Abstract
Population-based studies investigating the relationship of arthritis with mental health outcomes are lacking, particularly among low- and middle-income countries (LMICs). We investigated the relationship between arthritis and mental health (depression spectrum, psychosis spectrum, anxiety, sleep disturbances and stress) across community-dwelling adults aged ≥18 years across 46 countries from the World Health Survey. Symptoms of psychosis and depression were established using questions from the Mental Health Composite International Diagnostic Interview. Severity of anxiety, sleep problems, and stress sensitivity over the preceding 30 days were self-reported. Self-report lifetime history of arthritis was collected, including presence or absence of symptoms suggestive of arthritis: pain, stiffness or swelling of joints over the preceding 12-months. Multivariable logistic regression analyses were undertaken. Overall, 245,706 individuals were included. Having arthritis increased the odds of subclinical psychosis (OR = 1.85; 95%CI = 1.72–1.99) and psychosis (OR = 2.48; 95%CI = 2.05–3.01). People with arthritis were at increased odds of subsyndromal depression (OR = 1.92; 95%CI = 1.64–2.26), a brief depressive episode (OR = 2.14; 95%CI = 1.88–2.43) or depressive episode (OR = 2.43; 95%CI = 2.21–2.67). Arthritis was also associated with increased odds for anxiety (OR = 1.75; 95%CI = 1.63–1.88), sleep problems (OR = 2.23; 95%CI = 2.05–2.43) and perceived stress (OR = 1.43; 95%CI = 1.33–1.53). Results were similar for middle-income and low-income countries. Integrated interventions addressing arthritis and mental health comorbidities are warranted to tackle this considerable burden.
Introduction
Recent global burden of disease surveys have demonstrated that chronic musculoskeletal and joint conditions are leading causes of disability, particularly in Western societies1, 2. One of the main clusters of chronic musculoskeletal and joint disorders is arthritis, a broad term encompassing osteoarthritis (OA) and inflammatory arthritic conditions such as rheumatoid arthritis (RA). The hallmark features of arthritis in both OA and RA are pain and discomfort. Unsurprisingly, an increasing body of evidence has demonstrated that OA3 and RA4 are associated with high levels of disability and lower quality of life5.
Recently, there is increasing interest in the mental health burden of arthritis. Specifically, Matcham et al.6 in a meta-analysis of 72 studies established that 38% of people with RA met the criteria for depression according to the Patient Health Questionnaire7 whilst 16.8% had major depressive disorder, figures considerably higher than the general population. The presence of anxiety and depression in RA is important since it is known to predict treatment response in patients with RA8. Stubbs et al.9 recently conducted a meta-analysis and established that one fifth of people with OA had anxiety or depression. A recent longitudinal study in North America demonstrated that multisite OA is associated with an increased incidence of depression10. A number of single country studies have also demonstrated that RA11 and OA12 are associated with sleep disturbance. Sleep disturbance and perceived stress have also been demonstrated to be associated with worse outcomes in people with RA13. Thus, clearly, mental health symptoms are common and negatively impact the quality of life and treatment outcomes for people with arthritis.
Whilst progress has been made in understanding the mental health burden associated with arthritis, some pertinent limitations and gaps within the literature exist. First, to date, most studies considering arthritis and mental health have been based on clinical samples, and there is a lack of community-based studies. Moreover, there is a paucity of large representative multinational studies, particularly among low- and middle-income countries (LMICs). The majority of the world’s population resides in LMICs. A recent meta-analysis demonstrated that 3.16 million males and 14.87 million females were affected by RA in 2010 in LMICs with a rapid increase expected14. Resources to deal with the physical aspect of arthritis or mental health generally are not well established nor a priority in LMICs. Therefore, this comorbidity may be particularly challenging in this setting, and understanding the mental health burden of arthritis is important for planning service development. Moreover, people in LMICs are more likely to undertake labor-demanding jobs in the informal sector with no job security or compensation for lost income. Therefore, maintaining good mental and physical health is crucial for their livelihoods and general welfare. Furthermore, it is possible, for example, that pain associated with arthritis could increase the mental health burden and stress in an environment where reliance on income from labor-demanding jobs is widespread. Therefore, there is a need to elucidate the potential mental health burden among people with arthritis in LMICs. Second, the majority of studies considering mental health comorbidity and arthritis have focused on common mental disorders such as depression or anxiety and very few studies have considered psychosis for instance. However, there is an intriguing negative relationship that has been reported between schizophrenia and RA in Western counties15 and a paucity of data is available on arthritis and people with psychotic symptoms who do not meet the criteria for a diagnosis. In addition, there is increasing recognition that depression sits on a continuum with various subtypes, yet there is a lack of studies considering the relationship between arthritis and the depression continuum. Clearly, understanding a wider range of mental health comorbidities (including depression subtypes, psychosis, sleep disturbance, anxiety, and perceived stress) in arthritis important.
Given the aforementioned, the aim of the current study was to explore the relationship between arthritis and mental health (depression subtypes, psychosis, anxiety, sleep problems, and stress sensitivity). We hypothesized that people with arthritis in both low-income and middle-income countries would have worse mental health outcomes than those without arthritis.
Data and Methods
Procedures
The data for the current study was captured from the World Health Survey (WHS). The WHS was a cross-sectional study undertaken in 2002–2004 in 70 countries worldwide. Data were collected using single-stage random sampling and stratified multi-stage random cluster sampling across 10 and 60 countries respectively. Full details of the WHS are available elsewhere (http://www.who.int/healthinfo/survey/en/). In brief, persons aged ≥18 years with a valid home address were eligible to participate. Each member of the household had equal probability of being selected by utilizing Kish tables. A standardized questionnaire, translated accordingly was used across all countries. Linguists ensured that the translation was conducted to a high standard. The individual response rate (i.e. ratio of completed interviews among selected respondents after excluding ineligible respondents from the denominator) ranged from 63% (Israel) to 99% (Philippines)16. Ethical approval to conduct this study was obtained from the ethical boards at each study site (see Appendix 1 for details of approving board at each study site) and in accordance with each sites regulations. Sampling weights were generated to adjust for non-response and the population distribution reported by the United Nations Statistical Division. Informed consent was obtained from all participants.
Of the 70 countries, 69 had data which were publically available. Of these, 10 countries (Austria, Belgium, Denmark, Germany, Greece, Guatemala, Italy, Netherlands, Slovenia, and UK) were excluded due to lack of data on sampling information. Furthermore, 10 high-income countries (Finland, France, Ireland, Israel, Luxembourg, Norway, Portugal, Spain, Sweden, United Arab Emirates) were excluded in order to focus on LMICs. Of the remaining LMICs, Slovakia, Congo, and Swaziland were excluded as >25% of the data on arthritis was missing. Thus, the final sample consisted of 46 countries which corresponded to 20 low-income and 26 middle-income countries according to the World Bank classification at the time of the survey (2003).
Primary variables
Arthritis (exposure variable)
Individuals with a self-reported lifetime diagnosis of arthritis and/or typical symptoms of arthritis were considered to have arthritis. The specific question used to assess a lifetime diagnosis was “Have you ever been diagnosed with arthritis (a disease of the joints)”?
