Abstract
Background
Despite the clinical recommendation of exercise and diet for people with knee osteoarthritis (OA), there are no systematic reviews synthesising the effectiveness of combining physical activity and dietary restriction interventions on the musculoskeletal function of overweight and obese older adults with knee OA.
Objective
To evaluate the effectiveness of combined physical activity and dietary restriction programmes on body weight, body mass index (BMI) and the musculoskeletal function of overweight and obese older adults with knee OA.
Information sources
A detailed search strategy was applied to key electronic databases (Ovid, Embase, Web of Science andCumulative Index to Nursing and Allied Health Literature (CINAHL)) for randomised controlled trials (RCTs) published in English prior to 15 January 2017.
Participants
Participants with BMI ≥25 kg/m2, aged ≥55 years of age and with radiographic evidence of knee OA.
Interventions
Physical activity plus dietary restriction programmes with usual care or exercise as the comparators.
Outcome measures
Primary outcome measures were body weight, BMI or musculoskeletal function. Secondary outcome measures were pain and quality of life.
Results
One pilot and two definitive trials with n=794 participants were included. Two articles reporting additional data and outcome measures for one of the RCTs were identified. All included RCTs had an unclear risk of bias. Meta-analysis was only possible to evaluate mobility (6 min walk test) at 6 months and the pooled random effect 15.05 (95% CI −11.77 to 41.87) across two trials with n=155 participants did not support the combined intervention programme. Narrative synthesis showed clear differences in favour of a reduced body weight and an increased 6 min walk in the intervention group compared with control groups.
Conclusion
The quality of evidence of benefit of combining exercise and dietary interventions in older overweight/obese adults with knee OA is unclear.
Trail registration number
CRD42015019088 and ISRCTN, ISRCTN12906938.
Keywords: Exercise, diet, elderly, obesity, randomised controlled trials
Strengths and limitations of this study.
This is the first systematic review of combined physical activity and dietary restriction interventions in overweight and obese older adults with knee osteoarthritis.
The protocol of this review was registered in PROSPERO and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and the Cochrane handbook; Grading of Recommendation, Assessment, Development and Evaluation was used to evaluate the quality of the included trials.
The review included a mixed method analytical approach.
Few eligible studies were identified; however, important information is highlighted which could inform clinical practice.
Introduction
Rationale
Current evidence shows that the burden of chronic musculoskeletal conditions especially osteoarthritis (OA) increases with advancing age.1 OA is the most common type of arthritis affecting older adults. It is a degenerative joint disease that may affect any joint within the body causing chronic pain, functional limitation and emotional disturbance and may lead to disability and negatively affect quality of life (QOL).2–5 Knee OA is a common condition in older adults affecting about 3.64% of the global population in 2010.6 7 In the UK, there is approximately 4.7 million older adults aged 45 years or over experiencing knee OA symptoms.1 8 In addition, more than 20 million people seek treatment for knee OA in the USA.9 10 Given the increasing numbers of older adults in the population, combined with the increasing prevalence of obesity and being overweight throughout the population, it is anticipated that the incidence of knee OA will increase rapidly over the next decade.8
Unfortunately, there is no specific treatment for knee OA. Most recommendations describe three treatment modalities: non-pharmacological, pharmacological and surgical.11 12 Most knee OA evidence-based guidelines recommend non-surgical treatment13 14 and most general practitioners prefer the non-pharmacological and non-surgical interventions as the first line of treatment (recognised as ‘usual care’).11 These interventions are focused on patient education, self-management, pain reduction, function and QOL improvement, body weight reduction and exercise (either land-based or water-based).1 14–17 It is well known that obesity is an important risk factor for knee OA progression and several studies recommend obesity control for decreasing disease burden, since a decrease in body weight will lead to a reduction of joint load and inflammation.3 14 17 18 Weight reduction could be considered as a functional treatment in knee OA rehabilitation since a 12%–15% reduction compared with initial body weight has been shown to improve function and reduce pain.19 Moreover, the appropriate percentage of body weight reduction has been investigated in a systematic review and meta-analysis of five randomised controlled trials (RCTs).20 The review concluded that professional treatment of knee OA should include a weight reduction plan and patients should be encouraged to lose at least 5% of body weight over a 20-week period to achieve symptomatic relief.20
In addition to weight reduction, clinical guidelines for knee OA management and level 1 evidence recommend exercise therapy as the main intervention.20–24 Moderate intensity aerobic exercise (eg, walking) is recommended to maintain musculoskeletal function and reduce pain.20–22 However, the optimal exercise prescription for older adults is still unclear and further research is required.7 The demand for optimal exercise is increased in patients with obesity who may face more challenges and believe in the greater importance of physical activity compared with dietary intervention.25 26
Clinically combining a weight loss programme with exercise therapy may help overweight and obese older adults with knee OA to achieve a 10% loss of total body weight as well as safely relieve knee OA symptoms.3 Also, a recent RCT which included older adults has shown that a non-surgical treatment programme had longer-lasting beneficial effects, evidenced by a delayed requirement for elective total knee replacement (TKR) surgery in a secondary healthcare setting.27 Moreover, for those who are eligible for unilateral TKR, non-surgical intervention may delay their surgical intervention for several months.28 There are no systematic literature reviews synthesising the evidence of the effectiveness of combining physical activity and dietary restriction interventions on the musculoskeletal function of overweight and obese older adults with knee OA.
The aim of this review was to evaluate the effectiveness of combined physical activity and dietary restriction programmes on the musculoskeletal function of overweight and obese older adults with body mass index (BMI) ≥25 kg/m2, aged ≥55 years of age and with radiographic evidence of knee OA.
Objective
To evaluate the effectiveness of combined physical activity and dietary restriction programmes on body weight, BMI and the musculoskeletal function of overweight and obese older adults with knee OA.
Methods
Protocol and registration
A systematic review was conducted according to a predefined protocol following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)-P guidelines29 and the Cochrane handbook.30 The review was registered on PROSPERO on 01 April 2015 (CRD42015019088), and is reported in accordance with the PRISMA statement (see online supplementary data).29
bmjopen-2016-014537supp001.pdf (197.3KB, pdf)
Eligibility criteria
Inclusion criteria
Exclusion criteria
Full article not written in English.
Studies
Randomised controlled trials.
Interventions
Combined physical activity and dietary restriction programmes.
Comparators
Usual care (including advice or physical activity alone or dietary restriction alone) or exercise (participants received an exercise programme similar to the intervention group).
Outcome measures
Primary outcome measures: body weight, BMI, musculoskeletal function either self-reported function or objective functional performance measures, also, including mobility, joint range of motion (ROM) and muscle strength.
Secondary outcome measures: pain and QOL.
Information sources
The search employed sensitive, topic-based strategies designed for each database (to 10 December 2015):
The Cochrane Library: Controlled Trials Register, NHS Economic Evaluation Database.
Cumulative Index to Nursing and Allied Health Literature (CINAHL), Embase, Medline, Web of Science.
Hand searches in key journals and lists of references.
Unpublished research and grey literature such as Open Grey.
Government, official, organisational such as UK Department of Health, WHO and National Health Service (UK).
Clinical trials registration, theses abstracts and Google scholar.
Search
Search strategies of predefined search terms were developed and tested for applicability (ASA, and a specialist librarian from the University of Birmingham on 13 February 2015). The definitive search strategy was run by two independent researchers (ASA/AMK, 10 December 2015). Endnote X7 software was used for data management. Search results were imported and duplicates were removed. An example of the Medline Ovid search strategy is presented in table 1. The search was updated on 15 January 2017 to include studies published in 2016 by ASA/AMK and no eligible studies were identified.
