Abstract
Purpose
To investigate the effects of anti-vascular endothelial growth factor (VEGF) antibody on the survival of retinal ganglion cell (RGC)-5 cells differentiated with staurosporine under oxidative stress.
Methods
We used real-time polymerase chain reaction and Western blot to confirm the expression of VEGF, VEGF receptor (VEGFR)-1 and VEGFR-2 in RGC-5 cells differentiated with staurosporine for 6 hours. The differentiated RGC-5 cells were treated with 800 µM hydrogen peroxide (H2O2) for 24 hours to induce oxidative stress. Then, the survival rate of RGC-5 was confirmed by lactate dehydrogenase assay at each concentration (0, 0.01, 0.1, and 1 mg) using bevacizumab as the anti-VEGF antibody. The expression of VEGF, VEGFR-1, and VEGFR-2 was confirmed using real-time polymerase chain reaction.
Results
VEGF, VEGFR-1, and VEGFR-2 were all expressed in differentiated RGC-5 cells. When RGC-5 cells were simultaneously treated with bevacizumab and 800 µM H2O2, survival of RGC-5 decreased with bevacizumab concentration. VEGF expression in RGC-5 cells increased with increasing concentration of bevacizumab. Similar patterns were observed for VEGFR-1 and VEGFR-2, but the degree of increase was smaller than that for VEGF.
Conclusions
When bevacizumab was administered to differentiated RGC-5 cells, the cell damage caused by oxidative stress increased. Therefore, given these in vitro study results, caution should be exercised with bevacizumab treatment.
Keywords: Anti-vascular endothelial growth factor, Bevacizumab, Oxidative stress, Retinal ganglion cell, RGC-5
The hypothesis that a specific substance acts on neovascularization in retinal diseases was first proposed in 1956 [1] and it was determined that vascular endothelial growth factor (VEGF) is increased in the oxidative stress environment of the retina [2,3,4,5]. VEGF is a 46-kDa molecular weight glycoprotein that binds to receptors on the surface of vascular endothelial cells to proliferate and increase capillary permeability [6]. Previously, it was thought that VEGF function was restricted to endothelial cells. However, in recent studies, VEGF was shown to promote the development and maturation of neural tissues, including the retina [7]. In the normal development of the retina, VEGF acts as an essential factor in the production and survival and function of cells [8,9]. However, VEGF has been implicated in the development of neovascularization in various retinal vascular diseases such as exudative age-related macular degeneration, proliferative diabetic retinopathy, macular edema of retinal vein occlusion, and retinopathy of prematurity. In addition, it has been shown that the elevated level of VEGF in these diseases plays a key role in the progression of disease [2,10,11]. Recently, treatment with the anti-VEGF antibody bevacizumab has been widely used for these diseases in the field of ophthalmology, and positive treatment effects have been reported in many eye diseases that cause blindness [12,13]. However, since angiogenesis is an important mechanism that protects tissues against various ischemic injuries, bevacizumab administration for the inhibition of angiogenesis potentially has unexpected harmful effects on the tissue [8]. Previous studies have reported the safety and side effects of bevacizumab treatment [14]. One of the studies reported that bevacizumab injection resulted in the death of retinal ganglion cells (RGCs) in an animal model [15]. In this study, we investigated the effects of bevacizumab on the survival of retinal ganglion cells cultured in a hypoxic environment through experimental methods in order to establish a basis for the safe and effective use of anti-VEGF antibody therapy in various ophthalmic diseases.
Materials and Methods
Growth of cell lines
Differentiation of RGC-5 cells was used in this study. The RGC-5 cell line selectively retained the retinal ganglion cells in the mouse and was infected with the R-virus to maintain retinal ganglion cell characteristics [16,17]. In a previous study [18], staurosporine (Sigma, Poole, UK) was used at a concentration of 1 µg for a minimum of 6 hours to reach the final differentiation level of the RGC-5 cell line. In the present study, RGC-5 cells were treated with 1 µg staurosporine for 6 hours as well.
