Abstract
AIMS:
We hypothesized that if we control for food composition, caloric intake, light exposure, sleep schedule, and exercise, intermittent fasting would not influence the circadian pattern of melatonin. Therefore, we designed this study to assess the effect of intermittent fasting on the circadian pattern of melatonin.
METHODS:
Eight healthy volunteers with a mean age of 26.6 ± 4.9 years and body mass index of 23.7 ± 3.5 kg/m2 reported to the Sleep Disorders Center (the laboratory) on four occasions: (1) adaptation, (2) 4 weeks before Ramadan while performing Islamic intermittent fasting for 1 week (fasting outside Ramadan [FOR]), (3) 1 week before Ramadan (nonfasting baseline [BL]), and (4) during the 2nd week of Ramadan while fasting (Ramadan). The plasma levels of melatonin were measured using enzyme-linked immunoassays at 22:00, 02:00, 04:00, 06:00, and 11:00 h. The light exposure, meal composition, energy expenditure, and sleep schedules remained the same while the participants stayed at the laboratory.
RESULTS:
The melatonin levels followed the same circadian pattern during the three monitoring periods (BL, FOR, and Ramadan). The peak melatonin level was at 02:00 h and the trough level was at 11:00 h in all studied periods. Lower melatonin levels at 22:00 h were found during fasting compared to BL. Cosinor analysis revealed no significant changes in the acrophase of melatonin levels.
CONCLUSIONS:
In this preliminary report, under controlled conditions of light exposure, meal composition, energy expenditure, and sleep-wake schedules, intermittent fasting has no significant influence on the circadian pattern of melatonin.
Keywords: Circadian rhythm, fasting, light exposure, meals, Ramadan, sleep
The month of Ramadan, the 9th month of the Muslim lunar calendar, is a unique model of intermittent fasting, where people abstain from food and drink between dawn and sunset. Moreover, Ramadan is accompanied by several personal lifestyles and societal changes, including a delay in starting work, nocturnal prayers, and the opening of stores and shopping malls until predawn time.[1] Furthermore, habits and meal frequency and timing change during Ramadan, for example, some cultures prefer fried foods and consume an excessive amount of sweets.[1] Studies have shown that high fat and sugar intake can lead to changes in clock gene expression in the suprachiasmatic nucleus (SCN) and other peripheral brain nuclei (non-SCN brain nuclei).[2] During Ramadan, the usual circadian pattern of eating shifts suddenly, which results in an increase in caloric intake at night. The increased caloric intake at night has been proposed as a mechanism that possibly affects the circadian rhythm and results in a loss of the temporal control (circadian disruption) of metabolic processes during fasting,[3] given that the timing of meals and glucose levels have been shown to affect the circadian rhythm.[4,5,6]
The melatonin rhythm is one biological marker of circadian rhythmicity, which conveys messages to the body about the daily light/dark cycle.[7] Although several tissues in the body produce melatonin, the circulating neurohormone is derived almost exclusively from the pineal gland.[8] Melatonin is believed to be one of the best markers for circadian rhythm disruption because individual melatonin profiles are highly reproducible and are less affected by masking factors than are other markers of circadian rhythms, such as core body temperature or cortisol level.[9]
Two previous studies have suggested a shift delay in the peak of melatonin during Ramadan. However, neither study controlled for food intake, sleep/wake schedule, energy expenditure (exercise) nor the social habits that accompany Ramadan. In addition, there was no proper control for light exposure. Moreover, in both studies, the melatonin concentrations were not measured in the early morning, thus neglecting possible early morning peaks in melatonin concentration. Thus, whether Islamic intermittent fasting influences the circadian pattern of circulating melatonin remains undefined. We hypothesized that if we control for the above confounders, Ramadan daytime fasting will not influence the circadian pattern of circulating melatonin. Therefore, we designed the present study to assess the circadian pattern of plasma melatonin during and outside the Ramadan month while controlling for the sleep/wake schedule, sleep duration and quality, meal composition, energy expenditure, and light exposure.
Methods
Subjects
This study is a part of a research project to assess the effects of intermittent fasting on sleep architecture, circadian rhythm, hormonal changes, and different cellular biomarkers.[10,11] However, the current melatonin data have not been reported before. The study protocol has been described in details before.[10] Eight nonsmoking, healthy Muslim male volunteers between the ages of 20 and 35 years (weight = 69.1 ± 8.4 kg) provided written informed consent to participate in the study. Participants were informed of the project through advertising on bulletin boards in the university. The advertisement clearly stated that the volunteers were being recruited for research purposes. The selected volunteers were not on any medications, did not drink alcohol, did not perform shift work, and were not on vacation during the study period. None of the participants had sleep complaints or was on any dietary program. In addition, the selected volunteers were not practicing fasting as routine voluntary rituals before. Moreover, all participants have regular sleep/wake schedule and have morning chronotype confirmed by a validated Arabic version of the reduced Horne and Ostberg morningness–eveningness questionnaire.[12,13] The regularity of the sleep/wake schedule was assessed by wrist actigraphy monitoring (Philips/Respironics, Inc., Murrysville, Pennsylvania, USA) in all participants for 1 week (it was worn on the nondominant wrist). A regular sleep/wake schedule was defined as <1 h of daily variability in the bedtime and wake-up time.[10] None of the participants traveled 2 weeks prior to or during the study. Their work hours were from 07:30 to 16:30 h before Ramadan and from 10:00 to 15:00 h during Ramadan. The participants were instructed not to wear sunglasses during the study period.
