Abstract
Objectives
To identify barriers to effective pain management encountered by patients with chronic pain within the UK’s National Health Service (NHS).
Design
Secondary analysis of face-to-face, semistructured qualitative interviews using thematic analysis.
Setting
A community-based chronic pain clinic jointly managed by a nurse and pharmacist located in the North of England.
Participants
Nineteen adult (>18 years) patients with chronic pain discharged from a pain clinic, with the ability to understand and speak the English language.
Results
In general, patients were highly disappointed with the quality of pain management services provided both within primary and secondary care, and consequently were willing to seek private medical care. Barriers to effective pain management were divided into two main themes: healthcare professional-related and health systems-related. Three subthemes emerged under healthcare professionals-related barriers, namely (1) healthcare professionals’ lack of interest and empathy, (2) general practitioners’ (GP) lack of specialised knowledge in pain management and (3) lack of communication between healthcare professionals. Three subthemes emerged under health system-related barriers: (1) long waiting time for appointments in secondary care, (2) short consultation times with GPs and (3) lack of an integrated multidisciplinary approach.
Conclusions
The patients expressed a clear desire for the improved provision and quality of chronic pain management services within the NHS to overcome barriers identified in this study. An integrated holistic approach based on a biopsychosocial model is required to effectively manage pain and improve patient satisfaction. Future research should explore the feasibility, effectiveness and cost-effectiveness of integrated care delivery models for chronic pain management within primary care.
Keywords: Barriers, Pain management, Chronic pain, Primary care, General Practitioners
Introduction
Chronic pain is one of the leading causes of disability globally.1The prevention and/or effective management of chronic pain remains a serious challenge for public health authorities and healthcare systems around the world. It has been estimated that chronic pain affects 100 million adults in the USA2 and 28 million in the UK.3 Compared with patients with other chronic diseases, patients with chronic pain tend to have poorer quality of life and use more healthcare resources.4–6
Effective management of chronic pain is essential to limit its interference with sleep, work, physical and emotional functioning, thus reducing the humanistic, societal and economic burden associated with this condition. Unfortunately, management of chronic pain remains suboptimal within primary care.5, 7 This is primarily because primary care services are often based on a ‘biomedical model’ rather than a ‘biopsychosocial model’, the latter being appropriate given the multidimensional nature of chronic pain.8, 9 Multidisciplinary clinics based on the biopsychosocial model have been shown to be effective and cost-effective.8, 9 However, long waiting times for appointments, accessibility and affordability remain a serious concern.10
The study reported here builds further on our existing knowledge of the issues and challenges faced by patients with chronic pain especially within primary care settings.11 It describes findings from secondary analysis of qualitative data obtained during a mixed-methods study.12, 13 The main findings of the mixed-methods study are described elsewhere.13 The aim of undertaking this analysis was to identify barriers to effective pain management experienced by patients with chronic pain within the UK’s National Health Service (NHS).
Methods
A qualitative description14design consisting of semistructured, face-to-face interviews was used in this study. Qualitative description is commonly used by health service and practice researchers14 as it is considered the method of choice when straightforward description of patients’, caregivers’, relatives’ or healthcare professionals’ experiences with a particular phenomenon is desired.14
Sampling and recruitment
The interviews were conducted as part of a larger mixed-methods study that evaluated the effectiveness of an NHS nurse-pharmacist-managed pain clinic.12, 13 The study design and working of the clinic have been described in detail elsewhere.13, 15 Patients who were enrolled in the quantitative phase of the mixed-methods study and discharged from the clinic within the study period were invited to participate in the interviews. A combination of two sampling techniques, convenience sampling and maximum variation sampling, was used to recruit patients.16 Convenience sampling was used to recruit the first five patients and the remaining 14 patients were recruited using maximum variation sampling. The framework for maximum variation was based on baseline pain intensity, duration of chronic pain and gender. Data collection continued until achieving ‘Data saturation’, whereby no new themes emerged from the data.16 Each interview lasted between 30 and 45 min. Written informed consent was obtained from all the study participants prior to the interview.