Identification of VEGF, VEGF receptor (VEGFR)-1 and VEGFR-2 expression in differentiated RGC-5 cell lines
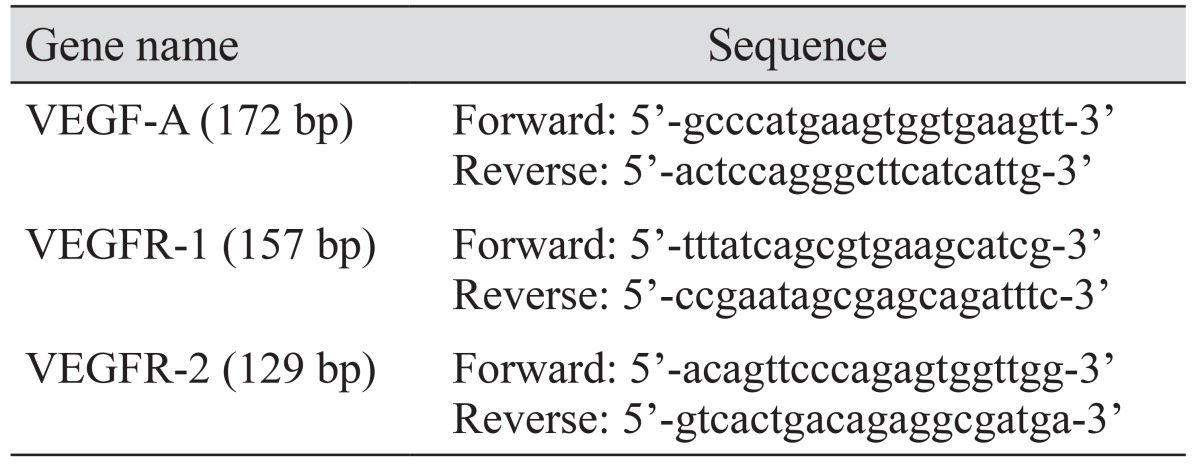
The expression of VEGF, VEGFR-1, and VEGFR-2 was assessed by real-time polymerase chain reaction (PCR) and Western blot (Table 1 and Fig. 1) after culturing RGC-5 cells differentiated using the above method.
Table 1. Primer sequences for real-time PCR.
PCR = polymerase chain reaction; VEGF = vascular endothelial growth factor; VEGFR = VEGF receptor.
Fig. 1. Expression of vascular endothelial growth factor (VEGF), VEGF receptor (VEGFR)-1 and VEGFR-2 assessed by real-time polymerase chain reaction. VEGF, VEGFR-1, and VEGFR-2 are all expressed in differentiated retinal ganglion cell-5 cells.
cDNA synthesis
cDNA was synthesized from the extracted total RNA according to the manufacturer's protocol using the SuperScript III First-Strand Synthesis System for real-time PCR (Gibco, Grand Island, NY, USA). Briefly, cultured RGC-5 cells were floated with trypsin and total RNA was extracted using RNeasy mini kit (Qiagen, Valencia, CA, USA). A combination of 1 µL of extracted total RNA, 1 µL of 50 µM oligo (dT), 1 µL of 10 mM deoxynucleoside triphosphate (dNTP) mix and diethyl pyrocarbonate (DEPC)-treated water for a total volume of 10 µL was incubated at 65℃ for 5 minutes. The mixture was then put on ice for 1 minute to stop the reaction. Next, 2 µL of 10 × reverse transcription (RT) buffer, 4 µL of 25 mM MgCl2, 2 µL of 0.1 M dithiothreitol (DTT), 1 µL of RNaseOUT (40 U/µL) and 1 µL of SuperScript III RT (200 U/µL) was added for a total volume of 20 µL. Thereafter, the cells were incubated at 50℃ for 50 minutes and incubated at 85℃ for 5 minutes to stop the reaction, and then the tubes were placed on ice. The reaction mixture was collected by light centrifugation and 1 µL of RNase H was added and incubated at 37℃ for 20 minutes to remove residual RNA. The resulting cDNA was stored at −20℃ until further processing.