Table 1.
Example of Medline Ovid search strategy 1948 to 10 December 2015
| # | Searches |
| 1 | Physical activity/ |
| 2 | Physical* adj2 (activity or training or therapy*) |
| 3 | (Exercis* or rehabilitation* or treatment*) |
| 4 | (Closed kinetic chain* or open kinetic chain* or isokinetic* or isometric* or anaerobic* or muscle* or stretching* or aerobic* or isotonic* or treadmill*or endurance* or walking*) adj1 (exercise*) |
| 5 | (Resist* adj2 (exercise* or therapy or training)) |
| 6 | 1 or 2 or 3 or 4 or 5 |
| 7 | Dietary restriction. mp. |
| 8 | Meal replacement.mp. |
| 9 | Weight loss/ or weight loss.mp. or intentional weight loss.mp. |
| 10 | Caloric Restriction/ or Obesity/ or Body Weight/ or hypo or hypocloric diet/ |
| 11 | Energy intake/ or adipos*/ or Body Mass Index/ or Overweight/ |
| 12 | Diet/ or Diet, Carbohydrate-Restricted/ or Diet, Reducing/ or Diet Therapy/ or Diet, Vegetarian/ |
| 13 | Obesity/ or obesity.mp. |
| 14 | ((Low carbohydrate* or low calor* or low fat* or vegetarian*) adj1 (diet*)) |
| 15 | (Diet adj2 (therapy* or treatment*)) |
| 16 | 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 |
| 17 | Aging/ |
| 18 | Exp aged/ |
| 19 | (55 adj2 (year* or age* or old*)) |
| 20 | (old* adj (adult* or people or person* or population* or men or women)) |
| 21 | (aging* adj (adult* or people or person* or population*or men or women)) |
| 22 | (elder* or senior* or geriatric* ?enarian or ageing) |
| 23 | (age* or aging or old* or elder*) adj1 (musc*)) |
| 24 | 17 or 18 or 19 or 20 or 21 or 22 or 23 |
| 25 | Pain/ or Knee Joint/ or Knee pain.mp. or Osteoarthritis, knee/ |
| 26 | Knee osteoarthritis.mp. or Osteoarthritis, knee/ |
| 27 | (Knee* adj (arthritis or osteoarthritis* or inflammation* or degeneration* or disease or pain*)) |
| 28 | (radiographic* or symptomatic* or clinical* adj1 (knee osteoarthritis*)) |
| 29 | 25 or 26 or 27 or 28 |
| 30 | Musculoskeletal function. mp. |
| 31 | Muscle function. mp. |
| 32 | Body composition/ |
| 33 | Mobility.mp. |
| 34 | (Gait or walking) adj1 (speed) |
| 35 | Functional ability.mp. |
| 36 | ‘Activity of daily’ living/ or. mp. |
| 37 | ‘Quality of life’/ |
| 38 | Balance.mp. |
| 39 | (musculoskeletal adj2(pain or disorder*)) |
| 40 | (Musc* adj (power or strength or performance or function or weakness)) |
| 41 | 41. 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 |
| 42 | 6 and 16 and 24 and 29 and 41 |
Study selection
The eligibility of included studies was independently assessed by two reviewers (ASA/AMK) according to the eligibility criteria. The reviewers screened the results of the search by titles and abstracts, and then full text. A study was considered to be eligible when both reviewers assessed the full text independently and found it to fulfil the eligibility criteria. A third reviewer (CAG) mediated in the case of disagreement. The inter-rater agreement was evaluated using Cohen’s Kappa measure.32
Data collection
Using a standardised form (developed by ASA) based on the Cochrane Consumers and Communication Review Group’s data extraction template,33 two reviewers (ASA/AMK) extracted data independently. A third reviewer (CAG) checked for consistency and clarity.
Data items
Items reported on the data extraction form for each trial included demographic information, methodology, intervention details and all specified reported outcomes.
Risk of bias in individual trials
The internal validity of each included trial was assessed using the Cochrane risk of bias assessment tool34 recommended by PRISMA.29 All domains of the risk of bias tool were assessed independently by two reviewers (ASA/CAG). A third reviewer (ABR) mediated in the case of disagreement.
Risk of bias across trials
Risk of bias was considered high if the proportion of information from trials with high risk of bias was sufficient to affect the interpretation of the results. Risk of bias was considered unclear if most information was from studies with a low or unclear risk of bias, and low if most information was from studies with a low risk of bias.34
Summary measures
Following data extraction, meta-analysis was possible for one key outcome measure across trials that applied similar interventions and compared with exercise at one assessment time-point (6 months). Meta-analysis was conducted using RevMan to assess the effectiveness of a combined intervention programme of diet and exercise on mobility (6 min walk test at 6 months) using the random effects model.35 36 Ninety-five per cent Cls were reported for the summary statistics and the SD was calculated from the SEs and CIs.37 38 Data for the other outcomes were available, but meta-analyses were not possible due to different assessment points or comparators. A modified narrative synthesis was used to present these data.39 40
Synthesis of results
A mixed method analysis was required to synthesise the available data.35–40 For the meta-analysis, no raw data were available, and therefore data analyses were conducted on the final summary statistics reports. SDs were estimated from reported SE and CI for all available data.36 Heterogeneity in treatment effects was considered by computation of I2. An analysis of the quality of the interventions was undertaken as the basis for interpretation of heterogeneity.36 37 For the modified narrative synthesis, change scores were used for trials when no other data were available.36–38 Two stages of a narrative synthesis were possible to apply; these comprised the development of a preliminary synthesis of findings of included trials, and an exploration of the relationships within and between trials.39 40
Developing a preliminary synthesis
A preliminary synthesis was developed using tabulation, textual description, grouping and clusters and data transformation. Tables were designed presenting the main characteristics of the eligible studies including eligibility criteria, intervention (number of participants, goal of weight loss, intervention period, setting and brief information about exercise and diet intervention), comparator, outcome measures and the main findings. Additional tables were used to organise studies with respect to specific outcome measures (primary or secondary) and the comparator group. Results were presented as mean (SD) by converting the continuous data from SEs or CIs to SD.39 40
Exploring the relationships within and between trials
A visual representation of the relationship between study characteristics and results was used to explore the relationships within and between trials.39 40
Additional analyses
The Grading of Recommendation, Assessment, Development and Evaluation (GRADE) approach was used to evaluate the quality of evidence included in the meta-analysis.41 42 Specific software (GRADEpro) was used.43 This approach provided a system for rating the quality of evidence and determining the strength of recommendations for clinical practice guidelines.41 42 It has five components: risk of bias, inconsistency, indirectness, imprecision and publication bias. Quality of evidence was categorised as ‘high’, ‘moderate’, ‘low’ and ‘very low’.41 42 Each RCT evaluated as ‘high’ quality evidence was modified according to five negative and two positive factors.41 42
The Cochrane risk of bias assessment tool was used for this component.34 According to the software, risk of bias was classified as not serious, serious or very serious. The quality of evidence was downgraded by one level if there was a serious limitation or by two levels if the limitation was very serious.41 42 Inconsistency was evaluated according to I² statistics. It may be considered low if I²<40%, moderate if I²=30%–60%, substantial if I²=50%–90% and considerable if I²=75%–100%.42 Inconsistency was considered as unserious if the reviewers were able to identify a plausible explanation for the heterogeneity and the quality of evidence was not downgraded.42 Otherwise, the quality of evidence was downgraded by one or two levels if inconsistency of the results was classified as serious or very serious.42 The quality of evidence was downgraded by one or two levels if there was indirectness between the study question and the applicability of the evidence.41
