Abstract
Objective
We performed a pooled analysis to examine cigarette smoking and household passive smoke exposure in relation to the risk of human papillomavirus (HPV) infection and cervical intraepithelial neoplasia grade 2+ (CIN2+).
Methods
Data were pooled from 12 cross-sectional studies for cervical cancer screenings from 10 provinces of China in 1999–2007. A total of 16,422 women were analyzed, along with 2,392 high-risk-HPV (hr-HPV) positive women and 381 CIN2+ cases. Pooled odds ratios (ORs) and 95% confidence intervals (CIs) were estimated using logistic regression models controlling for sexual and non-sexual confounding factors.
Results
There was an excess risk between active smoking and hr-HPV infection and CIN2+. Adjusted OR for ever smokers vs. never smokers was 1.45 (95% CI=1.10–1.91), for hr-HPV infection and 1.89 (95% CI=1.03–3.44), for CIN2+. Passive smoking had a slightly increased risk on the hr-HPV infection with adjusted OR 1.11 (1.00–1.24), but no statistical association was observed between passive smoke exposure and CIN2+. Compared with the neither active nor passive smokers, both active and passive smokers had a 1.57-fold (95% CI=1.14–2.15) increased risk of HPV infection and a 1.99-fold (95% CI=1.02–3.88) risk of CIN2+.
Conclusion
Our large multi-center cross-sectional study found active smoking could increase the risk of overall hr-HPV infection and CIN2+ adjusted by passive smoking and other factors. Passive smoking mildly increased the risk of HPV infection but not the CIN2+. An interaction existed between passive tobacco exposure and active smoking for hr-HPV infection and the CIN2+.
Keywords: Cervical Intraepithelial Neoplasia, Papillomaviridae, Infection, Smoking, Tobacco Smoke Pollution, Chinese, Women
INTRODUCTION
Cervical cancer is the fourth most commonly diagnosed cancer in women worldwide, with developing countries facing the greatest burden of disease: 18/100,000 women per year contract the disease in developing countries, and a disproportionate amount of women die because of this disease [1]. Persistent genital infection with oncogenic human papillomavirus (HPV) appears to be the most important cause of cervical cancer [2,3,4,5], but despite HPV's high prevalence (approximately 12.5% of women) [6], most women clear the virus before it can develop into cancer [7]. Thus, it is important to determine what factors play a role in the HPV infection or the cervical cancer following HPV infection.
Winkelstein first hypothesized in 1977 that smoking could be a risk factor for cervical cancer [8]. International epidemiological analyses have demonstrated that smoking is associated with an increased risk of squamous cell carcinoma [9]. However, the issue remains controversial today. In American cohorts where the female have a relative higher smoking prevalence ranging from 27.8%–32.4% [2,10,11,12], it has been reported that smoking is both protective against HPV infection [13], and conversely, that increased lifetime smoking duration is a risk factor for longer HPV persistence [12]. The female smoking prevalence in Asian studies also varies widely (38.4% in Japan [14], 19.8% in Thailand [15], 7.3% in South Korea [16], and 3.4% in China [17]). In these populations, the effect of smoking on HPV infection has also varied, with odds ratios (ORs) for smokers versus non-smokers ranging from 0.45 to 2.32 (Thailand and South Korea, respectively).
Moreover, the relationship between passive exposure to cigarette smoke and cervical neoplasia is less clear. Investigations conducted by Slattery and Trimble have demonstrated an increased cervical cancer risk among women exposed to passive smoke [10,18]. However, an early study failed to show a consistent association between cervical intraepithelial neoplasia (CIN) and passive smoke exposure [11]. A few studies evaluating passive smoke exposure/active smoking and cervical neoplasia have not been consistent in their findings for limitations including small sample size of non-smoker controls and the status of active and passive history of smoking concurrently, lack of specific information on HPV and sexual behavior, etc.
Our study is a pooled analysis of 12 population-based, cross-sectional studies of cervical cancer across China. This is the largest analysis conducted to date in China, providing a unique opportunity to analyze the relationship between tobacco smoking, high-risk-HPV (hr-HPV) infection, and CIN grade 2+ (CIN2+) prevalence in this population.
MATERIALS AND METHODS
1. Participants
Cervical cancer screenings were conducted in 12 population-based, cross-sectional studies in 10 provinces in the People's Republic of China from 1999–2007 by the Cancer Institute of the Chinese Academy of Medical Sciences (CICAMS), Cleveland Clinic, International Agency for Research on Cancer (IARC), and Program of Appropriate Technology in Health (PATH). The 12 projects names were Shanxi Province Cervical Cancer Screening Study (SPOCCS)1–4, Screening Technologies to Advance Rapid Testing (START)2003–2007, and International Agency for Research on Cancer (IARC)-1–3, respectively. The individual project designs and their specific methods were outlined in detail elsewhere [19,20,21,22,23,24,25,26], but to summarize, eligible women were sexually active, not pregnant, had an intact uterus, and had no history of CIN, cervical cancer, or pelvic irradiation. Written informed consent was obtained from all women. The human subjects review boards of CICAMS, Cleveland Clinic, PATH, or IARC approved these studies.
2. Procedures
Questionnaires that included information on socio-demographic characteristics, smoking history, reproductive history, menstrual factors, oral contraceptive use, and sexual behavior were administered by trained interviewers to study participants face-to-face. Questions on smoking habits included status of active (never, former, or current smoker [ever smoker]) and passive smoking (yes, no). Ever active smoker was defined as someone who reported any type of smoking for at least 6 months prior to the interview and included former and current smokers; passive smoker was defined as someone who lived in the same home as a smoking relative for 6 or more months. The gynecological examinations, specimen collection, cytology, and HPV DNA detection techniques have been described in the individual studies [20,21]. All HPV tests were based on hr-HPV DNA detection by Hybrid Capture 2 (HC2) assay (Qiagen, Gaithersburg, MD, USA) [25].