We also used a symptom-based approach to minimize reporting bias especially in areas where access to medical facilities is limited. The symptom-based algorithm was based on questions on typical clinical symptoms used in previous publications using the same questionnaire17, 18. Specifically, those who replied affirmatively to both of the following questions were considered to have arthritis: During the last 12 months, have you experienced: (a) pain, aching, stiffness or swelling in or around the joint (like arms, hands, legs or feet) which were not related to an injury and lasted for more than a month?; (b) stiffness in the joint in the morning after getting up from bed, or after a long rest of the joint without movement?
Mental health conditions (outcome variables)
Depression type
The severity of depressive symptoms was established based on the individual questions of the World Mental Health Survey version of the Mental Health Composite International Diagnostic Interview (CIDI), which assessed the duration and persistence of depressive symptoms in the past 12 months19. Following the algorithms used in a previous WHS publication20, four mutually exclusive groups were established based on the ICD-10 Diagnostic Criteria for Research (ICD-10-DCR) where criterion B referred to symptoms of depressed mood, loss of interest, and fatigability. The algorithms used to define the four groups were the following: (a) Depressive episode group: At least two criterion B symptoms together with a total of at least four depressive symptoms lasting two weeks most of the day or all of the day. (b) Brief depressive episode group: Same criteria as depressive episode above but duration did not meet the two-week duration criterion. (c) Subsyndromal depression: At least one criterion B symptom together with the total number of symptoms being three or less. The criteria of duration of at least two weeks and presence of symptoms during most of the day had to be met. (d) No depressive disorder group: None of the above.
Psychosis
Participants were asked whether they had ever been diagnosed as having schizophrenia or psychosis. All participants, regardless of a psychosis diagnosis, were asked questions on positive psychotic symptoms which came from the WHO Composite International Diagnostic Interview(CIDI) 3.019. This psychosis module has been reported to be highly consistent with clinician ratings with a kappa agreement coefficient of 0.82 for DSM-IV diagnosis of schizophrenia with even higher concordance observed for hallucinations and delusions21. Furthermore, psychotic experiences determined with the CIDI have been reported to be a good screening tool to identify those at high risk of developing psychosis22. The hallucinations question excluded conditions associated with sleep-related states or substance use. Specifically, respondents were asked the following questions with answer options ‘yes’ or ‘no’: During the last 12 months, have you experienced (i) ‘A feeling something strange and unexplainable was going on that other people would find hard to believe’? (delusional mood); (ii) ‘A feeling that people were too interested in you or there was a plot to harm you’? (delusions of reference and persecution); (iii) ‘A feeling that your thoughts were being directly interfered or controlled by another person, or your mind was being taken over by strange forces’? (delusions of control); (iv) ‘An experience of seeing visions or hearing voices that others could not see or hear when you were not half asleep, dreaming or under the influence of alcohol or drugs’? (hallucinations).
Individuals who endorsed at least one of the four above-mentioned psychotic symptoms were considered to have psychotic symptoms. Based on information on psychosis diagnosis and psychotic symptoms, a three-category psychosis variable was constructed: (i) no psychosis diagnosis and no psychotic symptoms (control); (ii) at least one psychotic symptom but no psychosis diagnosis (subclinical psychosis); and (iii) psychosis diagnosis23, 24.
Sleep problems
Sleep problems were assessed by the question “Overall in the last 30 days, how much of a problem did you have with sleeping, such as falling asleep, waking up frequently during the night or waking up too early in the morning”? with answer options none, mild, moderate, severe, and extreme. Those who answered severe and extreme were considered to have sleep problems. This definition has been used in previous publications using the same survey question on sleep problems18, 25, 26.
Anxiety
Anxiety was assessed by the question “Overall in the past 30 days, how much of a problem did you have with worry or anxiety”? Respondents could answer: none, mild, moderate, severe, or extreme. In the current study those who answered severe and extreme were categorized as having anxiety26, 27.
Perceived stress
Perceived stress in the last month was assessed by two questions: “How often have you felt that you were unable to control the important things in your life”?; and “How often have you found that you could not cope with all the things that you had to do?” The answer options to these questions were: never (score = 1), almost never (score = 2), sometimes (score = 3), fairly often (score = 4), very often (score = 5). The scores of the two questions were added to create a scale ranging from 2 to 1028. The highest quintile (cut-off ≥7) was used to define a high level of perceived stress.
Other variables
Variables on sex, age, highest education achieved (no formal education, primary education, secondary or high school completed, or tertiary education completed), wealth, setting (rural or urban), smoking, alcohol consumption, angina, asthma, diabetes, and Body Mass Index (BMI) were considered as potential correlates of arthritis based on past literature4, 29. Principal component analysis based on 15–20 assets was performed to establish country-wise wealth quintiles. The question on smoking was ‘Do you currently smoke any tobacco products such as cigarettes, cigars, or pipes’? with the answer options being ‘daily’, ‘yes, but not daily’, or ‘no, not at all’. This variable was dichotomized into those who smoked regardless of frequency (i.e. daily or not daily) (current smokers) and those who do not smoke. Alcohol consumption was assessed by first asking the question ‘Have you ever consumed a drink that contains alcohol (such as beer, wine, etc.)’? Respondents who replied ‘no’ were considered lifetime abstainers. If the respondent replied affirmatively, then he/she was asked how many standard drinks of any alcoholic beverage he/she had on each day of the past 7 days. The number of days in the past week in which 4 (female) or 5 (male) drinks were consumed was calculated, and a total of 1–2 and >3 days in the past 7 days were considered infrequent and frequent heavy drinking respectively. Those who have ever consumed alcohol but were neither an infrequent or frequent heavy drinker were considered to be non-heavy drinkers. A three-category variable was created: (a) lifetime abstainer or non-heavy drinker; (b) infrequent heavy drinker; and (c) frequent heavy drinker30. Asthma and diabetes were based solely on self-reported lifetime diagnosis. For angina, in addition to a self-reported diagnosis, a symptom-based diagnosis based on the Rose questionnaire was also used31. BMI was based on self-reported weight and height, and was calculated as weight in kilograms divided by height in meters squared. BMI was categorized as <18.5 (underweight), 18.5–24.9 (normal weight), 25.0–29.9 (overweight), and ≥30 (obese) kg/m2 32.
Statistical analysis
The statistical analysis was performed with Stata 14.1 (Stata Corp LP, College station, Texas). The age- and sex-adjusted prevalence of arthritis for each country was estimated by using the United Nations population pyramids for the year 2010 (http://esa.un.org/wpp/Excel-Data/population.htm) as the standard population using age strata of 18–34, 35–59, and ≥60 years. The subsequent analyses used the overall sample including all countries or samples by country-income level (i.e. low-income or middle-income countries). Multivariable binary logistic regression analysis with arthritis as the outcome was performed to assess the correlates of arthritis. The correlates considered were sex, age, education, wealth, setting, smoking, alcohol consumption, angina, asthma, diabetes, and BMI. In order to assess the association between arthritis (exposure variable) and the mental health outcomes, multivariable binary and multinomial logistic regression analyses were conducted. Multinomial logistic regression analysis was conducted for psychosis and depression type, which consisted of more than two categories. When anxiety, sleep problems, and perceived stress were the outcome, binary logistic regression analysis was conducted. These analyses adjusted for all the potential correlates mentioned above as they have been reported to be associated with both arthritis and mental health outcomes12, 33–37. All variables were included in the models as categorical variables with the exception of age (continuous variable). All regression analyses were adjusted for country by including dummy variables for each country in the models, as in previous WHS publications38, 39. We did not use multilevel models as multilevel analyses with complex study designs can produce potentially biased estimates40. Turkey was not included in the regression analyses as it lacked data on education. Furthermore, due to completely missing data, the analysis with perceived stress as the outcome did not include Brazil, Hungary, and Zimbabwe, while Morocco was omitted from the analysis with anxiety as the outcome. The sample weighting and the complex study design were taken into account in all analyses with the use of the Stata svy command. Results from the logistic regression models are presented as odds ratios (ORs) with 95% confidence intervals (CIs). The level of statistical significance was set at P < 0.05.