Data collection
Interviews were conducted by the first author, a research pharmacist trained in qualitative research, either in patients’ homes or at the pain clinic, depending on patients’ preferences. To limit recall bias, all patients were interviewed within 2 weeks of their discharge from the clinic. Interviews were audio-recorded. A semistructured interview schedule (online Supplementary file 1) was developed based on the literature and study objectives to guide the interviewer and ensure uniformity. The interview schedule guide covered the following areas: patients’ experiences of living with chronic pain (impact on physical functioning, sleep, emotions and so on), interaction with general practitioners (GPs)/primary care physicians (PCPs) and other healthcare providers, experiences of the referral system, expectations of the pain clinic, efficacy of the service and overall experiences. Patients were also provided with an opportunity to talk about any other issue related to chronic pain that was not covered during the interview.
bmjopen-2017-016454supp001.pdf (22.2KB, pdf)
Data analysis
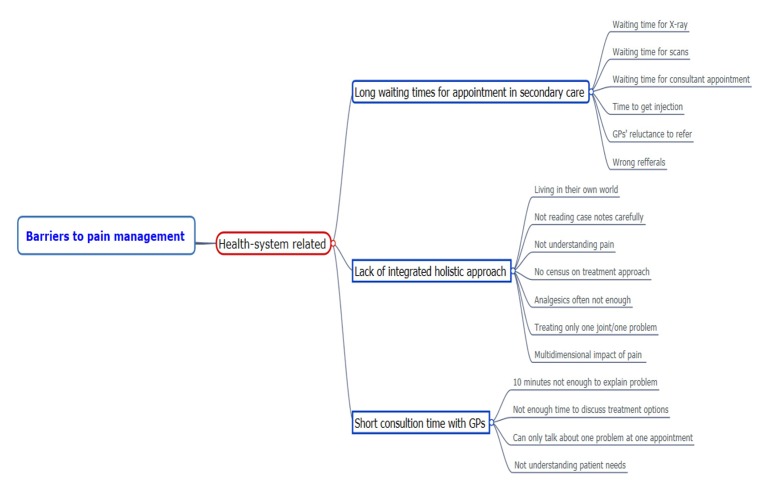
Data were analysed using thematic analysis.14 A six-step process proposed by Braun and Clarke was used to guide the data analysis.17 Each interview was transcribed verbatim and transcripts were checked against the original recording for accuracy by the interviewer (MAH). This also allowed him to familiarise himself with the data. Line-by-line coding was used to code individual transcripts, and the coding framework was checked independently by two experienced qualitative researchers for validity (MB, SJC). Duplicate codes were removed and different codes were sorted into potential themes. The relevant data extracts from individual interviews were gathered within these potential themes. Old themes were reviewed and sometimes renamed in the light of the emergence of new themes. An illustrative example of data analysis is presented in figure 1. Methods such as peer review/debriefing and providing rich thick description were used to enhance rigour and trustworthiness of study findings.16
Figure 1.
Example of data analysis.
Results
Nineteen patients were interviewed and their sociodemographic and clinical characteristics are shown in table 1. Emerging themes were classified under two overarching barriers: healthcare professional related-barriers and health system-related barriers (figure 1). Subthemes within each of these themes are described below, without any specific hierarchy/order.
Table 1.