3. Statistical analysis
Unconditional logistic regression was used to estimate the ORs and the corresponding 95% confidence intervals (CIs) of hr-HPV infection and CIN2+ based on smoking history. When calculating the ORs risk for CIN2+ and smoking status, the maximum likelihood estimates failed because the cell counts were small or zero in some studies; in these cases, exact logistic regression was used for analysis. Heterogeneity of the ORs among individual studies was tested using the χ2 based Cochran's Q statistic and the I2 statistic, and if the p-value was less than 0.05 and I2 less than 50%, there was no heterogeneity in the studies, or else a random effect model will be used for analysis.
The logistic models were constructed and adjusted by sexual and non-sexual confounding factors. Potential confounders included in these analyses were age (17–35, 36–49, ≥50), geographic area (rural, urban), education level (illiterate and primary school, middle school and above), age at menarche (≤15, ≥16), age at sexual debut (≤20, ≥21), lifetime number of sexual partners (1, ≥2), menopause (yes, no), parity (0, 1–2, ≥3), intrauterine device (IUD) (yes, no), oral contraceptives (yes, no), condoms (yes, no), sterilization (yes, no), husband had extramarital affair (yes, no) and passive smoking (yes, no). The models of CIN2+ prevalence were also adjusted for HPV infection status (+,−). Results were displayed in graphs with small diamonds and horizontal lines, representing the individual ORs and their corresponding 95% CIs respectively, while a bigger diamond was used to plot the overall OR for the pooled together. The individual women with the missing values were included by creating a category for “missing” for the relevant variable in order to avoid the exclusion of participants in the logistic regressions.
The interaction between active smoking or passive tobacco exposure was assessed for hr-HPV infection and CIN2+, the interactions were tested using likelihood ratio tests based on models with and without the interaction term(s). Linear trend chi-square tests were used to the homogeneity of the relationship between HPV infection and CIN2+ and the different smoking status (neither active nor passive smoking, only passive smoking, only active smoking, both active and passive smoking). Statistical analyses were performed using SAS 9.2 (SAS Institute Inc., Cary, NC, USA) and Stata 12.0 (StataCorp. LLC, College Station, TX, USA).
RESULTS
Data from 12 population-based cervical cancer screening studies was pooled to analyze the relationship between smoking status, hr-HPV infection, and risk of CIN2+. A total of 17,582 women from 12 individual studies were included for this pooled study initially, and after excluding some due to inadequate HPV results, lack of smoking status or/and incomplete outcome data, and 16,422 women remained for the final analysis in relation to the hr-HPV infection and 15,791 in relation to the CIN2+.
Table 1 presents tobacco exposure and the prevalence of hr-HPV infection and CIN2+ in both the 12 individual studies and pooled overall. Women in the individual studies had a similar average age (ranging from 35.8 to 43.4 years old). The relatively low rates of ever smokers and higher rates of passive smokers were listed for each study. Five studies (SPOCCSIII-3, START2004, START2005, START2006, and IARC-1) reported an ever smoker rate of less than 1%, while most studies except IARC-2 (42.7%) reported a passive smoker rate of over 63.0%. The pooled rates of ever smokers and passive smokers were 1.9% and 73.7%, respectively. All studies except START2005 found a hr-HPV infection rate greater than 12%, resulting in a pooled HPV infection rate of 14.6%. CIN2+ prevalence in the individual studies ranged from 1.2% to 4.4%, with a pooled rate of 2.3%. Furthermore, the more specific number of active and passive smokers in the hr-HPV infection and and CIN2+ in each site were also shown in the the Supplementary Table 1.
Table 1. Tobacco exposure and prevalence of HPV and CIN2+ in 12 population-based cervical cancer screening studies.
| Study | Study year; location | No. | Age range | Age, mean±SD | Ever smokers, No. (%) | Passive smokers, No. (%) | HPV prevalence, No. (%) | CIN2+ prevalence, No. (%) |
|---|---|---|---|---|---|---|---|---|
| SPOCCSIII-1 | 2006; Xiangyuan county, Shanxi province | 883 | 19−54 | 37.0±9.9 | 30 (3.4) | 706 (80.0) | 140 (15.9) | 22 (2.5) |
| SPOCCSIII-2 | 2006; Beijing city | 792 | 18−54 | 38.5±9.2 | 49 (6.2) | 514 (64.9) | 110 (13.9) | 9 (1.1) |
| SPOCCSIII-3 | 2006; Xinmi, Henan province | 864 | 20−54 | 37.2±9.8 | 3 (0.3) | 654 (75.7) | 107 (12.4) | 10 (1.2) |
| SPOCCSIII-4 | 2007; Shanghai city | 771 | 19−55 | 39.0±9.2 | 30 (3.9) | 535 (69.4) | 102 (13.2) | 11 (1.5) |
| START2003 | 2003; Xiangyuan county, Shanxi province | 1,817 | 29−50 | 38.0±5.6 | 75 (4.1) | 1,558 (85.7) | 332 (18.3) | 70 (3.9) |
| START2004 | 2004; Xiushui county, Jiangxi province | 1,625 | 29−49 | 39.4±5.4 | 4 (0.2) | 1,035 (63.7) | 306 (18.8) | 61 (4.1) |
| START2005 | 2005; Wudu county, Gansu province | 2,052 | 29−49 | 38.4±5.0 | 2 (0.1) | 1,666 (81.2) | 162 (7.9) | 32 (1.6) |
| START2006 | 2006; Qinxian county, Shanxi province | 2,500 | 29−55 | 41.4±5.8 | 19 (0.8) | 1,910 (76.4) | 305 (12.2) | 39 (1.6) |
| START2007 | 2007; Xiangyuan and Wuxiang county, Shanxi province | 2,528 | 30−55 | 43.4±6.1 | 30 (1.2) | 2,029 (80.3) | 402 (15.9) | 70 (2.9) |
| IARC-1 | 2004; Yangcheng county, Shanxi province | 745 | 19−59 | 40.8±10.7 | 0 (0.0) | 533 (71.5) | 119 (16.0) | 32 (4.4) |
| IARC-2 | 2005; Shenzhen city, Guangdong province | 1,137 | 17−59 | 35.8±9.2 | 20 (1.8) | 486 (42.7) | 159 (14.0) | 14 (1.3) |
| IARC-3 | 2005; Shenyang city, Dongbei province | 708 | 17−59 | 41.2±10.4 | 48 (6.8) | 475 (67.1) | 148 (20.9) | 11 (1.6) |
| Total | 16,422 | 17−59 | 39.6±7.7 | 310 (1.9) | 12,101 (73.7) | 2,392 (14.6) | 381 (2.3)* |
CIN2+, cervical intraepithelial neoplasia grade 2 or worse; HPV, human papillomavirus; IARC, International Agency for Research on Cancer; SD, standard deviation; SPOCCS, Shanxi Province Cervical Cancer Screening Study; START, Screening Technologies to Advance Rapid Testing.