The study protocol was approved by the College of Medicine Institutional Review Board at King Saud University, and written informed consent was obtained from the participants.
Study protocol
This study was performed during the last week of Rajab (month 7, Hijri), the first and last weeks of Shaban (month 8, Hijri), and the 2nd week of Ramadan (month 9, Hijri). The study period corresponded to the dates between June 25 and August 15, 2011, on the Gregorian calendar. Participants reported to the Sleep Disorders Center (the laboratory) on 4 occasions. During each visit, the participant spent 24 h at the laboratory and underwent overnight polysomnography (PSG) [Figure 1]:
Figure 1.
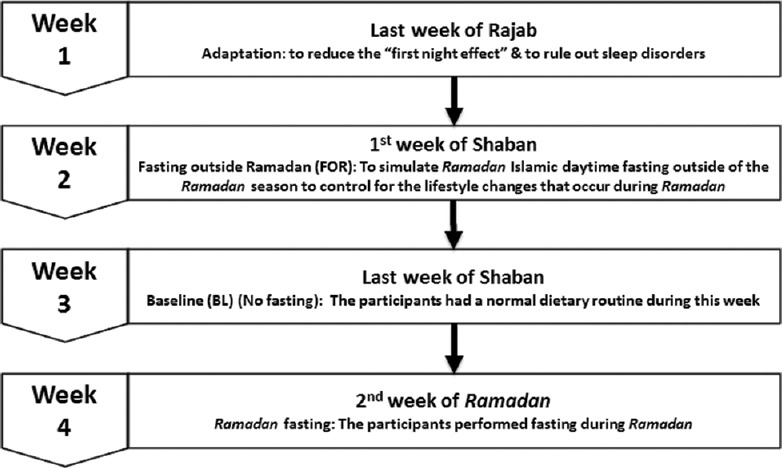
Study protocol
Initial visit
The participants came to their initial visit during the last week of Rajab (month 7, Hijri) to receive a medical checkup, to adapt to the sleeping environment and equipment, and to undergo an overnight sleep study (not included in the analysis) to reduce the “ first night effect”, which is known to affect the sleep architecture of the first night of PSG recording[14] and to rule out sleep disordered breathing. All the participants were given an actigraph to wear on their nondominant wrist, to wear at home to monitor their sleep/wake pattern.[15] The body weight was monitored during the study period.
Fasting outside Ramadan
This fasting period is not an element of the normal routine of religious Ramadan fasting. We introduced this protocol to simulate Ramadan Islamic daytime fasting outside of the Ramadan season to control for the lifestyle changes that occur during Ramadan, such as changes in the sleep/wake pattern, sleep duration, physical activity, and meal composition, which may influence melatonin secretion and circadian rhythmicity. This fasting period was completed 3 weeks before Ramadan to avoid any overlap with the baseline (BL) (nonfasting) or the Ramadan fasting and any carryover effects. The participants performed fasting for 7 days during the 1st week of the Shaban (month 8, Hijri). The participants reported to the laboratory for the last 24 h of the fasting week.
Baseline (nonfasting)
This visit occurred during the last week of the Shaban (month 8, Hijri) (BL without fasting). The participants had a normal dietary routine during this week and reported to the laboratory for the last 24 h of the week.
Ramadan (R)
This visit to the laboratory occurred during the last day of the 2nd week of Ramadan (month 9, Hijri) after fasting for 2 weeks.
The details of the protocol are described in previous publications.[10,11] Participants reported to the laboratory at approximately 18:00 h. During the laboratory stay, the participants received meals with fixed caloric intake (35 kcal/kg/24 h) based on their ideal body weight, and fixed proportions of carbohydrates, fats, and proteins. This was organized by a dietitian. Food items containing large amounts of 5-hydroxytryptamine or melatonin were avoided on the study nights and days.[16]
Meal timing
During BL, the participants had three meals: dinner at 20:00 h, breakfast at 07:15 h, and lunch at 12:00 h mid-day. During fasting outside Ramadan (FOR) and Ramadan, the participants had the following meals: breakfast (at sunset, between 18:30 and 18:55 h), dinner at 21:00 h, and suhur before dawn (between 03:00 and 03:15 h).
Blood specimen collection
On the day of admission to the laboratory, at 18:00 h, an intravenous cannula was placed in the antecubital vein for blood withdrawal. Blood samples were collected at 22:00, 02:00, 04:00, 06:00, and 11:00 h. The samples were immediately centrifuged at 4°C and stored at −70°C.
Fasting protocol
The fasting protocol has been described elsewhere.[10,11] During the FOR period, the participants were asked to fast for the 1st week of Shaban (7 days) to assess the effects of Islamic intermittent fasting in the absence of the lifestyle changes and eating habits that occur during Ramadan. During the following 3 weeks of Shaban, the participants maintained their routine activities and eating habits. The participants performed fasting during the month of Ramadan. During the FOR period, dawn (the beginning of fasting) occurred at approximately 03:37 h and sunset (the end of fasting) occurred at approximately 18:47 h, and during the 2nd week of Ramadan, dawn occurred at approximately 04:00 h and sunset occurred at approximately 18:34 h.
