Abstract
Objectives:
To assess knowledge, attitudes, and practices of primary care physicians (PCPs) toward topical corticosteroids (TCs).
Methods:
A cross-sectional, 53-item questionnaire based study on TCs was conducted among PCPs in Riyadh, Kingdom of Saudi Arabia between January and March 2015. A maximum score of 30 was calculated for the knowledge portion.
Results:
Out of 420 PCPs, 336 responded (80%). Most participants (89.6%) reported prescribing TCs. The mean knowledge score was 17.14 (SD=5.48). Only 39% PCPs correctly identified that there are 7 or 4 TCs potency groups (2 different classification systems). The MBBS/MD and diploma-certified physicians scored lower than board-qualified PCPs (p<0.05). Family medicine physicians scored higher than general practitioners (GPs) (p<0.05). Hospital-based PCPs scored better than private practice PCPs (p<0.05). Moreover, those who felt somewhat comfortable (32.5%) in treating dermatology patients were more knowledgeable (p<0.05). Lastly, 76.5% of physicians were interested in attending courses on dermatologic therapies.
Conclusion:
Knowledge of TCs among PCPs was inadequate. Targeted educational interventions delivered by dermatologists are recommended.
Both dermatologists and primary care physicians (PCPs) prescribe topical corticosteroids (TCs) to many skin disorders.1 Currently available TCs differ widely, and knowledge of such differences is vital for proper prescribing practices. When prescribing TCs, it is important to consider the indication, patient’s age, TCs potency, vehicle, frequency, duration, site of lesion, severity of disease, and associated adverse effects.2 The TCs are classified, based on their vaso-constrictive properties, into 4 potency groups according to the British National Formulary (BNF) and 7 classes based on the American system.3,4 Irrational prescription of TCs can result in unwanted effects.5 Topical corticosteroids can cause cutaneous side effects (atrophy, striae, telangiectasia, hypo-pigmentation, acne, rosacea, perioral dermatitis, and hypertrichosis), as well as systemic side effects (cataracts, hyperglycemia, and hypothalamic-pituitary-adrenal suppression).6 While their prescribing patterns have been studied,7-10 the knowledge based upon which these PCPs choose a TC has not been identified. Our study aims to assess the current knowledge, attitudes, and practices of PCPs toward TCs in Riyadh, Kingdom of Saudi Arabia (KSA). Such data would encourage the development of continuing medical education (CME) programs on dermatological therapies, to ensure their safety.
Methods
A cross-sectional study on knowledge, attitude, and practices toward TCs was conducted on PCPs working in primary care clinics (PCCs) in different regions of Riyadh, KSA. In our study, 7 public hospital PCCs, 15 private PCCs, and 27 primary healthcare centers were included. Trained medical students collected data in March 2015 from all PCPs (GPs, Family Medicine, Internal Medicine, and Pediatrics) in one of the primary care units selected. All PCPs encountered were included in the study. Incomplete questionnaires were excluded. Our questionnaire was pre-tested on 10 subjects at a PCC in a university hospital to estimate the time needed to answer all questions, and ensure their comprehension. Results of the pilot study were not included in the final analysis. The final self-administered questionnaire included 53 close-ended questions. The first part covered demographic characteristics (age, gender, nationality, qualification degree, specialty, years in practice, practice setting, and city). The second part contained 30 multiple-choice questions (MCQs) assessing knowledge towards TCs (potency, side effects, and indications of use). A maximum score of 30 was calculated for the knowledge portion. The second part also elicited physicians’ attitude towards treating dermatology patients and prescribing TCs (2 items, 5-point Likert scale), and their practice (7 items, MCQs). The third part containing 6 MCQs targeted their interest in dermatology-related educational courses and their main dermatology knowledge sources. Ethical approval was obtained from the Ethical Review Committee, College of Medicine, King Saud University. Riyadh, KSA. An informed consent was provided indicating the purpose of the study, benefits of participation, and their right to withdraw. All information was kept confidential. No incentives were given.