Sociodemographic characteristics of the patients
| ID |
Age
(years) |
Gender | Chronic pain duration in years |
Pain intensity
(baseline) |
| P. 1 | 36–40 | Female | 5–10 | 5 |
| P. 2 | 46–50 | Male | 5–10 | 5 |
| P. 3 | 61–65 | Male | 5–10 | 5 |
| P. 4 | 26–30 | Male | 5–10 | 6 |
| P. 5 | 71–75 | Female | <1 | 0 |
| P. 6 | 56–60 | Female | >10 | 7 |
| P. 7 | 36–40 | Male | 1–3 | 7 |
| P. 8 | 36–40 | Female | <1 | 7 |
| P. 9 | 51–55 | Male | 3–5 | 10 |
| P. 10 | 51–55 | Female | 3–5 | 7 |
| P. 11 | 41–45 | Female | 1–3 | 5 |
| P. 12 | 36–40 | Female | >1 | 8 |
| P. 13 | 51–55 | Male | 5–10 | 10 |
| P. 14 | 61–65 | Female | >10 | 5 |
| P. 15 | 51–55 | Male | 3–5 | 9 |
| P. 16 | 51–55 | Female | 1–3 | 6 |
| P. 17 | 46–50 | Female | >10 | 4 |
| P. 18 | 26–30 | Female | 1–3 | 5 |
| P. 19 | 46–50 | Male | >10 | 7 |
Adapted and modified from Hadi et al.13
Healthcare professionals-related barriers
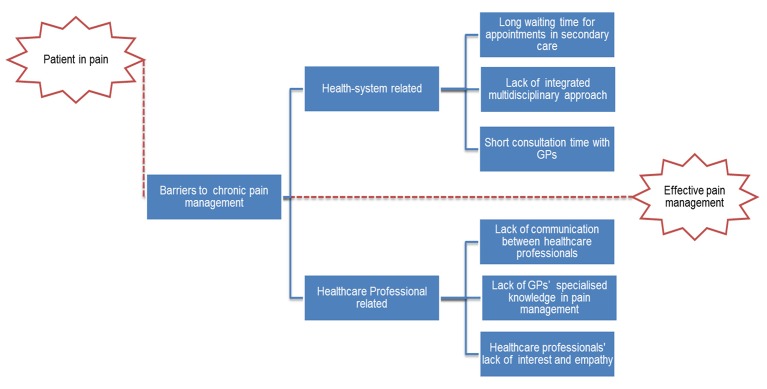
Healthcare professional-related barriers included lack of interest and empathy, lack of GP’s specialised knowledge in pain management and lack of communication between healthcare professionals. Since chronic pain was predominantly managed in primary care, a number of the barriers in this category were related to the GPs’ ability to assess and manage chronic pain (figure 2).
Figure 2.
Barriers to effective pain management. GP, general practitioner.
Healthcare professionals’ lack of interest and empathy
A number of patients expressed concerns over a perceived lack of interest shown by healthcare professionals, especially GPs, in listening to their problems and managing their pain. The patients felt that, as chronic pain was not a life-threatening disease (eg, cancer), healthcare professionals were not interested in identifying the cause of the pain. The patients were disappointed and felt that they were wasting their time in explaining their problem as no one was interested in listening to their problems. A few of the patients felt that rheumatologists were only interested in listening to their initial problems, but not to their other ongoing problems, which sometimes might have been of more importance to the patients.
“I went to my GP and was just told it’s wear and tear, age, nothing we can do about it, left it at that.” (P. 9, male)
“And then from rheumatology they don’t listen to you, they don’t…they listen to the initial problem and then they just do what they want to do.” (P. 4, male)
Some patients felt that the GPs did not appreciate the negative impact of chronic pain on their daily lives and were very frustrated. A number of the patients felt they were disbelieved and judged by healthcare professionals. They were annoyed by these attitudes and this led them to stop seeking further treatment from that particular healthcare professional. Patients felt that they were treated impersonally, being passed from one healthcare professional to another.
“The second physiotherapist I saw basically told me that the pain was in my imagination. So I had one appointment with him. I’m in enough pain not to be able to tolerate people who are telling me it’s not real, you know, because it is real.” (P. 10, female)
“…because the way that they treat you is absolutely disgusting from point to point, there’s no…you’re treated as a number, you’re not treated as a person.” (P. 4, male)
However, some patients praised some GPs who listened to them and showed a duty of care towards them.