Imprecision of evidence was downgraded in the presence of the following conditions: first, when the boundaries of the CI crossed the no effect line (threshold is completely within the recommended effect) and second, when the criteria for optimal information size (OIS) were not met.42 The criterion for OIS was that the total number of participants included in a systematic review (calculated from a meta-analysis) was less than the number of participants generated by a conventional sample size calculation for a single adequately powered trial. Imprecision was downgraded by one level if one of these conditions was not met or by two levels if both conditions were not met.41 42
Publication of bias was undetectable or strongly suspected according to GRADE software.43 The selective outcome reporting domain of the Cochrane risk of bias assessment tool was used to evaluate the publication bias.34 42 The quality of evidence was downgraded by one level if the selective outcome reporting domain was evaluated as unclear without justification or downgraded by two levels if evaluated as high.42
Results
Study selection
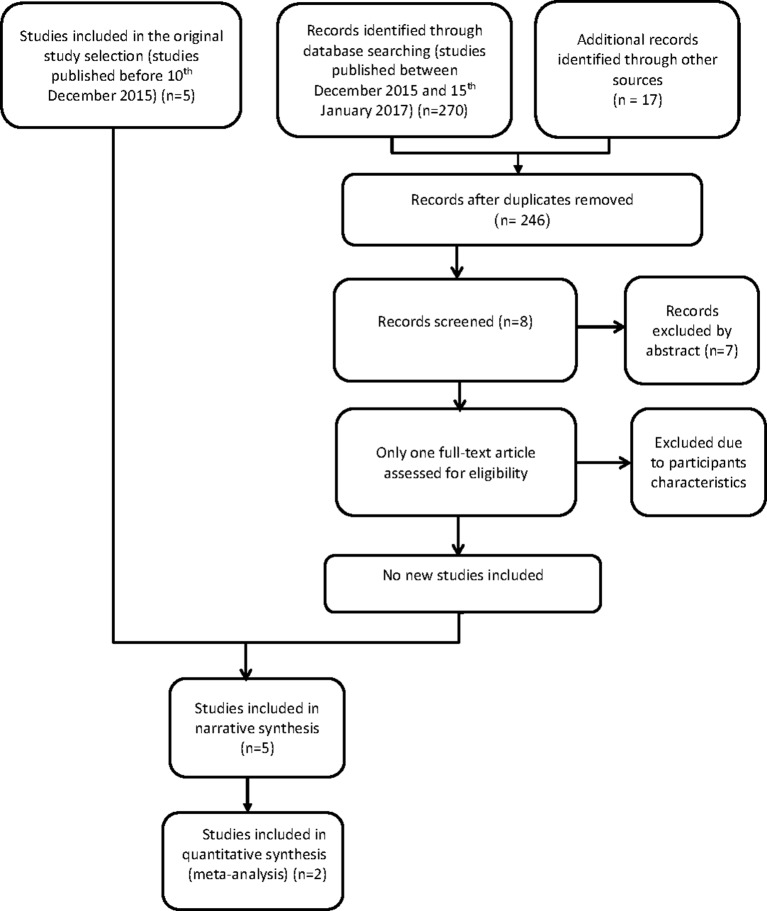
Three RCTs (n=794) were included. One was a pilot trial44 and two were definitive trials: the Arthritis, Diet and Activity Promotion Trial (ADAPT)45 and the Intensive Diet and Exercise for Arthritis (IDEA).3 For the ADAPT, there was a main trial report, and two additional articles with further analyses of additional outcome measures.46 47 The trials used two comparators: an exercise programme in the pilot study and IDEA trial,3 44 while usual care (healthy lifestyle) was the comparator in ADAPT.45 All of the included trials were conducted by the same group from the USA and published in English. No relevant unpublished studies were identified. The inter-rater agreement of the study selection process was excellent with k=0.82.32 There was one disagreement requiring consultation with the third reviewer (CAG), who was asked to clarify the eligibility of articles reporting the same trials. Specifically, one pilot study by Messier et al 44 44 did not clarify whether it was an external or internal pilot study. The senior author was contacted twice but no response was received. The third reviewer recommended it be treated as an external pilot study as there was nothing to indicate it was an internal pilot study in the article reporting the main trial.45 The study flow diagram is presented in figure 1.48
Figure 1.
Study selection flow diagram.48
Study characteristics
The main characteristics of the included trials are presented in table 2.
Table 2.
Descriptive data for the included trials
| Title/author/ year | Aim | Eligibility criteria | Methods | Comparator | Outcome measures | Assessment points | Result |
| Exercise and weight loss in obese older adults with knee OA: a preliminary study. Messier et al (2000)44 |
1) To determine if a combined dietary and exercise intervention results in significant weight loss in older obese adults with knee OA 2) To compare the effects of exercise plus dietary therapy with exercise alone on gait, strength, knee pain, biomarkers of cartilage degradation and physical function |
Inclusion Aged ≥60 years BMI ≥28 kg/m² Knee pain, radiographic evidence of knee OA Self-reported physical disability Exclusion Serious medical condition affecting safety Planned change of abode or admission to a nursing home within next 6 months. Unable to walk at least 420 ft in 6 min without assistive device Unable to walk on treadmill without assistive device Current participation in an exercise programme or other study Unable to participate or complete the study protocol |
Participants n=24 community-dwelling obese older adults Goal of weight loss 15 lb (6.8 kg) Period of intervention 6 months Setting University Health and Exercise Science Centre, USA Exercise Combined weight training and walking programme for 1 hour three times per week Dietary intervention Nutrition class 1 hour/week to instruct participants how to modify caloric intake using cognitive behaviour modification to change dietary habits to reach a group goal of an average weight loss then three group and one individual session held per month |
Exercise group (control) | Body weight, self-report questionnaire, physical performance and gait analysis Synovial fluid biomarkers (total proteoglycan (PG), keratan sulfate (KS) and interleukin-1β (IL-1β)) Frequency and intensity of knee pain (Likert scale) Disability by self-reported physical function using the Fitness Arthritis and Seniors Trial 6 min walk test and timed stair climbing to measure physical performance Kinetics and kinematics analysis of gait using motion analysis and force plate recorded at 3 and 6 months |
Data recorded at baseline, 3 and 6 months | Body weight reduced significantly in diet plus exercise group compared with exercise group with (p=0.007) Within group differences: The combined intervention group lost a mean of 18.8 lb (8.5 kg) at 6 months compared with 4.0 lb (1.8 kg) in the exercise group (p=0.01) No statistical differences were found between groups in self-reported performance measures of physical function and knee strength Statistically significant improvement in both groups in self-reported disability and knee pain intensity and frequency and physical performance At 6 months, the combined intervention group had a significantly greater loading rate (p=0.03) and maximum braking force (p=0.01) during gait No statistical differences were found between groups in knee pain scores Concentration level of KS decreased similarly in both groups The decrease in IL-1 correlated with joint pain (r=−0.77, p=0.043) |
| Exercise and dietary weight loss in overweight and obese older adults with knee OA Messier et al (2004)45 |
1) To determine whether long-term exercise and dietary weight loss are more effective, either separately or in combination, than usual care in improving physical function, pain and mobility in older overweight and obese adults with knee OA | Inclusion Aged ≥60 years BMI ≥28 kg/m² Knee pain, radiographic evidence of knee OA Self-reported physical disability Exclusion Serious medical problem Mini-Mental State Examination score of <24.3 Inability to finish 18 months study Inability to walk without assistive device Participation in another study 6-Reported alcohol consumption >14 drinks per week ST segment depression of at least 2 mm at an exercise level of 4 metabolic equivalent tasks (METS) or less, hypotension or complex arrhythmia during exercise Inability to complete the study protocol due to frailty, illness or other reason |
Participants n=316 community-dwelling obese older adults Goal of weight loss 5% of the total body weight over 18 months Period of intervention 18 months Setting The Claude D Pepper Older Americans Independence Centre, Wake Forest University, USA Exercise 1 hour 3 days/week consisted of an aerobic phase a resistance-training phase, a second aerobic phase and a cool-down phase Dietary intervention Based on principles from the group dynamics literature and social cognitive theory; divided into three phases: intensive (months 1–4), transition (months 5–6) and maintenance (months 7–18) Dietary weight loss plus exercise Combined the exercise and dietary weight loss programmes |
Usual care healthy lifestyle (control) Exercise group Dietary weight loss group |
Primary outcome Self-reported physical function using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Secondary outcomes Weight loss, 6 min walk distance, stair-climb time, WOMAC pain and stiffness scores and joint space width |