Polysomnography
A standard PSG recording was performed.[11] During PSG, the following parameters were monitored: four leads of electroencephalography (EEG) (EEG: C1-A4, C2-A3, O1-A4, and O2-A3), electrooculography, chin electromyography, electrocardiography, oxygen saturation, chest and abdominal wall movements, air flow (thermistor), and sleep position. Scoring was performed manually according to established scoring criteria.[17] The PSG recordings are described in a previous publication.[11]
The participants were asked to avoid any naps during the study day in the laboratory. During BL, the PSG recording began at 23:00 and was concluded at 07:00 h. During FOR and Ramadan, the PSG recording began at 23:00 h. During Ramadan, the participants had the suhur meal at 03:00 h, and the study was resumed from 03:45 until 07:45 h. During FOR, the participants had suhur at 03:15 h (to account for the shift in the dawn prayer time), and the study was resumed from 04:00 until 07:45 h. Alice 5 diagnostic equipment was used for data acquisition (Philips/Respironics, Inc., Murrysville, Pennsylvania, USA). The arousal index, which is a measure of sleep fragmentation, was defined as the number of arousals per 1 h of sleep. “Stage shifts” was defined as the total number of changes in sleep stage from lights out to lights on.
Light exposure in the laboratory
While in the laboratory, light exposure was controlled during the three study periods (BL, FOR, and Ramadan). From 18:00 h until bedtime, the light level was maintained at 50 lux. During the PSG recording, all lights were turned off and the light level was <1 lux. During suhur meal, light intensity was maintained <30 lux.[18] The light intensity was measured using SpectralStar Light Meter LX-1 (Japan).
Energy expenditure measurement
To control for the effect of exercise on melatonin secretion,[19] the energy expenditure was measured while the participants were at the laboratory using a SenseWear Pro Armband™ (Body Media, Pittsburgh, Pennsylvania, USA). The technical characteristics of the armband have been previously described.[20,21] Briefly, the armband is a small portable sensing device worn on the triceps of the right arm. The device provides information regarding the total energy expenditure and total sleep time. The sensors in the armband measure movements, skin temperature, galvanic skin response, and heat flux from the body. The measured physiological data were processed by advanced algorithms to calculate the total energy expenditure.[22] The accuracy of the armband has been validated in many studies and comparisons with double-labeled water and metabolic carts.[22,23,24]
Determination of melatonin levels
Plasma melatonin levels were determined by an enzyme-linked immunoassay (GenWay Biotech Inc., San Diego, California, USA). The limit of detection was 1.6 pg/mL, and the mean recovery was 102.4% (83%–125%). The intra-assay and inter-assay precision were 8.8–151.7 pg/mL and 5.6–134.3 pg/mL, respectively (the intra-assay and inter-assay coefficients of variation were 3.0%–11.4% and 6.4%–19.3%, respectively). The measurement procedure was carried out according to the manufacturer's instructions. During the blood sample collection, the illumination level was always <30 lux. The samples were constantly kept on ice and protected from light radiation to avoid melatonin degradation. All samples for melatonin were run in duplicate.
Statistical analysis
The data are expressed as the mean ± standard deviation. Energy expenditure was expressed as metabolic equivalents (METs). The average METs were calculated to obtain an overall hourly average for each day.
To obtain the best estimates of the overall acrophase for melatonin, we used a 24 h cosinor rhythmometry model 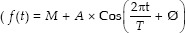 , where M = mesor; A = amplitude; Ø = acrophase, and T = 24 h.[25,26] The model was implemented for each participant's data during the three periods. Comparisons of the BL, FOR, and Ramadan fasting groups were performed using a repeated measures (RMs) ANOVA. When the normality test failed, Friedman's RM ANOVA on ranks test was used. Post hoc analyses were performed to determine the significant differences between individual groups. The results were considered statistically significant for P < 0.05. The data were analyzed using Statistical Package for Social Sciences (SPSS), IBM version 22 (SPSS Inc., Chicago, IL, USA) software.
, where M = mesor; A = amplitude; Ø = acrophase, and T = 24 h.[25,26] The model was implemented for each participant's data during the three periods. Comparisons of the BL, FOR, and Ramadan fasting groups were performed using a repeated measures (RMs) ANOVA. When the normality test failed, Friedman's RM ANOVA on ranks test was used. Post hoc analyses were performed to determine the significant differences between individual groups. The results were considered statistically significant for P < 0.05. The data were analyzed using Statistical Package for Social Sciences (SPSS), IBM version 22 (SPSS Inc., Chicago, IL, USA) software.
Results
The study group had a mean age of 26.6 ± 4.9 years and a body mass index of 23.7 ± 3.5 kg/m2. No differences were detected in body weight during the three study periods: 69.1 ± 8.4 kg, 67.5 ± 7.8 kg, and 66.3 ± 12.3 kg for BL, FOR, and Ramadan, respectively. Moreover, no differences were found in serum glucose measurements at 15:30 between BL, FOR, and Ramadan (6.1 ± 0.5, 5.7 ± 0.4, and 5.8 ± 0.5 mmol/L, respectively).