Real-time PCR
Real-time PCR was performed using the QuantiTect SYBR Green PCR kit (Qiagen). A mixture of 100 ng of cDNA, 2 µL of 20 µM primers, 25 µL of master mix, and DEPC-treated water was added to each sample to make a 50 µL mixture. The primer sequences are listed in Table 1.
Each primer product was identified via melting curve analysis. The temperature conditions of the amplification process are as follows. Cycle 1, 95℃ for 3 minutes; cycle 2 (50 cycles; step 1, 95℃ for 10 seconds; step 2, 55℃ for 45 seconds); cycle 3, 95℃ for 1 minute; cycle 4, 55℃ for 1 minute; cycle 5 (80 cycles; step 1, 55℃ for 10 seconds; step 2, increase set point temperature after 2nd cycle by 0.5℃). Each mRNA level was calculated using the 2-ΔCt method based on the Ct value using β-actin as the reference housekeeping gene.
Western blot
Sodium dodecyl sulfate polyacrylamide gel electrophoresis was performed with 10%–15% sodium dodecyl sulfate-polyacrylamide gel and 50 µg of cell lysate was loaded in each well. After electrophoresis, the cells were electro-transferred to Immobilon-P transfer membrane (Millipore, Billerica, MA, USA) under 200 mA for 2 hours. Three percent of BSA (AMRESCO, Solon, OH, USA) was used to inhibit nonspecific binding. After that, the primary antibody was added, reacted at room temperature for 1 hour, washed and secondary antibody was used. One of the ECL peroxidase-labeled anti-rabbit (Amersham, Piscataway, NJ, USA) or ECL peroxidase-labeled anti-mouse (Amersham) was selected for the primary antibody host, and then sensitized using Amersham ECL Western Blotting Detection Reagents (Amersham).
Induction of oxidative stress and evaluation of cell survival
The differentiated RGC-5 cells were treated with H2O2 (800 µM) for 24 hours to induce oxidative stress. Cell viability was assessed using lactate dehydrogenase (LDH) assay. The amount of LDH was measured via colorimetric assay (Calbiochem-Novabiochem, San Diego, CA, USA), and whole cells were frozen. In comparison with the amount of LDH measured after death, the degree of destruction was evaluated. Serial dilutions of commercially available bevacizumab (Avastin; Genentech, San Francisco, CA, USA) were performed to obtain treatment concentrations of 0.01, 0.1, and 1 mg/mL.
Statistical analysis
Data are expressed as the mean ± standard deviation of at least three different experiments performed from separate cell preparations, and at least triplicate determinations were performed for each experiment. Statistical tests to determine the difference between groups were performed by Mann-Whitney U-test using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA). A p-value of less than 0.05 was considered statistically significant.
Results
Effect of bevacizumab on the survival of RGC-5 cell line under oxidative stress
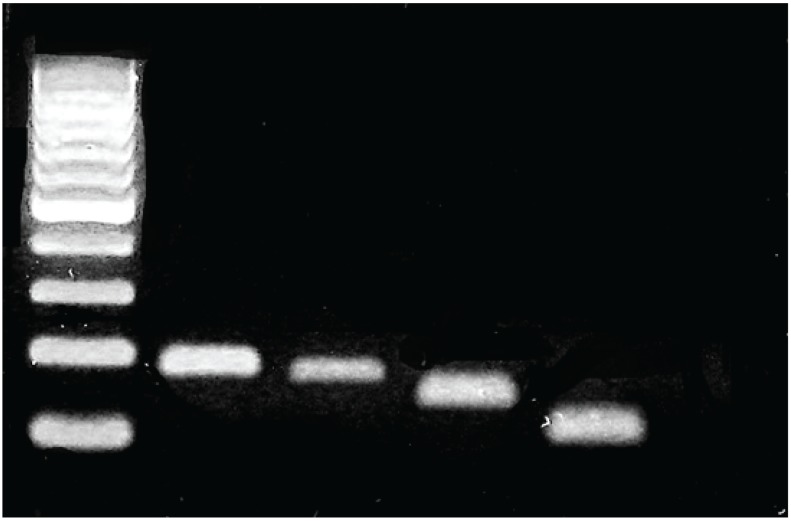
Oxidative stress was induced in RGC-5 cells treated for 24 hours using 800 µM H2O2. At that time, the RGC-5 cells were simultaneously treated with the anti-VEGF antibody, bevacizumab (0, 0.01, 0.1, and 1 mg), and the effect of this treatment on the survival was evaluated by LDH assay. We confirmed that the cell damage increased as the concentration of the bevacizumab increased. In the absence of oxidative stress, RGC-5 cytotoxicity increased following treatment with 1 mg bevacizumab, which was higher than oxidative stress-induced cytotoxicity (Fig. 2).