“…I don’t feel as they’ve [GPs] just been giving me anything just to get rid of me, no they’ve been good.” (P. 16, female)
Lack of GPs’ specialised knowledge in pain management
The main reason highlighted by patients for GPs’ inability to effectively manage chronic pain was a perceived lack of specialised knowledge in chronic pain management. The patients felt that the GPs do not have the right qualifications and skills to effectively manage chronic pain. Patients viewed GPs as having limited therapeutic options, with their approach towards pain management being confined to prescribing a range of analgesics, irrespective of whether the patients were gaining any benefit or not.
“I’m not saying my GP isn’t qualified but he is a general practitioner, he’s not a consultant and he’s not specialised in that area.” (P. 6, female)
“…According to them [GPs] all they could do was give me paracetamol, and the best was co-codamol.” (P. 9, male)
A few of the patients also felt that this lack of specialised knowledge was used as an excuse by the GPs to refer to the physiotherapist without establishing whether the patients actually needed physiotherapy or not.
“I think the GP finds it an easy…she doesn’t know…it’s the easy answer to shove you to the physio and let them have a look at you and then see what bounces back out of that.” (P. 4, male)
Lack of communication between healthcare professionals
Since the patients were referred to various specialists, they were concerned about the lack of communication between the different healthcare professionals, which often led to inconsistency in their approach towards pain management. The patients felt that a number of unnecessary referrals were made due to the lack of effective communication between healthcare professionals. These unnecessary referrals wasted both time and money and added to patients’ frustration.
“I think you tend to see everybody in isolation. So the physio will refer and they will write a little letter and they will refer to a podiatrist. But then the podiatrist kind of sees the problem from such a different light that they’re not really communicating with each other…” (P. 1, female)
“I went to the doctors, it’s nothing. Tennis elbow, then it was arthritis, then it wasn’t arthritis, then it was because of a previous injury. I came here, the physiotherapist looked at the x-ray and couldn’t understand why I’d been referred here.” (P. 9, male)
In some instances the lack of communication led to a clash of opinions between the healthcare professionals and left patients confused about their diagnosis.
“I was caught up in a bit of a battle between them two [Rheumatologist and Orthopaedic surgeon] because the rheumatologist was saying, no it’s not a rheumatology problem and the orthopaedic guy was saying, well we believe it is.” (P. 15, male)
Healthcare system-related barriers
Healthcare system-related barriers included short consultation time with GPs, long waiting time for appointments in secondary care and the lack of a holistic approach.
Short consultation time with GPs
Another problem frequently stated by patients was the short consultation time with GPs. This meant that the GPs could not listen to the patient’s full story and therefore could not design an individualised therapeutic plan to meet their needs.
“It’s the running of the GPs basically, we’re not getting heard [Pause], patients aren’t getting heard and listened to. There’s not enough time.” (P. 6, female)
“No sadly I don’t think the GPs have enough time to look at each individual and to go through their medical history to see if they can tweak it here and there to help that patient. Sadly they haven’t.” (P. 12, female)
In some cases, the patients felt that due to the limited consultation time, GPs just prescribed medicines as requested by them without obtaining a full history, putting them at high risk of experiencing an adverse or even life-threatening event.
“The GP was worried about the high blood pressure but didn’t take time to look at the medication she’d actually put me on, whereas the pharmacist pointed it out to her. Potentially according to the pharmacist, for three months, I was at high risk of having a stroke.” (P. 9, male)
Long waiting time for appointments in secondary care
The patients were concerned over the long waiting times not only for appointments with consultants but also for scans, X-rays and other tests. The long waiting time delayed the whole care process. The patients felt that there were too many potentially avoidable steps in the referral process, which contributed to their dissatisfaction with the service that they received from the NHS. In some instances, the patients remained for a long time under the care of their GPs without making any noticeable progress in terms of pain relief before being referred to a consultant/pain management service.
“You’re going round the houses to get back to where you want to be. It takes a long time, it does take a long time.” (P. 3, male)
“I was brought up to think that the Health Service would provide everything, but it doesn’t, not quickly enough.” (P. 5, female)
Since the patients were not happy with the long waiting time for the appointments in secondary care, they expressed their desire to go for private treatment, provided that they had the funds to meet the cost.