Data recorded at baseline, 6 and 18 months | Significant body weight loss in diet groups (p<0.05). Diet plus exercise and diet group lost an average of 5.7% and 4.9% of their body weight, respectively with 1.2% for the healthy lifestyle group Significant improvements in self- reported physical function (p<0.05), 6 min walk distance (p<0.05), stair-climb time (p<0.05) and knee pain (p<0.05) in the diet plus exercise group compared with the healthy lifestyle group Significant improvement in the 6 min walk distance in the exercise group (p<0.05) The diet-only group was not significantly different from the healthy lifestyle group with respect to any of the functional or mobility measures Changes in joint space width were not significantly different between groups |
| Effects of intensive diet and exercise on knee joint loads, inflammation and clinical outcomes among overweight and obese adults with knee OA is the Intensive Diet and Exercise for Arthritis randomised clinical trial Messier et al (2013)3 |
To determine whether a 10% reduction in body weight induced by diet, with or without exercise, would improve mechanistic and clinical outcomes more than exercise alone | Inclusion Aged ≥55 years Kellgren-Lawrence 14 grade 2 or 3 (mild or moderate) radiographic tibiofemoral OA or tibiofemoral plus patellofemoral OA of one or both knees, pain on most days due to knee OA. BMI from 27 to 41 Sedentary lifestyle (<30 min per week of formal exercise for the past 6 months) Participants usual medications could be maintained or adjusted depending on physician advice Exclusion Significant comorbid disease that would pose a safety threat or impair ability to participate, previous acute knee injury, patellofemoral OA in the absence of tibiofemoral OA Ability and willingness to modify dietary or exercise behaviours Excess alcohol use Inability to finish 18-month study or unlikely to be compliant Conditions that prohibit knee MRI Significant cognitive impairment or depression |
Participants n=454 Goal of weight loss 10%–15% of the total body weight Period of intervention 18 months Setting Wake Forest University and Wake Forest School of Medicine, USA Intensive weight loss intervention The diet included up to two meal-replacement shakes per day For the third meal, participants followed a weekly menu plan and recipes that were 500–750 kcal, low in fat and high in vegetables. Daily caloric intake was adjusted according to the rate of weight change between intervention visits. The initial diet plan provided an energy-intake deficit of 800– 1000 kcal/day as predicted by energy expenditure (estimated resting metabolism×1.2 activity factor) The exercise intervention It was conducted for 1 hour on 3 days/week for 18 months Participation was centre-based for the first 6 months After 6-month follow-up testing and a 2-week transition phase, participants could remain in the facility programme, opt for a home-based programme or combine that two. The programme consisted of aerobic walking (15 min), strength training (20 min), a second aerobic phase (15 min) and cool-down (10 min) |
Exercise group (control group) Dietary weight loss group |
Primary outcomes knee joint compressive force and plasma IL-6 concentration Secondary clinical outcomes Self-reported pain (range 0–20), function (range 0–68), mobility and health-related quality of life |
Participants were assessed at baseline, 6 and 18 months | Body weight was reduced significantly in both diet groups (diet and diet plus exercise) more than exercise group (p<0.001) Within group differences: the diet plus exercise group lost about 10.6 kg (11.4%), the diet group lost 8.9 kg (9.5%) and 1.8 kg (2.0%) of base line body weight No significant difference in walking speed and 6 min walk test between groups Significant pain reduction was observed in the diet plus exercise group at 18 months compared with exercise group (mean score, 1.02; 95% CI 0.33 to 1.71; p=0.004) The difference in the SF-36 (36-item short form survey) physical subscale was 2.81 units in diet plus exercise relative to exercise group (95% CI −4.76 to −0.86; p=0.005) No significant difference in the mental subscale between groups |
QA,osteoarthritis.
Methods
In the pilot trial by Messier et al,44 participants were randomised into two groups, a combined intervention and control group.44 The control group received an exercise programme similar to the intervention group. Messier et al 45 randomised participants into four groups: combined intervention, exercise, diet and a control group. The control group received health education plus telephone contact to obtain information on pain, medication use, illness and hospitalisation.45 Messier et al 3 randomised participants into three groups: combined intervention, diet group and exercise group. The exercise-alone group was the control. Duration of the trial was 6 months for the pilot trial44 and 18 months for ADAPT45 and IDEA.3
Participants
All participants were community dwelling, obese older adults with radiographic evidence of knee OA. A total of 794 participants aged 55 years or older were randomised into the included studies. One hundred and fifty-five participants were included in the meta-analysis.
Interventions
The pilot trial44 and two definitive trials3 45 were conducted by the same group from Wake Forest University, Winston-Salem, North Carolina, USA. The goal of weight loss varied from 6.8 kg over 6 months to 10%–15% of total body weight over 18 months of intervention. Outcomes were recorded at three time-points for the pilot trial (baseline, 3 months and 6 months) and for the two definitive trials (baseline, 6 months and 18 months). Exercise duration and frequency were similar in all included trials (1 hour/three times per week). Exercise types were aerobic exercise and resistance training. Principles from group dynamics and social-cognitive theory were used for behavioural treatment in the diet group in IDEA.3 The diet sessions were graded from intensive (facilitating behavioural changes by using self-regulatory skills) to transition stage (assisting participants who not reached their weight loss goals in establishing new goals) and maintenance stage (assisting patients who had reached their weight loss goals to maintenance of their weight loss). For the intensive weight loss trial, the daily caloric intake was adjusted according to the rate of weight change between intervention visits (low fat and high vegetable diet). The initial diet plan provided an energy-intake deficit of 800–1000 kcal/day, as predicted by an energy expenditure (estimated resting metabolism×1.2 activity factor), of at least 1200 kcal for men and 1100 kcal for women.3
Outcome measures
Due to few eligible studies, analysis was based on all of the outcomes of interest (body weight and BMI as well as musculoskeletal function), irrespective of whether they were specified as the primary or secondary outcome in the included trials (see below):
Messier et al 44: no primary or secondary outcomes were specified.
Messier et al 45: the ADAPT primary outcome was self-reported physical function measured using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Secondary outcomes included weight loss, 6 min walk distance, stair-climb time, WOMAC pain and stiffness scores and joint space width.45
Messier et al 3: in the IDEA trial, the primary outcomes were knee joint compressive force and plasma interleukin (IL)-6 concentration. Secondary outcome measures included WOMAC pain, WOMAC function, gait speed, 6 min walk test, QOL, body weight, height, BMI and body composition.3
Risk of bias within trials
Substantial inter-reviewer agreement was achieved on the risk of bias assessment (k=0.73).32 All of the included trials were evaluated as unclear risk of bias.34 Most of the key domains were assessed as unclear risk of bias within each trial (table 3).