Less than 5% of the data was missing for all variables used in the analysis with the exception of education (8.1%), wealth (8.4%), alcohol consumption (5.2%), BMI (30.1%), diabetes (15.9%), and psychosis (15.8%). For the regression analyses, we conducted multiple imputation of missing values using the mi commands in Stata using chained equations (20 imputations)41. This method uses information from all other variables except the one being imputed to impute missing values. The variables included in the imputation model were the outcome and all other covariates42. A predictive mean matching algorithm was used for continuous variables, while for dichotomous and ordinal variables, binary logistic regression models and ordered logistic regression models, respectively, were used. The results based on complete case analysis were similar (Appendixs 2 and 3).
Results
A total of 245,706 individuals (LIC = 102,211 and MIC = 143,495) constituted the final analytical sample. Overall, there were more females than males (50.7% vs. 49.3%), and the mean (SD) age was 38.4 (16.0) years. The sample size of each country ranged from 929 (Latvia) to 38,746 (Mexico) (Table 1). The age- and sex-adjusted prevalence of arthritis in the overall sample was 22.4% (95%CI = 21.9%–22.8%) with the corresponding figures for low-income and middle-income countries being 23.4% (95%CI = 22.7%–24.1%) and 20.9 (95%CI = 20.4%–21.9%) respectively. This figure ranged from 7.2% (Myanmar) to 42.6% (Malawi) with high prevalence also being observed in Chad (40.6%), Morocco (34.7%), and India (32.4%) (Table 1, Fig. 1). The sample characteristics are shown in Table 2. In the overall sample, female sex, older age, lower education, poverty, rural setting, smoking, lower alcohol consumption, angina, asthma, diabetes, higher BMI, and all the mental health outcomes were more common among those with arthritis (Table 2).
Table 1.
Sample size and age- and sex-adjusted prevalence of arthritis by country.
| Country | Low-income countries | Middle-income countries | |||
|---|---|---|---|---|---|
| Unweighted N | % (SE) | Country | Unweighted N | % (SE) | |
| Bangladesh | 5,942 | 24.0 (1.1) | Bosnia Herzegovina | 1,031 | 18.8 (1.8) |
| Burkina Faso | 4,948 | 20.2 (1.4) | Brazil | 5,000 | 20.6 (0.7) |
| Chad | 4,870 | 40.6 (1.4) | China | 3,994 | 14.2 (1.1) |
| Comoros | 1,836 | 18.5 (1.4) | Croatia | 993 | 22.8 (1.4) |
| Ethiopia | 5,089 | 31.2 (1.2) | Czech Republic | 949 | 24.0 (1.9) |
| Ghana | 4,165 | 19.0 (0.8) | Dominican Republic | 5,027 | 20.1 (0.8) |
| India | 10,687 | 32.4 (1.3) | Ecuador | 5,675 | 16.9 (0.9) |
| Ivory Coast | 3,251 | 21.5 (1.2) | Estonia | 1,020 | 27.4 (1.7) |
| Kenya | 4,640 | 15.4 (0.9) | Georgia | 2,950 | 23.0 (0.9) |
| Laos | 4,988 | 12.9 (0.7) | Hungary | 1,419 | 30.1 (1.2) |
| Malawi | 5,551 | 42.6 (1.1) | Kazakhstan | 4,499 | 21.7 (0.8) |
| Mali | 4,886 | 19.9 (0.9) | Latvia | 929 | 24.2 (1.7) |
| Mauritania | 3,902 | 28.4 (1.2) | Malaysia | 6,145 | 14.2 (0.5) |
| Myanmar | 6,045 | 7.2 (0.6) | Mauritius | 3,968 | 15.2 (0.9) |
| Nepal | 8,820 | 30.1 (0.6) | Mexico | 38,746 | 9.7 (0.3) |
| Pakistan | 6,501 | 19.7 (0.8) | Morocco | 5,000 | 34.7 (1.1) |
| Senegal | 3,461 | 27.3 (1.2) | Namibia | 4,379 | 15.5 (1.0) |
| Vietnam | 4,174 | 9.4 (0.9) | Paraguay | 5,288 | 18.5 (0.6) |
| Zambia | 4,165 | 9.0 (0.7) | Philippines | 10,083 | 27.3 (0.8) |
| Zimbabwe | 4,290 | 11.8 (0.7) | Russia | 4,427 | 22.5 (1.2) |
| South Africa | 2,629 | 20.9 (1.3) | |||
| Sri Lanka | 6,805 | 14.7 (0.8) | |||
| Tunisia | 5,202 | 30.9 (0.9) | |||
| Turkey | 11,481 | 19.1 (0.7) | |||
| Ukraine | 2,860 | 25.1 (1.3) | |||
| Uruguay | 2,996 | 14.1 (0.5) | |||
Abbreviation: SE standard error.
All age- and sex-adjusted weighted estimates were calculated using the United Nations population pyramids for the year 2010.
Figure 1.
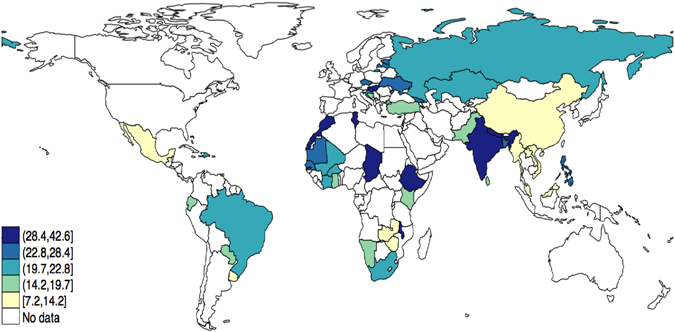
Age- and sex-adjusted prevalence (%) of arthritis. Estimates were calculated using the United Nations population pyramids for the year 2010. The figure was created with STATA 13.1 (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP).
Table 2.