Table 1 shows the sleep pattern at home. There was a significant delay in bedtime and wake-up time during Ramadan due to the accompanying delay in the start time of work. No significant differences in bedtime and wake-up time were found between BL and FOR. No differences were detected between the nocturnal sleep duration and total sleep duration (nocturnal sleep and naps) among the three study periods.
Table 1.
Sleep pattern while at home
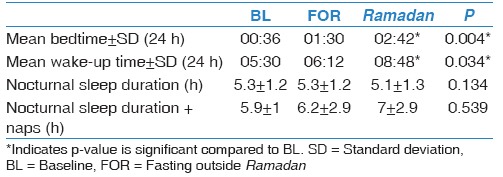
Table 2 shows the sleep parameters and the energy expenditure during monitoring in the laboratory. The sleep efficiency was relatively lower than normal (BL = 79.3% ±9.6%, FOR = 70.7% ±11.1%, and Ramadan = 74.2% ±7.3%), which could be related to the disruptive effect of blood collection. Otherwise, no changes were detected in sleep parameters. Energy expenditure was reported for 24 h (day and night), during the daytime (from dawn to sunset), and at night (sunset to dawn). No significant changes were found in energy expenditure during the three monitoring periods (BL, FOR, and Ramadan).
Table 2.
Sleep parameters and energy expenditure during monitoring at the Sleep Disorders Center (the laboratory)
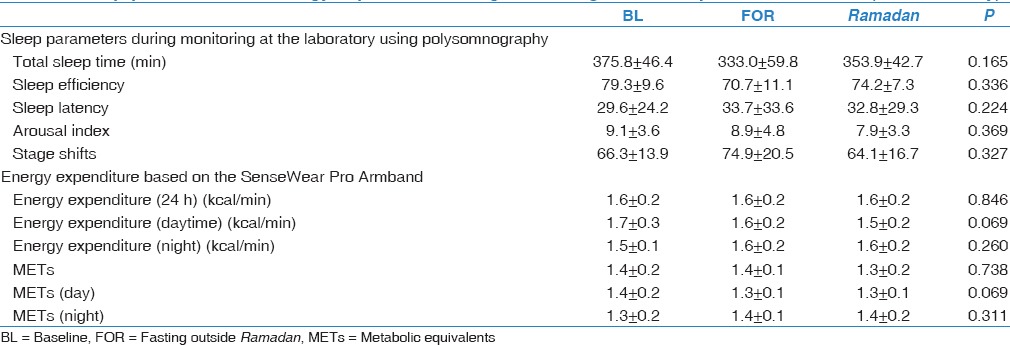
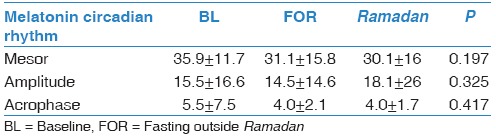
Figure 2 shows the pattern of melatonin concentrations during BL, FOR, and Ramadan fasting. Clearly, the melatonin levels followed the same circadian pattern during BL, FOR, and Ramadan. During the three study periods (BL, FOR, and Ramadan), the melatonin levels showed the same peak level at 02:00 h. The documented trough level was at 11:00 h in all studied periods (BL, FOR, and Ramadan). However, the plasma melatonin level at 22:00 h was lower during fasting (FOR and Ramadan) than at BL, with a significantly lower level for Ramadan versus BL (28 ± 18.7 pg/mL versus 25.7 ± 19.5 pg/mL, respectively, P < 0.05). Moreover, at 11:00 h, the melatonin levels were significantly higher during FOR than at BL (28 ± 18.7 pg/mL versus 25.7 ± 19.5 pg/mL, respectively, P < 0.05). Cosinor analysis of the melatonin plasma levels [Table 3] revealed no significant changes in the acrophase during the three periods.
Figure 2.
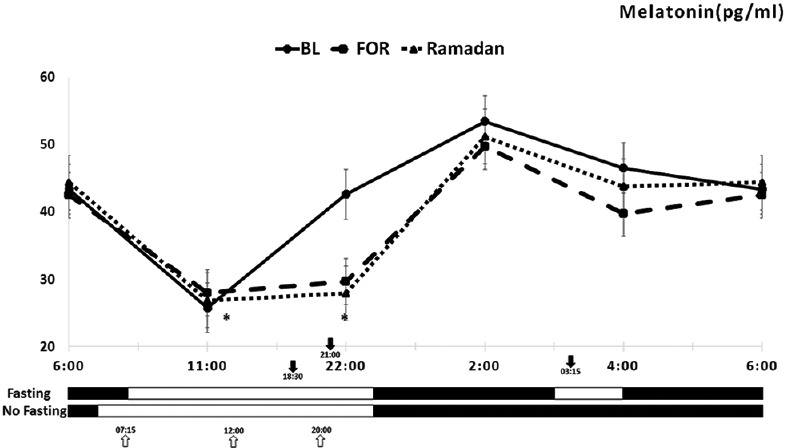
Circadian pattern of plasma melatonin concentrations in eight healthy male volunteers before and during Ramadan daytime fasting. Each point represents the mean and standard deviation of eight participants. Values at baseline ( ), baseline fasting before Ramadan (
), baseline fasting before Ramadan ( ), and Ramadan (-▴-) are presented. The dark-headed arrows indicate the meal time during fasting (Ramadan and baseline fasting), and the white-headed arrows indicate the meal time during baseline. (
), and Ramadan (-▴-) are presented. The dark-headed arrows indicate the meal time during fasting (Ramadan and baseline fasting), and the white-headed arrows indicate the meal time during baseline. ( ) indicates awake, and (
) indicates awake, and ( ) indicates sleep
) indicates sleep
Table 3.
