Abstract
Apixaban is an oral anticoagulant that directly inhibits Factor Xa and is indicated for the prophylaxis and treatment of deep venous thrombosis and stroke prevention in non-valvular atrial fibrillation. Rectus sheath hematoma is a rare, life-threatening complication of anticoagulant treatment. We describe a case of an elderly patient on apixaban for the treatment of deep venous thrombosis who developed severe abdominal pain during hospitalization. Computed tomography of the abdomen revealed left rectus sheath hematoma. Apixaban was discontinued and the patient was monitored for extension of the hematoma. After 2 days she was discharged home. Outpatient computed tomography 1 month later showed complete resolution of the rectus sheath hematoma. We recommend that clinicians become aware of the potential for rare and serious bleeding complications of anticoagulants and identify the need for early recognition and prompt management.
Key words: Rectus sheath hematoma, apixaban, anticoagulation
Competing interest statement
Conflicts of interest: Dr. Kaatz - consultant: Boehringer-Ingelheim, Janssen, Daiichi Sankyo, Bristol-Myers Squibb/Pfizer, Portola; speaker’s bureau: Janssen, Boehringer-Ingelheim, Bristol-Myers Squibb/Pfizer, and CSL Behring.
Introduction
Anticoagulants are the leading cause of adverse drug reactions and the number one category of medications with adverse reactions leading to hospitalization.1 The advent of direct-acting oral anticoagulants (DOACs) has changed the landscape of anticoagulation treatment. Clinical trials have shown that DOACs have at least non-inferior efficacy and superior safety when compared to vitamin K antagonists. One potential but rare bleeding complication of anticoagulation is rectus sheath hematoma, which carries a risk of complications if not diagnosed and managed appropriately. Rectus sheath hematoma has been reported as a complication of traditional oral anticoagulants and low-molecular-weight heparin,2,3 although thus far it has rarely been identified in patients receiving DOAC therapy.4
We report a case of apixaban-associated rectus sheath hematoma in a patient initiated on anticoagulation for acute treatment of deep vein thrombosis.
Case Report
A 68-year-old morbidly obese female with a history of hypertension, diabetes mellitus, hyperlipidemia, obstructive sleep apnea, osteoarthritis, depression/anxiety, and about 1-month post-left total knee replacement presented to the emergency department with complaints of shortness of breath, cough, wheezing, and bilateral lower extremity pain and swelling. Her blood pressure was 158/75 mm Hg, pulse 118 beats/minute, respiratory rate 20 breaths/minute, and temperature 37.6°C (99.7°F). She weighed 135 kg with a body mass index of 60 kg/m2. Laboratory studies showed normal white blood cell count, hemoglobin of 9.7 g/dL (normal range 11.5-15.5 g/dl), hematocrit of 31.1% (normal range 34%-46%), platelets of 277x103/mm3 (normal range 140-425×l03/mm3), normal protime/international normalized ratio, blood urea nitrogen of 23 mg/dL (normal range 7-17 mg/dL), and normal creatinine. Computed tomography (CT) was negative for pulmonary embolism. Arterial duplex of the bilateral lower leg revealed thrombus in the left common femoral vein, likely provoked by her recent knee replacement surgery. Clinical and radiological evidence were otherwise consistent with heart failure, prompting admission for diuresis and medical management.
Upon admission, the patient was administered enoxaparin, 1 mg/kg subcutaneously twice daily, for bridging to warfarin. On day 2 of admission, she had transitioned from enoxaparin and warfarin to apixaban, 10 mg orally twice daily. The first dose of apixaban was administered at the time that the next usual dose of enoxaparin was due.
On day 3 of admission after 3 doses of apixaban, the patient started complaining of acute onset, severe abdominal pain in the midepigastric area with radiation to the back. At that time, she was hemodynamically stable. Her abdomen was noted to have severe tenderness on the left to superficial touch but otherwise was soft and non-distended. She underwent urgent CT of the abdomen with contrast, which showed left rectus sheath hematoma measuring approximately 10×4×17 cm (Figure 1). Apixaban was discontinued and she remained hemodynamically stable. An inferior vena cava filter was placed by vascular surgery on day 4 of hospitalization, as the patient’s anticoagulation therapy was withheld in the setting of significant hematoma and acute deep vein thrombosis. By day 5, the hemoglobin had decreased 7.0 g/dL and the hematocrit to 22.3%, prompting transfusion of 2 units of packed red blood cells. No fresh frozen plasma or prothrombin complex concentrate was administered. Two days later, ultrasonography showed stabilization of the hematoma, and the patient was discharged.