Sample characteristics (overall and by country-income level and the presence of arthritis).
| Characteristic | Category | Overall | Low-income countries | Middle-income countries | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Arthritis | Total | Arthritis | Total | Arthritis | |||||
| No | Yes | No | Yes | No | Yes | |||||
| 49.3 | 51.9 | 39.0 | 50.5 | 52.9 | 41.4 | 47.7 | 50.6 | 35.8 | ||
| Female | 50.7 | 48.1 | 61.0 | 49.5 | 47.1 | 58.6 | 52.3 | 49.4 | 64.2 | |
| Age (years) | Mean | 38.4 | 35.9 | 48.1 | 36.8 | 34.6 | 45.1 | 40.5 | 37.6 | 51.8 |
| (SD) | (16.0) | (14.8) | (16.8) | (15.3) | (14.1) | (16.8) | (16.6) | (15.4) | (16.4) | |
| Educationa | No formal | 26.5 | 23.4 | 38.4 | 40.6 | 36.4 | 56.6 | 7.0 | 5.5 | 13.2 |
| ≤Primary | 30.9 | 30.9 | 30.8 | 32.9 | 34.0 | 28.7 | 28.1 | 26.8 | 33.7 | |
| Secondary completed | 33.4 | 36.0 | 23.4 | 20.5 | 22.8 | 11.5 | 51.2 | 54.2 | 39.7 | |
| Tertiary completed | 9.2 | 9.6 | 7.5 | 6.0 | 6.8 | 3.1 | 13.6 | 13.5 | 13.5 | |
| Wealth | Poorest | 20.1 | 19.3 | 23.5 | 20.2 | 19.6 | 23.0 | 20.1 | 19.0 | 24.2 |
| Poorer | 20.1 | 19.4 | 22.7 | 20.0 | 19.2 | 22.8 | 20.1 | 19.6 | 22.5 | |
| Middle | 20.0 | 20.0 | 20.0 | 19.9 | 19.8 | 20.0 | 20.2 | 20.3 | 20.1 | |
| Richer | 19.8 | 20.4 | 17.6 | 20.0 | 20.5 | 18.0 | 19.7 | 20.3 | 17.3 | |
| Richest | 20.0 | 20.9 | 16.2 | 20.0 | 20.9 | 16.2 | 19.9 | 20.9 | 16.1 | |
| Setting | Rural | 55.7 | 54.6 | 59.5 | 74.8 | 73.8 | 80.6 | 31.0 | 30.5 | 32.7 |
| Urban | 44.3 | 45.4 | 40.5 | 25.2 | 26.2 | 19.4 | 69.0 | 69.5 | 67.3 | |
| Smoking | No | 73.1 | 73.4 | 72.0 | 73.3 | 74.4 | 68.6 | 72.9 | 72.1 | 76.3 |
| Yes | 26.9 | 26.6 | 28.0 | 26.7 | 25.6 | 31.4 | 27.1 | 27.9 | 23.7 | |
| Alcohol | Never/non-heavy | 95.4 | 95.1 | 96.3 | 97.8 | 97.9 | 97.5 | 92.4 | 91.9 | 94.7 |
| consumption | Infrequent heavy | 3.6 | 3.8 | 2.8 | 1.5 | 1.5 | 1.6 | 6.2 | 6.7 | 4.3 |
| Frequent heavy | 1.0 | 1.0 | 0.9 | 0.7 | 0.7 | 0.8 | 1.4 | 1.5 | 1.0 | |
| Angina | No | 85.7 | 90.5 | 66.8 | 85.2 | 89.7 | 67.5 | 86.3 | 91.4 | 65.9 |
| Yes | 14.3 | 9.5 | 33.2 | 14.8 | 10.3 | 32.5 | 13.7 | 8.6 | 34.1 | |
| Asthma | No | 94.9 | 95.9 | 91.1 | 95.9 | 97.0 | 91.8 | 93.7 | 94.6 | 90.2 |
| Yes | 5.1 | 4.1 | 8.9 | 4.1 | 3.0 | 8.2 | 6.3 | 5.4 | 9.8 | |
| Diabetes | No | 97.0 | 97.9 | 93.7 | 98.1 | 98.6 | 95.8 | 95.5 | 96.8 | 90.8 |
| Yes | 3.0 | 2.1 | 6.3 | 1.9 | 1.4 | 4.2 | 4.5 | 3.2 | 9.2 | |
| BMI (kg/m2) | 18.5–24.9 | 57.6 | 59.3 | 50.5 | 62.1 | 63.1 | 57.7 | 53.3 | 55.6 | 43.9 |
| 25.0–29.9 | 19.8 | 19.2 | 22.6 | 11.5 | 11.2 | 13.0 | 27.9 | 27.0 | 31.6 | |
| ≥30 | 9.1 | 8.0 | 13.7 | 6.1 | 5.7 | 7.7 | 12.0 | 10.3 | 19.2 | |
| <18.5 | 13.5 | 13.5 | 13.2 | 20.3 | 20.0 | 21.6 | 6.8 | 7.1 | 5.4 | |
| Psychosis | Symptom (−) Diagnosis (−) | 85.0 | 87.3 | 75.8 | 85.9 | 88.4 | 75.7 | 83.7 | 85.7 | 76.0 |
| Symptom (+) Diagnosis (−) | 13.9 | 11.9 | 21.8 | 12.9 | 10.7 | 21.6 | 15.4 | 13.6 | 22.1 | |
| Diagnosis (+) | 1.1 | 0.8 | 2.3 | 1.2 | 0.9 | 2.7 | 0.9 | 0.6 | 1.9 | |
| Depression type | No depression | 88.4 | 91.3 | 75.6 | 88.3 | 91.3 | 74.5 | 88.5 | 91.2 | 77.1 |
| Subsyndromal depression | 2.4 | 1.9 | 4.8 | 3.0 | 2.3 | 6.2 | 1.6 | 1.3 | 2.8 | |
| Brief depressive episode | 2.7 | 2.2 | 5.0 | 2.3 | 1.9 | 4.2 | 3.4 | 2.7 | 6.1 | |
| Depressive episode | 6.5 | 4.6 | 14.6 | 6.4 | 4.5 | 15.1 | 6.6 | 4.8 | 13.9 | |
| Anxietyb | No | 88.4 | 90.6 | 79.8 | 90.9 | 93.2 | 82.2 | 85.2 | 87.4 | 76.6 |
| Yes | 11.6 | 9.4 | 20.2 | 9.1 | 6.8 | 17.8 | 14.8 | 12.6 | 23.4 | |
| Sleep problems | No | 92.3 | 94.9 | 81.8 | 93.0 | 95.4 | 83.7 | 91.3 | 94.3 | 79.3 |
| Yes | 7.7 | 5.1 | 18.2 | 7.0 | 4.6 | 16.3 | 8.7 | 5.7 | 20.7 | |
| Perceived stressc | No | 80.5 | 83.0 | 70.9 | 76.0 | 78.5 | 66.4 | 88.9 | 91.4 | 79.3 |
| Yes | 19.5 | 17.0 | 29.1 | 24.0 | 21.5 | 33.6 | 11.1 | 8.6 | 20.7 | |
Abbreviation: SD standard deviation; BMI body mass index.
Data are % unless otherwise stated.
All estimates are based on weighted sample.
aTurkey is not included as it lacked information on education.
bMorocco is not included as it lacked information on anxiety.
cBrazil, Hungary, and Zimbabwe are not included as they lacked information on perceived stress.
The correlates of arthritis estimated by multivariable binary logistic regression are presented in Table 3. In the overall sample, female sex, older age, lower education, poverty, smoking, angina, asthma, diabetes, and higher BMI were associated with arthritis. Similar correlates were found in the samples stratified by country-income level although there were some differences. Specifically, wealth and BMI were not significantly associated with arthritis in low-income countries.
Table 3.