Assuming knowledge of TCs is 50% with precision of 5% and level of significance 0.05, we needed 384 subjects. Assuming a 10% non-response rate, the total required sample was 423. Data management and analysis were carried out using the Statistical Package for Social Sciences (SPSS, IBM Corp, Amonk, NY, USA) software version 21.11 Descriptive statistics (mean, standard deviation, frequencies, and percentages) were used to quantify quantitative and categorical study variables. Student’s t-test for independent samples was used to compare the mean values of knowledge scores, in relation to study variables with 2 categories. One-way analysis of variance (ANOVA) was used to compare the mean values of knowledge scores in relation to study variables with more than 2 categories. Post Hoc Tukey’s test was carried out to perform the pair-wise comparison of mean knowledge scores between different groups in each study variable. A p-value of <0.05 was considered statistically significant.
Results
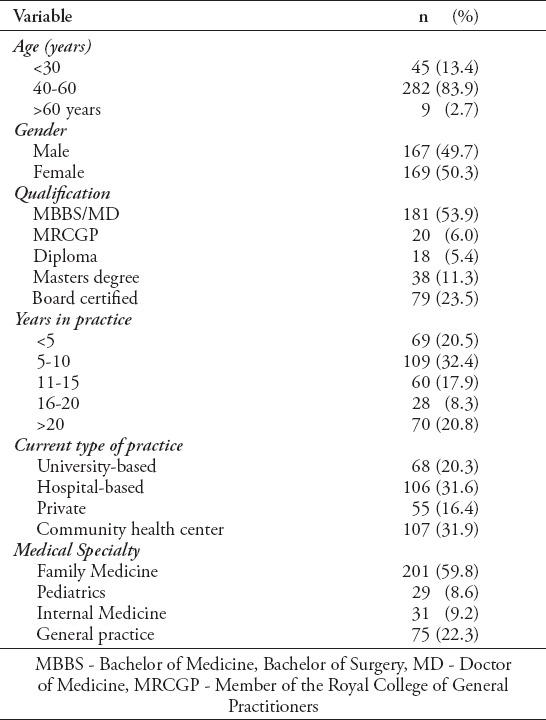
Out of 420 PCPs, 336 completed the questionnaires, with an 80% response rate (Table 1).
Table 1.
Demographic characteristics of the participating primary care physicians in Riyadh, Kingdom of Saudi Arabia (N=336)
Knowledge
Most PCPs (88.4%) were aware that different classes of potency exist; however, 39.9% physicians correctly identified the presence of 7 or 4 potency groups. When asked to rank the potency of 4 surveyed TCs, 51.2% respondents were able to identify hydrocortisone acetate 1% cream as a low potent topical steroid. There was a low level of agreement on the potency ranking of mometasone furoate 0.1% cream (36.6%), and betamethasone 0.1% cream (17.3%) as mid-potency, and clobetasol propionate 0.05% cream (19%) as a super high potent TCs. More than 50% of PCPs agreed that TCs can lead to skin atrophy, hypopigmentation, striae, and telangiectasia. However, less than half were aware that perioral dermatitis, hypertrichosis, acne, Cushing’s disease, cataract, and hypothalamic pituitary axis suppression are possible side effects. When asked to select diseases that can be relieved by TCs, 94.9% selected atopic dermatitis, 81.3% selected psoriasis, 54.5% selected alopecia areata, and 36.9% selected vitiligo. However, 33.9% incorrectly responded that TCs can be used in all skin rashes, and 37.8% in acne vulgaris. A total knowledge score between 0 and 30 was calculated for each participant, which reflected the number of correct answers regarding TCs knowledge. The mean knowledge score among PCPs surveyed was found to be 17.14 (SD= 5.48) (Figure 1).
Figure 1.