Figure 1.
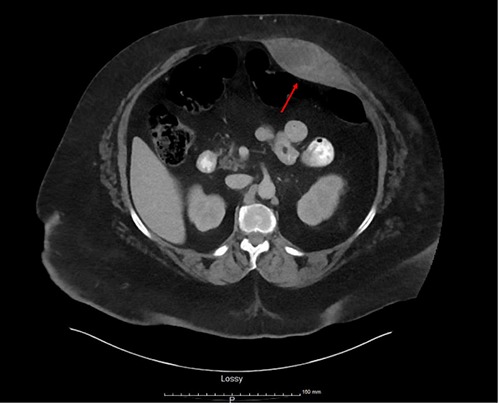
Computed tomography image showing left rectus sheath hematoma measuring approximately 10×4×17 cm.
At her follow-up visit 1 week later, the patient had a routine examination without associated complaints. No pertinent findings of the leg or filter were documented on physical examination. Her blood counts remained stable. Outpatient CT 1 month later showed resolution of the rectus sheath hematoma. Aspirin, 81 mg daily, was started upon hematoma resolution in lieu of full anticoagulation.
Discussion
Apixaban is a direct factor Xa inhibitor, which interrupts the common pathway of the coagulation cascade. Apixaban is approved for the prevention and treatment of deep vein thrombosis and pulmonary embolism, as well as for reducing the risk of thromboembolic stroke in patients with non-valvular atrial fibrillation. Treatment with apixaban does not require routine monitoring.5 Unlike warfarin, there are no specific antidotes for the anticoagulant effect of the anti-Xa DOACs. As such, the current mainstay of management of bleeding complications includes supportive care with local measures and hemodynamic or transfusion support. For severe bleeding, prothrombin complex concentrate and recombinant activated factor VII have been recommended.6
Rectus sheath hematoma is a rare but substantial complication associated with significant morbidity and occasional mortality. It is the result of bleeding into the rectus sheath from damage to the superior or inferior epigastric arteries or their branches, or from a direct tear of the rectus muscle.7 Common risk factors and causes of rectus sheath hematoma, while difficult to fully evaluate given the rare incidence, include anticoagulation, blunt or penetrating trauma or surgical trauma, pregnancy, female gender, older age, hypertension, medical conditions such as collagen vascular disorders, degenerative muscle diseases, or hematologic disorders and rectus muscle strain due to exercise, and increased abdominal pressure from straining or severe coughing.7-10 Early recognition and assessment, in conjunction with timely treatment, is the cornerstone approach to reducing potential complications associated with rectus sheath hematoma, such as hemodynamic instability, abdominal compartment syndrome, and occasionally death. Management of rectus sheath hematoma depends on factors such as the severity and size of the hematoma, the hemodynamic status of the patient, and the extent of anticoagulation.11 Less severe rectus sheath hematoma is usually self-limiting and can be managed with conservative treatment such as rest, analgesia, ice, and compression. For patients who are hemodynamically unstable, fluid resuscitation or blood transfusion and reversal of anticoagulation may be warranted. Higher severity hematomas may require more invasive management, such as angiography with embolization or surgical exploration and evacuation.2,3,7,8
A search of the literature identified only 3 case reports of DOAC-associated rectus sheath hematoma, one associated with apixaban and two with rivaroxaban. Aktas et al.4 reported a spontaneous rectus sheath hematoma in a 71-year-old female treated with apixaban for non-valvular atrial fibrillation for 3 months prior to presentation. The apixaban dose was appropriate per labeled indication, although the patient had renal impairment and was on concurrent therapy with diltiazem, an inhibitor of P-glycoprotein and CYP3A4, posing a drug interaction and possible increased risk of bleeding. The rectus sheath hematoma was diagnosed after the patient presented with abdominal pain for 24 h, in the presence of coughing precipitated by an upper respiratory tract infection. The patient had experienced no trauma or other inciting events. Management was conservative, consisting of removal of the offending agent, fluid resuscitation, and serial hemoglobin measurements. Ultimately, the patient’s apixaban was reinitiated at a lower dose 5 days post-intervention with no further complaints at 1-week follow-up after discharge.4
Kocayigit et al.12 reported a spontaneous rectus sheath hematoma in a 75-year-old female treated with rivaroxaban for non-valvular atrial fibrillation, initiated 3 days prior to presentation. The patient had presented to the emergency department with complaints of fatigue and abdominal pain after rigorous coughing. She had no recent trauma or surgery and was not taking any other medications that could have contributed to the rectus sheath hematoma. Rivaroxaban was discontinued, fluid resuscitation and packed red blood cells were administered, and the patient was referred to surgery due to hemodynamic instability. The authors did not report the patient outcome.12
Talari et al.13 reported a spontaneous rectus sheath hematoma in a 65-year-old male treated with rivaroxaban for deep vein thrombosis and pulmonary embolism. The patient presented with right-sided abdominal pain after 1 week of dry vigorous coughing due to losartan. Losartan and rivaroxaban were discontinued and packed red blood cells were given. No surgical intervention was required, and the patient clinically improved over time.