Correlates of arthritis assessed by multivariable binary logistic regression analysis.
| Characteristic | Overall | Low-income countries | Middle-income countries | |||
|---|---|---|---|---|---|---|
| OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Sex | ||||||
| Male | 1.00 | 1.00 | 1.00 | |||
| Female | 1.58*** | [1.50,1.67] | 1.56*** | [1.45,1.69] | 1.62*** | [1.51,1.74] |
| Age (years) | 1.04*** | [1.04,1.04] | 1.04*** | [1.04,1.04] | 1.04*** | [1.04,1.05] |
| Education | ||||||
| No formal | 1.00 | 1.00 | 1.00 | |||
| ≤Primary | 0.95 | [0.88,1.01] | 0.94 | [0.86,1.02] | 0.95 | [0.84,1.07] |
| Secondary completed | 0.75*** | [0.69,0.82] | 0.71*** | [0.63,0.80] | 0.82** | [0.72,0.94] |
| Tertiary completed | 0.69*** | [0.62,0.78] | 0.62*** | [0.51,0.76] | 0.78** | [0.66,0.92] |
| Wealth | ||||||
| Poorest | 1.00 | 1.00 | 1.00 | |||
| Poorer | 1.04 | [0.97,1.13] | 1.08 | [0.97,1.20] | 0.98 | [0.88,1.08] |
| Middle | 0.97 | [0.90,1.05] | 0.98 | [0.88,1.09] | 0.94 | [0.85,1.04] |
| Richer | 0.90* | [0.82,0.98] | 0.92 | [0.81,1.04] | 0.86** | [0.76,0.96] |
| Richest | 0.86** | [0.78,0.95] | 0.88 | [0.76,1.01] | 0.84** | [0.74,0.95] |
| Setting | ||||||
| Rural | 1.00 | 1.00 | 1.00 | |||
| Urban | 0.94 | [0.87,1.01] | 0.93 | [0.82,1.05] | 0.95 | [0.87,1.04] |
| Smoking | ||||||
| No | 1.00 | 1.00 | 1.00 | |||
| Yes | 1.16*** | [1.08,1.23] | 1.17** | [1.07,1.29] | 1.16*** | [1.07,1.26] |
| Alcohol consumption | ||||||
| Never/non-heavy | 1.00 | 1.00 | 1.00 | |||
| Infrequent heavy | 1.01 | [0.89,1.16] | 1.26 | [0.97,1.64] | 0.94 | [0.81,1.09] |
| Frequent heavy | 0.96 | [0.77,1.20] | 1.17 | [0.88,1.55] | 0.82 | [0.59,1.15] |
| Angina | 2.90*** | [2.71,3.10] | 2.86*** | [2.59,3.15] | 2.92*** | [2.69,3.17] |
| Asthma | 1.49*** | [1.34,1.66] | 1.49*** | [1.28,1.75] | 1.50*** | [1.31,1.73] |
| Diabetes | 1.58*** | [1.38,1.82] | 1.85*** | [1.45,2.36] | 1.39*** | [1.18,1.64] |
| BMI (kg/m2) | ||||||
| 18.5–24.9 | 1.00 | 1.00 | 1.00 | |||
| 25.0–29.9 | 1.12** | [1.05,1.21] | 1.06 | [0.95,1.19] | 1.21*** | [1.11,1.32] |
| ≥30.0 | 1.34*** | [1.20,1.50] | 1.17 | [0.97,1.42] | 1.56*** | [1.39,1.74] |
| <18.5 | 0.99 | [0.91,1.08] | 0.97 | [0.87,1.08] | 1.02 | [0.89,1.16] |
Abbreviation: OR odds ratio; CI confidence interval; BMI Body mass index.
The models are adjusted for all variables in the table and country.
Turkey is not included in the regression analyses as it lacked information on education.
*p < 0.05, **p < 0.01, ***p < 0.001.
Mental health comorbidity and arthritis
The associations between arthritis and mental health outcomes estimated by multinomial and logistic regression are illustrated in Table 4. In the overall sample, after adjusting for potential confounders, having arthritis increased the odds of having subclinical psychosis (OR = 1.85; 95%CI = 1.72–1.99) or a psychosis diagnosis (OR = 2.48; 95%CI = 2.05–3.01) compared to no psychosis. The odds for all types of depression compared to no depression were also increased in those with arthritis: subsyndromal depression (OR = 1.92; 95%CI = 1.64–2.26); brief depressive episode (OR = 2.14; 95%CI = 1.88–2.43); depressive episode (OR = 2.43; 95%CI = 2.21–2.67). Furthermore, arthritis was also associated with increased odds for anxiety (OR = 1.75; 95%CI = 1.63–1.88); sleep problems (OR = 2.23; 95%CI = 2.05–2.43) and perceived stress (OR = 1.43; 95%CI = 1.33–1.53). The results for middle-income and low-income countries were similar.
Table 4.
The association between arthritis and mental health outcomes estimated by multinomial and binary logistic regression.
| Outcome | Overall | Low-income countries | Middle-income countries | |||
|---|---|---|---|---|---|---|
| OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Multinomial logistic regression | ||||||
| Psychosis | ||||||
| Symptom (−) Diagnosis (−) | 1.00 | 1.00 | 1.00 | |||
| Symptom (+) Diagnosis (−) | 1.85*** | [1.72,1.99] | 1.77*** | [1.59,1.97] | 1.98*** | [1.79,2.18] |
| Diagnosis (+) | 2.48*** | [2.05,3.01] | 2.27*** | [1.77,2.91] | 2.98*** | [2.24,3.97] |
| Depression type | ||||||
| No depression | 1.00 | 1.00 | 1.00 | |||
| Subsyndromal depression | 1.92*** | [1.64,2.26] | 1.89*** | [1.55,2.30] | 2.06*** | [1.59,2.67] |
| Brief depressive episode | 2.14*** | [1.88,2.43] | 2.09*** | [1.75,2.49] | 2.23*** | [1.86,2.68] |
| Depressive episode | 2.43*** | [2.21,2.67] | 2.39*** | [2.10,2.73] | 2.51*** | [2.21,2.83] |
| Binary logistic regression | ||||||
| Anxietya | 1.75*** | [1.63,1.88] | 1.69*** | [1.53,1.86] | 1.84*** | [1.65,2.05] |
| Sleep problems | 2.23*** | [2.05,2.43] | 2.25*** | [1.99,2.55] | 2.21*** | [1.98,2.47] |
| Perceived stressb | 1.43*** | [1.33,1.53] | 1.40*** | [1.28,1.52] | 1.49*** | [1.35,1.65] |
Abbreviation: OR odds ratio; CI confidence interval.
All models are adjusted for sex, age, education, wealth, setting, smoking, alcohol consumption, angina, asthma, diabetes, BMI, and country.
Turkey is not included in the regression analyses as it lacked information on education.
aMorocco is not included as it lacked information on anxiety.
bBrazil, Hungary, and Zimbabwe are not included as they lacked information on perceived stress.