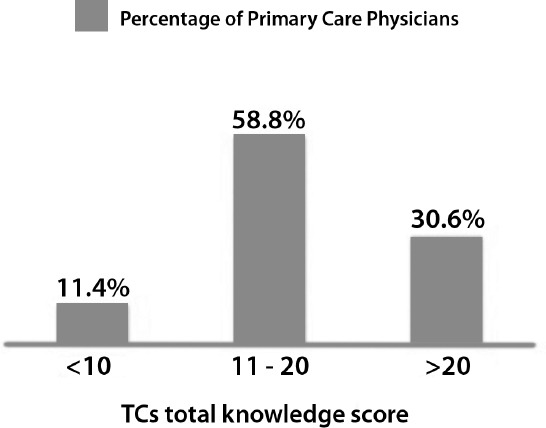
Topical corticosteroids (TCs) total knowledge score distribution among primary care physicians in Riyadh, Kingdom of Saudi Arabia (N=336).
Attitude and practice, and their association with total knowledge score
The majority of PCPs (89.6%) have prescribed TCs to one of their patients; 85% of PCPs have prescribed TCs to adults, 61.9% to children, 22.3% to infants, and 14.9% to pregnant women. Respondents’ attitudes towards treating dermatology patients were well-distributed across a 5-point Likert scale, ranging from very comfortable to very uncomfortable, and only 40.7% felt comfortable managing patients with skin problems. When asked about the approximate percentage of skin related visits, 85.7% responded with being exposed to less than 25%. When comparing the mean knowledge score, we found that those exposed to less than 10% of visits (45.8%) had a significantly lower score than those who were exposed to 10-25% of skin related visits (39.9%) (p=0.016). Also, those who felt somewhat uncomfortable (17.3%) scored lower than those who felt somewhat comfortable (34.5%) toward treating dermatology patients (p=0.003).
Associations between total knowledge score with PCPs characteristics
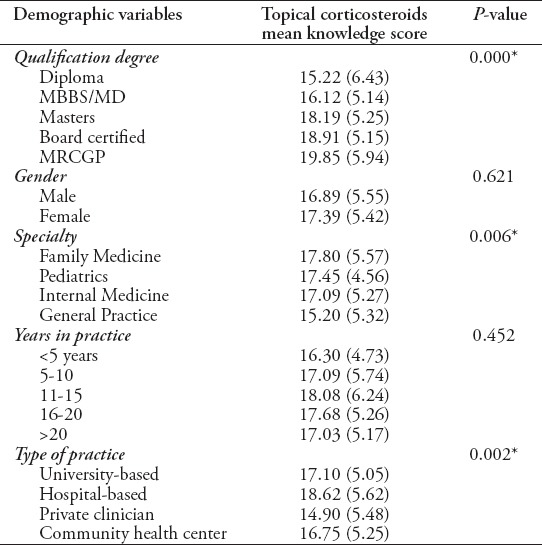
Statistically significant differences in mean knowledge scores were identified among PCPs with different practice settings, medical specialties, and qualifications (Table 2).
Table 2.
Mean knowledge scores in relation to primary care physicians’ characteristics (n=336).
Interest in dermatology-related education and knowledge sources
The majority of PCPs (84.4%) were interested in attending dermatology-related CME activity. Seventy-four percent of participants prefer conduction of dermatology-related activities annually. One-third of participants (28.1%) never attended a dermatology-related course. Textbooks were ranked first as the main source of their current knowledge on TCs among 57.1% physicians, followed by the Internet (53%).
Discussion
Dermatologic diseases are commonly encountered in PCCs. In a retrospective study conducted during a 2-year period, 36.5% of PCC patients had a cutaneous complaint.12 Another study conducted in a PCC in KSA,13 revealed that 11.5% of all new patients presenting between 1993 and 1994 had skin disorders. With the recent expansion of primary care services, the exposure of PCPs to skin disorders is expected to increase.14,15 In KSA, evidence is lacking regarding the level of proficiency of PCPs in dermatology. Only one study was conducted in 2002 with the purpose of assessing PCPs abilities in recognizing skin disorders, which showed a lack of overall proficiency.16
The PCPs need to be aware of the dangers of TCs misuse. In India, 2 studies reported patients that developed steroid induced dermatosis due TCs misuse for cosmetic purposes.17,18 In a study that assessed TCs phobia, it was reported that the most common source of patient information regarding TCs safety was the PCP. Thus, highlighting the need for the provision of better information to PCPs.19
Participants had poor knowledge when asked about potency classification of selected TC agents. It is concerning that only 19% PCPs identified clobetasol-propionate as super-high potency, given that 44.3% have reported prescribing it. Our findings differ to those reported in a recent study, which showed that most dermatologists were knowledgeable on the correct potency ranking of commonly prescribed TCs.20
Highly potent TCs can be absorbed well enough in children and infants due to their larger surface area to body weight ratio, leading to systemic side effects.6 It is therefore worrisome to find that although most participants were aware of TCs’ local side effects, less than half recognized their possible systemic side effects, even though 62% of PCPs have reported prescribing them to children, and 39% to infants.