*There were 15,791 women with complete pathology results.
Table 2 shows baseline characteristics for never smokers vs. ever smokers and passive vs. non-passive smokers in the pooled study. When compared to never smokers, ever smokers were more civic women. They were more likely to have a high educational level, to have had early sexual debut, to be post-menopausal and nulliparous, to have had multiple sexual partners and husbands with extramarital affairs, to use oral contraceptives, condoms or IUD rather than sterilization, to also be passive smokers, and to have hr-HPV or CIN2+. Compared to non-passive smokers, passive smokers were more likely to be between the ages of 36 and 49 years, to be from rural areas, to have a lower education level, to have had late age of menarche and early sexual debut, to be premenopausal, to have had multiple sexual partners and more than 3 parities, to use sterilization as a contraceptive, and to have HPV. Similarly, the associations between these baseline characteristics and the hr-HPV infection and CIN2+ were also evaluated, which additionally provided information on the potential confounding factors shown in the Supplementary Table 2.
Table 2. Baseline characteristics of women in pooled analysis, based on active or passive smoking status.
| Characteristics | Active smoking | Passive smoking | |||||
|---|---|---|---|---|---|---|---|
| Never smoker | Ever smoker | p-value | No | Yes | p-value | ||
| No. of subjects | 16,112 | 310 | 4,321 | 12,101 | |||
| Age (yr) | 0.103 | <0.001 | |||||
| 17–35 | 5,089 (31.6) | 84 (27.1) | 1,477 (34.2) | 3,696 (30.5) | |||
| 36–49 | 9,359 (58.1) | 185 (59.7) | 2,328 (53.9) | 7,216 (59.6) | |||
| ≥50 | 1,664 (10.3) | 41 (13.2) | 516 (11.9) | 1,189 (9.8) | |||
| Geographic area | <0.001 | <0.001 | |||||
| Rural | 12,851 (79.8) | 163 (52.6) | 2,923 (67.7) | 10,091 (83.4) | |||
| Urban | 3,261 (20.2) | 147 (47.4) | 1,398 (32.3) | 2,010 (16.6) | |||
| Education level | 0.006 | <0.001 | |||||
| Illiterate and primary school | 6,766 (42.0) | 106 (34.2) | 1,565 (36.2) | 5,307 (43.9) | |||
| Middle school and above | 9,346 (58.0) | 204 (65.8) | 2,756 (63.8) | 6,794 (56.1) | |||
| Age at menarche | 0.426 | <0.001 | |||||
| ≤15 | 9,095 (56.4) | 182 (58.7) | 2,575 (59.6) | 6,702 (55.4) | |||
| ≥16 | 7,017 (43.6) | 128 (41.3) | 1,746 (40.4) | 5,399 (44.6) | |||
| Age at sexual debut | 0.003 | <0.001 | |||||
| ≤20 | 7,681 (47.7) | 174 (56.1) | 1,819 (42.1) | 6,036 (49.9) | |||
| ≥21 | 8,431 (52.3) | 136 (43.9) | 2,502 (57.9) | 6,065 (50.1) | |||
| Menopause* | 0.014 | 0.006 | |||||
| Yes | 1,650 (10.3) | 45 (14.6) | 494 (11.5) | 1,201 (10.0) | |||
| No | 14,414 (89.7) | 264 (85.4) | 3,818 (88.5) | 10,860 (90.0) | |||
| Lifetime No. of sexual partners* | <0.001 | 0.026 | |||||
| 1 | 13,734 (85.3) | 187 (60.3) | 3,709 (85.9) | 10,212 (84.4) | |||
| ≥2 | 2,370 (14.7) | 123 (39.7) | 611 (14.1) | 1,882 (15.6) | |||
| Parity* | <0.001 | <0.001 | |||||
| 0 | 385 (2.4) | 23 (7.6) | 137 (3.3) | 271 (2.3) | |||
| 1−2 | 10,700 (67.6) | 201 (66.6) | 2,930 (70.2) | 7,971 (66.6) | |||
| ≥3 | 4,754 (30.0) | 78 (25.8) | 1,106 (26.5) | 3,726 (31.1) | |||
| Contraceptive use* | |||||||
| Oral contraceptives | 500 (3.1) | 29 (9.4) | <0.001 | 185 (4.3) | 344 (2.8) | <0.001 | |
| Condoms | 1,873 (11.6) | 67 (21.6) | <0.001 | 824 (19.1) | 1,116 (9.2) | <0.001 | |
| IUD | 3,921 (24.3) | 100 (32.3) | 0.001 | 1,195 (27.7) | 2,826 (23.4) | <0.001 | |
| Sterilization | 10,092 (62.6) | 150 (48.4) | <0.001 | 2,265 (52.4) | 7,977 (65.9) | <0.001 | |
| Husband's extramarital affair | <0.001 | 0.462 | |||||
| Yes | 1,344 (8.3) | 80 (25.8) | 363 (8.4) | 1,061 (8.8) | |||
| No | 14,768 (91.7) | 230 (74.2) | 3,958 (91.6) | 11,040 (91.2) | |||
| HPV positive | 2,321 (14.4) | 71 (22.7) | <0.001 | 585 (13.5) | 1,807 (14.9) | 0.026 | |
| CIN2+* | 366 (2.4) | 15 (5.1) | 0.003 | 99 (2.4) | 282 (2.4) | 0.854 | |
| Passive smoking | <0.001 | ||||||
| Yes | 11,842 (73.5) | 259 (83.5) | |||||
| No | 4,270 (26.5) | 51 (16.5) | |||||
Values are presented as number of subjects (%).