***p < 0.001.
Discussion
The current large scale study involving almost a quarter of a million people over 46 LMICs established that the age- and sex-adjusted prevalence of arthritis was 22.4% across all countries and 23.4% in low-income and 20.9% in middle-income countries. In the overall sample, the correlates of arthritis estimated by multivariable logistic regression included female sex, older age, lower education, poverty, smoking, angina, asthma, diabetes, and higher BMI. In LMICs collectively, we observed that people with arthritis were consistently more likely to have depression (all subtypes), subclinical psychosis, established psychotic disorder, sleep problems, anxiety, and higher levels of perceived stress. The increased mental health comorbidity among those with arthritis was consistently raised in those in both low-income and middle-income countries.
The prevalence of arthritis (22.3%) found in our LMIC sample was higher than a previous meta-analysis on the prevalence of RA which reported that 0.16% (95%CI: 0.11–0.20%) and 0.75% (95%CI: 0.60–0.90%) of males and females respectively had RA14. Moreover, this is also higher than the prevalence of OA reported in a recent global burden of disease survey of 3% and 5% in males and females respectively in Africa and central Asia29. However, a previous study using similar definitions of arthritis as in our study have found similarly high figures in 9 LMICs, although the sample was limited to adults aged 50 years or older18. The potential reason for this might be the self-report questions used in the WHS in addition to a reflection in a potentially heightened prevalence of pain and stiffness among the sample.
In accordance with the literature in high-income countries6, 8–10, we observed heightened odds for all depression subtypes among those with arthritis versus controls. In many ways, the heightened mental health comorbidity among those with arthritis is unsurprising given the potential impact of pain, disability, and pressure to continue earning to provide an income for the family. It is interesting to note that all depression subtypes were associated with heightened odds with arthritis and to the best of our knowledge, our paper is the first multinational paper to consider this relationship. This in contrast to recent work among people with back pain in LMICs, where an incremental increased odds of depression was noted with more severe depression subtypes43. It is also perhaps of little surprise that people with arthritis were more likely to have anxiety, sleep disturbances, and perceived stress. These relationships may potentially be explained by increased levels of pain associated with arthritis. Specifically, the underlying shared pathophysiology of pain and depression could account for this, since both depression and pain facilitate modulation in the periaqueductal gray, amygdala, and hypothalamus regions44, 45. Second, arthritis46, pain, and depression47 are associated with and exacerbated by low levels of physical activity and social isolation48, 49. Thus, it is possible that these factors, which were not assessed in the current study, are implicated in the link between arthritis and worse mental health. Increasing physical activity has established efficacy in reducing both depression50, 51 and pain as well as their associated disability52 and could therefore be key to reducing the burden of this comorbidity and improving function. Finally, within the context of some LMICs, the high prevalence of HIV and tuberculosis53 may account for both the depression54 and pain associated with arthritis55.
The increased odds of arthritis among people with a diagnosis of psychosis has to the best of our knowledge not been previously reported in LMICs, and data on the relation between subclinical psychosis and arthritis is scarce. Furthermore, very few community-based multinational studies exist on these associations even in high-income countries. Our finding that arthritis is associated with higher odds for psychotic disorders (e.g. schizophrenia) is in contrast to the trend that has previously been reported. A recent meta-analysis with polygenic risk score analysis found that people with schizophrenia are at reduced odds of RA, although this does not appear to be related to polygenic risk scores and may be more related to environmental risk factors such as the anti-inflammatory effects of antipsychotic medication56. A nationally representative study in Taiwan found that people with schizophrenia were not more likely than controls to develop OA (HR = 0.89; 95%CI = 0.81–1.01), p = 0.53)57. Thus, it appears that people with psychosis in LMICs may be more likely to have arthritis compared to their high-income counterparts. The precise reasons for this are unclear and future studies are warranted to assess whether our results may be replicated. RA aside, there is evidence that any history of autoimmune disease (including psoriasis, which can have a significant joint component) can increase the odds of developing schizophrenia58. In terms of the heightened odds for subclinical psychosis in arthritis, this may be explained by the psychological distress caused by the symptoms of arthritis (e.g. pain) which has been associated with psychotic symptoms in the general population30, 59, 60.
It is established from studies conducted in high-income countries that comorbid mental health outcomes among those with arthritis are associated with worse pain and poorer treatment outcomes8, 10, 61. Thus clearly integrated mental and physical healthcare is essential. However, in the context of arthritis, there is a paucity of evidence-based literature, in particular intervention studies. Regardless, the current data have important public health implications, particularly since the data were multi-national, population-based, and predominantly nationally representative, rather than most literature to date which is derived from clinical samples. Understanding and treating comorbid mental health outcomes among those with arthritis is essential. An important environmental barrier in the care of people with mental and physical health problems in LMICs is the lack of integrated mental and physical healthcare services and the poorly developed community-based psychiatric services62. Closer integration of primary and mental health care in these countries is needed, but without obscuring the responsibility for arthritis and mental health assessment, prevention and management63. We suggest that people with arthritis are assessed for the mental health conditions assessed in our study (i.e., depression, anxiety, sleep disturbance, stress and psychosis) so that appropriate interventions can be provided. More research is required to understand the mental health burden of arthritis in LMICs and context-specific trials and evaluations in LMICs therefore are urgently needed.
Some study design limitations need to be considered. First, the categorization of arthritis was based on self-report and it was not possible to explore in more detail the type, nature, and severity of arthritis. In particular, it was not possible to differentiate between OA and RA and other forms of arthritis. Thus, clearly, future research is required to disentangle the nature and mental health impact of the different forms of arthritis in LMICs. Second, the study sample only included non-institutionalized individuals. Thus, those with severe mental disorders or arthritis could have been omitted from the sample, leading to an underestimate of the associations. Next, we adjusted for a variety of potential confounders but we cannot preclude the possibility of residual confounding. For example, we were only able to adjust for a limited number of physical comorbidities. Finally, the data is cross-sectional thus it is not possible to disentangle the directionality of the relationships observed. It is important that future research attempts to understand the underlying explanatory factors of the relationships we observed. In particular, research considering psychotic disorders and RA are required among LMICs.
In conclusion, our large community-based study has demonstrated that arthritis is associated with a broad range of elevated mental health comorbidity. For the first time we demonstrated on a multinational scale that depression subtypes, psychosis spectrum, stress sensitivity and anxiety are increased in those with arthritis. Future longitudinal research is required to elucidate the course, trajectory, and outcomes of comorbid mental health and arthritis in LMICs.
Electronic supplementary material
Acknowledgements
BS receives funding from the National Institute for Health Research Collaboration for Leadership in Applied Health Research & Care Funding scheme. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health. AK’s work was supported by the Miguel Servet contract financed by the CP13/00150 and PI15/00862 projects, integrated into the National R+D+I and funded by the ISCIII - General Branch Evaluation and Promotion of Health Research - and the European Regional Development Fund (ERDF-FEDER). DV is funded by the Research Foundation – Flanders (FWO – Vlaanderen).