“…if I could afford it I’d go private, put it that way.” (P. 4, male)
Patients who were able to afford it went on to seek care from the private sector and felt that the service provided there was much better than the NHS. As the patients had already paid into the NHS as taxpayers, they expected a good service from it. They were annoyed by the fact that they perceived the treatment was in fact better in the private sector, and they had to pay again to obtain this good service.
“I find the private sector, you know, service is much better. I do, I’ve found the NHS physio not very… [Pauses], if you are paying for treatment it is better, let’s face it.” (P. 11, female)
“You wait so long in the [National] Health Service. But I had no alternative really except pay to see somebody, and that really rankles me, I don’t want to do that. Because I’ve paid into it, haven’t I? And my husband all these years.” (P. 5, female)
Lack of integrated multidisciplinary approach
The set-up and the working of chronic pain management services in the NHS were seen as a hindrance in delivering integrated holistic care to patients. As chronic pain has a multidimensional impact on patients’ lives, a unidimensional approach towards its management based on the biomedical model may not achieve optimum outcomes. The patients felt that they were not managed as a whole, but that specialists instead focused on only one of the affected areas or joints. Therefore, there was a lack of a holistic approach in terms of the working and integration of chronic pain services and also in terms of management of patients with chronic pain.
“Within the NHS, every individual is great and they work really hard and they’re really supportive, but they seem to be very caught in their little boxes and can’t, or aren’t allowed to, step outside them to maybe provide a more effective solution sometimes.” (P. 1, female)
“He was not interested in any other joints, just the left elbow and I wanted them to look at all.” (P. 9, male)
The patients stressed the need for a collaborative approach and believed that structural reforms were needed within the NHS so that it could better serve the needs of the population of patients with chronic pain. However, the patients felt that the current situation of pain management services is unlikely to improve as the NHS is not willing to spend money to make the necessary reforms to improve chronic pain management.
“As well as the physical pain it can cause emotional problems and I think it’s important to have a service where kind of all of that can be addressed together.” (P. 18, female)
“I don’t know whether that’s a cost thing, whether arthritis is not a sexy disease like cancer or other things that the NHS want to throw money at.” (P. 9, 51-year-old male)
Discussion
The aim of this study was to explore the perspectives of patients with chronic pain on the barriers hindering the effective delivery of quality pain management services. Identifying such barriers could facilitate healthcare professionals’ and policy makers’ ability to design and implement strategies to improve delivery of pain management services. This is especially important in front-line primary care settings, as access to adequate therapy has been declared to be a human right by various international resolutions.18,19
In this study various healthcare professional-related and health system-related barriers have been highlighted. Since chronic pain is primarily managed within primary care, a number of themes revolved around GPs’ ability to manage pain. In general, patients expressed considerable dissatisfaction with the quality of care provided by the NHS. However, it should be noted that patient satisfaction is primarily determined by patient expectations.20 A mismatch between patients’ expectations and treatment outcome can lead to dissatisfaction. A systematic review reported that the best pain reduction intervention reduces pain, on average, only by 30% in about half of treated patients, meaning patients expecting cure or substantial reductions in pain are likely to be dissatisfied.21 Therefore, managing patients’ expectations before and during treatment is critical in ensuring their satisfaction.