Table 3.
Summary assessment of the overall risk of bias for each trial
| Study (author, year) |
Component of risk of bias | Summary risk of bias | |||||
| 1 | 2 | 3 | 4 | 5 | 6 | ||
| Messier et al, 200044 | U | U | U | U | L | U | Unclear (5) Low (1) |
| Rejeski et al, 200246 | U | U | U | L | L | U | Unclear (4) Low (2) |
| Messier et al, 200445 | L | U | U | L | L | U | Unclear (3) Low (3) |
| Focht et al, 200547 | U | U | U | L | L | U | Unclear (4) Low (2) |
| Messier et al, 20133 | L | U | U | L | L | U | Unclear (3) Low (3) |
Risk of bias across trials
Risk of bias across trials was evaluated as unclear,34 only component 5 (selective outcome reporting) was evaluated as low risk of bias for all studies. For the ‘blinding of participants, personnel and outcome assessor’ component, all trials were evaluated as having unclear risk of bias as no strategies were reported to address the issue of outcome assessor unblinding. Also, for the ‘other sources of bias’ components, all trials were evaluated with unclear risk of bias due to unclear reporting.
Results of individual trials and synthesis of results
Quantitative synthesis
Meta-analysis was possible for only one outcome measure at one assessment time-point. Meta-analysis was used to assess the effect of the combined intervention programme compared with exercise on the 6 min walk test (metres) after 6 months of intervention. Only two trials3 44 with unclear risk of bias with n=155 participants were available for meta-analysis. The pooled random effects (15.05, 95% CI −11.77 to 41.87) did not support a combined intervention effect (figure 2).
Figure 2.
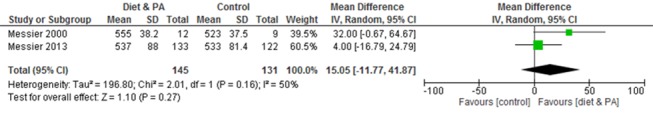
6 min walk test (metres) at 6 months.
Synthesis of results
Modified narrative synthesis
With respect to the guidelines for a narrative synthesis, only two elements were possible to apply: developing a preliminary synthesis and exploring the relationships within and between studies.39 40
Developing a preliminary synthesis
Tabulation was used to present primary and secondary outcome measures that were not included in the meta-analysis: body weight, knee ROM, physical function, mobility, pain and QOL. Studies including a comparison of the combined intervention programme with an exercise intervention are presented in tables 4-5.
Table 4.
Preliminary synthesis for the primary outcome measures at baseline and after intervention: body weight, knee ROM, physical function and mobility comparing the combined intervention programme with an exercise intervention
| Category | Outcome measure | Assessment point(months) | Study | Intervention group | Control group | ||||||
| M0 (SD0) |
N0 | M1 (SD1) |
N1 | M0 (SD0) |
N0 | M1 (SD1) |
N1 | ||||
| Body weight | Body weight (kg) | 6 | Messier et al, 200044 | 91 (13) | 13 | 82.5 (4) | 12 | 109 (17) | 11 | 107.2 (15) | 9 |
| 6 | Messier et al, 20133 | 93 (14.7) | 152 | 84.3 (14.7) | 133 | 92.3 (14.6) | 150 | 92.4 (15.4) | 122 | ||
| 18 | Messier et al, 20133 | 93 (14.7) | 152 | 82.4 (15.2) | 121 | 92.3 (14.6) | 150 | 90.5 (15) | 115 | ||
| Knee ROM | ROM | 6 | Messier et al, 200044 | 55.27* (N/A) | 13 | 56.47 (0.91) | 12 | 55.27* (N/A) | 11 | 56.73 (1.02) | 9 |
| Estimated concentric extension (degree) | 6 | Messier et al, 200044 | 30.7 (N/A) | 13 | 31 (N/A) | 12 | 30.7 (N/A) | 11 | 33.4 (N/A) | 9 | |
| Estimated concentric flexion | 6 | Messier et al, 200044 | 18.2 (N/A) | 13 | 18.5 (N/A) | 12 | 18.2 (N/A) | 11 | 20.8 (N/A) | 9 | |
| Physical function | Physical function (WOMAC) | 18 | Messier et al, 20133 | 24.6 (11.7) | 152 | 14.2 (10.4) | 121 | 23.1 (10.3) | 150 | 17.6 (9.8) | 115 |
| Mobility | 6 min walk test (m) |
18 | Messier et al, 20133 | 467 (87.9) | 152 | 537 (92.6) | 121 | 480 (90.3) | 150 | 525 (79.2) | 115 |
| Stair climb (s) |
6 | Messier et al, 200044 | 9.81* | 13 | 7.4 (0.32) | 12 | 9.81* | 11 | 8.7 (0.36) | 9 | |
M0 (SD0), mean and SD at baseline; N0, participants number at baseline; M1 (SD1), mean and SD after intervention; N1; participants number after intervention; N/A, data not available.
Table 5.
Preliminary synthesis for the secondary outcome measures at baseline and after intervention: body weight, pain and QOL comparing the combined intervention programme with an exercise intervention
| Category | Assessment point(months) | Outcome measure | Study | Intervention group | Control group | ||||||
| M0 (SD0) | N0 | M1 (SD1) | N1 | M0 (SD0) | N0 | M1 (SD1) | N1 | ||||
| Pain | WOMAC pain | 6 | Messier et al, 20133 | 6.7 (3.4) | 152 | 4.6 (2.9) | 133 | 6.1 (2.9) | 150 | 4.5 (3) | 122 |
| WOMAC pain | 18 | Messier et al, 20133 | 6.7 (3.4) | 152 | 3.7 (3.1) | 121 | 6.1 (2.9) | 150 | 4.4 (2.7) | 115 | |
| QOL | SF-36 physical component | 6 | Messier et al, 20133 | 36.6 (9.41) | 152 | 43.5 (9) | 133 | 36.8 (9) | 150 | 41.5 (9) | 122 |
| SF-36 mental component | 6 | Messier et al, 20133 | 57.2 (6.6) | 152 | 56.9 (7.3) | 133 | 56.5 (8.4) | 150 | 56.1 (7.6) | 122 | |
| SF-36 physical component | 18 | Messier et al, 20133 | 36.6 (9.41) | 152 | 44.7 (8.7) | 121 | 36.8 (9) | 150 | 42.0 (9) | 115 | |
| SF-36 mental component | 18 | Messier et al, 20133 | 56.1 (6.5) | 152 | 57.2 (6.6) | 121 | 56.5 (8.4) | 150 | 55.4 (7.6) | 115 | |
M0 (SD0), mean and SD at baseline; N0, participants number at baseline; M1 (SD1), mean and SD after intervention; N1, participants number after intervention; N/A, data not available.
Tabulation was used to compare the effect of the combined intervention programme compared with usual care (healthy lifestyle) on primary and secondary outcome measures: body weight, physical function, mobility, pain and QOL (tables 6-7).
Table 6.