Fig. 2. Effects of bevacizumab on the survival of retinal ganglion cell (RGC)-5 cells under oxidative stress with 800 µM H2O2 for 24 hours. As the concentration of bevacizumab increases, the RGC-5 death rate increases. With the presence of bevacizumab, cell death increased without oxidative stress. Values are presented as mean ± standard deviation (*values are significantly different from the control; p < 0.05 by Mann-Whitney U-test).
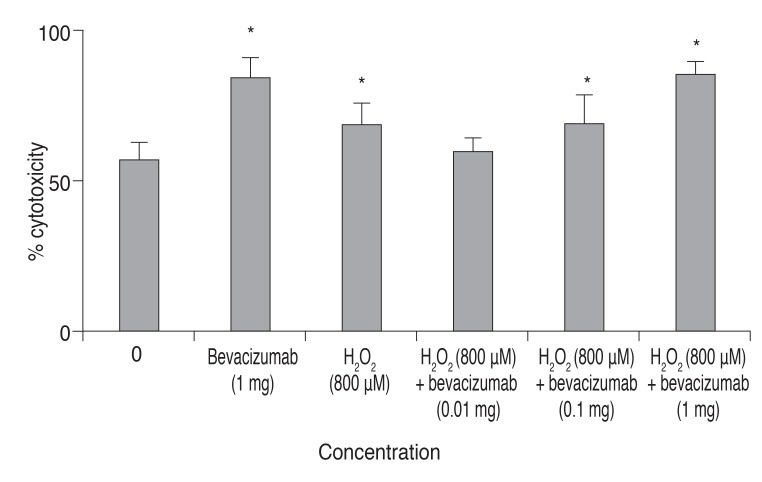
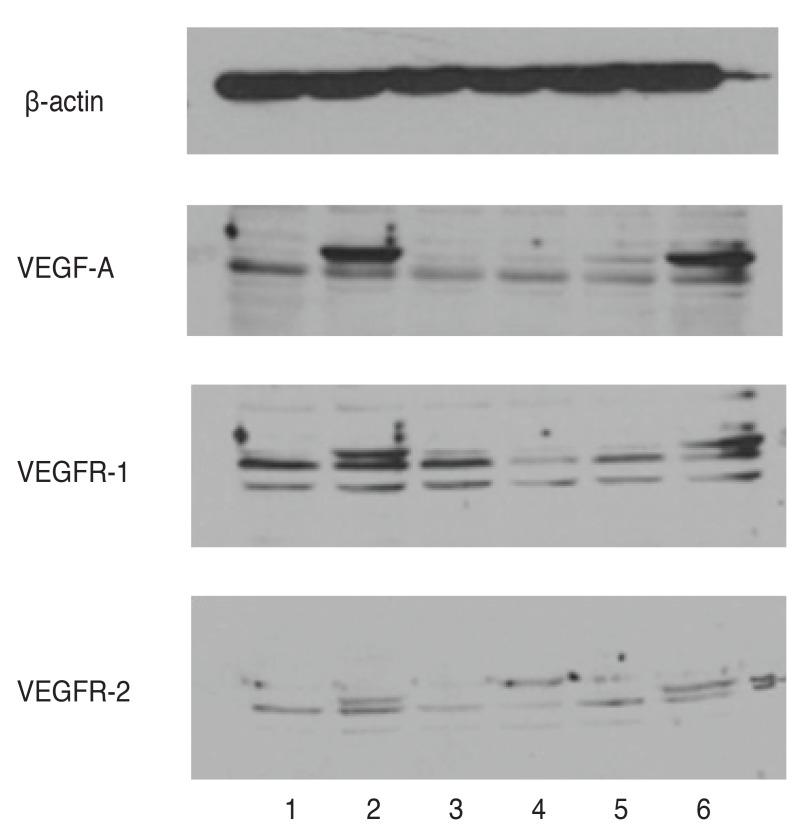
Effect of bevacizumab on the expression of VEGF, VEGFR-1 and VEGFR-2 in RGC-5 Cells
The expression of VEGF, VEGFR-1, and VEGFR-2 in bevacizumab-treated RGC-5 cells was confirmed by Western blot analysis. In addition, the expression of VEGF, VEGFR-1, and VEGFR-2 increased as the concentration of bevacizumab increased, and the expression of VEGF, VEGFR-1, and VEGFR-2 increased in RGC-5 cells treated by H2O2 alone (Fig. 3).
Fig. 3. Western blot analysis of vascular endothelial growth factor (VEGF), VEGF receptor (VEGFR)-1 and VEGFR-2 in retinal ganglion cell (RGC)-5 cells treated with bevacizumab. The expression of VEGF, VEGFR-1, and VEGFR-2 increased with the increase in bevacizumab concentration, and the expression of VEGF, VEGFR-1, and VEGFR-2 was increased in RGC-5 cells treated with H2O2. 1, control; 2, bevacizumab 1 mg; 3, H2O2 800 µM; 4, bevacizumab 0.01 mg + H2O2 800 µM; 5, bevacizumab 0.1 mg + H2O2 800 µM; 6, bevacizumab 1 mg + H2O2 800 µM.
Discussion