A common perception existed among patients that GPs lacked the specialised knowledge needed to manage chronic pain effectively. In studies from the UK and USA, GPs/PCPs (primary care providers) have described helplessness and dissatisfaction with their own ability to manage patients with chronic pain.22–24 This lack of confidence may be explained by inadequate coverage of chronic pain in undergraduate medical curricula, highlighted in studies from the Europe and USA.25, 26 Furthermore, in the UK, significant increase in GPs’ workload due to funding cuts in primary care services and difficulties retaining GPs within the NHS might also be compromising GPs’ ability to effectively manage chronic pain.27 Between 2010/2011 and 2014/2015 face-to-face and telephone consultations grew by 13% and 63%, respectively. However, the GP workforce grew by only 4.75% during the same period.27 The ageing population, increase in the number of patients with multimorbidity and growing patient expectations are exacerbating these workload pressures.27
A key concern expressed by patients was poor patient–professional partnerships due to lack of trust, empathy and communication. For patients with long-term conditions, effective patient–physician relations can improve patients’ health28 and encourage self-management, key for chronic pain management. The lack of trust between patients and doctors may have negative impact on patient outcomes.28–30 Another key issue highlighted by the patients was the lack of interdisciplinary chronic pain services within the NHS. A need to reform chronic pain services within the NHS was also emphasised in order to facilitate the effective delivery of quality services. The UK’s National Pain Audit found that of the 204 pain services evaluated, only 40% of clinics in England met the minimum criteria for multidisciplinary clinics by having a psychologist, a physiotherapist and a physician.31 The clinical and cost-effectiveness of multidisciplinary clinics have been well documented in the literature,8,9 and therefore access to and affordability of multidisciplinary clinics should be made a priority to improve chronic pain management.
Patients were also concerned about the long waiting time for consultations in secondary care. The waiting time for 6 months or more from the time of referral to treatment is associated with a worsening of health-related quality of life and psychological well-being.32 The International Association for the Study of Pain Task Force on Wait Times has recommended waiting times for urgent or semiurgent and routine appointments to be within 4 and 8 weeks, respectively.33 In the UK, prior to the publication of the core standards of pain management services by the Faculty of Pain Medicine, Royal College of Anaesthetics,34 in 2015, generic waiting times standards, usually 18 weeks, were being followed as reported in the National Pain Audit.31 The patients also felt that the lack of communication between healthcare professionals led to unnecessary referrals, adding to patients’ frustration. This also partly contributed to the long waiting time for appointments in secondary care.
There are some limitations to our research findings. First, since these findings have been drawn from the secondary analysis of qualitative data that were collected as part of a mixed-methods study, some of the barriers might not have been identified as the interview guide was not exclusively developed to explore barriers to effective pain management. However, as mentioned earlier, the interview guide had questions related to patients’ experiences of healthcare services and interactions with healthcare professionals. Second, the generalisability/transferability of study findings should be carefully considered as the data were collected from the patients discharged from a single community-based pain clinic and therefore may not necessarily reflect experiences of patients with chronic pain living in other UK cities. However, the patients were referred to the pain clinic by different general practices within the catchment area. Furthermore, the sample was quite diverse in terms of chronic pain conditions, duration of chronic pain and pain sites.
Implications for practice and policy
The study findings have highlighted a perceived need to improve quality and delivery of healthcare services for patients with chronic pain. Ideally, a national action plan involving all key stakeholders should be developed with the aim of improving access to and delivery of pain services within the NHS. Since chronic pain is primarily managed within primary care, there is a need to increase resources in this setting as a first step. Given the high workload for GPs, other healthcare professionals, such as nurses and pharmacists, could be engaged in greater numbers in chronic pain management within primary care settings.13,35 Based on the findings of the present study and previously published literature, areas for improvement in terms of chronic pain management service delivery include, but not limited to, improving GPs’ capacity to manage pain, engaging patients in decision making and promoting self-management, developing evidence-based referral guidelines, improving communication between healthcare professionals and integrating existing services, and developing multidisciplinary pain clinics.
Conclusion
The present study has identified a number of barriers to effective management of chronic pain. Given that access to adequate pain relief is a human right,18, 19 health policy makers should recognise suboptimal management of chronic pain as a serious public health issue and design multifaceted strategy to improve quality and delivery of chronic pain services. Identifying barriers should be seen as the first step to designing more effective chronic pain services. Without having a clear vision, political will and chronic pain as research priority, the current situation is unlikely to improve.
Supplementary Material
Footnotes
Acknowledgements: The authors would like to thank all the patients who participated in the study. The authors are also grateful to Linda Simpson, Clinical Pharmacist at the Boots Pharmacy, for her help in patient recruitment.
