Abstract
Objectives
To determine the incidence of unplanned readmissions to pediatric intensive care units (PICUs) within one year and examine risk factors associated with repeated readmission.
Design, Settings, & Patients
Retrospective cohort study of 93,379 patients discharged between 2009 and 2010 from 76 North American PICUs.
Measurements
Outcomes of index admissions and unplanned readmissions were compared. Timing of readmissions and variation of proportion of readmissions across sites were examined. Cumulative incidence curves for readmission were constructed. Time-to-event analyses were performed to examine factors associated with readmission within one year and to estimate their hazard ratios (HR).
Main Results
Eleven percent (10,233) of patients had 15,625 unplanned readmissions within one year to the same PICU; 3.4% had two or more readmissions. Readmissions had significantly higher PICU mortality and longer PICU length of stay, compared to index admissions (4.0% versus 2.5%, and 2.5 versus 1.6 days, all P<0.001). Median time to readmission was 30 days for all readmissions; 3.5 days for readmissions during the same hospitalization; and 66 days for different hospitalizations. Time-to-event analyses showed that having more complex chronic conditions (CCCs) was associated with earlier readmission—adjusted HR 2.9 for one CCC; HR 4.8 for two CCC; HR 9.6 for three or more CCC, all P<0.001 compared no CCC). Most specific CCC conferred a greater risk of readmission, and some had considerably higher risk than others.
Conclusions
Unplanned readmissions occurred in a sizable minority of PICU patients. Patients with CCCs and particular conditions were at much higher risk for readmission.
Keywords: Hospital Readmission, Intensive Care Units, Pediatric, Child
Introduction
Anecdotally and from studies that record more admissions than patients (1–2), it is known that some children, for example those with complex chronic conditions (CCC), are repeatedly admitted to pediatric intensive care units (PICUs) for both planned and unplanned reasons. Unplanned readmissions are a focus of healthcare quality measurement, as they may be preventable (3) and are associated with worse outcomes (4–5) and higher costs (6–7). Furthermore, repeated critical illness and hospitalization negatively impact patients and families (8–10). Except for a few studies focused on early readmissions (4) and readmissions during the same hospitalization (11–13), it is not known how often unplanned PICU readmissions occur and who are at most risk.
Using a multi-institutional cohort, we sought to determine the incidence and outcomes of unplanned PICU readmissions within one year and examine the patient characteristics and conditions that are associated with repeated readmission. This information will permit clinicians and administrators to better plan resources and interventions to address such readmissions, as well as provide anticipatory guidance to patients and families.
Methods
We performed a retrospective cohort study of patients discharged between 2009 and 2010 and followed for one year at 92 North American PICUs that participated in the Virtual Pediatric Systems (VPS, LLC, Los Angeles, CA). VPS contains encounter-level information entered by VPS-trained persons at the individual sites. Annual certification of data definitions, routine interrater reliability testing, and automated and manual data cleaning queries ensure data validity and quality (14). Our outcome was unplanned PICU readmissions within one year of index PICU discharge, during the same or different hospitalization and to the same PICU. Sites varied in the duration of data contributed (submitted as 3-month quarters). To ensure one year of follow-up, we included only sites that contributed ≥5 consecutive quarters of data, and no study patients were drawn from the last year of data contributed by a site. For example, if a site had 10 consecutive quarters of data (eg, July 2009 through December 2011), study patients were those discharged during the first 6 quarters (July 2009 through December 2010), but all 10 quarters could be used to identify these patients’ unplanned readmissions within one year from index discharge. Unique patient identifiers permitted detection of readmissions to the same PICU, but not to another PICU (VPS or otherwise). We excluded patients who died during their first admission.
For all admissions, multiple patient and clinical variables were available, as well as dates/times of admission and discharge, diagnoses, and procedures. Demographics included gender, age, race, insurance, and number of CCCs. Patients of all ages were included as adults are cared for in PICUs (15). CCCs were defined using Feudtner’s definition (16) and identified among diagnoses using a list of VPS codes developed by Edwards et al. (17). Sites that did not report secondary diagnoses were excluded, because we considered CCC particularly relevant to readmission risk. Admission variables included planned, peri-operative, trauma, patient origin, risk of PICU mortality, and whether invasive ventilation via endotracheal tube or tracheostomy was used. Risk of mortality was estimated using Paediatric Index of Mortality 2 (PIM2) (18) and was used as a proxy for admission severity-of-illness. Discharge variables included disposition location, discharge season, and PICU length of stay (LOS). Discharge season was included to control for seasonal illness variation (19–20) and was categorized as four 3-month blocks.
Analysis
Characteristics were reported as proportions/rates and 95% confidence intervals (CI), means and standard deviations (SD), and medians and interquartile ranges (IQR). Characteristics of included and excluded sites were compared using Pearson’s chi2 test. Characteristics of admissions (index and planned readmissions) and unplanned readmissions were compared using Pearson’s chi2 test, unpaired two-tailed t-test, or Mann-Whitney U test. To compare outcomes of index admissions and unplanned readmissions, we performed bivariate analyses of their PICU LOS and mortality (index admissions resulting in death were included in mortality comparison only). We reported the primary reasons for admissions and unplanned readmissions, which are the first diagnosis in VPS.
To describe variation across PICUs, we calculated the median proportion of unplanned readmissions within one year and the ranges of these readmissions among the sites.