CIN2+, cervical intraepithelial neoplasia grade 2 or worse; HPV, human papillomavirus; IUD, intrauterine device.
*Smaller sample size than categorical groups due to missing values.
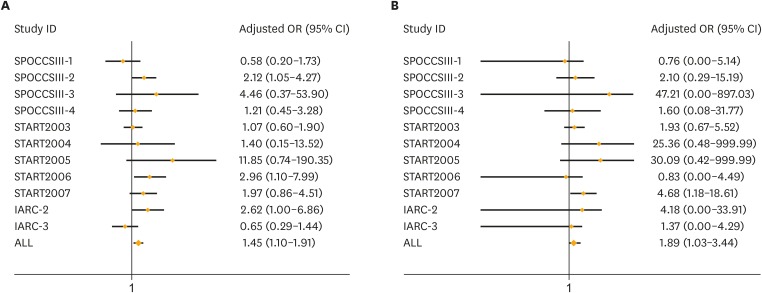
Fig. 1 displays adjusted ORs and 95% CIs for the relationship between active smoking and risk of HPV infection and CIN2+. There were no significant heterogeneity detected for the ORs between active smoking and HPV infection (I2=38%; p=0.100) or the CIN2+ (I2=12%; p=0.330) in each study. Active smokers had a statistically significant increased risk of HPV infection and CIN2+ than never smokers in pooled analyses. As showed in the part A and B of the Fig. 1, after being adjusted by multivariate, the relative likelihoods of both HPV infection and CIN2+ for ever smokers were statistically significant (OR=1.45; 95% CI=1.10–1.91, for HPV infection; OR=1.89; 95% CI=1.03–3.44, for CIN2+). However, a low active smoking rate and a limited number of CIN2+ cases in some individual studies led to wide and unstable 95% CIs of ORs.
Fig. 1.
Adjusted ORs and 95% CIs for the relationships between active smoking and risk of HPV infection (A) and CIN2+ (B) in the individual and pooled studies. (A) Logistic models were adjusted by age, area, education, age at menarche, age at sexual debut, sexual partners, menopause, parity, intrauterine device, oral contraceptives, condoms, sterilization, husband's affair, active, and passive smoking mutually; (B) Logistic-models were additionally adjusted for HPV infection.
CI, confidence interval; CIN2+, cervical intraepithelial neoplasia grade 2 or worse; HPV, human papillomavirus; IARC, International Agency for Research on Cancer; OR, odds ratio; SPOCCS, Shanxi Province Cervical Cancer Screening Study; START, Screening Technologies to Advance Rapid Testing.
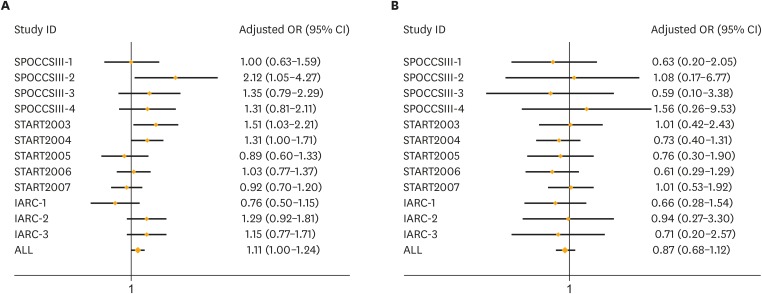
Fig. 2 shows the associations between passive smoking and risk of HPV and CIN2+ in individual and pooled studies. There were also no significant heterogeneity detected between passive smoking and HPV infection (I2=39%; p=0.080) or the CIN2+ (I2=0%; p=0.740). In the adjusted logistic models, passive and active tobacco exposures were adjusted mutually. Higher exposure to a smoking environment was slightly associated with a higher risk of HPV infection in the pooled study. Pooled OR and 95% CI for HPV infection was 1.11 (1.00–1.24) which was showed in the part A of the Fig. 2. No statistically significant association was found between passive smoking and risk of CIN2+ in the pooled analysis. The overall adjusted OR was 0.87 (0.68–1.12).
Fig. 2.
Adjusted ORs and 95% CIs for the relationships between passive smoking and risk of HPV infection (A) and CIN2+ (B) in the individual and pooled studies. (A) Logistic models were adjusted by age, area, education, age at menarche, age at sexual debut, sexual partners, menopause, parity, intrauterine device, oral contraceptives, condoms, sterilization, husband's affair, active, and passive smoking mutually; (B) Logistic-models were additionally adjusted for HPV infection.
CI, confidence interval; CIN2+, cervical intraepithelial neoplasia grade 2 or worse; HPV, human papillomavirus; IARC, International Agency for Research on Cancer; OR, odds ratio; SPOCCS, Shanxi Province Cervical Cancer Screening Study; START, Screening Technologies to Advance Rapid Testing.
Table 3 presents multivariable ORs and 95% CIs for the associations between active smoking and risk of HPV infection and CIN2+ in the pooled analysis, stratified by passive smoking status. Passive smokers were more likely than non-passive smokers to be ever smokers, to have hr-HPV or CIN2+. Among passive smokers, the risk of hr-HPV infection (OR=1.39; 95% CI=1.03–1.89) and CIN2+ (OR=2.39; 95% CI=1.26–4.54) were significantly associated with active tobacco use, while no statistically significant association was observed among non-passive smokers. A significantly statistical interaction was found between active smoking and passive smoking in hr-HPV (p<0.001) and CIN2+ models (p<0.001). Joint ORs were also calculated by the adjusted regressions in order to evaluate the associations between 4 different combinations of active or passive smoking status with hr-HPV infection and CIN2+ in the Table 4. Compared with the neither active nor passive smokers, both active and passive smokers had a 1.57-fold (95% CI=1.14–2.15) increased risk of HPV infection and a 1.99-fold (95% CI=1.02–3.88) risk of CIN2+. There was a significant increased trend of the hr-HPV infection among the non-smokers, only passive smokers, only active smokers and both smokers (p<0.001), while there were still no significant trend between smoking and CIN2+ (p=0.086).
