Abstract
Background
Pulmonary contusion (PC) is the most frequent blunt chest injury which could be used to identify patients at high-risk of clinical deterioration. We aimed to investigate the clinical correlation between PC volume and outcome in patients with blunt chest trauma (BCT).
Material/Methods
BCT patients with PC were identified retrospectively from the prospectively collected trauma registry database over a 2-year period. Contusion volume was measured and expressed as percentage of total lung (CTCV) volume using three-dimensional reconstruction of thoracic CT images on admission. Data included patients’ demographics, mechanism of injury (MOI) and injury severity, associated injuries, CTCV, mechanical ventilation, complications, and mortality.
Results
A total of 226 BCT patients were identified to have PC with a mean age of 35.2 years. Motor vehicle crash (54.4%) and falls (16.4%) were the most frequent MOIs. Bilateral PC (61.5%) was more prevalent than right-sided (19.5%) and left-sided PC (19%). CTCV had a significant positive correlation with ISS; whereas, age and PaO2/FiO2 ratio showed a negative correlation (p<0.05 for all). The median CTCV was significantly higher in patients who developed in-hospital complications (p=0.02). A CTCV >20% was associated with increasedrisk of acute respiratory distress syndrome (ARDS), blood transfusion and prolonged mechanical ventilation. However, multiple linear regression analysis showed that CTCV alone was not an independent predictor of in-hospital outcomes. Presence of chest infection, CTCV, and Injury Severity Scores were predictors of ARDS.
Conclusions
Quantifying pulmonary contusion volume could allow identification of patients at high-risk of ARDS. CTCV has a significant correlation with injury severity in patients with BCT. Further prospective studies are needed to address the validity of CTCV in the patients care.
MeSH Keywords: Blunt Trauma; Chest Injuries; Lung Contusions; Lung Volume, Multidetector Computed Tomography
Background
Blunt chest trauma (BCT) causing structural damage to the thoracic region is associated with substantial morbidity and mortality, especially in polytrauma patients [1]. Pulmonary contusion (PC) is the most frequent chest injury (25–80%) with significant mortality (10–20%) in severely injured patients [2,3]. Therefore, patients who sustained significant blunt thoracic injuries are anticipated to have PC [4]. Motor vehicle crashes (MVCs) are the major cause of blunt thoracic trauma resulting in PC [5]. Crash parameters indicating higher severity are correlated well with the risk of developing PC [2].
Plain chest radiograph is a conventional tool to detect PC, and is limited by the possibility of delayed appearance of the characteristic injury findings [6]. Also, it fails to diagnose, or underestimates, the size of the PC which misleads the actual clinical picture [7]. A recent meta-analysis suggested ultrasonography to be a better screening tool for the diagnosis of PC but with inaccurate quantification [3]. Computed tomography (CT) is the modality of choice to diagnose and quantify PC volume (CTCV) in chest trauma patients [8]. An earlier study demonstrated prognostic implications of a novel CT volume index score in polytrauma patients with PC [9]. It has been suggested that patients with CTCV scores >20% of total lung volume are at increased risk for developing pulmonary complications. Therefore, this score can be used for risk-stratification and early management in subsets of chest trauma patients identified to be at higher risk of these complications. Accurate measurement of contusion volume helps in predicting patients at increased risk of developing acute respiratory distress syndrome (ARDS) [10]. These findings argue for the clinical implications of contusion volume in identifying patients at increased risk of clinical deterioration. Therefore, we aimed to investigate the clinical correlation between PC volume and outcome in patients with BCT.
Material and Methods
It is a retrospective analysis of all BCT patients with PC identified from the trauma registry database at Hamad General Hospital, the only Level I trauma center in the state of Qatar between 2012 and 2014. Data included demographics, initial vitals, base deficit, serum lactate, chest abbreviated injury scale (AIS), chest tube insertion, intubation, long bone fracture, polytrauma, blood transfusion, affected lung(s), lung contusion volume, injury severity score (ISS), chest infection, acute respiratory distress syndrome (ARDS), ventilatory days, intensive care unit (ICU), and hospital length of stay (LOS) and mortality. The in-hospital outcomes measures included mechanical ventilation, duration of ICU and hospital length of stay, and complications (chest infection and/or ARDS and/or mortality).