Using descriptive statistics and histograms, we described the time from index PICU discharge to unplanned readmission for readmissions during the same and different hospitalizations. We constructed curves for cumulative incidences of unplanned PICU readmission within one year by number of CCC and for specific chronic conditions, using only time to first unplanned readmission.
We examined factors associated with unplanned PICU readmission within one year and estimated their hazard ratios (HR), using Cox proportional hazard conditional risk set models (time from the previous event) for multiple failure-time data (21). This modeling allows for multiple unplanned readmissions for the same patient where time to each readmission was measured from the previous (unplanned or planned) PICU discharge. Patients were censored at one year from index discharge. PICU mortality was treated as non-informative censoring, rather than a competing risk, because it is relatively rare. Estimation of risk was stratified for each sequential unplanned readmission within one year, with index admission being the first stratum. Stratified risk did not change with planned readmissions. Unplanned readmissions beyond the fourth were consider within the fourth stratum because few patients had >4 within one year. To accommodate multiple levels of clustering, patients were treated as random effects, and PICU sites were adjusted for as a fixed effect.
Two models were fitted: 1) a model in which the number of CCCs was a primary predictor; and 2) a model with covariates for specific chronic conditions. Factors adjusted for in these models included the characteristics listed above. Because of non-linear relationships with readmission, age was parsimoniously divided into an ordinal variable, and PIM2 and LOS were transformed into cubic splines. Institutional variables included number of licensed PICU beds (≤ 17, 18–24, ≥25 beds), presence of a separate intermediate-level care unit, and presence of a pediatric critical care fellowship program. The PICU’s average daily census by quarter of discharge was used as a metric of ICU strain, which has been shown to affect ICU triage decisions (22). Sepsis diagnosis was included because many survivors of pediatric severe sepsis have unplanned hospital readmissions (23). Independent variables for the final models were included if their P-value was <0.2 in multivariate analysis. Race and insurance were excluded because they were unavailable for a sizable proportion of observations.
When information was available for only a subgroup of the patients, we noted this in the text or tables. Statistical significance was determined using a P-value of <0.05. Stata 14 (StataCorp LP, College Station, TX) was used for analyses and figures. Because all data were deidentified, this study qualified for exemption from review by the University of California, San Francisco Committee on Human Research.
Results
There were 76 included and 16 excluded PICUs; included sites had more pediatric beds then excluded sites (Table 1). Supplemental Figure 1 is a flowchart of included and excluded patients, admissions, and units. The 76 units contributed 442 quarters of data between 2009 and 2010. After excluding 2,437 patients who died during their first admission, 93,379 patients and 115,157 total admissions remained for analysis. Of these patients, 10,233 (11%) had 15,625 unplanned readmissions within one year—7.6% had one readmission, 2.0% had two, 1.4% had ≥3. Unplanned readmissions within one year accounted for 20% of all ICU patient-care days. Twenty-one percent of patients with a CCC had an unplanned readmission, compared to 4% of patients without a CCC. Twenty-six percent of unplanned readmissions were during the same hospitalization.
Table 1.
Institutional characteristics of study sites
| Characteristic, n (%) | Included sites n=76 (100%) | Excluded sitesa n=16 (100%) | P value |
|---|---|---|---|
| Number of licensed pediatric beds | 0.03 | ||
| ≤ 110 | 18 (24) | 5 (31) | |
| 111–249 | 27 (35) | 10 (63) | |
| ≥ 250 | 31 (41) | 1 (6) | |
| Number of licensed pediatric ICU beds | 0.77 | ||
| ≤ 17 | 28 (37) | 7 (44) | |
| 18–24 | 31 (41) | 5 (31) | |
| ≥ 25 | 17 (22) | 4 (25) | |
| Affiliated PCCM fellowship program | 37 (49) | 6 (38) | 0.42 |
| Number of consecutive quarters of datab | |||
| 5–8 | 21 (28) | ||
| 9–10 | 21 (28) | ||
| 11–12 | 34 (45) |
ICU, intensive care unit; PCCM, pediatric critical care medicine
14 excluded sites because they contributed <5 consecutive quarters of data; 2 excluded sites contributed ≥5 quarters of consecutive data but did not report secondary diagnoses
Study patients were not drawn from the last 4 quarters of a site’s data, though unplanned readmissions could be identified during those quarters
The proportion of admissions that were unplanned readmissions within one year varied among PICUs, ranging 4.6–26.9% (median 13.5%, IQR 10.6–15.1%).
Characteristics of admissions and unplanned readmission are presented in Table 2. Readmitted admissions more often patients who were younger, on public insurance, had CCCs, and invasively ventilated during their index PICU admission. Trauma patients were less frequently readmitted. The PICU mortality for index admissions was 2.5% versus 4.0% for unplanned readmissions (P<0.001). The median PICU LOS for index admissions was 1.6 days (IQR 0.9–3.4) versus 2.5 days (IQR 1.1–6.0, P<0.001) for unplanned readmissions. Unplanned readmissions were primarily due to respiratory, infectious, and neurological conditions; index admissions and planned readmissions were commonly due to respiratory, cardiac, and neurological conditions (Supplemental Table 1).
Table 2.