Table 3. Adjusted ORs and 95% CIs between active smoking and risk of hr-HPV infection and CIN2+ by passive smoking status in the pooled study.
| Passive smoking | Active smoking | hr-HPV infection | CIN2+ | ||
|---|---|---|---|---|---|
| Prevalence, No. (%) | Adjusted OR* (95% CI) | Prevalence, No. (%) | Adjusted OR* (95% CI) | ||
| No | No | 573/4,270 (13.42) | Reference | 98/4,118 (2.38) | Reference |
| Yes | 12/51 (23.53) | 1.60 (0.82–3.11) | 1/50 (2.00) | 0.46 (0.06–3.66) | |
| Yes | No | 1,748/11,842 (14.76) | Reference | 268/11,378 (2.35) | Reference |
| Yes | 59/259 (22.78) | 1.39 (1.03–1.89) | 14/245 (5.71) | 2.39 (1.26–4.54) | |
P for interaction between the passive and active smoking status: hr-HPV infection (p<0.001) and CIN2+ (p<0.001).
CI, confidence interval; CIN2+, cervical intraepithelial neoplasia grade 2 or worse; hr-HPV, high-risk-human papillomavirus; OR, odds ratio.
*Logistic models were adjusted by age, area, education, age at menarche, age at sexual debut, sexual partners, menopause, parity, intrauterine device, oral contraceptives, condoms, sterilization, husband's affair, and active smoking, whereas CIN2+ models were additionally adjusted for HPV infection status.
Table 4. Adjusted ORs and 95% CIs between 4 different combinations of active or passive smoking status with hr-HPV infection and CIN2+ in the pooled study.
| Joint smoking status | hr-HPV infection | CIN2+ |
|---|---|---|
| Neither active nor passive smoking | Reference | Reference |
| Only passive smoking | 1.12 (1.01–1.24) | 0.80 (0.62–1.04) |
| Only active smoking | 1.54 (0.80–2.99) | 0.43 (0.06–3.40) |
| Both active and passive smoking | 1.57 (1.14–2.15) | 1.99 (1.02–3.88) |
| p-trend | <0.001 | 0.086 |
Values are presented as adjusted OR (95% CI).
CI, confidence interval; CIN2+, cervical intraepithelial neoplasia grade 2 or worse; hr-HPV, high-risk-human papillomavirus; OR, odds ratio.
*Logistic models were adjusted by age, area, education, age at menarche, age at sexual debut, sexual partners, menopause, parity, intrauterine device, oral contraceptives, condoms, sterilization, husband's affair, and joint smoking status, whereas CIN2+ models were additionally adjusted for HPV infection status.
DISCUSSION
This large multi-center cross-sectional study found a statistically significant association between active smoking and overall HPV or CIN2+ prevalence in the presence of passive smoking; a slightly significant association between passive smoking and overall HPV infection; and no association between passive smoking and CIN2+ regardless of active smoking status. Significant associations between active smoking and HPV infection and CIN2+ were observed among passive smokers. These results are based on the hypothesis that hr-HPV infection and CIN2+ have similar risk factors considering that hr-HPV infection is a necessary precursor of cervical cancer.
A controversial issue is becoming clear: smoking is certainly an independent risk factor of cervical cancer. A similar study conducted a pooled analysis of IARC multi-centric case-control studies and showed that ever-smokers had an excess risk of cervical cancer that persisted even after controlling for the strong effect of HPV and for other potential cofactors in the progression from infection to cancer [27]. Another large multinational and longitudinal cohort study prospectively assessed the role of tobacco smoking on the risk of developing intercultural communicative competence (ICC) and pre-cancer and confirmed the role of tobacco smoking as an important risk factor for both CIN3/carcinoma in situ (CIS) and ICC after taking into account HPV exposure (as determined by HPV serology). The low level of smoking in Chinese populations limited our ability to study the association between tobacco smoking and CIN3+/squamous cell carcinoma (SCC), but these and other studies have shown the magnitude of this association causes as much as a 2-fold increase in risk of either CINs or SCC/ICC [28,29,30,31]. The causes or mechanisms of this phenomenon are still unclear, but many studies have focused on tobacco-related carcinogens including nicotine, cotinine, benzo[a]pyrene, and 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone [32,33,34,35]. Given the importance of HPV infection in the progression of the cervical cancer, our study explored the role of tobacco on the risk of contracting HPV, and it showed that active smoking produced a 1.45-fold increased risk of contracting HPV, but after adjusting for HPV status and sexual behavior risk factors, the risk of CIN2+ increased to 1.89-fold, indicating that tobacco is related to CIN2+ partly because it increases the rate of HPV infection. There may be residual confounding that is responsible for these findings; for example, another study suggested that smoking could appear to increase the risk of acquiring a cervical HPV infection, because of the confounding effect of risky sexual behavior, which is strongly correlated with smoking [36].