Cosinor summary of plasma melatonin circadian rhythm during baseline, baseline fasting, and Ramadan
Discussion
Several lifestyle changes that accompany Ramadan fasting, such as changes in the sleep/wake pattern, sleep duration, physical activity, and meal composition, may influence melatonin secretion and circadian rhythmicity.[1,21,27,28] Indeed, current evidence shows that changes such as light exposure,[29] sleep/wake schedule and sleep duration,[29] meal composition,[16] and exercise[19] influence plasma melatonin levels. The present study was designed to assess the changes in the plasma levels of melatonin during intermittent fasting, while controlling for potential confounders that might affect the levels of the hormone, such as the sleep/wake schedule, sleep duration and quality, physical activity, light exposure, and meal composition. Moreover, to control for potential confounders that accompany the lifestyle changes during Ramadan, we assessed the effects of intermittent Islamic FOR. To our knowledge, this is the first study to assess the effects of intermittent Islamic fasting on melatonin plasma concentrations outside of the Ramadan season.
The main finding of this study is that melatonin levels followed the same circadian pattern during BL, FOR, and Ramadan, although there was a decrease at 22:00 h during the 2nd week of Ramadan compared to BL Figure 1. However, in our study, when a cosinor model was used; no shift delay was detected in the acrophase during the three periods.
During Ramadan, food and fluid intake are shifted to the hours of darkness, thus partially reversing the normal circadian pattern of eating and drinking. In theory, these changes could affect circadian rhythmicity in fasting individuals, with effects including changes in several hormone systems and the core body temperature.[1] A limited number of studies has objectively assessed the circadian rhythm changes during Ramadan, and the results suggested a shift delay in the circadian rhythmicity of body temperature.[3,21,30] In a well-designed study, Roky et al. continuously recorded body temperature for 24 h in six healthy participants during Ramadan using a rectal thermistor probe and reported delays in both the occurrence of the acrophase and bathyphase of body temperature (i.e., the times at which the calculated maximum and minimum values, respectively, occur in the cycle).[30] The shift delay in core body temperature was attributed to the shift to night time meals during Ramadan.[30] Whether a shift delay also occurs in the circadian rhythm of melatonin secretion remained unknown.
Theoretically, changes in the circadian pattern of body temperature during Ramadan should also be associated with alterations in the circadian pattern of melatonin secretion, although some studies suggested that shifting the meal time influences the core body temperature rhythm but not the melatonin rhythm.[31,32] To date, two studies have assessed melatonin secretion during Ramadan. In the first study, the plasma melatonin levels were measured in blood samples obtained every 4 h (omitting the 02:00 time point to avoid sleep disturbances) before and on the 23rd day of Ramadan.[33] The investigators reported a smaller and delayed night peak and a flatter slope in serum melatonin concentrations during Ramadan.[33] In the second study, saliva samples for melatonin were collected from eight healthy volunteers at three-time points over a 24 h period (08:00, 16:00, and 00:00) 1 week before Ramadan and on the 7th and 21st days of Ramadan.[28] A significant decrease in melatonin concentrations at 00:00 and 16:00 h was reported during Ramadan compared to BL levels; however, similar trends in melatonin profiles were observed during Ramadan but with a flatter slope.[28] A major limitation in those previous two studies was that melatonin was not measured in the early morning hours, which overlooks the possibility of a late peak in melatonin concentrations. Moreover, neither study properly controlled for differences in light exposure, sleep schedule, or the social habits that accompany Ramadan.
To overcome the shortcomings of these studies, we assessed circadian patterns in melatonin during intermittent fasting outside the month of Ramadan and during the 2nd week of Ramadan after controlling for light exposure, sleep schedule, sleep duration, and meal composition. A trough in melatonin levels was observed at 11:00 h and a peak at 02:00 h during all studied periods, which indicates that intermittent fasting has no significant influence on the circadian pattern of melatonin.