Author Contributions
Study conception B.S., N.V., A.K. Data analysis A.K., B.S. Data interpretation—B.S., N.V., D.V., T.T., C.K., P.S., M.S., J.M., K.K., T.P., A.F.C., A.K. Drafting of manuscript – B.S., N.V., A.K. Providing critical revisions and approval of final version – B.S., N.V., D.V., T.T., C.K., P.S., M.S., J.M., K.K., T.P., A.F.C., A.K.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-07688-6
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Vos T, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380:2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray CJ, et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990-2013: quantifying the epidemiological transition. Lancet. 2015;386:2145–2191. doi: 10.1016/S0140-6736(15)61340-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boutron I, et al. Disability and quality of life of patients with knee or hip osteoarthritis in the primary care setting and factors associated with general practitioners’ indication for prosthetic replacement within 1 year. Osteoarthritis Cartilage. 2008;16:1024–1031. doi: 10.1016/j.joca.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 4.Cross M, et al. The global burden of rheumatoid arthritis: estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 2014;73:1316–1322. doi: 10.1136/annrheumdis-2013-204627. [DOI] [PubMed] [Google Scholar]
- 5.Smith E, et al. The global burden of other musculoskeletal disorders: estimates from the Global Burden of Disease 2010 study. Ann. Rheum. Dis. 2014;73:1462–1469. doi: 10.1136/annrheumdis-2013-204680. [DOI] [PubMed] [Google Scholar]
- 6.Matcham F, Rayner L, Steer S, Hotopf M. The prevalence of depression in rheumatoid arthritis: a systematic review and meta-analysis. Rheumatology. 2013;52:2136–2148. doi: 10.1093/rheumatology/ket169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal Of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matcham F, Norton S, Scott DL, Steer S, Hotopf M. Symptoms of depression and anxiety predict treatment response and long-term physical health outcomes in rheumatoid arthritis: secondary analysis of a randomized controlled trial. Rheumatology (Oxford) 2016;55:268–278. doi: 10.1093/rheumatology/kev306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stubbs B, Aluko Y, Myint PK, Smith TO. Prevalence of depressive symptoms and anxiety in osteoarthritis: a systematic review and meta-analysis. Age Ageing. 2016;45:228–235. doi: 10.1093/ageing/afw001. [DOI] [PubMed] [Google Scholar]
- 10.Veronese N, et al. Association between lower limb osteoarthritis and incidence of depressive symptoms: data from the osteoarthritis initiative. Age Ageing. 2016 doi: 10.1093/ageing/afw216. [DOI] [PubMed] [Google Scholar]
- 11.Kim JH, et al. Association of sleep duration with rheumatoid arthritis in Korean adults: analysis of seven years of aggregated data from the Korea National Health and Nutrition Examination Survey (KNHANES) BMJ Open. 2016;6:e011420. doi: 10.1136/bmjopen-2016-011420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parmelee PA, Tighe CA, Dautovich ND. Sleep disturbance in osteoarthritis: linkages with pain, disability, and depressive symptoms. Arthritis Care Res (Hoboken) 2015;67:358–365. doi: 10.1002/acr.22459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Treharne GJ, et al. Sleep disruption frequency in rheumatoid arthritis: perceived stress predicts poor outcome over one year. Musculoskeletal Care. 2007;5:51–64. doi: 10.1002/msc.99. [DOI] [PubMed] [Google Scholar]
- 14.Rudan I, et al. Prevalence of rheumatoid arthritis in low- and middle-income countries: A systematic review and analysis. J. Glob. Health. 2015;5:010409. doi: 10.7189/jogh.05.010101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee SH, et al. New data and an old puzzle: the negative association between schizophrenia and rheumatoid arthritis. Int. J. Epidemiol. 2015;44:1706–1721. doi: 10.1093/ije/dyv136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moussavi S, et al. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370:851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 17.Garin N, et al. Global Multimorbidity Patterns: A Cross-Sectional, Population-Based, Multi-Country Study. J. Gerontol. A Biol. Sci. Med. Sci. 2016;71:205–214. doi: 10.1093/gerona/glv128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koyanagi A, et al. Chronic conditions and sleep problems among adults aged 50 years or over in nine countries: a multi-country study. PLoS One. 2014;9:e114742. doi: 10.1371/journal.pone.0114742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int. J. Methods Psychiatr. Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ayuso-Mateos JL, Nuevo R, Verdes E, Naidoo N, Chatterji S. From depressive symptoms to depressive disorders: the relevance of thresholds. Br. J. Psychiatry. 2010;196:365–371. doi: 10.1192/bjp.bp.109.071191. [DOI] [PubMed] [Google Scholar]
- 21.Cooper L, Peters L, Andrews G. Validity of the Composite International Diagnostic Interview (CIDI) psychosis module in a psychiatric setting. J Psychiatr. Res. 1998;32:361–368. doi: 10.1016/S0022-3956(98)00021-1. [DOI] [PubMed] [Google Scholar]
- 22.Hanssen MS, Bijl RV, Vollebergh W, van Os J. Self-reported psychotic experiences in the general population: a valid screening tool for DSM-III-R psychotic disorders? Acta Psychiatr. Scand. 2003;107:369–377. doi: 10.1034/j.1600-0447.2003.00058.x. [DOI] [PubMed] [Google Scholar]
- 23.Stubbs B, et al. Physical Activity Levels and Psychosis: A Mediation Analysis of Factors Influencing Physical Activity Target Achievement Among 204 186 People Across 46 Low- and Middle-Income Countries. Schizophr. Bull. 2016 doi: 10.1093/schbul/sbw111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stubbs B, et al. Physical multimorbidity and psychosis: comprehensive cross sectional analysis including 242,952 people across 48 low- and middle-income countries. BMC Med. 2016;14:189. doi: 10.1186/s12916-016-0734-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stranges S, Tigbe W, Gomez-Olive FX, Thorogood M, Kandala NB. Sleep problems: an emerging global epidemic? findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep. 2012;35:1173–1181. doi: 10.5665/sleep.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koyanagi A, Stickley A. The Association between Sleep Problems and Psychotic Symptoms in the General Population: A Global Perspective. Sleep. 2015;38:1875–1885. doi: 10.5665/sleep.5232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wong KO, Hunter Rowe B, Douwes J, Senthilselvan A. Asthma and wheezing are associated with depression and anxiety in adults: an analysis from 54 countries. Pulm. Med. 2013;2013:929028. doi: 10.1155/2013/929028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.DeVylder JE, et al. Stress Sensitivity and Psychotic Experiences in 39 Low- and Middle-Income Countries. Schizophr. Bull. 2016;42:1353–1362. doi: 10.1093/schbul/sbw044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cross M, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 2014;73:1323–1330. doi: 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 30.Koyanagi A, Stickley A. The association between psychosis and severe pain in community-dwelling adults: Findings from 44 low- and middle-income countries. J. Psychiatr. Res. 2015;69:19–26. doi: 10.1016/j.jpsychires.2015.07.020. [DOI] [PubMed] [Google Scholar]
- 31.Rose GA. The diagnosis of ischaemic heart pain and intermittent claudication in field surveys. Bull. World Health Organ. 1962;27:645–658. [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ. Tech. Rep. Ser. 894 (2000). [PubMed]
- 33.Arokiasamy P, et al. The impact of multimorbidity on adult physical and mental health in low- and middle-income countries: what does the study on global ageing and adult health (SAGE) reveal? BMC Med. 2015;13:178. doi: 10.1186/s12916-015-0402-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Koyanagi A, Oh H, Stubbs B, Haro JM, DeVylder JE. Epidemiology of depression with psychotic experiences and its association with chronic physical conditions in 47 low- and middle-income countries. Psychol. Med. 2017;47:531–542. doi: 10.1017/S0033291716002750. [DOI] [PubMed] [Google Scholar]
- 35.McCrea RL, Berger YG, King MB. Body mass index and common mental disorders: exploring the shape of the association and its moderation by age, gender and education. Int. J. Obes. (Lond) 2012;36:414–421. doi: 10.1038/ijo.2011.65. [DOI] [PubMed] [Google Scholar]
- 36.Jane-Llopis E, Matytsina I. Mental health and alcohol, drugs and tobacco: a review of the comorbidity between mental disorders and the use of alcohol, tobacco and illicit drugs. Drug Alcohol Rev. 2006;25:515–536. doi: 10.1080/09595230600944461. [DOI] [PubMed] [Google Scholar]
- 37.Lipari, R. N. & Van Horn, S. In The CBHSQ Report (Substance Abuse and Mental Health Services Administration (US), 2013). [PubMed]
- 38.Koyanagi A, Stickley A, Haro JM. Psychotic symptoms and smoking in 44 countries. Acta Psychiatr. Scand. 2016 doi: 10.1111/acps.12566. [DOI] [PubMed] [Google Scholar]
- 39.Koyanagi A, Oh H, Stickley A, Haro JM, DeVylder J. Risk and functional significance of psychotic experiences among individuals with depression in 44 low- and middle-income countries. Psychol. Med. 2016;46:2655–2665. doi: 10.1017/S0033291716001422. [DOI] [PubMed] [Google Scholar]
- 40.Rabe-Hesketh S, Skrondal A. Multilevel modelling of complex survey data. J. R. Stat. Soc. 2006;169:805–827. doi: 10.1111/j.1467-985X.2006.00426.x. [DOI] [Google Scholar]
- 41.StataCorp. http://www.stata.com/manuals13/mimiimputechained.pdf.