Our study showed that physicians with only MBBS/MD and diploma degrees scored lower than those with board certification, which is likely a reflection of their higher postgraduate education. In a review study conducted to compare dermatologic diagnoses by PCPs with that of dermatologists, they found that family medicine physicians out-performed both internal medicine physicians and general practitioners.21 Similarly, our results have shown that PCPs practicing family medicine scored higher than general practitioners suggesting the broader training experience offered in family medicine residency programs. The PCPs who felt comfortable treating dermatology patients achieved higher knowledge scores. This may suggest that comfort levels might be a reflection of their knowledge background. Also, physicians who reported exposure to less than 10% of skin-related visits had the lowest knowledge scores. Such findings are not surprising, as the less exposure to dermatological complaints, the less experience the physician will gain with their therapies.
Knowledge gaps towards TCs among PCPs could be attributed to the lack of dermatology postgraduate training courses for PCPs. It is encouraging to find that most participants were interested in attending annual dermatology-related CME activities. In a study aimed to assess the learning outcomes of a 10-week postgraduate training course in dermatology among PCPs, most PCPs reported modifying their approach in managing common skin disorders after the course.22 The presence of such evidence coupled with the high interest in dermatology-related courses among surveyed PCPs is motivating to plan CME activities.
Study limitations
Include the use of convenience sample. The proportion of skin-related visits was based on PCPs’ approximation due to the lack of such records in most PCCs. Also, there might be non-respondent bias with the possibility that PCPs who are interested in dermatology might have been more inclined to complete the survey.
In conclusion, our findings suggest that the knowledge of TCs among PCPs in Riyadh is inadequate. With the increasing expectations from PCPs to provide dermatologic care, the need for postgraduate training courses in dermatology is essential. Further studies are needed to assess PCPs’ competence in managing dermatologic disorders.
References
- 1.Sulzberger MB, Witten VH. The effect of topically applied compound F in selected dermatoses. J Invest Dermatol. 1952;19:101–102. doi: 10.1038/jid.1952.72. [DOI] [PubMed] [Google Scholar]
- 2.Ference JD, Last AR. Choosing topical corticosteroids. Am Fam Physician. 2009;79:135–140. [PubMed] [Google Scholar]
- 3.Goa KL. Clinical pharmacology and pharmacokinetic properties of topically applied corticosteroids. A review. Drugs. 1988;36(Suppl 5):51–61. doi: 10.2165/00003495-198800365-00011. [DOI] [PubMed] [Google Scholar]
- 4.Jacob SE, Steele T. Corticosteroid classes: a quick reference guide including patch test substances and cross-reactivity. J Am Acad Dermatol. 2006;54:723–727. doi: 10.1016/j.jaad.2005.12.028. [DOI] [PubMed] [Google Scholar]
