127.8 MHz, and a 16-channel surface/cardiac coil (SENSE, Philips Medical Systems, Best, The Netherlands) were used. The multiparametric MRI included triplanar T2-weighted turbo-spin echo (T2W MRI), diffusion weighted MRI (DW MRI) with apparent diffusion coefficient (ADC) mapping, high b-value DW MRI (b=2000 s/mm2) and axial dynamic contrast enhanced imaging (DCE MRI). mpMRI pulse sequence parameters used were based on recommendations of PI-RADS [10, 11] (Table 1).
Table 1.
MRI pulse sequence parameters
| T2W MRI | DW MRI | DCE MRI | |
|---|---|---|---|
| FOV (mm) | 140 × 140 | 140 × 140 | 262 × 262 |
| Acquisition Matrix | 304 × 234 | 112 × 109 | 188 × 96 |
| TR/TE (ms) | 4434/120 | 4986/54 | 3.7/2.3 |
| Flip Angle (degrees) | 90 | 90 | 8.5 |
| Slice Thickness (mm), no gaps | 3.00 | 3.00 | 3.00 |
| Image Reconstruction Matrix (pixels) | 512 × 512 | 256 × 256 | 256 × 256 |
| Reconstruction Voxel Scanning Resolution (mm/pixel) | 0.27 × 0.27 × 3.00 | 0.55 × 0.55 × 2.73 | 1.02 × 1.02 × 3.00 |
| Time for Acquisition (min:sec) | 2:48 | 4:54 | 5:16 |
Each prostate mpMRI was evaluated by two radiologists (P.L.C. and B.T. with 15 and 7 years of experience in prostate MRI, respectively). The radiologists were blinded to patient specific details (age, ethnicity, PSA levels, digital rectal exam findings, prior biopsy/histopathology findings, family history). The evaluation was performed on T2W MRI, ADC maps of DWI, high b-value DWI (b=2000 s/mm2) and DCE MRI using the hospital PACS (Carestream Health, Rochester, New York, USA). Additionally, each patient’s whole gland prostate volume was measured using an in-house developed software (iCAD Inc, Nashua, New Hampshire, USA).
Prostate Biopsy
Patients who had suspicious areas identified on mpMRI underwent both SBx and FgBx including targeting of subcapsular lesions. The FgBx was performed with the UroNav platform (InVivo, Gainesville, Florida, USA) [12]. Biopsies were performed by a senior urologist and senior interventional oncologist (P.A.P. and B.J.W., with over 15 years of experience each in prostate biopsy). Along with the SBx 12 core standard of care biopsy, on average, 2 lesions per patient were targeted for FgBx biopsy (as determined by mpMRI evaluation).
Histopathology
Biopsy core specimens were evaluated and assigned with a Gleason score by a senior genitourinary pathologist (M.J.M., with an experience of 25 years).
Comparison of Subcapsular Biopsy Results with Systematic Biopsy Results
Tumor detection rates of SBx and FgBx were compared using Gleason scores. The targeted sites were matched with the corresponding sextant biopsy sites for a more focused regional histological comparison. Index lesions were determined based on the biopsy result confirming the highest Gleason score.
Evaluation of the Impact of Detection of Subcapsular Lesions on Clinical Management
A retrospective analysis was initially performed using laboratory and clinical results (i.e. PSA and DRE), and if available, prior biopsy results to categorize the pre-imaging clinical management status of the patients. Next, the actual clinical management following mpMRI, FgBx and SBx was determined.
Patients were placed into four initial categories based on their lab and histology results, using the National Comprehensive Cancer Network (NCCN) guidelines [13]. Patients with elevated PSA and no previous biopsy were considered to be biopsy naïve. Patients who had elevated PSA, with negative prior biopsy were considered to be inconclusive. Patients with a previous positive biopsy (required under NCCN criteria) but no previous treatment history were considered to be on active surveillance. Patients with a previous positive biopsy who were offered active therapy but declined were considered to be on active therapy.
After the mpMRI and MRI/TRUS fusion guided biopsy results, patients were then re-classified using the same categories with the addition of a no further management group. This category would include patients who were biopsy negative. The change in patient assignment was compiled.