The risks of HPV infection and CIN2+ for passive smokers were estimated by the similar confounding including the active smoking, but the risks were different with those for active smokers. Passive smoking mildly increased the risk of HPV infection but not the risk of CIN2+ following infection; this may be because passive smokers who test HPV positive at one time are more likely to clear their infections, whereas CIN2+ cases develop from persistent infection. However, the interaction between passive and active smoking was statistically significant; that is, active smokers who are also passive smokers have an even higher risk of HPV or CIN2+ than active smokers who are not exposed to secondhand smoke. However, few studies reported the active smoking, passive smoking and HPV infection. Consistent with our study, the pooled data from the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort showed active smoking was a definite risk factor on cervical lesions, but passive smoking could not be detected as an independent risk factor in the absence of active smoking [28,37]. Another community-based case-control study found second-smokers had no significant risk compared with non-smokers, but second-smokers with a lifetime exposure of more than 20 pack-year cigarettes had a 7-fold increased risk (adjusted OR [95% CI]=7.2 [2.5–20.6]) [38]. Additionally, a study with high-grade squamous intraepithelial lesion (HSIL)/low-grade squamous intraepithelial lesions (LSIL) as the main outcome found the African-American women with a passive smoke exposure for more than 1 year had a elevated risk compared with the never exposure (adjusted OR [95% CI]=1.5 [1.0–2.2]), but the White women did not have the same results (adjusted OR [95% CI]=1.4 [0.7–2.8]) [39]. Due to the limited number of cancer cases, further large epidemiological studies, including more cervical cancer and pre-cancer cases, are needed to confirm these results.
The major strengths of our study were its large size and the use of similar questionnaires across individual studies such that important risk factors could all be adjusted in the same way. However, our study also has some limitations. First, smoking behavior was based on self-report in questionnaires rather than by detection of cotinine level, but agreement between self-report and urine cotinine level tended to be high (kappa=0.872) [40]. Secondly, we did not collect information about second-hand smoke from the workplace or other locations, only smoke from family members living together. Thus, neither the duration nor the intensity of passive smoking could be estimated, and the dose-dependent relationship could not be obtained. Thirdly, active smokers were not divided between those who purchased commercial cigarettes and those who smoked home-grown tobacco leaf (although the proportion of the home-grown tobacco smokers was low), but as the various additives in commercial cigarettes may cause additional harm to the health, this study may have underestimated the risk of the tobacco. Fourthly, HPV result in the pooled analysis was based on the detection by HC2 test, which cannot discriminate individual genotype, the effects of the smoking on the risk of the specific hr-HPV infection cannot be evaluated in our study. Finally, our study was based on a relatively small number of ever smokers, especially in each individual study, so our results may have been skewed by a few smokers.
Overall, this large, cross-sectional study shows a significant association between the risks of HPV infection and CIN2+ and active smoking. However, our results suggest a hazardous effect of active smoking against risk of cervical cancer who is both active and passive smokers. However, given the low rate of active smoking, principally by prevalence of the CIN3+ or SCC, larger sample size studies with more active smokers and HPV/CIN2+ cases are needed to elucidate the roles of active and passive tobacco smoking in the etiology of cervical cancer.
Since smoking is a modifiable health behavior, considerable public health benefit can be derived from availing ourselves of early opportunities for prevention and control, so the anti-smoking campaign and regulations launched by relative department in local area currently is really a good beginning.
ACKNOWLEDGMENTS
We thank the local doctors and the women who participated in our study from Beijing, Gansu, Guangdong, Jiangsu, Jiangxi, Henan, Shanghai, Shanxi, and Xinjiang, as well as the Bill & Melinda Gates Foundation, the International Agency for Research on Cancer, and the Cleveland Clinic for their generous support.
Footnotes
Funding: This work was funded by the grant from the National Natural Science Foundation of China (81322040, 8140120533) and Basic Research Grant from Cancer Hospital, Chinese Academy of Medical Sciences (CAMS) (JK2013A19).
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
The abstract has been showed in the IARC 50th Anniversary Conference: Global Cancer: Occurrence, Causes, and Avenues to Prevention on 7–10 June 2016 in Centre de Congrès Lyon, France.
- Conceptualization: F.R.M., H.S.Y., Z.F.H., Z.R., W.A.I., Q.Y.L.
- Data curation: F.R.M.
- Formal analysis: F.R.M., Z.R.
- Funding acquisition: Z.F.H.
- Investigation: H.S.Y., Z.F.H., Z.R., Z.X., Q.Y.L.
- Methodology: F.R.M., H.S.Y., Z.R.
- Project administration: Z.F.H., Q.Y.L.
- Resources: Z.F.H., Z.X., Q.Y.L.
- Software: F.R.M.
- Supervision: Q.Y.L.
- Validation: F.R.M., H.S.Y.
- Visualization: F.R.M.
- Writing - original draft: F.R.M., H.S.Y., Z.R., W.A.I.
- Writing - review & editing: F.R.M., H.S.Y., Q.Y.L.