A number of recent studies have shown that bevacizumab injection therapy in the vitreous cavity has a remarkable therapeutic effect in many retinal vascular diseases including exudative age-related macular degeneration, diabetic retinopathy, and neovascular glaucoma [12,13]. However, VEGF plays an important role in the neuroprotection, development and maturation of the nerve tissues of the retina [7]. Normally, VEGF-mediated angiogenesis in the human body occurs to protect cells in a hypoxic environment. The administration of bevacizumab to inhibit angiogenesis may cause unintended cytotoxicity and ischemic damage [9]. Furthermore, the use of bevacizumab in patients with optic nerve weakness, such as glaucoma, is likely to cause damage to the retinal ganglion cells, which play an important pathophysiological role in glaucoma. In glaucoma, there is reduction of the retinal nerve fiber layer thickness and loss of retinal ganglion cells [19], and retinal ganglion cell damage may cause an irreversible field defect or visual loss.
Although intraocular pressure reduction still remains the mainstay of glaucoma therapy, recent studies have suggested that intraocular pressure reduction alone cannot prevent irreversible damage to retinal ganglion cells. Neuroprotection is a strategy for glaucoma treatment, and a number of studies have addressed the factors affecting the survival and death of the retinal ganglion cells [20,21]. Foxton et al. [15] observed that VEGF-A stimulates the survival of retinal ganglion cells in the glaucoma experimental model, and VEGF-A blockade significantly exacerbates neuronal cell death. Saint-Geniez et al. [8] reported a reduction in retinal ganglion cell thickness when VEGF expression was suppressed.