Contributors: MAH conceived the idea. MAH and KM recruited patients. MAH analysed data under the supervision of MB, DPA and SJC. MAH prepared the first draft, which was revised with intellectual input by MB, DPA and SJC. All authors have read and approved the final version.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: Yorkshire and the Humber – Leeds West NHS Ethics Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Additional supporting data are available upon request from the corresponding author.
References
- 1. Vos T, Flaxman AD, Naghavi M, et al. . Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2163–96. 10.1016/S0140-6736(12)61729-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Institute of Medicine Report from the Committee on Advancing Pain Research, Care, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education and Research. The National Academies Press, 2011. http://books.nap.edu/openbook.php?record_id=13172&page=1. [PubMed] [Google Scholar]
- 3. Fayaz A, Croft P, Langford RM, et al. . Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJ Open 2016;6:e010364 10.1136/bmjopen-2015-010364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Blyth FM, March LM, Brnabic AJ, et al. . Chronic pain and frequent use of health care. Pain 2004;111:51–8. 10.1016/j.pain.2004.05.020 [DOI] [PubMed] [Google Scholar]
- 5. Breivik H, Collett B, Ventafridda V, et al. . Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006;10:287–333. 10.1016/j.ejpain.2005.06.009 [DOI] [PubMed] [Google Scholar]
- 6. Laas K, Roine R, Räsänen P, et al. . Health-related quality of life in patients with common rheumatic diseases referred to a university clinic. Rheumatol Int 2009;29:267–73. 10.1007/s00296-008-0673-x [DOI] [PubMed] [Google Scholar]
- 7. McDermott ME, Smith BH, Elliott AM, et al. . The use of medication for chronic pain in primary care, and the potential for intervention by a practice-based pharmacist. Fam Pract 2006;23:46–52. 10.1093/fampra/cmi068 [DOI] [PubMed] [Google Scholar]
- 8. Guzman J. Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ 2001;322:1511–6. 10.1136/bmj.322.7301.1511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Scascighini L, Toma V, Dober-Spielmann S, et al. . Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology 2008;447:670–8. 10.1093/rheumatology/ken021 [DOI] [PubMed] [Google Scholar]
- 10. Lynch ME, Campbell FA, Clark AJ, et al. . Waiting for treatment for chronic pain - a survey of existing benchmarks: toward establishing evidence-based benchmarks for medically acceptable waiting times. Pain Res Manag 2007;12:245–8. 10.1155/2007/891951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Glajchen M. Chronic pain: treatment barriers and strategies for clinical practice. J Am Board Fam Pract 2001;14:211–8. [PubMed] [Google Scholar]
- 12. Hadi MA, Alldred DP, Closs SJ, et al. . A mixed-methods evaluation of a nurse-pharmacist-managed pain clinic: design, rationale and limitations. Can Pharm J 2013;146:197–201. 10.1177/1715163513490400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hadi MA, Alldred DP, Briggs M, et al. . Effectiveness of a community based nurse-pharmacist managed pain clinic: a mixed-methods study. Int J Nurs Stud 2016;53:219–27. 10.1016/j.ijnurstu.2015.09.003 [DOI] [PubMed] [Google Scholar]
- 14. Sandelowski M. What's in a name? qualitative description revisited. Res Nurs Health 2010;33:77–84. 10.1002/nur.20362 [DOI] [PubMed] [Google Scholar]
- 15. Hadi MA, Alldred DP, Briggs M, et al. . A combined nurse-pharmacist managed pain clinic: joint venture of public and private sectors. Int J Clin Pharm 2012;34:1–3. 10.1007/s11096-011-9591-1 [DOI] [PubMed] [Google Scholar]
- 16. Green J, Thorogood N. Qualitative Methods for Health Research. 2009. London: Sage. [Google Scholar]
- 17. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Phychol 2006;2:77–101. [Google Scholar]
- 18. International Association for the Study of Pain and delegates of International Pain Summit 2010: Declaration that Access to Pain Management is a Fundamental Human Right. 2010. http://www.iasp-pain.org/Content/NavigationMenu/Advocacy/DeclarationofMontr233al/default.htm (accessed 10 July 2016).