Characteristics of PICU admissions by readmission status
| Characteristic, % (95% CI) | Not readmitted n=99,532 (85%) | Readmitted n=15,625 (15%) |
|---|---|---|
| Male sex† | 55.9 (55.6–56.2) | 54.6 (53.8–55.4) |
| Age, months, median (IQR)* | 55 (12–150) | 46 (13–152) |
| Racea | ||
| Caucasian† | 51.9 (51.5–52.2) | 49.7 (48.8–50.6) |
| African American* | 18.6 (18.3–18.9) | 21.1 (20.4–21.9) |
| Hispanic* | 18.2 (17.9–18.5) | 19.8 (19.1–20.6) |
| Asian/Indian/Pacific Islander† | 2.7 (2.6–2.8) | 2.3 (2.1–2.6) |
| Other/mixed | 5.6 (5.4–5.7) | 5.2 (4.8–5.6) |
| Unspecified* | 3.1 (3–3.3) | 1.9 (1.7–2.2) |
| Insuranceb | ||
| Medicaid/Medicare/Government* | 51.1 (50.6–51.5) | 62.6 (61.4–63.7) |
| Commercial* | 43.7 (43.3–44.2) | 34.8 (33.6–35.9) |
| Self-Pay* | 3.2 (3.1–3.4) | 1.2 (0.9–1.5) |
| Other† | 2 (1.8–2.1) | 1.5 (1.2–1.8) |
| Complex chronic condition | ||
| No CCC* | 48 (47.7–48.3) | 13.8 (13.2–14.3) |
| 1 CCC* | 23.5 (23.2–23.7) | 18.3 (17.7–18.9) |
| 2 CCC* | 13.5 (13.3–13.8) | 18.6 (18–19.2) |
| ≥3 CCC* | 15 (14.8–15.2) | 49.4 (48.6–50.1) |
| Unplanned* | 68.1 (67.8–68.4) | 100 |
| Pre-/post-operative* | 37.7 (37.4–38) | 12.7 (12.2–13.2) |
| Origin | ||
| Emergency Department | 46.2 (45.9–46.5) | 45.5 (44.7–46.2) |
| OR/PACU/procedure suite* | 34.7 (34.4–35) | 9.5 (9.1–10) |
| General ward* | 11 (10.8–11.1) | 29.9 (29.1–30.6) |
| Another ICU* | 3.3 (3.2–3.4) | 1.7 (1.5–1.9) |
| Intermediate/telemetry unit* | 1.5 (1.4–1.6) | 7.1 (6.7–7.5) |
| Chronic/rehabilitation facility* | 0.1 (0.1–0.2) | 0.8 (0.7–1) |
| Outpatient/home* | 2.7 (2.6–2.8) | 5.2 (4.8–5.5) |
| Other | 0.5 (0.4–0.5) | 0.4 (0.3–0.5) |
| Trauma* | 9.5 (9.3–9.7) | 1.5 (1.4–1.7) |
| PIM2 risk of mortality, %, mean (SD)* | 2.2 (5.4) | 3.6 (8.1) |
| Invasive ventilation used during admission* | 29.6 (29.3–29.9) | 33.3 (32.6–34) |
| Disposition | ||
| General ward* | 65.5 (65.2–66.8) | 56 (55.2–56.8) |
| Another ICU | 2.3 (2.3–2.4) | 2 (1.8–2.2) |
| Intermediate/telemetry unit† | 12.1 (11.9–12.3) | 14.2 (13.7–14.8) |
| OR | 0.5 (0.4–0.5) | 0.5 (0.4–0.7) |
| Chronic/rehabilitation facility* | 0.8 (0.7–0.8) | 2 (1.8–2.2) |
| Home* | 17.8 (17.6–18) | 20.8 (20.2–21.5) |
| Hospice† | 0 (0–0.1) | 0.2 (0.1–0.2) |
| Other† | 0.9 (0.9–1) | 0.3 (0.2–0.4) |
| LOS, days, median (IQR)* | 1.6 (0.9–3.5) | 2.5 (1.1–6) |
CCC, complex chronic condition; CI, confidence interval; PACU, post-anesthesia care unit; ICU, intensive care unit; IQR, interquartile range; LOS, length of stay; OR, operating room; PIM, Paediatric Index of Mortality; PICU, pediatric intensive care unit; SD, standard deviation
P < 0.05;
P ≤ 0.001 by chi2 test, t-test, or Mann-Whitney U test
Based on 72,558 (74%) index admissions from 55 sites that supplied race
Based on 41,847 (43%) index admissions from 30 sites that supplied insurance
The timing of unplanned readmissions is shown in Supplemental Figure 2. The median time to readmission was 30 days (IQR 5–106) for all readmissions; 3.5 days (IQR 1.2–9.0) for readmissions during the same hospitalization and 66 days (IQR 24–151) for different hospitalizations. Figure 1 and Supplemental Figure 3 depict the cumulative incidence curves grouped by number of CCCs and specific conditions, respectively, using only time to first unplanned readmission.
Figure 1.