In this study, we investigated the effects of bevacizumab concentration on RGC-5 cell survival under oxidative stress. We found that cytotoxicity increased when bevacizumab was applied to the differentiated RGC-5 cell line, and cell damage increased with increasing bevacizumab concentration. In addition, even in the absence of oxidative stress, when bevacizumab was applied to the RGC-5 cell line, the cytotoxicity of the cell line increased, and was greater than that from oxidative stress (Fig. 2). Our results confirm that bevacizumab, which is widely used clinically, would inhibit retinal ganglion cell survival. In addition, we confirmed that VEGF, VEGFR-1, and VEGFR-2 were all produced in the RGC-5 cells used in this experiment. When bevacizumab and 800 µM H2O2 were simultaneously treated with RGC-5, cell damage and the expression of VEGF in RGC-5 itself was also increased according to the increased concentration of bevacizumab.
This study shows that a high concentration of bevacizumab increases cell death in retinal ganglion cells. However, since this experiment was not performed in vivo, we were unable to show different mechanisms and patterns in the human body due to interactions with other cells under oxidative stress. In the present study, we used the RGC-5 cell line, which has been reported to be cross-contaminated with a mouse fibroblast cell line [22]. Furthermore, the RGC-5 cell line may not accurately represent the characteristics of all retinal ganglion cells. Therefore, additional experiments and studies will be needed to determine whether other animal models and primary retinal ganglion cells will produce similar results in the future.
This study is expected to provide a basis for the safe and effective use of bevacizumab in various ophthalmic diseases including glaucoma. In the future, bevacizumab should be used at the minimum concentration that does not cause cytotoxicity. In addition, intravitreal injection of bevacizumab for the treatment of retinal vascular disease often needs to be repeated rather than administered as a single treatment. Therefore, studies on the benefits and risks of long-term treatment according to the frequency of injection are needed to prevent potential adverse effects of indiscriminate bevacizumab treatment. In particular, considering the fact that bevacizumab treatment may have a negative effect on eyes with optic nerve damage such as glaucoma, treatment should be performed according to individual characteristics and more attention should be focused on these conditions. In addition, long-term large-scale clinical trials and animal models are needed in the future to evaluate the efficacy and safety of bevacizumab therapy.
Acknowledgements
This study was supported by a faculty research grant of Yonsei University College of Medicine for 2008 (research project No. 6-2008-0201).
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Wise GN. Retinal neovascularization. Trans Am Ophthalmol Soc. 1956;54:729–826. [PMC free article] [PubMed] [Google Scholar]
- 2.Adamis AP, Miller JW, Bernal MT, et al. Increased vascular endothelial growth factor levels in the vitreous of eyes with proliferative diabetic retinopathy. Am J Ophthalmol. 1994;118:445–450. doi: 10.1016/s0002-9394(14)75794-0. [DOI] [PubMed] [Google Scholar]
- 3.Miller JW, Adamis AP, Shima DT, et al. Vascular endothelial growth factor/vascular permeability factor is temporally and spatially correlated with ocular angiogenesis in a primate model. Am J Pathol. 1994;145:574–584. [PMC free article] [PubMed] [Google Scholar]
- 4.Drobek-Slowik M, Karczewicz D, Safranow K. The potential role of oxidative stress in the pathogenesis of the age-related macular degeneration (AMD) Postepy Hig Med Dosw (Online) 2007;61:28–37. [PubMed] [Google Scholar]
- 5.Beatty S, Koh H, Phil M, et al. The role of oxidative stress in the pathogenesis of age-related macular degeneration. Surv Ophthalmol. 2000;45:115–134. doi: 10.1016/s0039-6257(00)00140-5. [DOI] [PubMed] [Google Scholar]