The current study concurs with the previous studies[28,33] in reporting lower nocturnal melatonin levels. In general, most studies consistently found a decrease in nocturnal melatonin concentrations during fasting, even during short-term experimental fasting.[34,35,36] Although the exact mechanisms involved in the reduction of melatonin levels during fasting are unknown, this finding could be related to the shift in meal time. In a study that assessed the effects of a single morning and evening carbohydrate-rich meal for 3 consecutive days on the circadian phase of salivary melatonin rhythms under controlled constant routine conditions in ten healthy participants, the nocturnal melatonin secretion after the last morning meal was elevated compared to that for the evening meal.[31] Another plausible mechanism is the rise in nocturnal cortisol levels during Ramadan, which could be associated with a drop in melatonin levels.[37,38] In addition, the decrease in melatonin synthesis could be due to a decrease in glucose supply.[39] The latter hypothesis is supported by findings showing that melatonin levels are decreased secondary to mild hypoglycemia and that glucose supplementation during fasting ameliorates the decrease in melatonin levels.[35] Nevertheless, hypoglycemia is not believed to occur in healthy individuals during Ramada n fasting.[28,40,41] Moreover, glucose level did not change significantly in the current study.
Although the present study was conducted under well-controlled conditions, the meal time during fasting periods could not be matched to the BL because the shift in meal time is an essential part of the religious practice during fasting. The effect of meal time on melatonin levels in humans remains undefined. Indeed, there are very few uncontrolled studies investigating the effects of meal timing on circadian rhythms in humans.[31] In shift workers, meal timing does not appear to be a strong synchronizer of circadian rhythms.[42] In fact, daily meal timing does not usually entrain circadian rhythms controlled by the SCN clock in the presence of the photic synchronizer.[43,44] In contrast to the peripheral organs, the SCN clock seems to be invulnerable to feeding time and remains in phase with the light–dark cycle.[45,46]
A number of limitations of the present study must be considered. An important one is the relatively small number of participants examined due to the time constraints of the study protocol. Nevertheless, small participant numbers are typical in studies that use objective continuous assessment methods under controlled conditions and must be conducted within a limited time (the month of Ramadan) as both of these factors limit the number of recruited volunteers.[10,21,28,30,31,33] Second, the fact that the participants were recruited within a university setting, which may limit how well the sample represents the general population since individuals in this group are more likely to be more educated than the general public. Third, females were not included as females have to break their fast while having menstruation.
Conclusion
Our investigation of plasma melatonin concentration in eight fasting participants during and before Ramadan revealed that under controlled conditions of light exposure, meals, and sleep-wake schedules, intermittent fasting does not significantly influence the circadian pattern of circulating melatonin. Larger studies are needed to assess the circadian pattern of melatonin during intermittent diurnal fasting while controlling for potential confounders.
Financial support and sponsorship
This work was supported by the Strategic Technologies Program of the National Plan for Sciences and Technology and Innovation in the Kingdom of Saudi Arabia (MED511-02-08).
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We are extremely grateful to the study participants who took the time from their busy schedules to participate in the study. Without their participation and feedback, this study would not have been possible.
References
- 1.Bahammam A. Does Ramadan fasting affect sleep? Int J Clin Pract. 2006;60:1631–7. doi: 10.1111/j.1742-1241.2005.00811.x. [DOI] [PubMed] [Google Scholar]
- 2.Oosterman JE, Kalsbeek A, La Fleur SE, Belsham DD. Impact of nutrients on circadian rhythmicity. Am J Physiol Regul Integr Comp Physiol. 2015;308:R337–50. doi: 10.1152/ajpregu.00322.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roky R, Iraki L, HajKhlifa R, Lakhdar Ghazal N, Hakkou F. Daytime alertness, mood, psychomotor performances, and oral temperature during Ramadan intermittent fasting. Ann Nutr Metab. 2000;44:101–7. doi: 10.1159/000012830. [DOI] [PubMed] [Google Scholar]
- 4.Hirota T, Okano T, Kokame K, Shirotani-Ikejima H, Miyata T, Fukada Y. Glucose down-regulates Per1 and Per2 mRNA levels and induces circadian gene expression in cultured Rat-1 fibroblasts. J Biol Chem. 2002;277:44244–51. doi: 10.1074/jbc.M206233200. [DOI] [PubMed] [Google Scholar]