Supplementary Materials
Real numbers of active and passive smoking and the HPV infection and CIN2+ in each site after adjustment in the pooled analysis
Associations with the HPV infection and CIN2+: ORs and 95% CIs of being HPV infection and CIN2+ women according to potential confounding factors
References
- 1.Arbyn M, Castellsagué X, de Sanjosé S, Bruni L, Saraiya M, Bray F, et al. Worldwide burden of cervical cancer in 2008. Ann Oncol. 2011;22:2675–2686. doi: 10.1093/annonc/mdr015. [DOI] [PubMed] [Google Scholar]
- 2.Schiffman MH, Bauer HM, Hoover RN, Glass AG, Cadell DM, Rush BB, et al. Epidemiologic evidence showing that human papillomavirus infection causes most cervical intraepithelial neoplasia. J Natl Cancer Inst. 1993;85:958–964. doi: 10.1093/jnci/85.12.958. [DOI] [PubMed] [Google Scholar]
- 3.Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189:12–19. doi: 10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 4.Vaccarella S, Franceschi S, Herrero R, Muñoz N, Snijders PJ, Clifford GM, et al. Sexual behavior, condom use, and human papillomavirus: pooled analysis of the IARC human papillomavirus prevalence surveys. Cancer Epidemiol Biomarkers Prev. 2006;15:326–333. doi: 10.1158/1055-9965.EPI-05-0577. [DOI] [PubMed] [Google Scholar]
- 5.IARC Working Group on the Evaluation of Carcinogenic Risks to Humans Human papillomaviruses. IARC Monogr Eval Carcinog Risks Hum. 2007;90:1–636. [PMC free article] [PubMed] [Google Scholar]
- 6.Vaccarella S, Herrero R, Snijders PJ, Dai M, Thomas JO, Hieu NT, et al. Smoking and human papillomavirus infection: pooled analysis of the International Agency for Research on Cancer HPV Prevalence Surveys. Int J Epidemiol. 2008;37:536–546. doi: 10.1093/ije/dyn033. [DOI] [PubMed] [Google Scholar]
- 7.Hildesheim A, Schiffman MH, Gravitt PE, Glass AG, Greer CE, Zhang T, et al. Persistence of type-specific human papillomavirus infection among cytologically normal women. J Infect Dis. 1994;169:235–240. doi: 10.1093/infdis/169.2.235. [DOI] [PubMed] [Google Scholar]
- 8.Winkelstein W., Jr Smoking and cancer of the uterine cervix: hypothesis. Am J Epidemiol. 1977;106:257–259. doi: 10.1093/oxfordjournals.aje.a112460. [DOI] [PubMed] [Google Scholar]
- 9.Appleby P, Beral V, Berrington de González A, Colin D, Franceschi S, Goodill A, et al. Carcinoma of the cervix and tobacco smoking: collaborative reanalysis of individual data on 13,541 women with carcinoma of the cervix and 23,017 women without carcinoma of the cervix from 23 epidemiological studies. Int J Cancer. 2006;118:1481–1495. doi: 10.1002/ijc.21493. [DOI] [PubMed] [Google Scholar]
- 10.Slattery ML, Robison LM, Schuman KL, French TK, Abbott TM, Overall JC, Jr, et al. Cigarette smoking and exposure to passive smoke are risk factors for cervical cancer. JAMA. 1989;261:1593–1598. [PubMed] [Google Scholar]
- 11.Coker AL, Rosenberg AJ, McCann MF, Hulka BS. Active and passive cigarette smoke exposure and cervical intraepithelial neoplasia. Cancer Epidemiol Biomarkers Prev. 1992;1:349–356. [PubMed] [Google Scholar]
- 12.Giuliano AR, Sedjo RL, Roe DJ, Harri R, Baldwi S, Papenfuss MR, et al. Clearance of oncogenic human papillomavirus (HPV) infection: effect of smoking (United States) Cancer Causes Control. 2002;13:839–846. doi: 10.1023/a:1020668232219. [DOI] [PubMed] [Google Scholar]
- 13.Ho GY, Bierman R, Beardsley L, Chang CJ, Burk RD. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med. 1998;338:423–428. doi: 10.1056/NEJM199802123380703. [DOI] [PubMed] [Google Scholar]
- 14.Fujita M, Tase T, Kakugawa Y, Hoshi S, Nishino Y, Nagase S, et al. Smoking, earlier menarche and low parity as independent risk factors for gynecologic cancers in Japanese: a case-control study. Tohoku J Exp Med. 2008;216:297–307. doi: 10.1620/tjem.216.297. [DOI] [PubMed] [Google Scholar]
- 15.Sukvirach S, Smith JS, Tunsakul S, Muñoz N, Kesararat V, Opasatian O, et al. Population-based human papillomavirus prevalence in Lampang and Songkla, Thailand. J Infect Dis. 2003;187:1246–1256. doi: 10.1086/373901. [DOI] [PubMed] [Google Scholar]
- 16.Shin HR, Lee DH, Herrero R, Smith JS, Vaccarella S, Hong SH, et al. Prevalence of human papillomavirus infection in women in Busan, South Korea. Int J Cancer. 2003;103:413–421. doi: 10.1002/ijc.10825. [DOI] [PubMed] [Google Scholar]
- 17.Zhao FH, Forman MR, Belinson J, Shen YH, Graubard BI, Patel AC, et al. Risk factors for HPV infection and cervical cancer among unscreened women in a high-risk rural area of China. Int J Cancer. 2006;118:442–448. doi: 10.1002/ijc.21327. [DOI] [PubMed] [Google Scholar]
- 18.Trimble CL, Genkinger JM, Burke AE, Hoffman SC, Helzlsouer KJ, Diener-West M, et al. Active and passive cigarette smoking and the risk of cervical neoplasia. Obstet Gynecol. 2005;105:174–181. doi: 10.1097/01.AOG.0000148268.43584.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Belinson JL, Pretorius RG, Zhang WH, Wu LY, Qiao YL, Elson P. Cervical cancer screening by simple visual inspection after acetic acid. Obstet Gynecol. 2001;98:441–444. doi: 10.1016/s0029-7844(01)01454-5. [DOI] [PubMed] [Google Scholar]
- 20.Belinson JL, Qiao YL, Pretorius RG, Zhang WH, Rong SD, Huang MN, et al. Shanxi Province cervical cancer screening study II: self-sampling for high-risk human papillomavirus compared to direct sampling for human papillomavirus and liquid based cervical cytology. Int J Gynecol Cancer. 2003;13:819–826. doi: 10.1111/j.1525-1438.2003.13611.x. [DOI] [PubMed] [Google Scholar]
- 21.Pan Q, Belinson JL, Li L, Pretorius RG, Qiao YL, Zhang WH, et al. A thin-layer, liquid-based pap test for mass screening in an area of China with a high incidence of cervical carcinoma. A cross-sectional, comparative study. Acta Cytol. 2003;47:45–50. doi: 10.1159/000326474. [DOI] [PubMed] [Google Scholar]