- 42.Vancampfort, D. et al. Perceived Stress and its Relationship with Chronic Conditions and Multimorbidity Among 229,293 Community-Dwelling Adults in 44 Low-and Middle-Income Countries. Am. J. Epidemiol. in press (2017). [DOI] [PubMed]
- 43.Stubbs B, et al. The epidemiology of back pain and its relationship with depression, psychosis, anxiety, sleep disturbances, and stress sensitivity: Data from 43 low- and middle-income countries. Gen. Hosp. Psychiatry. 2016;43:63–70. doi: 10.1016/j.genhosppsych.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 44.Ossipov MH, Dussor GO, Porreca F. Central modulation of pain. J. Clin. Invest. 2010;120:3779–3787. doi: 10.1172/JCI43766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Millan MJ. Descending control of pain. Prog. Neurobiol. 2002;66:355–474. doi: 10.1016/S0301-0082(02)00009-6. [DOI] [PubMed] [Google Scholar]
- 46.Stubbs B, Hurley M, Smith T. What are the factors that influence physical activity participation in adults with knee and hip osteoarthritis? A systematic review of physical activity correlates. Clin. Rehabil. 2015;29:80–94. doi: 10.1177/0269215514538069. [DOI] [PubMed] [Google Scholar]
- 47.Stubbs B, et al. Physical activity and depression: a large cross-sectional, population-based study across 36 low- and middle-income countries. Acta Psychiatr. Scand. 2016;134:546–556. doi: 10.1111/acps.12654. [DOI] [PubMed] [Google Scholar]
- 48.Saito T, Kai I, Takizawa A. Effects of a program to prevent social isolation on loneliness, depression, and subjective well-being of older adults: a randomized trial among older migrants in Japan. Arch. Gerontol. Geriatr. 2012;55:539–547. doi: 10.1016/j.archger.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 49.Mammen G, Faulkner G. Physical activity and the prevention of depression: a systematic review of prospective studies. Am. J. Prev. Med. 2013;45:649–657. doi: 10.1016/j.amepre.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 50.Schuch FB, et al. Exercise improves physical and psychological quality of life in people with depression: A meta-analysis including the evaluation of control group response. Psychiatry Res. 2016;241:47–54. doi: 10.1016/j.psychres.2016.04.054. [DOI] [PubMed] [Google Scholar]
- 51.Schuch FB, et al. Exercise as a treatment for depression: A meta-analysis adjusting for publication bias. J. Psychiatr. Res. 2016;77:42–51. doi: 10.1016/j.jpsychires.2016.02.023. [DOI] [PubMed] [Google Scholar]
- 52.Uthman, O. A. et al. Exercise for lower limb osteoarthritis: systematic review incorporating trial sequential analysis and network meta-analysis. BMJ (Clinical Research Ed.) 347, f5555–f5555, doi:10.1136/bmj.f5555 (2013). [DOI] [PMC free article] [PubMed]
- 53.Deribew A, et al. Common mental disorders in TB/HIV co-infected patients in Ethiopia. BMC Infect. Dis. 2010;10:201. doi: 10.1186/1471-2334-10-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kinyanda, E. et al. Risk of major depressive disorder among older persons living in HIV-endemic central and southwestern Uganda. AIDS Care, 1–6, doi:10.1080/09540121.2016.1191601 (2016). [DOI] [PubMed]
- 55.Molony E, et al. Low back pain and associated imaging findings among HIV-infected patients referred to an HIV/palliative care clinic. Pain Med. 2014;15:418–424. doi: 10.1111/pme.12239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Euesden J, Breen G, Farmer A, McGuffin P, Lewis CM. The relationship between schizophrenia and rheumatoid arthritis revisited: genetic and epidemiological analyses. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2015;168b:81–88. doi: 10.1002/ajmg.b.32282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Huang SW, et al. Association between psychiatric disorders and osteoarthritis: a nationwide longitudinal population-based study. Medicine (Baltimore) 2016;95:e4016. doi: 10.1097/MD.0000000000004016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Benros ME, et al. Autoimmune diseases and severe infections as risk factors for schizophrenia: a 30-year population-based register study. Am. J. Psychiatry. 2011;168:1303–1310. doi: 10.1176/appi.ajp.2011.11030516. [DOI] [PubMed] [Google Scholar]
- 59.Saha S, Scott JG, Varghese D, McGrath JJ. The association between general psychological distress and delusional-like experiences: a large population-based study. Schizophr. Res. 2011;127:246–251. doi: 10.1016/j.schres.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 60.Stubbs B, et al. The prevalence and moderators of clinical pain in people with schizophrenia: A systematic review and large scale meta-analysis. Schizophr. Ress. 2014;160:1–8. doi: 10.1016/j.schres.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 61.Denkinger, M. D., Lukas, A., Nikolaus, T., Peter, R. & Franke, S. Multisite pain, pain frequency and pain severity are associated with depression in older adults: results from the ActiFE Ulm study. Age Ageing (2014). [DOI] [PubMed]
- 62.Weinmann S, Koesters M. Mental health service provision in low and middle-income countries: recent developments. Curr. Opin. Psychiatry. 2016;29:270–275. doi: 10.1097/YCO.0000000000000256. [DOI] [PubMed] [Google Scholar]
- 63.Petersen I, et al. Promotion, prevention and protection: interventions at the population- and community-levels for mental, neurological and substance use disorders in low- and middle-income countries. Int. J. Ment. Health Syst. 2016;10:30. doi: 10.1186/s13033-016-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