While the previously defined categories remained the same, if any of the patients were now shown to be biopsy negative, after FgBx with standard of care SBx, they were re-grouped to be monitored by their annual PSA and DRE findings.
Statistical Analysis
Statistical analysis was performed using GraphPad Prism (version 6.01 for Windows, San Diego, CA). The Mann-Whitney U Test was used to compare the median age, PSA, whole prostate volumes, and PSA density between the positive and negative biopsy groups. For this analysis, lesions positive on mpMRI and positive on FgBx were classified as “FgBx positive.” Lesions positive on mpMRI and negative on FgBx were classified as “FgBx negative.”
Results
Patient Cohort
From January 2010 to July 2014, a total of 992 consecutive patients underwent mpMRI at 3 Tesla followed by SBx and FgBx. Of these, 33 (3%) men were identified as having a suspicious lesion in the posterior subcapsular region on mpMRI. In these 33 men, the median age was 63 years (range 52–76), and median PSA was 6.1 ng/mL (range 1.22–65.20) [Table 2]. Twenty-five of these patients (75.8%) had elevated PSA (>4.0 ng/mL) and DRE was abnormal (nodularity, induration, or asymmetry) in three cases (9%) [Table 3].
Table 2.
Patient Demographics
| Patients (n=33) | Mean | 95% CI of mean |
Median | 95% CI of median |
|---|---|---|---|---|
| Age (years) | 63 | 61 – 65 | 63 | 59 – 66 |
| PSA (ng/mL) | 8.4 | 4.6 – 12 | 6.1 | 4.8 – 8.5 |
| MRI volume (mL) | 53 | 44 – 61 | 50 | 43 – 59 |
| PSA density (ng/mL/cc) | 0.15 | 0.12 – 0.19 | 0.13 | 0.099 – 0.16 |
Table 3.
Differences between FgBx positive and negative group
| FgBx Positive | FgBx Negative | Total | p- value |
||
|---|---|---|---|---|---|
| Patients | 24 | 9 | 33 | ||
| Age (years) | Median [95% CI] | 64 [59 – 68] | 63 [55 – 67] | 0.43 | |
| Race | White | 19 | 7 | 26 | |
| Black | 4 | 1 | 5 | ||
| Other | 1 | 1 | 2 | ||
| PSA (ng/mL) | Median [95% CI] | 6.0 [4.4 – 8.3] | 8.6 [4.8 – 9.9] | 0.31 | |
| MRI volume (mL) | Median [95% CI] | 46 [32 – 59] | 59 [43 – 90] | 0.047 | |
| PSA density (ng/mL/cc) | Median [95% CI] | 0.14 [0.09 – 0.20] | 0.13 [0.067 – 0.17] | 0.73 | |
| DRE positive | 3 | 0 | 3 | ||
| Family history of PCa | 13 | 2 | 15 | ||
| Previous diagnosis of PCa | 14 | 1 | 15 |
Fifteen patients were previously diagnosed with prostate cancer and were on active surveillance at the time of presentation based on NCCN criteria. Of these previously diagnosed patients, 12 had Gleason 3+3, while three patients had low volume (<25%) Gleason 3+4. Of the remaining cases, 11 were biopsy naïve, and 7 were biopsy negative with elevated PSA. All patients were clinical Stage T1c at the time of presentation as they were previously diagnosed by needle biopsy without the use of imaging.
Histopathology and overall cancer detection
Among the 33 mpMRI subcapsular positive lesions, 24 (73%) had a positive biopsy for prostate cancer [Table 3]. All were positive on FgBx, whereas 19 (79%) were positive on SBx [Table 4]. Thus, FgBx resulted in a 19% increase in tumor positive biopsy yield when a subcapsular lesion was identified and targeted using the mpMRI. In this patient group, clinically significant cancer was more often detected on FgBx than with SBx [Table 5]. However, the overall mean Gleason scores were similar, 6.8 versus 6.7, between SBx and FgBx, respectively. Gleason scores of 3+3 were found in 6 cases (31%), 3+4 in 10 cases (52%), and 4+4 in 3 cases (15%), respectively, by SBx. Gleason scores of 3+3 were found in 8 cases (33%), 3+4 in 11 cases (45%), 4+3 in 2 cases (8%), and 4+4 in 3 cases (12%) by targeted FgBx of subcapsular lesions. Five cases (26%) were upgraded on FgBx when compared with SBx, and four of these cases (17%) were further upgraded to clinically significant disease (Gleason 4+3 and higher).