- 19. World Medical Association. WMA Resolution on the Access to Adequate Pain Treatment, Adopted by the 62nd WMA General Assembly, Montevideo, Uruguay. 2011. http://www.wma.net/en/30publications/10policies/p2/index.html (accessed 27 Jun 2016).
- 20. Geurts JW, Willems PC, Lockwood C, et al. . Patient expectations for management of chronic non-cancer pain: a systematic review. Health Expect 2016 10.1111/hex.12527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Turk DC, Wilson HD, Cahana A. Treatment of chronic non-cancer pain. Lancet 2011;377:2226–35. 10.1016/S0140-6736(11)60402-9 [DOI] [PubMed] [Google Scholar]
- 22. Upshur CC, Luckmann RS, Savageau JA. Primary care provider concerns about management of chronic pain in community clinic populations. J Gen Intern Med 2006;21:652–5. 10.1111/j.1525-1497.2006.00412.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stannard C, Johnson M. Chronic pain management--can we do better? an interview-based survey in primary care. Curr Med Res Opin 2003;19:703–6. 10.1185/030079903125002478 [DOI] [PubMed] [Google Scholar]
- 24. Ponte CD, Johnson-Tribino J. Attitudes and knowledge about pain: an assessment of West Virginia family physicians. Fam Med 2005;37:477–80. [PubMed] [Google Scholar]
- 25. Briggs EV, Battelli D, Gordon D, et al. . Current pain education within undergraduate medical studies across Europe: Advancing the Provision of Pain Education and Learning (APPEAL) study. BMJ Open 2015;5:e006984.:e006984. 10.1136/bmjopen-2014-006984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mezei L, Murinson BB. Johns Hopkins Pain Curriculum Development Team. Pain education in North American medical schools. J Pain 2011;12:1199–208. [DOI] [PubMed] [Google Scholar]
- 27. Baird B, Charles A, Honeyman M, et al. . Understanding pressures in general practice. The King's Fund, 2016. https://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/Understanding-GP-pressures-Kings-Fund-May-2016.pdf (assessed 14 Jan 2016). [Google Scholar]
- 28. Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ 1995;152:1423–33. [PMC free article] [PubMed] [Google Scholar]
- 29. May C, Allison G, Chapple A, et al. . Framing the doctor-patient relationship in chronic illness: a comparative study of general practitioners' accounts. Sociol Health Illn 2004;26:135–58. 10.1111/j.1467-9566.2004.00384.x [DOI] [PubMed] [Google Scholar]
- 30. Kenny DT. Constructions of chronic pain in doctor-patient relationships: bridging the communication chasm. Patient Educ Couns 2004;52:297–305. 10.1016/S0738-3991(03)00105-8 [DOI] [PubMed] [Google Scholar]
- 31. Price C, Hoggart B, Olukog O, et al. . National Pain Audit Final Report 2010-2012. London UK: The British Pain Society, 2012. [Google Scholar]
- 32. Lynch ME, Campbell F, Clark AJ, et al. . A systematic review of the effect of waiting for treatment for chronic pain. Pain 2008;136:97–116. 10.1016/j.pain.2007.06.018 [DOI] [PubMed] [Google Scholar]
- 33. International Association for the Study of Pain Task Force on Wait-Times. Recommendations for wait-times. http://www.iasp-pain.org/files/Content/NavigationMenu/EducationalResources/IASP_Wait_Times.pdf (assessed 01 Jan 2017).
- 34. Faculty of Pain Medicine of the Royal College of Anaesthetics. Core standards for pain management in the UK. http://www.rcoa.ac.uk/system/files/FPM-CSPMS-UK2015.pdf (assessed 01 Jan 2017).
- 35. Hadi MA, Alldred DP. Promoting the role of pharmacists in chronic pain management: how can we make an impact on policy and practice? Int J Pharm Pract 2015;23:165–6. 10.1111/ijpp.12181 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-016454supp001.pdf (22.2KB, pdf)