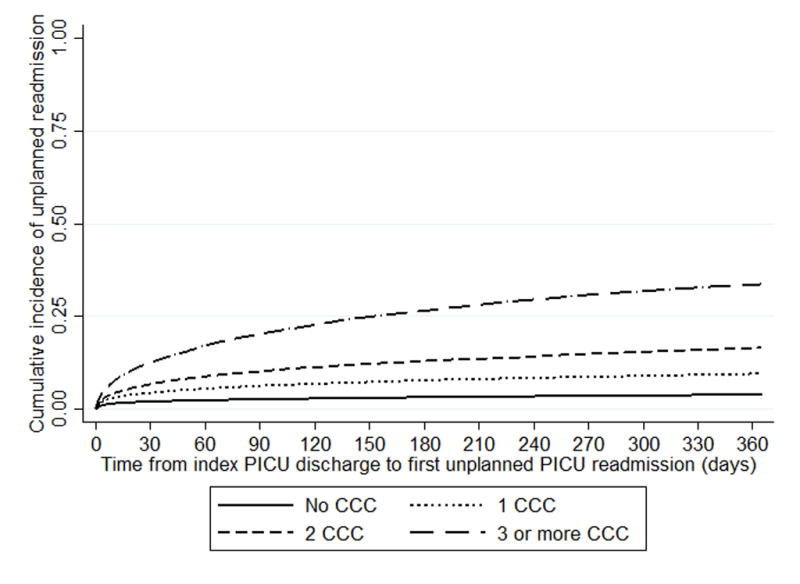
Cumulative incidences of unplanned PICU readmission within one year by number of complex chronic conditions.
Time-to-event analyses showed that having a CCC was significantly associated with earlier unplanned PICU readmission, after controlling for age, PIM2 score, whether the admission was unplanned, perioperative, trauma-related, or from another institution, use of invasive ventilation, discharge disposition, PICU site, number of PICU and pediatric beds, and each unit’s average daily census by quarter. Having more CCCs was associated with greater hazard of readmission (HR 2.9 for one CCC; HR 4.8 for two CCCs; HR 9.6 for ≥ three CCCs, all P<0.001 and compared to not having a CCC) (Table 3). Other variables were also significantly associated with greater or lower hazard for readmission. Being over 18 months of age was associated with lower hazards of readmission, compared to being 0–1 months. PICU admissions for perioperative or trauma reasons were associated with lower hazards of readmission. Compared to being discharged to the general ward, most disposition locations were associated with lower hazards for readmission. Unplanned admission and using invasive ventilation were associated with higher hazards for readmission.
Table 3.
Hazard ratios of predictor variables in base model of unplanned PICU readmission within one yeara
| Patient or admission variable | HR (95% CI) | P value |
|---|---|---|
| Complex chronic condition | ||
| No CCC (reference) | ||
| 1 CCC | 2.86 (2.68–3.05) | <0.001 |
| 2 CCC | 4.78 (4.48–5.1) | <0.001 |
| ≥3 CCC | 9.56 (8.98–10.2) | <0.001 |
| Age | ||
| 0–1 months (reference) | ||
| 2–3 months | 1.13 (1.03–1.24) | 0.008 |
| 4-–5 months | 1.08 (0.98–1.19) | 0.11 |
| 6–17 months | 0.96 (0.89–1.03) | 0.26 |
| 18 mon – 4 yr | 0.77 (0.71–0.83) | <0.001 |
| 5–9 years | 0.66 (0.61–0.72) | <0.001 |
| 10–17 years | 0.76 (0.71–0.82) | <0.001 |
| 18–29 years | 0.76 (0.69–0.84) | 0.001 |
| ≥30 years | 0.71 (0.5–0.995) | 0.047 |
| Unplanned index admission | 1.46 (1.37–1.55) | <0.001 |
| Perioperative | 0.7 (0.66–0.74) | <0.001 |
| Trauma | 0.57 (0.51–0.64) | <0.001 |
| Admitted from another institution | 0.85 (0.81–0.89) | <0.001 |
| Invasive ventilation used during admission | 1.09 (1.04–1.14) | <0.001 |
| Disposition | ||
| General ward (reference) | ||
| Intermediate/telemetry unit | 1.05 (0.99–1.11) | 0.1 |
| Another ICU | 0.43 (0.36–0.52) | <0.001 |
| Operating room | 0.79 (0.63–0.99) | 0.04 |
| Chronic/rehabilitation facility | 0.9 (0.8–1.02) | 0.1 |
| Hospice | 0.24 (0.1–0.57) | 0.002 |
| Home | 0.88 (0.84–0.92) | <0.001 |
| Other | 0.51 (0.38–0.69) | <0.001 |
| Admitted to PICU with | ||
| Pediatric beds | ||
| ≤110 (reference) | ||
| 111–249 | 1.72 (1–2.98) | 0.05 |
| ≥250 | 2.18 (1.22–3.88) | 0.008 |
| ICU beds | ||
| ≤17 (reference) | ||
| 18–24 | 0.84 (0.63–1.13) | 0.25 |
| ≥25 | 0.66 (0.51–0.84 | 0.001 |
CCC, complex chronic condition; CI, confidence interval; PACU, post-anesthesia care unit; ICU, intensive care unit; IQR, interquartile range; OR, odds ratio; PICU, pediatric intensive care unit
Model adjusted for PICU site and the unit’s average daily census by quarter at patients’ discharge, as well as PIM2 score as cubic splines.
In the model with specific chronic conditions, most conditions were associated with greater risk of earlier readmission, after adjusting for the other conditions and the same covariates controlled for in the CCC model (Table 4). Chronic heart failure, bronchopulmonary dysplasia, cystic fibrosis, miscellaneous chronic respiratory conditions, cerebral palsy, static encephalopathy, muscular dystrophy, spinal muscular atrophy type 1, miscellaneous neurologic/neuromuscular conditions, central nervous system tumors, solid tumors, hemopoietic cancers, miscellaneous gastrointestinal conditions, renal conditions, diabetes, metabolic conditions, immunologic conditions, and congenital infections all had >50% higher hazards for readmission. Hemopoietic cancers had the highest hazard for readmission (HR 2.1 [95% CI 1.9–2.3]). Asthma was associated with a statistically lower hazard of readmission.