- 5.Rathi SK, D’Souza P. Rational and ethical use of topical corticosteroids based on safety and efficacy. Indian J Dermatol. 2012;57:251–259. doi: 10.4103/0019-5154.97655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hengge UR, Ruzicka T, Schwartz RA, Cork MJ. Adverse effects of topical glucocorticosteroids. J Am Acad Dermatol. 2006;54:1–15. doi: 10.1016/j.jaad.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 7.Rathod SS, Motghare VM, Deshmukh VS, Deshpande RP, Bhamare CG, Patil JR. Prescribing practices of topical corticosteroids in the outpatient dermatology department of a rural tertiary care teaching hospital. Indian J Dermatol. 2013;58:342–345. doi: 10.4103/0019-5154.117293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sweileh WM. Audit of prescribing practices of topical corticosteroids in outpatient dermatology clinics in north Palestine. East Mediterr Health J. 2006;12:161–169. [PubMed] [Google Scholar]
- 9.Stern RS. The pattern of topical corticosteroid prescribing in the United States 1989-1991. J Am Acad Dermatol. 1996;35(2 Pt 1):183–186. doi: 10.1016/s0190-9622(96)90319-9. [DOI] [PubMed] [Google Scholar]
- 10.Al Khaja KA, Damanhori AH, Al-Ansari TM, Sequeira RP. Topical corticosteroids in infants: prescribing pattern and prescribing errors in Bahrain. Pharm World Sci. 2007;29:395–399. doi: 10.1007/s11096-007-9087-1. [DOI] [PubMed] [Google Scholar]
- 11.IBM Corp. IBM SPSS Statistics for Windows, Version 21.0. Armonk (NY): IBM Corp; 2012. [Google Scholar]
- 12.Lowell BA, Froelich CW, Federman DG, Kirsner RS. Dermatology in primary care: Prevalence and patient disposition. J Am Acad Dermatol. 2001;45:250–255. doi: 10.1067/mjd.2001.114598. [DOI] [PubMed] [Google Scholar]
- 13.Al-Shammari S, Al-Sheikh O. Skin morbidity pattern among patients seen at a University primary care clinic in Riyadh, Saudi Arabia. The Gulf Journal of Dermatology and Venereology. 1996;3(2):22–25. [Google Scholar]
- 14.Ministry of Health. General Directorate of Statistics & Information, Health statistic book. Riyadh (Saudi Arabia): Ministry of Health; 2013. [Updated 2013 March 6; Accessed 2015 Feb 2015 10]. Available from: http://www.moh.gov.sa/en/Ministry/Statistics/book/Documents/Statistics-Book-1434.pdf . [Google Scholar]
- 15.Al-Mazrou Y, Al-Shehri A, Rao M. Principles and practice of primary health care, Kingdom of Saudi Arabia, Ministry of health. General Directorate of Health Center. 1990 [Google Scholar]
- 16.Al-Hoqail IA, Gad A, Crawford RI. Dermatology practice in primary health care services: where do we stand in the Middle East? Int J Dermatol. 2002;41:4–7. doi: 10.1046/j.1365-4362.2002.01294.x. [DOI] [PubMed] [Google Scholar]
- 17.Rathi S. Abuse of topical steroid as cosmetic cream: A social background of steroid dermatitis. Indian J Dermatol. 2006;51:154–155. [Google Scholar]
- 18.Saraswat A, Lahiri K, Chatterjee M, Barua S, Coondoo A, Mittal A, et al. Topical corticosteroid abuse on the face: a prospective, multicenter study of dermatology outpatients. Indian J Dermatol Venereol Leprol. 2011;77:160–166. doi: 10.4103/0378-6323.77455. [DOI] [PubMed] [Google Scholar]
- 19.Charman CR, Morris AD, Williams HC. Topical corticosteroid phobia in patients with atopic eczema. Br J Dermatol. 2000;142:931–936. doi: 10.1046/j.1365-2133.2000.03473.x. [DOI] [PubMed] [Google Scholar]
- 20.Sandoval LF, Davis SA, Feldman SR. Dermatologists’ knowledge of and preferences regarding topical steroids. J Drugs Dermatol. 2013;12:786–789. [PubMed] [Google Scholar]
- 21.Federman DG, Concato J, Kirsner RS. Comparison of dermatologic diagnoses by primary care practitioners and dermatologists. A review of the literature. Arch Fam Med. 1999;8:170–172. doi: 10.1001/archfami.8.2.170. [DOI] [PubMed] [Google Scholar]
- 22.Lam TP, Yeung CK, Lam KF. What are the learning outcomes of a short postgraduate training course in dermatology for primary care doctors? BMC Med Educ. 2011;11:20. doi: 10.1186/1472-6920-11-20. [DOI] [PMC free article] [PubMed] [Google Scholar]