Table 4.
Systematic 12 Core Sextant Bx vs. MRI/TRUS Fusion Guided Bx for Overall Cancer Detection
| mpMRI Biopsies | Positive (FgBx) | Negative (FgBx) |
|---|---|---|
| Positive (SBx) | 19 | 0 |
| Negative (SBx) | 5 | 9 |
| Totals | 24 | 9 |
Table 5.
Gleason Grades
| GLEASON GRADE | TRUS SBx | FgBx |
|---|---|---|
| 6 (3+3) | 6 | 8 |
| 7 (3+4) | 10 | 11 |
| 7 (4+3) | - | 2 |
| 8 (4+4) | 3 | 3 |
| 9 (4+5) | - | - |
| 9 (5+4) | - | - |
| 10 (5+5) | - | - |
| TOTALS | 19 | 24 |
Subcapsular cancer detection
Among the 24 patients who had FgBx positive biopsies, 18 (75%) were confirmed to have subcapsular prostate cancer on FgBx. In the remaining six cases non-subcapsular cancer was found on FgBx, only one of which was clinically significant (Gleason >3+4 with 25% biopsy core involvement). Two mpMRI positive lesions for subcapsular cancer were not detected on initial biopsy, and were placed on active surveillance for Gleason 3+3 disease and for atypical gland presentation in biopsy cores obtained from a different location, respectively. These two cases later showed progression of subcapsular prostate lesions and a positive biopsy on FgBx, supporting the initial mpMRI findings of subcapsular prostate cancer.
The comparison of clinically significant subcapsular cancer on FgBx with the closest corresponding sextant biopsy result revealed 20 FgBx targets positive with 18 (85%) harboring clinically significant disease while the corresponding regions on SBx showed clinically significant disease in only 6 (30%).
Multiparametric MRI Whole Prostate Volumes
The median whole prostate volume based on mpMRI planimetric measurement was 50mL. Most prostate glands were enlarged due to secondary transition zone hyperplasia. In evaluation of the effect of prostate volume on subcapsular cancer detection by FgBx, there was a statistically significant difference (p=0.047) between the rate of positive yields from larger and smaller prostate glands. The median volume of biopsy positive cases (46mL, 95% CI 32–59) was smaller than biopsy negative cases (59mL, 95% CI 43–90) [Figure 2].
Figure 2.
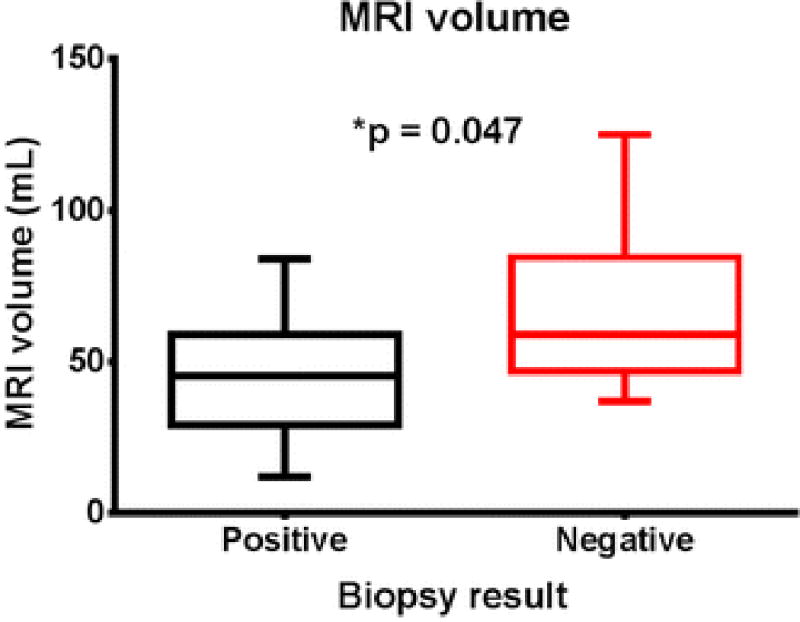
Planimetric prostate mpMRI volumes showing a statistically significant (p=0.03) difference between the biopsy positive and negative cases. Positive cases had a median whole prostate MRI volume of 45 mL, while the negative cases had a median volume of 59 mL.