Preliminary synthesis for the primary outcome measures at baseline and after intervention: physical function and mobility comparing the combined intervention programme with usual care
| Category | Outcome measure | Assessment point (months) | Study | Intervention group | Control group | ||||||
| M0 (SD0) | N0 | M1 (SD1) | N1 | M0 (SD0) | N0 | M1 (SD1) | N1 | ||||
| Body weight | Body weight (kg) |
18 | Messier et al, 200445 | 92 (1.7) | 76 | 86.8 (N/A) | 58 | 96 (1.8) | 78 | 94.9 (N/A) | 67 |
| Physical function | Physical function (WOMAC) | 6 | Messier et al, 200445 | 23.6 (12.2) | 76 | 17.9* (N/A) | 63 | 26 (11.4) | 78 | 22.4* (N/A) | 70 |
| Physical function (WOMAC) | 18 | Messier et al, 200445 | 23.6 (12.2) | 76 | 29.3* (N/A) | 58 | 26 (11.4) | 78 | 29.4 (N/A) | 67 | |
| Mobility | 6 min walk test (m) |
6 | Messier et al, 200445 | 416.2 (98.7) | 76 | 482.3 (100) | 63 | 434.6 (96.4) | 78 | 429 (108) | 70 |
| 6 min walk test (m) |
18 | Messier et al, 200445 | 416.2 (98.7) | 76 | 477.8 (99.7) | 58 | 434.6 (96.4) | 78 | 429.9 (104.7) | 67 | |
| 6 min walk test (m) |
18 | Focht et al, 200547 | 414.5 (85.3) | N/A | 465 (96.3) | N/A | 433.4 (81.9) | N/A | 430 (79.5) | N/A | |
| Stair climb (s) |
6 | Messier et al, 200445 | 10.9 (5.8) | 76 | 8.8 (6.2) | 63 | 9.5 (5.6) | 78 | 9.9 (6.3) | 70 | |
| Stair climb (s) |
18 | Focht et al, 200547 | 10.4 (7.3) | N/A | 8.9 (5.4) | NA | 9.4 (4.9) | N/A | 9.9 (5.6) | N/A | |
*Estimated value from figure 2 in ref. 45.
M0 (SD0), mean and SD at baseline; N0, participants number at baseline; M1 (SD1), mean and SD after intervention; N1, participants number after intervention; N/A, data not available.
Table 7.
Preliminary synthesis for the secondary outcome measures at baseline and after intervention: body weight, pain and QOL comparing the combined intervention programme with usual care
| Category | Outcome measure | Assessment point (months) | Study | Intervention group | Control group | ||||||
| M0 (SD0) | N0 | M1 (SD1) | N1 | M0 (SD0) | N0 | M1 (SD1) | N1 | ||||
| Pain | Pain scale (WOMAC) | 6 | Messier et al, 200445 | 7.3 (3.6) | 76 | 5.5 (3.7) | 63 | 7.3 (3.4) | 78 | 6.2 (3.9) | 70 |
| Pain scale (WOMAC) | 18 | Messier et al, 200445 | 7.3 (3.6) | 76 | 5.1 (3.6) | 58 | 7.3 (3.4) | 78 | 6 (3.7) | 67 | |
| QOL | SF-36 physical component |
Average of 6 and 18 | Rejeski et al., 200246 | 35.39 (10.5) | 68 | 40.57 (N/A)* | N/A | 33.60 (8.4) | 68 | 40.57 (N/A)* | N/A |
| SF-36 mental component |
Average of 6 and 18 | Rejeski et al., 200246 | 52.85 (10.7) | 68 | 53.51 (N/A)* | N/A | 52.70 (10.9) | 68 | 53.31 (N/A)* | N/A | |
M0 (SD0), mean and SD at baseline; N0, participants number at baseline; M1 (SD1), mean and SD after intervention; N1, participants number after intervention; N/A, data not available, *, only SEM data available; SD1 data could not be calculated due to missing N1 value.
Exploring the relationships within and between studies
Characteristics of the trials are presented in table 2. All included trials were conducted by the same research group. The eligibility criteria were very similar across studies. The exercise intervention included strengthening and aerobic exercise. The intervention frequency (1 hour/three times per week) was the same across the included trials. Further details about the design of the trials are presented above.
Tables 4 and 6 show differences between the intervention group and the control group (despite the comparator) with respect to body weight and the 6 min walk distance. These differences were consistent with the results from the included trials. The diet plus exercise group in the pilot study44 lost weight compared with the control group (p=0.01) after 6 months of intervention44 and this was also the case with respect to the longer duration intervention trial (18 months) in which the intervention group lost significantly (p <0.001) more weight than the exercise group.3 However, in ADAPT45 both groups (intervention and healthy lifestyle) lost weight (p<0.05) after 18 months of intervention,45 although there was a significant difference in the 6 min walk result in favour of the diet plus exercise group (p<0.05).45 Also, there was a significant difference (p=0.005) in the 6 min walk between the intervention and exercise groups in the IDEA trial.3
Additional analysis
No further analyses were possible owing to the lack of reported information and low number of included trials.
Grading the quality of evidence
A summary assessment was undertaken to draw conclusions about the overall quality of evidence for the combined intervention on mobility using GRADE software.43 Both trials included in the meta-analysis3 44 were evaluated as ‘high’ quality evidence before being downgraded as they were RCTs, before being modified according to five negative and two positive factors.41 42 The quality of evidence for a combined intervention programme of physical activity and diet on walking distance (metres) within 6 min after a period of 6 months of intervention was evaluated as moderate (table 8).
Table 8.
Factors determining the quality of evidence according to GRADE
| Factor | Judgement | Explanation |
| 1. Risk of bias | Not serious |
|
| 2. Inconsistency | Not serious |
|
| 3. Indirectness | Not serious |
|
| 4. Imprecision | Serious |
|
| 5. Publication bias | Undetected |
|
Discussion
Summary of evidence
This is the first systematic review and mixed method analysis investigating the effectiveness of combining dietary restriction and physical activity interventions for musculoskeletal function in overweight/obese older adults with knee OA. One pilot trial44 and two definitive trials3 45 (794 participants) conducted by the same research group (Wake Forest University) were included. The intervention programme was compared with exercise training in one definitive trial (IDEA)3 and the pilot trial,44 while usual care was the comparator in the ADAPT.45 Two additional articles46 47 which reported further outcomes of the ADAPT were identified.45
Data syntheses of this review were conducted using both meta-analysis and modified narrative synthesis. Although visual inspection of the tables of results indicated that the combined programme enhanced body weight reduction, and improved mobility, there was moderate evidence for no effect. Changes of BMI scores were not reported in the included studies. Meta-analysis was possible for only the 6 min walk test at 6 months and was not possible for the other outcome measures due to the inconsistency of assessment points or the comparator. The pooled random effect of two trials3 44 with 155 participants did not support the combined intervention programme (15.05, 95% CI −11.77 to 41.87) (although with a total effect of 15 m deemed not clinically significant according to previous literature).49 50 Although the meta-analyses showed substantial heterogeneity I²=50%, this was classified as not serious using the GRADE evaluation tool41 42 as it was assessed as likely to be due to high variability in both the sample size and effect size. Clinical heterogeneity across trials was limited to comparator and duration. Overall, the quality of evidence was downgraded to moderate due to imprecision of the results according to GRADE.43 All included trials were reported as having an unclear risk of bias, which was mainly due to unclear reporting of some information.34 For instance, both the ‘blinding of participants, personnel and outcome assessor’ and the ‘other sources of bias’ component were evaluated as unclear for all trials.