Table 4.
Hazard ratios of specific chronic conditions in model of unplanned PICU readmission within one yeara
| Chronic condition/categories | HR (95% CI) | P value |
|---|---|---|
| Cardiac | ||
| Arrhythmia, chronic | 1.03 (0.87–1.23) | 0.73 |
| Congenital heart disease, simple | 1.18 (1.1–1.28) | <0.001 |
| Congenital heart disease, complex | 1.45 (1.36–1.55) | <0.001 |
| Heart failure, chronic | 1.55 (1.4–1.72) | <0.001 |
| Heart transplant | 1.23 (0.92–1.6) | 0.16 |
| Pulmonary hypertension | 1.13 (1.02–1.25) | 0.02 |
| Respiratory/airway | ||
| Asthma | 0.93 (0.88–0.99) | 0.03 |
| Bronchopulmonary dysplasia | 1.54 (1.41–1.7) | <0.001 |
| Cystic fibrosis | 1.72 (1.39–2.12) | <0.001 |
| Pulmonary hypoplasia | 1.19 (0.9–1.59) | 0.22 |
| Upper airway anomaly | 1.26 (1.18–1.34) | <0.001 |
| Other chronic respiratory condition | 1.63 (1.51–1.75) | <0.001 |
| Neurologic | ||
| Cerebral palsy | 1.51 (1.42–1.61) | <0.001 |
| Epilepsy | 1.21 (1.14–1.28) | <0.001 |
| Static encephalopathy or generalized developmental delay | 1.7 (1.61–1.78) | <0.001 |
| Hydrocephalus | 1.36 (1.27–1.46) | <0.001 |
| Muscular dystrophy | 1.61 (1.38–1.88) | <0.001 |
| Spina bifida | 1.36 (1.21–1.53) | <0.001 |
| Spinal cord injury (including paralysis) | 1.23 (1.1–1.37) | <0.001 |
| Spinal muscular atrophy, type 1 | 1.98 (1.69–2.33) | <0.001 |
| Other neurologic/neuromuscular condition | 1.65 (1.56–1.75) | <0.001 |
| Oncologic | ||
| Bone marrow transplant | 1.40 (1.2–1.65) | <0.001 |
| Central nervous system tumor | 1.81 (1.67–1.96) | <0.001 |
| Hemopoietic | 2.11 (1.91–2.33) | <0.001 |
| Solid tumor | 1.82 (1.65–2) | <0.001 |
| Gastrointestinal | ||
| Liver failure | 1.44 (1.26–1.64) | <0.001 |
| Other GI condition | 1.55 (1.42–1.69) | <0.001 |
| Hematologic | ||
| Sickle cell | 1.41 (1.13–1.75) | 0.002 |
| Other hematologic | 1.3 (1.17–1.45) | <0.001 |
| Renal condition | 1.52 (1.38–1.68) | <0.001 |
| Endocrinologic | ||
| Diabetes | 1.54 (1.41–1.68) | <0.001 |
| Other endocrinologic condition | 1.38 (1.29–1.48) | <0.001 |
| Metabolic condition | 1.85 (1.72–1.98) | <0.001 |
| Immunologic condition | 1.64 (1.49–1.8) | <0.001 |
| Genetic abnormality/syndrome | 1.41 (1.34–1.49) | <0.001 |
| Rheumatologic condition | 1.29 (1.06–1.58) | 0.01 |
| Prematurity | 1.21 (1.13–1.3) | <0.001 |
| Congenital infection | 1.69 (1.25–2.28) | 0.001 |
CI, confidence interval; GI, gastrointestinal; HR, hazard ratio; PICU, pediatric intensive care unit;
Model adjusted for age, unplanned admission, trauma admission, perioperative admission, sepsis during admission, use of invasive ventilation, disposition location, discharge season, number of pediatric hospital beds, number of PICU beds, PICU site, the unit’s average daily census by quarter at patients’ discharge, and PIM2 score.
Gender, patient origin, sepsis diagnosis, PICU LOS, discharge season, and presence of a pediatric critical care fellowship program were not included in the models as they were not associated with earlier readmission (P>0.2).
Discussion
Repeated illness and unplanned PICU admissions can lead to physical and psychological morbidity for patients and considerable stress for families (8–10). For institutions, lengthy unplanned PICU readmissions may be obstacles to hospital efficiency, potentially delaying admissions of other critically ill patients or patients needing major elective surgeries. Thus, readmissions are relevant to patients, families, clinicians, and administrators. This is the first study to examine the frequency, timing, and outcomes of unplanned PICU readmissions within one year and to explore their reasons and risk factors.
Previous studies of PICU readmissions focused on early unplanned readmissions, included only readmissions within the same hospitalization, conflated planned and unplanned readmissions, and/or reflected a single institution (4, 11–12, 24–26). These studies showed that chronic conditions were associated with PICU readmissions. Similarly, studies of hospitalized children showed that CCCs and number of CCCs were associated with rehospitalization (27–29). In a study of 72 U.S children’s hospitals, Berry et al. found that 22% of patients in 2003 were rehospitalized within a year; 3% experienced ≥4 rehospitalizations (29). Feudtner et al. found a 17% 1-year incidence of rehospitalization among children admitted to 38 U.S. children’s hospitals in 2004 (30). Patients with any CCC (excluding hematologic/immunologic) were more likely to be rehospitalized than those without CCCs. Feudtner also found that patients who had hospitalizations prior to their index admission were more likely to be rehospitalized.