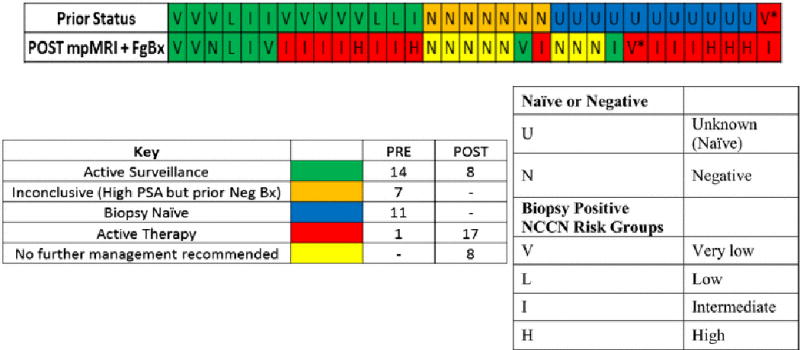
Impact on clinical management
The results of mpMRI and FgBx ultimately changed the clinical management in 27 of 33 patients (81%) with subcapsular lesions. Of the 11 patients who were biopsy naïve prior to FgBx, 7 (63%) became eligible for active therapy [Figure 3], while 3 (27%) were biopsy negative and returned back to watchful waiting, and one patient (9%) was grouped into active surveillance. For the 8 patients who were inconclusive prior to FgBx, 5 (62.5%) were determined to be biopsy negative and required no further management, 2 (25%) were placed under active surveillance, and one patient (12.5%) became eligible for active therapy. In the 13 patients who initially presented while on active surveillance, 8 (61.5%) were recommended for active therapy, while 5 patients (38%) remained on active surveillance. One patient was already recommended for active therapy at time of presentation.
Figure 3.
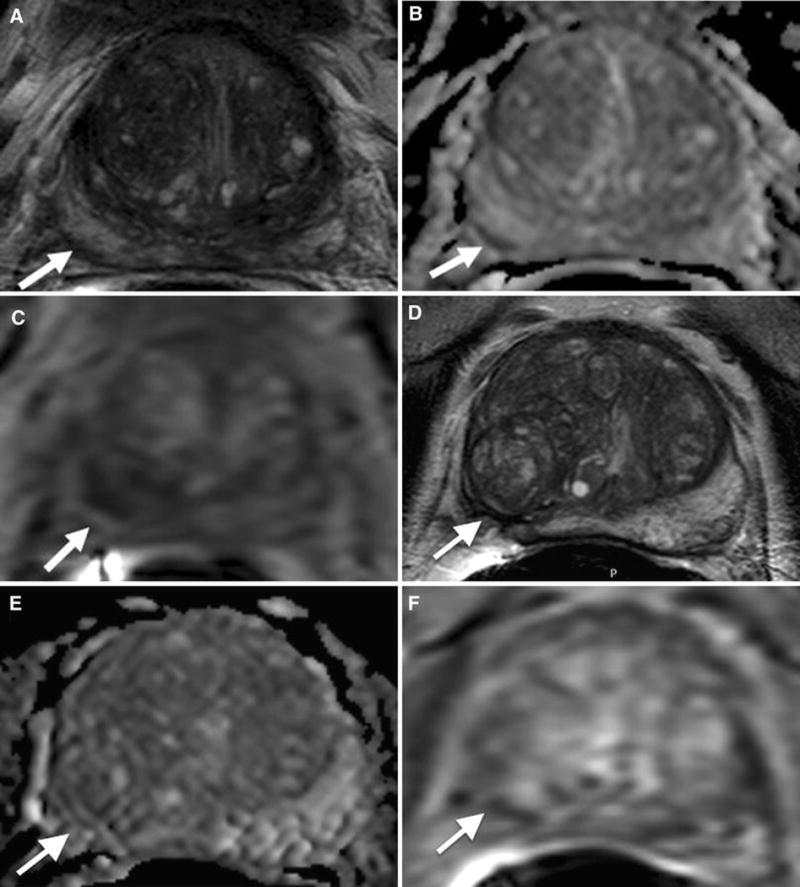
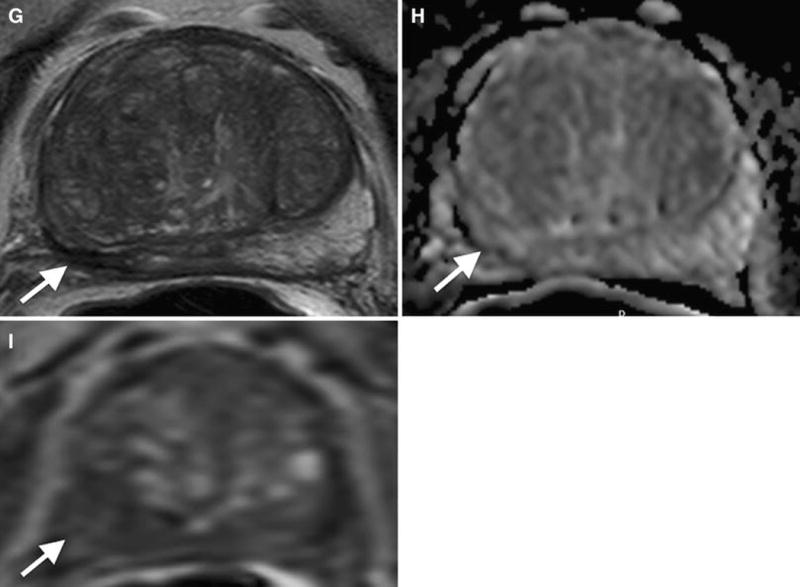
A 58 year old patient, with a PSA of 6.65 ng/mL, with familial history of prostate cancer, and history of two previous negative 12 core TRUS sextant biopsies. Baseline axial T2W MRI shows a right base subcapsular peripheral zone lesion (3a). Axial diffusion weighted image shows a hypointense lesion corresponding to the subcapsular lesion (3b). Axial dynamic contrast enhanced image shows early hyper-enhancement in the right base peripheral zone (3c). Patient elected for focal laser ablation. One year post focal laser ablation (FLA) patient’s axial T2W MRI shows treated area as diffusely hypointense with shrinkage and retraction, representative of necrotic changes (3d). Axial diffusion weighted image no longer shows hypointense