- 5.Iwanaga H, Yano M, Miki H, Okada K, Azama T, Takiguchi S, et al. Per2 gene expressions in the suprachiasmatic nucleus and liver differentially respond to nutrition factors in rats. JPEN J Parenter Enteral Nutr. 2005;29:157–61. doi: 10.1177/0148607105029003157. [DOI] [PubMed] [Google Scholar]
- 6.Sherman H, Gutman R, Chapnik N, Meylan J, le Coutre J, Froy O. Caffeine alters circadian rhythms and expression of disease and metabolic markers. Int J Biochem Cell Biol. 2011;43:829–38. doi: 10.1016/j.biocel.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 7.Pandi-Perumal SR, Srinivasan V, Maestroni GJ, Cardinali DP, Poeggeler B, Hardeland R. Melatonin: Nature's most versatile biological signal? FEBS J. 2006;273:2813–38. doi: 10.1111/j.1742-4658.2006.05322.x. [DOI] [PubMed] [Google Scholar]
- 8.Zawilska JB, Skene DJ, Arendt J. Physiology and pharmacology of melatonin in relation to biological rhythms. Pharmacol Rep. 2009;61:383–410. doi: 10.1016/s1734-1140(09)70081-7. [DOI] [PubMed] [Google Scholar]
- 9.Miles A, Thomas R. Melatonin – A diagnostic marker in laboratory medicine? In: Miles A, Philbrick DR, Thompson C, editors. Melatonin: Clinical Perspectives. Oxford: Oxford University Press; 1988. pp. 253–79. [Google Scholar]
- 10.Alzoghaibi MA, Pandi-Perumal SR, Sharif MM, BaHammam AS. Diurnal intermittent fasting during Ramadan: The effects on leptin and ghrelin levels. PLoS One. 2014;9:e92214. doi: 10.1371/journal.pone.0092214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bahammam AS, Almushailhi K, Pandi-Perumal SR, Sharif MM. Intermittent fasting during Ramadan: Does it affect sleep? J Sleep Res. 2014;23:35–43. doi: 10.1111/jsr.12076. [DOI] [PubMed] [Google Scholar]
- 12.Adan A, Almirall H. Horne and östberg morningness-eveningness questionnaire: A reduced scale. Pers Individ Dif. 1991;12:241–53. [Google Scholar]
- 13.BaHammam AS, Almistehi W, Albatli A, AlShaya S. Distribution of chronotypes in a large sample of young adult Saudis. Ann Saudi Med. 2011;31:183–6. doi: 10.4103/0256-4947.78207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agnew HW, Jr, Webb WB, Williams RL. The first night effect: An EEG study of sleep. Psychophysiology. 1966;2:263–6. doi: 10.1111/j.1469-8986.1966.tb02650.x. [DOI] [PubMed] [Google Scholar]
- 15.Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003;26:342–92. doi: 10.1093/sleep/26.3.342. [DOI] [PubMed] [Google Scholar]
- 16.Peuhkuri K, Sihvola N, Korpela R. Dietary factors and fluctuating levels of melatonin. Food Nutr Res. 2012;56:1–9. doi: 10.3402/fnr.v56i0.17252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berry RB, Brooks R, Gamaldo CE, Harding SM, Lloyd RM, Marcus CL, et al. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, Version 2.1. Darien, Illinois: American Academy of Sleep Medicine; 2014. [Last accessed on 2017 Feb 05]. Available from: http://www.aasmnet.org . [Google Scholar]
- 18.Cajochen C, Zeitzer JM, Czeisler CA, Dijk DJ. Dose-response relationship for light intensity and ocular and electroencephalographic correlates of human alertness. Behav Brain Res. 2000;115:75–83. doi: 10.1016/s0166-4328(00)00236-9. [DOI] [PubMed] [Google Scholar]
- 19.Escames G, Ozturk G, Baño-Otálora B, Pozo MJ, Madrid JA, Reiter RJ, et al. Exercise and melatonin in humans: Reciprocal benefits. J Pineal Res. 2012;52:1–11. doi: 10.1111/j.1600-079X.2011.00924.x. [DOI] [PubMed] [Google Scholar]
- 20.Dorminy CA, Choi L, Akohoue SA, Chen KY, Buchowski MS. Validity of a multisensor armband in estimating 24-h energy expenditure in children. Med Sci Sports Exerc. 2008;40:699–706. doi: 10.1249/MSS.0b013e318161ea8f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.BaHammam A, Alrajeh M, Albabtain M, Bahammam S, Sharif M. Circadian pattern of sleep, energy expenditure, and body temperature of young healthy men during the intermittent fasting of Ramadan. Appetite. 2010;54:426–9. doi: 10.1016/j.appet.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 22.Malavolti M, Pietrobelli A, Dugoni M, Poli M, Romagnoli E, De Cristofaro P, et al. A new device for measuring resting energy expenditure (REE) in healthy subjects. Nutr Metab Cardiovasc Dis. 2007;17:338–43. doi: 10.1016/j.numecd.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 23.Johannsen DL, Calabro MA, Stewart J, Franke W, Rood JC, Welk GJ. Accuracy of armband monitors for measuring daily energy expenditure in healthy adults. Med Sci Sports Exerc. 2010;42:2134–40. doi: 10.1249/MSS.0b013e3181e0b3ff. [DOI] [PubMed] [Google Scholar]
- 24.Mackey DC, Manini TM, Schoeller DA, Koster A, Glynn NW, Goodpaster BH, et al. Validation of an armband to measure daily energy expenditure in older adults. J Gerontol A Biol Sci Med Sci. 2011;66:1108–13. doi: 10.1093/gerona/glr101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nelson W, Tong YL, Lee JK, Halberg F. Methods for cosinor-rhythmometry. Chronobiologia. 1979;6:305–23. [PubMed] [Google Scholar]