Our study expands on previous ones by concentrating on unplanned PICU readmissions, both “early” or “late” and during the same or different hospitalizations, in a multi-institutional cohort. We observed that 11% of PICU patients had an unplanned readmission within one year; over 3% had two or more. Readmissions had higher mortality rates and longer PICU LOS compared to index admissions, and they accounted for almost a fifth of patient-care days, making their impact disproportionate to their numbers. Eighty-six percent of readmitted children had a CCC. Children with a CCC had a greater than a two-fold risk of unplanned PICU readmission, compared to children without CCCs. This risk increased the more CCCs a patient had. When specific chronic conditions were examined, most conditions conferred a greater risk of readmission, and some had considerably higher risk than others. Notably, most patients, even those with CCC, do not experience a readmission within one year.
Unplanned PICU readmissions are likely an indication of medical fragility (11) and high acute and outpatient/community care needs. Such readmissions may increase as the number of children with CCC grows. Appreciating which patients are more likely to experience readmission could be helpful in providing tailored anticipatory guidance about repeated illness and readmission risks to families (31), as well as concentrate resource planning and efforts to mitigate preventable readmissions (32). For instance, high-risk patients might be kept in the PICU longer to ensure clinical stability, transferred to intermediate care, or provided more intense disposition planning and outpatient follow-up. Additionally, for children with CCC who are in and out of the PICU, pediatric critical care medicine could adopt a patient-centered specialty practice model (33), where intensivists more actively participate in these children’s “medical neighborhood”, as opposed to providing mostly discrete and transitory care. Some PICUs have moved towards this model by instituting “primary PICU attendings”—one intensivist remains a consistent physician-presence for the patient/family and care team throughout the child’s PICU stay and despite changes in the intensivist(s) who orchestrates day-to-day management. Conceivably, the primary PICU attending’s involvement could extend beyond the child’s PICU or hospital stay (eg, involvement in outpatient communication between the primary/complex care provider and specialty providers). The potential patient-centered and institutional benefits of a primary PICU attending or other manifestations of a PICU patient-centered specialty practice model should be explored and studied quantitatively and qualitatively.
This study has several limitations. First, like other readmission studies (34), we assumed patients received all their critical care at their index institution and we did not have data about patients who were readmitted to a different PICU, died outside their index PICU, or transferred care to other institutions. Thus, we likely underestimated the frequency of PICU readmission (35). However, many patients with CCC tend to receive their on-going care in their respective regional, tertiary center (36). Second, some of the study patients’ index admission were likely readmissions of previous admissions that we did not have data on. Third, causes of readmission are undoubtedly multifactorial and interconnected. This is especially true for patients with CCCs, who often depend on multiple people/systems of care to avoid hospitalization (30, 37–40). VPS contains only PICU data; thus, many potential clinical and nonclinical factors could not be controlled for. The potential confounding from differences among institutions in their tendencies to admit patients to their PICU was somewhat mitigated by adjusting for PICU site. Fourth, several variables likely became less relevant to the risk of readmission the further in time from discharge (eg, PIM2, discharge season and location). We did not include interaction terms between these variables and time between admissions because doing so would have violated the assumption of proportional hazards. Finally, we may have introduced bias by excluding sites that reported <5 consecutive quarters of data. However, we do not believe this potential bias to be systematic.
Conclusions
In this multi-institutional study, we found that unplanned PICU readmissions occurred in a sizable minority of PICU patients, that the PICU mortality and LOS was greater in these readmissions than index admissions, and that patients with CCCs and particular conditions were at higher risk for earlier readmission. Further critical care and non-critical care research is needed to further identify patients most at risk for unplanned readmissions and to improve care systems so as to reduce their number and impact. Such efforts could include PICU providers becoming more actively involved in some patients’ medical neighborhood and on-going care.
Supplementary Material
Supplemental Figure 1. Flowchart of included and excluded patients, admissions, and units.
Supplemental Figure 2. Distribution of unplanned readmissions within one year by time from PICU discharge. A) All unplanned readmissions. B) Unplanned readmissions during the same hospitalization. C) Unplanned readmissions during different hospitalizations.
Supplemental Figure 3. Cumulative incidences of PICU patients readmitted within year by specific chronic condition or condition categories. A) Patients with cardiac conditions. B) Patients with respiratory conditions. C) Patients with neurologic/neuromuscular conditions. D) Patients with oncologic conditions. E) Patients with GI, hematologic, or endocrinologic conditions. F) Patients with other conditions.
Supplemental Table 1. Reasons for admission
Acknowledgments
We thank the VPS, LLC for providing the data for this study. No endorsement or editorial restriction of the interpretation of these data or opinions of the authors have been implied or stated. We also thank Dr. Gloria Chiang for her reading of the manuscript.
Funding/Support: Dr. Edwards is supported by a National Institutes of Health K23 grant (K23 HD 082361)
Abbreviations
- CCC
complex chronic condition
- CI
confidence interval
- HR
hazard ratio
- IQR
interquartile range
- LOS
length of stay
- PIM
Paediatric Index of Mortality
- PICU
pediatric intensive care unit
- SD
standard deviations
- VPS
Virtual Pediatric Intensive Care Unit Systems
Footnotes
This study was performed at University of California, San Francisco and Columbia University Medical Center.