features at the site of the subcapsular lesion (3e). Axial dynamic contrast enhanced image shows no focal hyper-enhancement in the treated subcapsular lesion (3f). One year post-FLA follow-up fusion guided biopsy confirmed negative mpMRI findings. Two year post focal laser ablation (FLA) patient’s axial T2W MRI shows treated area as region of resolution and fibrotic changes (3g). Axial diffusion weighted image shows no hypointense features at the site of the subcapsular lesion (3h). Axial dynamic contrast enhanced image shows no focal hyper-enhancement in the treated subcapsular lesion (3i). Two year post-FLA follow-up guided biopsy confirmed negative mpMRI findings.
This effect on clinical management is summarized in Table 6, which also demonstrates the differences in National Comprehensive Cancer Network (NCCN) risk categories. The most up-to-date NCCN guidelines for prostate cancer (Version 1.2015) were used to stratify patients into different risk groups (very low, low, intermediate, and high) at baseline according to outside histopathology results (PRE) and after undergoing mpMRI + FgBx (POST). The NCCN guidelines only apply for patients with confirmed prostate cancer. Thus, the subsets of patients who were biopsy naïve or had inconclusive prior results (negative prior biopsy despite rising PSA) were labeled descriptively in Table 6. We observed that seven patients previously classified as very low- (n=5) or low- (n=2) risk based on outside biopsy results were found to have higher risk disease, and were subsequently categorized in the intermediate- (n=6) or high- (n=1) NCCN risk groups. These seven patients then became eligible for active therapy according to NCCN recommendations for intermediate to high-risk prostate cancer.