- 26.Cornelissen G. Cosinor-based rhythmometry. Theor Biol Med Model. 2014;11:16. doi: 10.1186/1742-4682-11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sadiya A, Ahmed S, Siddieg HH, Babas IJ, Carlsson M. Effect of Ramadan fasting on metabolic markers, body composition, and dietary intake in Emiratis of Ajman (UAE) with metabolic syndrome. Diabetes Metab Syndr Obes. 2011;4:409–16. doi: 10.2147/DMSO.S24221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.BaHammam A. Effect of fasting during Ramadan on sleep architecture, daytime sleepiness and sleep pattern. Sleep Biol Rhythms. 2004;2:135–43. [Google Scholar]
- 29.Cajochen C, Jewett ME, Dijk DJ. Human circadian melatonin rhythm phase delay during a fixed sleep-wake schedule interspersed with nights of sleep deprivation. J Pineal Res. 2003;35:149–57. doi: 10.1034/j.1600-079x.2003.00072.x. [DOI] [PubMed] [Google Scholar]
- 30.Roky R, Chapotot F, Hakkou F, Benchekroun MT, Buguet A. Sleep during Ramadan intermittent fasting. J Sleep Res. 2001;10:319–27. doi: 10.1046/j.1365-2869.2001.00269.x. [DOI] [PubMed] [Google Scholar]
- 31.Kräuchi K, Cajochen C, Werth E, Wirz-Justice A. Alteration of internal circadian phase relationships after morning versus evening carbohydrate-rich meals in humans. J Biol Rhythms. 2002;17:364–76. doi: 10.1177/074873040201700409. [DOI] [PubMed] [Google Scholar]
- 32.Johnston JD. Physiological responses to food intake throughout the day. Nutr Res Rev. 2014;27:107–18. doi: 10.1017/S0954422414000055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bogdan A, Bouchareb B, Touitou Y. Ramadan fasting alters endocrine and neuroendocrine circadian patterns. Meal-time as a synchronizer in humans? Life Sci. 2001;68:1607–15. doi: 10.1016/s0024-3205(01)00966-3. [DOI] [PubMed] [Google Scholar]
- 34.Michalsen A, Schlegel F, Rodenbeck A, Lüdtke R, Huether G, Teschler H, et al. Effects of short-term modified fasting on sleep patterns and daytime vigilance in non-obese subjects: Results of a pilot study. Ann Nutr Metab. 2003;47:194–200. doi: 10.1159/000070485. [DOI] [PubMed] [Google Scholar]
- 35.Röjdmark S, Wetterberg L. Short-term fasting inhibits the nocturnal melatonin secretion in healthy man. Clin Endocrinol (Oxf) 1989;30:451–7. doi: 10.1111/j.1365-2265.1989.tb00445.x. [DOI] [PubMed] [Google Scholar]
- 36.Bahammam A. Effect of fasting during Ramadan on sleep architecture, daytime sleepiness and sleep pattern. Sleep Biol Rhythms. 2004;2:135–43. [Google Scholar]
- 37.al-Hadramy MS, Zawawi TH, Abdelwahab SM. Altered cortisol levels in relation to Ramadan. Eur J Clin Nutr. 1988;42:359–62. [PubMed] [Google Scholar]
- 38.Sliman NA, Ajlouni KS, Faisal K. Effect of fasting on some blood hormones in healthy Muslim males. Mutah J Res Stud. 1993;8:91–109. [Google Scholar]
- 39.Chik CL, Ho AK, Brown GM. Effect of food restriction on 24-h serum and pineal melatonin content in male rats. Acta Endocrinol (Copenh) 1987;115:507–13. doi: 10.1530/acta.0.1150507. [DOI] [PubMed] [Google Scholar]
- 40.Azizi F. Research in Islamic fasting and health. Ann Saudi Med. 2002;22:186–91. doi: 10.5144/0256-4947.2002.186. [DOI] [PubMed] [Google Scholar]
- 41.Ajabnoor GM, Bahijri S, Borai A, Abdulkhaliq AA, Al-Aama JY, Chrousos GP. Health impact of fasting in Saudi Arabia during Ramadan: Association with disturbed circadian rhythm and metabolic and sleeping patterns. PLoS One. 2014;9:e96500. doi: 10.1371/journal.pone.0096500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Reinberg A. Chronobiology and nutrition. In: Reinberg A, Smolensky MH, editors. Biological Rhythms and Medicine: Cellular, Metabolic, Physiologic, and Pharmacologic Aspects. New York: Springer-Verlag; 1983. pp. 265–300. [Google Scholar]
- 43.Marchant EG, Mistlberger RE. Anticipation and entrainment to feeding time in intact and SCN-ablated C57BL/6j mice. Brain Res. 1997;765:273–82. doi: 10.1016/s0006-8993(97)00571-4. [DOI] [PubMed] [Google Scholar]
- 44.Challet E, Mendoza J. Metabolic and reward feeding synchronises the rhythmic brain. Cell Tissue Res. 2010;341:1–11. doi: 10.1007/s00441-010-1001-9. [DOI] [PubMed] [Google Scholar]
- 45.Inouye SI. Restricted daily feeding does not entrain circadian rhythms of the suprachiasmatic nucleus in the rat. Brain Res. 1982;232:194–9. doi: 10.1016/0006-8993(82)90625-4. [DOI] [PubMed] [Google Scholar]
- 46.Wakamatsu H, Yoshinobu Y, Aida R, Moriya T, Akiyama M, Shibata S. Restricted-feeding-induced anticipatory activity rhythm is associated with a phase-shift of the expression of mPer1 and mPer2 mRNA in the cerebral cortex and hippocampus but not in the suprachiasmatic nucleus of mice. Eur J Neurosci. 2001;13:1190–6. doi: 10.1046/j.0953-816x.2001.01483.x. [DOI] [PubMed] [Google Scholar]