Conflict of Interest Disclosures: The authors have no potential financial or other conflicts of interest to disclose.
References
- 1.Graham RJ, Dumas HM, O’Brien JE, et al. Congenital neurodevelopmental diagnoses and an intensive care unit: defining a population. Pediatr Crit Care Med. 2004;5:321–328. doi: 10.1097/01.pcc.0000128892.38431.2b. [DOI] [PubMed] [Google Scholar]
- 2.Namachivayam SP, Alexander J, Slater A, et al. Five-Year Survival of Children With Chronic Critical Illness in Australia and New Zealand. Crit Care Med. 2015;43:1978–1985. doi: 10.1097/CCM.0000000000001076. [DOI] [PubMed] [Google Scholar]
- 3.National Quality Forum. [Accessed July 31, 2015];NQF Endorses All-Cause Unplanned Readmissions Measures. Available at: http://www.qualityforum.org/News_And_Resources/Press_Releases/2012/NQF_Endorses_All-Cause_Unplanned_Readmissions_Measures.aspx.
- 4.Edwards JD, Lucas AR, Stone PW, et al. Frequency, risk factors, and outcomes of early unplanned readmissions to PICUs. Crit Care Med. 2013;41:2773–2783. doi: 10.1097/CCM.0b013e31829eb970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pollack MM, Patel KM, Ruttimann UE. PRISM III: an updated Pediatric Risk of Mortality score. Crit Care Med. 1996;24:743–752. doi: 10.1097/00003246-199605000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Regenstein M, Andres E. Reducing hospital readmissions among medicaid patients: a review of the literature. Qual Manag Health Care. 2014;23:20–42. doi: 10.1097/QMH.0000000000000016. [DOI] [PubMed] [Google Scholar]
- 7.Gay JC, Agrawal R, Auger KA, et al. Rates and impact of potentially preventable readmissions at children’s hospitals. J Pediatr. 2015;166:613–619. doi: 10.1016/j.jpeds.2014.10.052. [DOI] [PubMed] [Google Scholar]
- 8.Manning JC, Hemingway P, Redsell SA. Long-term psychosocial impact reported by childhood critical illness survivors: a systematic review. Nurs Crit Care. 2014;19:145–156. doi: 10.1111/nicc.12049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Netzer G, Sullivan DR. Recognizing, naming, and measuring a family intensive care unit syndrome. Ann Am Thorac Soc. 2014;11:435–441. doi: 10.1513/AnnalsATS.201309-308OT. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Latour JM, van Goudoever JB, Schuurman BE, et al. A qualitative study exploring the experiences of parents of children admitted to seven Dutch pediatric intensive care units. Intensive Care Med. 2011;37:319–325. doi: 10.1007/s00134-010-2074-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Odetola FO, Clark SJ, Dechert RE, et al. Going back for more: an evaluation of clinical outcomes and characteristics of readmissions to a pediatric intensive care unit. Pediatr Crit Care Med. 2007;8:343–347. doi: 10.1097/01.PCC.0000269400.67463.AC. [DOI] [PubMed] [Google Scholar]
- 12.Kanter RK. Post-intensive care unit pediatric hospital stay and estimated costs. Crit Care Med. 2000;28:220–223. doi: 10.1097/00003246-200001000-00036. [DOI] [PubMed] [Google Scholar]
- 13.Carroll CL, Uygungil B, Zucker AR, et al. Identifying an at-risk population of children with recurrent near-fatal asthma exacerbations. J Asthma. 2010;47:460–464. doi: 10.3109/02770903.2010.481344. [DOI] [PubMed] [Google Scholar]
- 14.Virtual Pediatric Systems, LLC. [Accessed October 31, 2016];Shaping the future of pediatric critical care through collaborative improvement. Available at: http://media.wix.com/ugd/40378f_5dadc442dddf4278bf70b46f937f827c.pdf.