Table 6.
Clinical Management
|
Discussion
This study demonstrates that posterior subcapsular lesions can be challenging to diagnose by TRUS biopsy and that multi-parametric MRI with FgBx helps identify these tumors. The value of mpMRI in detecting clinically relevant prostate cancers has been repeatedly demonstrated, however the majority of detected lesions are ovoid or spherical [14, 15]. Much of our understanding of subcapsular lesions comes from a study by Cheng at al. who evaluated low volume tumors on whole mount prostate specimens in 62 radical prostatectomies [16]. The most common location was the posterior half of the prostate (79%), and many of these tumors were subcapsular. Approximately 16% of these lesions had significant components of Gleason 4 suggesting the potential for biologic aggressiveness. Thus, Cheng et al. raised awareness of the potential significance of subcapsular cancers. In our study, elements of Gleason 4 were found in two thirds of confirmed cases. Given the lower rates of Gleason 4 detection with SBx, and upgrading with FgBx, there may be value in using mpMRI with FgBx to better characterize subcapsular cancers. We demonstrated a much higher positive biopsy rate in detecting subcapsular prostate cancer on FgBx (85%) compared to corresponding regions on SBx (30%). While this result may be expected from biopsies specifically targeting those tumors, it also demonstrates that using SBx alone may miss a substantial proportion of subcapsular tumors (70%) due to their peripheral location and a reluctance to biopsy through the capsule. Another finding was that there was a change in clinical management for 27 of the 33 (81%) patients with mpMRI with targeted subcapsular lesions having undergone fusion-guided biopsy. These findings support the need for accurate detection and targeted biopsy to optimize the management strategy of subcapsular prostate cancers.
There was a statistically significant difference in the mpMRI prostate volumes of the biopsy positive and negative cases. Prostates with significant benign prostatic hyperplasia (BPH) will often exhibit a compressed peripheral zone making the subcapsular lesion more difficult to detect which is a possible explanation for this occurence. Smaller prostate glands have repeatedly been shown to have higher diagnostic yields. For instance, Nix, et al. found that very low distal apical cancers of the prostate were more often found in smaller prostates [6]. A study by Walton-Diaz, et al. [17] corroborated this finding, showing that overall detection rate with FgBx was inversely correlated to prostate size. Prostates under 40mL in volume had a detection rate of 71%, whereas prostates 40–55mL in size (i.e. our positive biopsy median), and prostates 55–70mL in volume had detection rates of 57.5% and 46.9%, respectively. It is impossible to know whether BPH lowers the risk of subcapsular cancers or simply masks them. Therefore, it is especially important in larger glands to look for subcapsular lesions.
There are several limitations to this study. The population from which these patients were identified is mostly a referral population and thus, may be weighted toward unusually located lesions. Additionally, since in such a cohort of patients radical prostatectomy is not always performed and whole mount histopathology is therefore not available, we used TRUS and fusion guided biopsy in establishing a definitive diagnosis of our MRI findings. This creates difficulty in our ability to determine false negatives and true negatives. Since these lesions are quite small, and therefore, difficult to biopsy, there may be some underestimation of the rate of cancer. It is interesting to note that two cases whom originally were identified as having subcapsular prostate lesions on mpMRI were initially biopsy negative, but later on were re-biopsied at these target locations and found to be biopsy positive. The reason for the initial false negative is unclear, but may be due to technical limitations of biopsies. Also, endorectal coils were used in this study and may have augmented the detection of subcapsular cancers. It is unclear if such lesions can be as easily detected without an endorectal coil.
In conclusion, our study demonstrates that mpMRI with an endorectal coil can aid in the identification of subcapsular prostate cancers that have evaded diagnosis with conventional strategies. mpMRI + FgBx had a higher biopsy yield compared with the current standard of care SBx and facilitated decision-making about the next steps in management. By recognizing subcapsular cancers earlier and more accurately, patients with these cancers will more quickly get the treatment they need before the development of extracapsular extension.