Results from the trial by Messier et al 44 indicated no statistically significant differences across groups with regard to self-reported performance measures of physical function, knee pain scores, knee strength and biomechanical measures (synovial fluid, keratan sulfate and level of IL-1) after 6 months of intervention. Findings from Messier et al 45 indicated a statistically significant benefit of the combined intervention in terms of self-reported physical function, 6 min walk test, stair climb and knee pain. The findings from Messier et al 3 indicated a significant improvement in the 6 min walk test and walking speed in the intervention group. Moreover, there was a significant reduction (p<0.05) of body weight among the intervention groups in all trials. In the current review, the finding of no effect of a combined intervention programme may be due to the very low number of included trials (and participants) but probably is not due to low compliance. Compliance of the diet and exercise group to the exercise programme at 6 months was higher in the pilot study44 compared with the IDEA trial.3 In the pilot study,44 compliance (ratio of the number of exercise sessions attended to the total number of the exercise sessions prescribed with the exercise programme) was 82.6% for the exercise group and 94.7% for diet plus exercise group. For the IDEA trial,3 399/454 participants (88%) completed the study; compliance of the diet and exercise group was 70% at 6 months and 58% at 18 months with no adverse events and no significant differences between groups.
In addition to diet and exercise, two current trials MEDIC128 and MEDIC227 have reported that a multimodal approach of education, neuromuscular exercise, insoles and, if indicated, a dietary weight loss programme and pain medication are effective for adults and older adults with moderate-to-severe knee OA. These studies were not included in this review due to the wide age range across participants. MEDIC128 included 9 participants and MEDIC227 included 12 participants below the age of 55 years and there was no subgroup analysis of older participants. In MEDIC1,28 the participants were eligible for TKR and were randomised to non-surgical and surgical treatment followed by the intervention programme. Both interventions showed substantial improvement, but the surgical treatment resulted in greater pain relief and functional improvement after 12 months compared with non-surgical treatment alone. However, only 26% of the patients who were assigned to receive non-surgical treatment alone underwent TKR in the following year.28 In MEDIC2,27 participants had radiographic confirmation of OA (Kellgren-Lawrence grade ≥1), but were not eligible for a TKR. The 12-week non-surgical treatment programme consisted of individualised progressed neuromuscular exercise, patient education, insoles, dietary advice and prescription of pain medication if indicated, while usual care comprised two leaflets with information and advice on knee OA and recommended treatments. This non-surgical treatment programme was found to be more effective with respect to pain, activities of daily living and QOL at 12 months compared with usual care, although it was not possible to determine which of the components within this multi-intervention programme were most effective and whether the intervention as a whole would be equally effective in older patients with OA.27
The main limitation of this review is that only few eligible studies were identified. Thus, the optimal components of dietary and exercise interventions in terms of type, duration and quantity suitable for this population are still unclear. Future studies are required in this field to optimise outcome measures and methods of delivering a programme at an acceptable cost, prior to a future adequately powered definitive trial.
Conclusion
Based on current evidence synthesised in this review, it is hard to judge the effectiveness of a combined programme of diet and physical activity due to the low number of included trials and participants and the quality of available evidence. Only moderate quality evidence was available to investigate the intervention programmes. However, the narrative synthesis suggests that interventions with a focus on reduction of body weight and/or improved mobility are worthy of further evaluation. Further adequately powered RCTs testing the effects of a combined intervention against each component individually are required to optimise diet and exercise interventions using a multimodal approach.
Supplementary Material
Acknowledgments
The authors would like to thank Lynn Harris, Library Services, University of Birmingham for her contribution to the development of the search strategies.
Footnotes
Contributors: ASA led the review and contributed to all stages, including development of the search strategy, running the searches, assessing trials eligibility, data extraction and synthesis (including risk of bias and Grading of Recommendation, Assessment, Development and Evaluation analysis), and preparation of the manuscript. CAG and ABR provided expertise in systematic review methodology and risk of bias analysis. AMK assisted with assessment of eligibility of included studies and data extraction. All authors read and provided feedback on the preparation of this manuscript according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2009 checklist and approved the final manuscript.
Funding: This review is a part of a PhD programme undertaken by ASA, and is fully funded by the King Saud University, Kingdom of Saudi Arabia, Riyadh and the Saudi Arabian Cultural Bureau, United Kingdom, London.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: There are no additional unpublished data from the review.
References
- 1. Imamura M, Imamura ST, Kaziyama HH, et al. Impact of nervous system hyperalgesia on pain, disability, and quality of life in patients with knee osteoarthritis: a controlled analysis. Arthritis Rheum 2008;59:1424–31. 10.1002/art.24120 [DOI] [PubMed] [Google Scholar]
- 2. Arthritis Foundation. What is arthritis [online]. 2015. http://www.arthritis.org/about-arthritis/understanding-arthritis/ (accessed Jul 2016).
- 3. Messier SP, Mihalko SL, Legault C, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA 2013;310:1263–73. 10.1001/jama.2013.277669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pouli N, Das Nair R, Lincoln NB, et al. The experience of living with knee osteoarthritis: exploring illness and treatment beliefs through thematic analysis. Disabil Rehabil 2014;36:600–7. 10.3109/09638288.2013.805257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Heidari B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: part I. Caspian J Intern Med 2011;2:205. [PMC free article] [PubMed] [Google Scholar]
- 6. Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012;380:2163–96. 10.1016/S0140-6736(12)61729-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hammerich AS, Anemaet WK. Applying the evidence for Exercise prescription in older adults with knee osteoarthritis. Curr Geriatr Rep 2016;5:179–90. 10.1007/s13670-016-0178-5 [DOI] [Google Scholar]
- 8. Arthritis Research UK. Osteoarthritis in General Practice, Data and perspectives (online). 2013. http://www.arthritisresearchuk.org/policy-and-public-affairs/reports-and-resources/reports.aspx (accessed Jul 2016).