- 15.Edwards JD, Houtrow AJ, Vasilevskis EE, et al. Multi-institutional profile of adults admitted to pediatric intensive care units. JAMA Pediatr. 2013;167:436–443. doi: 10.1001/jamapediatrics.2013.1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: A population-based study of Washington State, 1980–1997. Pediatrics. 2000;106:205–209. [PubMed] [Google Scholar]
- 17.Edwards JD, Houtrow AJ, Vasilevskis EE, et al. Chronic conditions among children admitted to U.S. pediatric intensive care units: their prevalence and impact on risk for mortality and prolonged length of stay. Crit Care Med. 2012;40:2196–2203. doi: 10.1097/CCM.0b013e31824e68cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Slater A, Shann F, Pearson G. PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Med. 2003;29:278–285. doi: 10.1007/s00134-002-1601-2. [DOI] [PubMed] [Google Scholar]
- 19.Pendergraft TB, Stanford RH, Beasley R, et al. Seasonal variation in asthma-related hospital and intensive care unit admissions. J Asthma. 2005;42:265–271. doi: 10.1081/jas-200057893. [DOI] [PubMed] [Google Scholar]
- 20.Dodek PM, Norena M, Keenan SP, et al. Intensive care unit admissions for community-acquired pneumonia are seasonal but are not associated with weather or reports of influenza-like illness in the community. J Crit Care. 2011;26:228–233. doi: 10.1016/j.jcrc.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 21.Cleves M. [Accessed May 14, 2015];Analysis of multiple failure-time survival data. 2009 Available from: http://www.stata.com/support/faqs/statistics/multiple-failure-time-data/
- 22.Wagner J, Gabler NB, Ratcliffe SJ, et al. Outcomes among patients discharged from busy intensive care units. Ann Intern Med. 2013;159:447–455. doi: 10.7326/0003-4819-159-7-201310010-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Czaja AS, Zimmerman JJ, Nathens AB. Readmission and late mortality after pediatric severe sepsis. Pediatrics. 2009;123:849–857. doi: 10.1542/peds.2008-0856. [DOI] [PubMed] [Google Scholar]
- 24.Czaja AS, Hosokawa PW, Henderson WG. Unscheduled readmissions to the PICU: epidemiology, risk factors, and variation among centers. Pediatr Crit Care Med. 2013;14:571–579. doi: 10.1097/PCC.0b013e3182917a68. [DOI] [PubMed] [Google Scholar]
- 25.Bernard AM, Czaja AS. Unplanned pediatric intensive care unit readmissions: a single-center experience. J Crit Care. 2013;28:625–633. doi: 10.1016/j.jcrc.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 26.Bastero-Miñón P, Russell JL, Humpl T. Frequency, characteristics, and outcomes of pediatric patients readmitted to the cardiac critical care unit. Intensive Care Med. 2012;38:1352–1357. doi: 10.1007/s00134-012-2592-2. [DOI] [PubMed] [Google Scholar]
- 27.Brittan MS, Sills MR, Fox D, et al. Outpatient follow-up visits and readmission in medically complex children enrolled in medicaid. J Pediatr. 2015;166:998–1005. doi: 10.1016/j.jpeds.2014.12.022. [DOI] [PubMed] [Google Scholar]
- 28.Cohen E, Berry JG, Camacho X, et al. Patterns and costs of health care use of children with medical complexity. Pediatrics. 2012;130:e1463–1470. doi: 10.1542/peds.2012-0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berry JG, Hall DE, Kuo DZ, et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children’s hospitals. JAMA. 2011;305:682–690. doi: 10.1001/jama.2011.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Feudtner C, Levin JE, Srivastava R, et al. How well can hospital readmission be predicted in a cohort of hospitalized children? A retrospective, multicenter study. Pediatrics. 2009;123:286–293. doi: 10.1542/peds.2007-3395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Edwards JD. Anticipatory guidance on the risks for unfavorable outcomes among children with medical complexity. J Pediatr. 2017;180:247–250. doi: 10.1016/j.jpeds.2016.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Auger KA, Mueller EL, Weinberg SH, et al. A Validated Method for Identifying Unplanned Pediatric Readmission. J Pediatr. 2016;170:105–112. doi: 10.1016/j.jpeds.2015.11.051. [DOI] [PubMed] [Google Scholar]
- 33.Huang X, Rosenthal MB. Transforming specialty practice--the patient-centered medical neighborhood. N Engl J Med. 2014;370:1376–1379. doi: 10.1056/NEJMp1315416. [DOI] [PubMed] [Google Scholar]
- 34.Berry JG, Toomey SL, Zaslavsky AM, et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013;309:372–380. doi: 10.1001/jama.2012.188351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khan A, Nakamura MM, Zaslavsky AM, et al. Same-Hospital Readmission Rates as a Measure of Pediatric Quality of Care. JAMA Pediatr. 2015;169:905–912. doi: 10.1001/jamapediatrics.2015.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chamberlain LJ, Chan J, Mahlow P, et al. Variation in specialty care hospitalization for children with chronic conditions in California. Pediatrics. 2010;125:1190–1199. doi: 10.1542/peds.2009-1109. [DOI] [PubMed] [Google Scholar]
- 37.Coller RJ, Klitzner TS, Saenz AA, et al. The Medical Home and Hospital Readmissions. Pediatrics. 2015;136:e1550–1560. doi: 10.1542/peds.2015-1618. [DOI] [PubMed] [Google Scholar]
- 38.Brittan M, Albright K, Cifuentes M, et al. Parent and Provider Perspectives on Pediatric Readmissions: What Can We Learn About Readiness for Discharge? Hosp Pediatr. 2015;5:559–565. doi: 10.1542/hpeds.2015-0034. [DOI] [PubMed] [Google Scholar]
- 39.Nilsson D. Psycho-social problems faced by “frequent flyers” in a pediatric diabetes unit. Soc Work Health Care. 2001;33:53–69. doi: 10.1300/j010v33n03_05. [DOI] [PubMed] [Google Scholar]
- 40.Berry JG, Ziniel SI, Freeman L, Kaplan W, et al. Hospital readmission and parent perceptions of their child’s hospital discharge. Int J Qual Health Care. 2013;25:573–581. doi: 10.1093/intqhc/mzt051. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Flowchart of included and excluded patients, admissions, and units.
Supplemental Figure 2. Distribution of unplanned readmissions within one year by time from PICU discharge. A) All unplanned readmissions. B) Unplanned readmissions during the same hospitalization. C) Unplanned readmissions during different hospitalizations.
Supplemental Figure 3. Cumulative incidences of PICU patients readmitted within year by specific chronic condition or condition categories. A) Patients with cardiac conditions. B) Patients with respiratory conditions. C) Patients with neurologic/neuromuscular conditions. D) Patients with oncologic conditions. E) Patients with GI, hematologic, or endocrinologic conditions. F) Patients with other conditions.
Supplemental Table 1. Reasons for admission