References
- 1.Prostate Cancer Home Page - National Cancer Institute. 2014 Available from: http://www.cancer.gov/cancertopics/types/prostate.
- 2.George AK, Pinto PA, Rais-Bahrami S. Multiparametric MRI in the PSA Screening Era. BioMed Research International. 2014;2014:465816. doi: 10.1155/2014/465816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Muller BG, et al. Imaging modalities in focal therapy: patient selection, treatment guidance, and follow-up. Curr Opin Urol. 2014;24(3):218–24. doi: 10.1097/MOU.0000000000000041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sankineni S, Osman M, Choyke PL. Functional MRI in Prostate Cancer Detection. Biomed Res Int. 2014;2014:590638. doi: 10.1155/2014/590638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Turkbey B, et al. Documenting the location of prostate biopsies with image fusion. BJU Int. 2011;107(1):53–7. doi: 10.1111/j.1464-410X.2010.09483.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nix JW, et al. Very distal apical prostate tumours: identification on multiparametric MRI at 3 Tesla. BJU Int. 2012;110(11 Pt B):E694–700. doi: 10.1111/j.1464-410X.2012.11503.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ouzzane A, et al. Combined multiparametric MRI and targeted biopsies improve anterior prostate cancer detection, staging, and grading. Urology. 2011;78(6):1356–62. doi: 10.1016/j.urology.2011.06.022. [DOI] [PubMed] [Google Scholar]
- 8.Volkin D, et al. Multiparametric magnetic resonance imaging (MRI) and subsequent MRI/ultrasonography fusion-guided biopsy increase the detection of anteriorly located prostate cancers. BJU Int. 2014;114(6b):E43–9. doi: 10.1111/bju.12670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenkrantz AB, Verma S, Turkbey B. Prostate Cancer: Top Places Where Tumors Hide on Multiparametric MRI. American Journal of Roentgenology. 2015;204(4):W449–56. doi: 10.2214/AJR.14.13280. [DOI] [PubMed] [Google Scholar]
- 10.Barentsz JO, et al. ESUR prostate MR guidelines 2012. Eur Radiol. 2012;22(4):746–57. doi: 10.1007/s00330-011-2377-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Turkbey B, et al. Multiparametric 3T prostate magnetic resonance imaging to detect cancer: histopathological correlation using prostatectomy specimens processed in customized magnetic resonance imaging based molds. J Urol. 2011;186(5):1818–24. doi: 10.1016/j.juro.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pinto PA, et al. Magnetic resonance imaging/ultrasound fusion guided prostate biopsy improves cancer detection following transrectal ultrasound biopsy and correlates with multiparametric magnetic resonance imaging. J Urol. 2011;186(4):1281–5. doi: 10.1016/j.juro.2011.05.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohler JL, et al. Prostate cancer, version 2.2014. J Natl Compr Canc Netw. 2014;12(5):686–718. doi: 10.6004/jnccn.2014.0072. [DOI] [PubMed] [Google Scholar]
- 14.Dianat SS, Carter HB, Macura KJ. Performance of multiparametric magnetic resonance imaging in the evaluation and management of clinically low-risk prostate cancer. Urol Oncol. 2014;32(1):39.e1–10. doi: 10.1016/j.urolonc.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lawrentschuk N, Fleshner NN. The role of magnetic resonance imaging in targeting prostate cancer in patients with previous negative biopsies and elevated prostate-specific antigen levels. BJU Int. 2009;103(6):730–3. doi: 10.1111/j.1464-410X.2008.08205.x. [DOI] [PubMed] [Google Scholar]
- 16.Cheng L. Anatomic distribution and pathologic characterization of small-volume prostate cancer (<0.5 ml) in whole-mount prostatectomy specimens. Mod Pathol. 2005;18(8):1022–6. doi: 10.1038/modpathol.3800431. [DOI] [PubMed] [Google Scholar]
- 17.Walton Diaz A. Can magnetic resonance-ultrasound fusion biopsy improve cancer detection in enlarged prostates? J Urol. 2013;190(6):2020–5. doi: 10.1016/j.juro.2013.05.118. [DOI] [PMC free article] [PubMed] [Google Scholar]