- 22.Pretorius RG, Kim RJ, Belinson JL, Elson P, Qiao YL. Inflation of sensitivity of cervical cancer screening tests secondary to correlated error in colposcopy. J Low Genit Tract Dis. 2006;10:5–9. doi: 10.1097/01.lgt.0000192694.85549.3d. [DOI] [PubMed] [Google Scholar]
- 23.Dai M, Bao YP, Li N, Clifford GM, Vaccarella S, Snijders PJ, et al. Human papillomavirus infection in Shanxi Province, People's Republic of China: a population-based study. Br J Cancer. 2006;95:96–101. doi: 10.1038/sj.bjc.6603208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pretorius RG, Zhang WH, Belinson JL, Huang MN, Wu LY, Zhang X, et al. Colposcopically directed biopsy, random cervical biopsy, and endocervical curettage in the diagnosis of cervical intraepithelial neoplasia II or worse. Am J Obstet Gynecol. 2004;191:430–434. doi: 10.1016/j.ajog.2004.02.065. [DOI] [PubMed] [Google Scholar]
- 25.Zhao FH, Lin MJ, Chen F, Hu SY, Zhang R, Belinson JL. Performance of high-risk human papillomavirus DNA testing as a primary screen for cervical cancer: a pooled analysis of individual patient data from 17 population-based studies from China. Lancet Oncol. 2010;11:1160–1171. doi: 10.1016/S1470-2045(10)70256-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cagle AJ, Hu SY, Sellors JW, Bao YP, Lim JM, Li SM, et al. Use of an expanded gold standard to estimate the accuracy of colposcopy and visual inspection with acetic acid. Int J Cancer. 2010;126:156–161. doi: 10.1002/ijc.24719. [DOI] [PubMed] [Google Scholar]
- 27.Roura E, Castellsagué X, Pawlita M, Travier N, Waterboer T, Margall N, et al. Smoking as a major risk factor for cervical cancer and pre-cancer: results from the EPIC cohort. Int J Cancer. 2014;135:453–466. doi: 10.1002/ijc.28666. [DOI] [PubMed] [Google Scholar]
- 28.Castellsagué X, Bosch FX, Muñoz N. Environmental co-factors in HPV carcinogenesis. Virus Res. 2002;89:191–199. doi: 10.1016/s0168-1702(02)00188-0. [DOI] [PubMed] [Google Scholar]
- 29.Castellsagué X, Muñoz N. Chapter 3: Cofactors in human papillomavirus carcinogenesis--role of parity, oral contraceptives, and tobacco smoking. J Natl Cancer Inst Monogr. 2003;2003:20–28. [PubMed] [Google Scholar]
- 30.Muñoz N, Castellsagué X, de González AB, Gissmann L. Chapter 1: HPV in the etiology of human cancer. Vaccine. 2006;24(Suppl 3):S3/1–S3/10. doi: 10.1016/j.vaccine.2006.05.115. [DOI] [PubMed] [Google Scholar]
- 31.International Collaboration of Epidemiological Studies of Cervical Cancer Comparison of risk factors for invasive squamous cell carcinoma and adenocarcinoma of the cervix: collaborative reanalysis of individual data on 8,097 women with squamous cell carcinoma and 1,374 women with adenocarcinoma from 12 epidemiological studies. Int J Cancer. 2007;120:885–891. doi: 10.1002/ijc.22357. [DOI] [PubMed] [Google Scholar]
- 32.Melikian AA, Sun P, Prokopczyk B, El-Bayoumy K, Hoffmann D, Wang X, et al. Identification of benzo[a]pyrene metabolites in cervical mucus and DNA adducts in cervical tissues in humans by gas chromatography-mass spectrometry. Cancer Lett. 1999;146:127–134. doi: 10.1016/s0304-3835(99)00203-7. [DOI] [PubMed] [Google Scholar]
- 33.Hellberg D, Nilsson S, Haley NJ, Hoffman D, Wynder E. Smoking and cervical intraepithelial neoplasia: nicotine and cotinine in serum and cervical mucus in smokers and nonsmokers. Am J Obstet Gynecol. 1988;158:910–913. doi: 10.1016/0002-9378(88)90093-2. [DOI] [PubMed] [Google Scholar]
- 34.Harrison KL, Khan NS, Dey P, Povey AC. N7-methyldeoxyguanosine levels in DNA isolated from cervical cytology samples are associated with smoking. Int J Cancer. 2006;119:961–963. doi: 10.1002/ijc.21900. [DOI] [PubMed] [Google Scholar]
- 35.Prokopczyk B, Cox JE, Hoffmann D, Waggoner SE. Identification of tobacco-specific carcinogen in the cervical mucus of smokers and nonsmokers. J Natl Cancer Inst. 1997;89:868–873. doi: 10.1093/jnci/89.12.868. [DOI] [PubMed] [Google Scholar]
- 36.Collins S, Rollason TP, Young LS, Woodman CB. Cigarette smoking is an independent risk factor for cervical intraepithelial neoplasia in young women: a longitudinal study. Eur J Cancer. 2010;46:405–411. doi: 10.1016/j.ejca.2009.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Louie KS, Castellsague X, de Sanjose S, Herrero R, Meijer CJ, Shah K, et al. Smoking and passive smoking in cervical cancer risk: pooled analysis of couples from the IARC multicentric case-control studies. Cancer Epidemiol Biomarkers Prev. 2011;20:1379–1390. doi: 10.1158/1055-9965.EPI-11-0284. [DOI] [PubMed] [Google Scholar]
- 38.Tsai HT, Tsai YM, Yang SF, Wu KY, Chuang HY, Wu TN, et al. Lifetime cigarette smoke and second-hand smoke and cervical intraepithelial neoplasm--a community-based case-control study. Gynecol Oncol. 2007;105:181–188. doi: 10.1016/j.ygyno.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 39.Coker AL, Bond SM, Williams A, Gerasimova T, Pirisi L. Active and passive smoking, high-risk human papillomaviruses and cervical neoplasia. Cancer Detect Prev. 2002;26:121–128. doi: 10.1016/s0361-090x(02)00039-9. [DOI] [PubMed] [Google Scholar]
- 40.Waggoner SE, Darcy KM, Tian C, Lanciano R. Smoking behavior in women with locally advanced cervical carcinoma: a Gynecologic Oncology Group study. Am J Obstet Gynecol. 2010;202:283.e1–283.e7. doi: 10.1016/j.ajog.2009.10.884. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Real numbers of active and passive smoking and the HPV infection and CIN2+ in each site after adjustment in the pooled analysis
Associations with the HPV infection and CIN2+: ORs and 95% CIs of being HPV infection and CIN2+ women according to potential confounding factors