- 9. Felson DT, Lawrence RC, Hochberg MC, et al. Osteoarthritis: new insights. part 2: treatment approaches. Ann Intern Med 2000;133:726–37. 10.7326/0003-4819-133-9-200011070-00015 [DOI] [PubMed] [Google Scholar]
- 10. Bhatia D, Bejarano T, Novo M. Current interventions in the management of knee osteoarthritis. Journal of Pharmacy and Bioallied Sciences 2013;5:30. 10.4103/0975-7406.106561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abbott JH, Robertson MC, Chapple C, et al. Manual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee: a randomized controlled trial 1: clinical effectiveness. Osteoarthritis Cartilage 2013;21:525–34. 10.1016/j.joca.2012.12.014 [DOI] [PubMed] [Google Scholar]
- 12. Dejaco C, Singh YP, Perel P, et al. 2015 recommendations for the management of polymyalgia rheumatica: a European League Against Rheumatism/American College of Rheumatology Collaborative initiative. Arthritis Rheumatol 2015;67:2569–80. 10.1002/art.39333 [DOI] [PubMed] [Google Scholar]
- 13. Fernandes L, Hagen KB, Bijlsma JW, et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis 2013;72:1125–35. 10.1136/annrheumdis-2012-202745 [DOI] [PubMed] [Google Scholar]
- 14. McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage 2014;22:363–88. 10.1016/j.joca.2014.01.003 [DOI] [PubMed] [Google Scholar]
- 15. Ryan P, Sawin KJ. The individual and Family Self-Management Theory: background and perspectives on context, process, and outcomes. Nurs Outlook 2009;57:217–25. 10.1016/j.outlook.2008.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kao MH, Tsai YF, Chang TK, et al. The effects of self-management intervention among middle-age adults with knee osteoarthritis. J Adv Nurs 2016;72:1825–37. 10.1111/jan.12956 [DOI] [PubMed] [Google Scholar]
- 17. Yusuf E. Pharmacologic and Non-Pharmacologic treatment of Osteoarthritis. Curr Treatm Opt Rheumatol 2016;2:111–25. 10.1007/s40674-016-0042-y [DOI] [Google Scholar]
- 18. Coggon D, Reading I, Croft P, et al. Knee osteoarthritis and obesity. Int J Obes 2001;25:622–7. 10.1038/sj.ijo.0801585 [DOI] [PubMed] [Google Scholar]
- 19. Huang MH, Chen CH, Chen TW, et al. The effects of weight reduction on the rehabilitation of patients with knee osteoarthritis and obesity. Arthritis Care Res 2000;13:398–405. [DOI] [PubMed] [Google Scholar]
- 20. Christensen R, Bartels EM, Astrup A, et al. Effect of weight reduction in obese patients diagnosed with knee osteoarthritis: a systematic review and meta-analysis. Ann Rheum Dis 2007;66:433–9. 10.1136/ard.2006.065904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Messier SP. Diet and exercise for obese adults with knee osteoarthritis. Clin Geriatr Med 2010;26:461–77. 10.1016/j.cger.2010.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Roddy E, Zhang W, Doherty M. Aerobic walking or strengthening exercise for osteoarthritis of the knee? A systematic review. Ann Rheum Dis 2005;64:544–8. 10.1136/ard.2004.028746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Patrick DL, Ramsey SD, Spencer AC, et al. Economic evaluation of aquatic exercise for persons with osteoarthritis. Med Care 2001;39:413–24. 10.1097/00005650-200105000-00002 [DOI] [PubMed] [Google Scholar]
- 24. Minor MA, Hewett JE, Webel RR, Kay DR, et al. Efficacy of physical conditioning exercise in patients with rheumatoid arthritis and osteoarthritis. Arthritis Rheum 1989;32:1396–405. 10.1002/anr.1780321108 [DOI] [PubMed] [Google Scholar]
- 25. Marks R. Knee osteoarthritis, obesity and exercise therapy-A complex issue. Journal of Obesity & Eating Disorders 2016;2 10.21767/2471-8203.100017 [DOI] [Google Scholar]
- 26. Ekram AR, Cicuttini FM, Teichtahl AJ, et al. Weight satisfaction, management strategies and health beliefs in knee osteoarthritis patients attending an outpatient clinic. Intern Med J 2016;46:435–42. 10.1111/imj.13007 [DOI] [PubMed] [Google Scholar]
- 27. Skou ST, Rasmussen S, Laursen MB, et al. The efficacy of 12 weeks non-surgical treatment for patients not eligible for total knee replacement: a randomized controlled trial with 1-year follow-up. Osteoarthritis Cartilage 2015;23:1465–75. 10.1016/j.joca.2015.04.021 [DOI] [PubMed] [Google Scholar]
- 28. Skou ST, Roos EM, Laursen MB, et al. A Randomized, Controlled Trial of Total Knee Replacement. N Engl J Med 2015;373:1597–606. 10.1056/NEJMoa1505467 [DOI] [PubMed] [Google Scholar]
- 29. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151:264–9. 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- 30. Higgins JPT, Green S, eds Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. the Cochrane Collaboration, 2011. http://www.cochrane-handbook.org/ (accessed Jul 2016).
- 31. Brandt KD, Fife RS, Braunstein EM, et al. Radiographic grading of the severity of knee osteoarthritis: relation of the Kellgren and Lawrence grade to a grade based on joint space narrowing, and correlation with arthroscopic evidence of articular cartilage degeneration. Arthritis Rheum 1991;34:1381–6. 10.1002/art.1780341106 [DOI] [PubMed] [Google Scholar]
- 32. Hsu LM, Field R. Interrater AgreementMeasures: comments on Kappa,Cohen's Kappa, Scott's π, and Aickin's α. Understanding Statistics 2003;2:205–19. 10.1207/S15328031US0203_03 [DOI] [Google Scholar]
- 33. Consumers and Communication Group resources for authors. Data Extraction Template (word format). http://cccrg.cochrane.org/author-resources (accessed Jul 2016).
- 34. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Green S, Higgins JP. Chapter 2: Preparing a cochrane review In: Higgins JP, Green S, eds eds Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. http://handbook.cochrane.org/chapter_2/2_preparing_a_cochrane_review.htm (accessed Jul 2016).
- 36. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177–88. 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 37. Centre for Reviews and Dissemination (CRD). Systematic reviews: crd’s Guidance for Undertaking Reviews in Healthcare. 3rd edn York: CRD University of York, York Publishing Services Ltd, 2009. https://www.york.ac.uk/media/crd/Systematic_Reviews.pdf (accessed Jul 2016). [Google Scholar]
- 38. Deeks JJ, Higgins JP, Altman DG. Chapter 9: Analyzing data and undertaking meta-analyses In: Higgins JP, Green S, eds eds Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. http://handbook.cochrane.org/chapter_9/9_8_chapter_information.htm (accessed Jul 2016).
- 39. Rodgers M, Arai L, Britten N, et al. ; Guidance on the conduct of narrative synthesis in systematic reviews: a comparison of guidance-led narrative synthesis versus meta-analysis 14th Cochrane Colloquium, 2006:23–6. [Google Scholar]
- 40. Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis in systematic reviews. ESRC methods programme 2006;15:047–71. [Google Scholar]
- 41. Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines 6. Rating the quality of evidence–imprecision. J Clin Epidemiol 2011;64:1283–93. 10.1016/j.jclinepi.2011.01.012 [DOI] [PubMed] [Google Scholar]
- 42. Schünemann H, Brozek J, Oxman A. GRADE handbook for grading quality of evidence and strength of recommendation. the GRADE Working Group, 2009. http://gdt.guidelinedevelopment.org/app/handbook/handbook.html(accessed Jul 2016).
- 43. Grading quality of evidence and strength of recommendations. www.gradepro.org (accessed Jul 2016).
- 44. Messier SP, Loeser RF, Mitchell MN, et al. Exercise and weight loss in obese older adults with knee osteoarthritis: a preliminary study. J Am Geriatr Soc 2000;48:1062–72. 10.1111/j.1532-5415.2000.tb04781.x [DOI] [PubMed] [Google Scholar]
- 45. Messier SP, Loeser RF, Miller GD, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the Arthritis, Diet, and activity Promotion Trial. Arthritis Rheum 2004;50:1501–10. 10.1002/art.20256 [DOI] [PubMed] [Google Scholar]
- 46. Rejeski WJ, Focht BC, Messier SP, et al. Obese, older adults with knee osteoarthritis: weight loss, exercise, and quality of life. Health Psychol 2002;21:419–26. 10.1037/0278-6133.21.5.419 [DOI] [PubMed] [Google Scholar]
- 47. Focht BC, Rejeski WJ, Ambrosius WT, et al. Exercise, self-efficacy, and mobility performance in overweight and obese older adults with knee osteoarthritis. Arthritis Rheum 2005;53:659–65. 10.1002/art.21466 [DOI] [PubMed] [Google Scholar]
- 48. Stovold E, Beecher D, Foxlee R, et al. Study flow diagrams in Cochrane systematic review updates: an adapted PRISMA flow diagram. Syst Rev 2014;3:54. 10.1186/2046-4053-3-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Gremeaux V, Troisgros O, Benaïm S, et al. Determining the minimal clinically important difference for the six-minute walk test and the 200-meter fast-walk test during cardiac rehabilitation program in coronary artery disease patients after acute coronary syndrome. Arch Phys Med Rehabil 2011;92:611–9. 10.1016/j.apmr.2010.11.023 [DOI] [PubMed] [Google Scholar]
- 50. Perera S, Mody SH, Woodman RC, et al. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc 2006;54:743–9. 10.1111/j.1532-5415.2006.00701.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-014537supp001.pdf (197.3KB, pdf)