Conclusions
Clinicians should have a high suspicion of rectus sheath hematoma in patients on anticoagulant therapy, including DOACs, who present with acute abdominal pain and other associated symptoms. This report emphasizes the need for careful use of DOACs, calling attention to the need for appropriate monitoring assays and DOAC reversal agents.
Acknowledgments
The authors would like to thank Ibrahim Sayyid, MD, and Kelly Rudd, PharmD, FCCP, BCPS, CACP, for their contributions to this patient’s care and assisting with the review of this manuscript.
References
- 1.Shehab N, Lovegrove MC, Geller AI, et al. US emergency department visits for outpatient adverse drug events, 2013-2014. JAMA 2016;316:2115-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sheth HS, Kumar R, DiNella J, et al. Evaluation of risk factors for rectus sheath hematoma. Clin Appl Thromb Hemost 2016;22:292-6. [DOI] [PubMed] [Google Scholar]
- 3.Sullivan LE, Wortham DC, Laytton KM. Rectus sheath hematoma with low molecular weight heparin administration: a case series. BMC Res Notes 2014;7:586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aktas H, Inci S, Dogan P, Izgu I. Spontaneous rectus sheath hematoma in a patient treated with apixaban. Intractable Rare Dis Res 2016;5:47-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bristol-Myers Squibb Company. Eliqus (apixaban) [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2016. [Google Scholar]
- 6.Kaatz S, Crowther M. Reversal of target-specific oral anticoagulants. J Thromb Thrombolysis 2013;36:195-202. [DOI] [PubMed] [Google Scholar]
- 7.Hatjipetrou A, Anyfantakis D, Kastanakis M. Rectus sheath hematoma: a review of the literature. Int J Surg 2015;13:267-71. [DOI] [PubMed] [Google Scholar]
- 8.Cherry WB, Mueller PS. Rectus sheath hematoma: a review of 126 cases at a single institution. Medicine (Baltimore) 2006;85:105-10. [DOI] [PubMed] [Google Scholar]
- 9.Alla VM, Karnam SM, Kaushik M, Porter J. Spontaneous rectus sheath hematoma. West J Emerg Med 2010; 11: 76-9. [PMC free article] [PubMed] [Google Scholar]
- 10.Donaldson J, Knowles CH, Clark SK, et al. Rectus sheath haematoma associated with low molecular weight heparin: a case series. Ann R Coll Surg Engl 2007;89:309-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stillman K, Kellar J. Rectus sheath hematoma: an unfortunate consequence of novel anticoagulants. West J Emerg Med 2015;16:420-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kocayigit I, Can Y, Sahinkus S, et al. Spontaneous rectus sheath hematoma during rivaroxaban therapy. Indian J Pharmacol 2014;46:339-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Talari G, Talari P, Sweigart J, Ahmed S. Rare case of losartan-induced cough complicated by rectus sheath haematoma: in a patient on rivaroxaban therapy. BMJ Case Rep 2016;2016: bcr2016217801. [DOI] [PMC free article] [PubMed] [Google Scholar]