- 6.Esser S, Wolburg K, Wolburg H, et al. Vascular endothelial growth factor induces endothelial fenestrations in vitro. J Cell Biol. 1998;140:947–959. doi: 10.1083/jcb.140.4.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Y, Mao XO, Xie L, et al. Vascular endothelial growth factor overexpression delays neurodegeneration and prolongs survival in amyotrophic lateral sclerosis mice. J Neurosci. 2007;27:304–307. doi: 10.1523/JNEUROSCI.4433-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saint-Geniez M, Maharaj AS, Walshe TE, et al. Endogenous VEGF is required for visual function: evidence for a survival role on muller cells and photoreceptors. PLoS One. 2008;3:e3554. doi: 10.1371/journal.pone.0003554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Storkebaum E, Lambrechts D, Carmeliet P. VEGF: once regarded as a specific angiogenic factor, now implicated in neuroprotection. Bioessays. 2004;26:943–954. doi: 10.1002/bies.20092. [DOI] [PubMed] [Google Scholar]
- 10.Aiello LP, Avery RL, Arrigg PG, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med. 1994;331:1480–1487. doi: 10.1056/NEJM199412013312203. [DOI] [PubMed] [Google Scholar]
- 11.Ferrara N, Mass RD, Campa C, Kim R. Targeting VEGF-A to treat cancer and age-related macular degeneration. Annu Rev Med. 2007;58:491–504. doi: 10.1146/annurev.med.58.061705.145635. [DOI] [PubMed] [Google Scholar]
- 12.Ozaki H, Seo MS, Ozaki K, et al. Blockade of vascular endothelial cell growth factor receptor signaling is sufficient to completely prevent retinal neovascularization. Am J Pathol. 2000;156:697–707. doi: 10.1016/S0002-9440(10)64773-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gragoudas ES, Adamis AP, Cunningham ET, Jr, et al. Pegaptanib for neovascular age-related macular degeneration. N Engl J Med. 2004;351:2805–2816. doi: 10.1056/NEJMoa042760. [DOI] [PubMed] [Google Scholar]
- 14.van der Reis MI, La Heij EC, De Jong-Hesse Y, et al. A systematic review of the adverse events of intravitreal anti-vascular endothelial growth factor injections. Retina. 2011;31:1449–1469. doi: 10.1097/IAE.0b013e3182278ab4. [DOI] [PubMed] [Google Scholar]
- 15.Foxton RH, Finkelstein A, Vijay S, et al. VEGF-A is necessary and sufficient for retinal neuroprotection in models of experimental glaucoma. Am J Pathol. 2013;182:1379–1390. doi: 10.1016/j.ajpath.2012.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Charles I, Khalyfa A, Kumar DM, et al. Serum deprivation induces apoptotic cell death of transformed rat retinal ganglion cells via mitochondrial signaling pathways. Invest Ophthalmol Vis Sci. 2005;46:1330–1338. doi: 10.1167/iovs.04-0363. [DOI] [PubMed] [Google Scholar]
- 17.Maher P, Hanneken A. The molecular basis of oxidative stress-induced cell death in an immortalized retinal ganglion cell line. Invest Ophthalmol Vis Sci. 2005;46:749–757. doi: 10.1167/iovs.04-0883. [DOI] [PubMed] [Google Scholar]
- 18.Na KD, Kang SY, Seong GJ, et al. Ischemic preconditioning and the role of protein kinase C in cultured retinal ganglion cell line. J Korean Ophthalmol Soc. 2008;49:979–986. [Google Scholar]
- 19.Na JH, Lee K, Lee JR, et al. Detection of macular ganglion cell loss in preperimetric glaucoma patients with localized retinal nerve fibre defects by spectral-domain optical coherence tomography. Clin Exp Ophthalmol. 2013;41:870–880. doi: 10.1111/ceo.12142. [DOI] [PubMed] [Google Scholar]
- 20.Chen SD, Wang L, Zhang XL. Neuroprotection in glaucoma: present and future. Chin Med J (Engl) 2013;126:1567–1577. [PubMed] [Google Scholar]
- 21.Weinreb RN. Glaucoma neuroprotection: what is it? Why is it needed? Can J Ophthalmol. 2007;42:396–398. [PubMed] [Google Scholar]
- 22.Krishnamoorthy RR, Clark AF, Daudt D, et al. A forensic path to RGC-5 cell line identification: lessons learned. Invest Ophthalmol Vis Sci. 2013;54:5712–5719. doi: 10.1167/iovs.13-12085. [DOI] [PubMed] [Google Scholar]