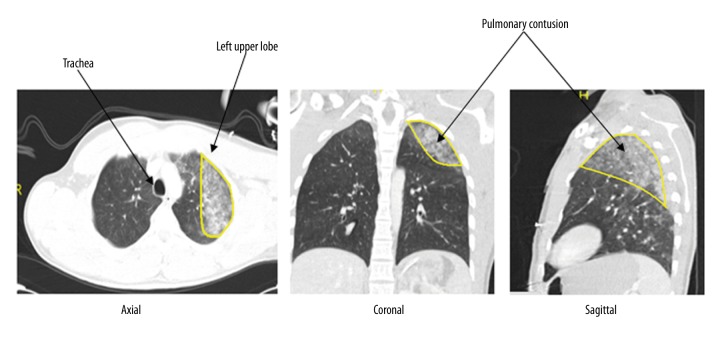
CT volume was calculated based on the ratio of contused lung to the total lung volume, to measure the volume of lung contusion. The detection and quantification of PC was based on CT scan evaluation performed by a consultant radiologist. Trauma patients with suspected thoracic and abdominal injury were scanned using a Siemens Somatom 64-slice CT scanner (Siemens Health Services, Erlangen, Germany) after administration of intravenous contrast. Images were evaluated in soft tissue, lung, and bone windows for assessment of injury. Pulmonary contusions appeared as areas of lung consolidation. Three-dimensional volumetric analysis of the data was performed on the workstation (Figure 1). The total lung volume and volume of each contusion was calculated. The total volume of lung contusions in both lungs was then calculated and expressed as a percentage of the lung volume. Moreover, chest x-ray was performed according to ATLS algorithm for management of trauma patients. Blood transfusion was performed in hemodynamically unstable patients as per the discretion of the treating physician. It was considered an indication of hemorrhagic shock, if an unstable patient did not respond to the initial two liters of normal saline.
Figure 1.
Thoracic computed tomography scan showing pulmonary contusion in left lung.
Polytrauma was defined as ISS of greater than 15 points, AIS score of three or greater in at least two body regions and at least one of five standardized pathologic conditions: hypotension (systolic blood pressure ≤90 mm Hg), unconsciousness (GCS score ≤8), acidosis (BE ≤–6.0), coagulopathy (PTT ≥40 seconds or INR ≥1.4), and age (≥70 years) [11].
Pulmonary complications were defined as the development of respiratory tract infection, empyema, or ARDS. The diagnosis of chest infection(pneumonia) was confirmed by positive culture of sputum and/or the combination of fever, leukocytosis and a suspected infiltrate on chest x-ray. ARDS was defined according to the Berlin modification of the American European Consensus [12] which includes acute onset of known clinical insult (within one week), PaO2/FiO2 ratio of less than 300 mm Hg with with a minimum of 5cm H2O PEEP, bilateral opacities on chest radiograph, and respiratory failure not fully explained by heart failure or fluid overload.
Pulmonary or lung contusion is an entity involving injury to the alveolar capillaries, without any tear or cut in the lung tissue which results in collection of blood and other fluids within the pulmonary tissue [13]. A previous study showed a critical contusion volume (>20%) of total lung volume to be considered as the maximally sensitive and specific screening value for the development of complications [9]. Therefore, we categorized contusion volume into two groups as CTCV <20% and CTCV ≥20%.
Patients with lung atelectasis were excluded from the study and no CT scan measure was taken into consideration. Atelectasis can be distinguished from lung contusion radiologically by CT scan [14,15]. The ratio between the arterial, oxygenation pressure (PaO2) and the fraction of inspired oxygen (FiO2) were calculated to reflect the functional status on oxygenation (PaO2/FiO2 ratio). In this calculation, the PaO2 was used from the first arterial blood sample obtained during initial evaluation in the resuscitation room. The FiO2 was determined depending on the intubation status. For intubated patients, a FiO2 of 1.0 was used, because of routine oxygenation with 100% O2 in the emergency department. For non-intubated patients a FiO2 of 0.60 was used, because of routine oxygenation with a non-rebreathing mask, using 10 to 15 L O2 per minute. This study was approved by the Medical Research Center (IRB# 13331/13) at Hamad Medical Corporation, Doha, Qatar.
Statistical analysis
The data were presented as proportions for categorical variables, and medians (range), or mean ± standard deviation (SD) for continuous variables. Correlations between CTCV score and outcomes were made using univariate and multivariate analysis to investigate whether CTCV score could predict outcomes in trauma patients. Univariate Pearson’s correlation analysis was performed between continuous predictor variables (CTCV, age, ISS, and PaO2/FiO2 ratio) and continuous outcome variables (hospital LOS, ICU LOS, and ventilator days). The correlation between contusion volumes and pooled outcomes (chest infection, ARDS and/or mortality) were analyzed using side-by-side box plots. Receiver operating curve (ROC) analysis was performed for contusion volume to predict in-hospital outcomes.
Differences between categorical variables (i.e., chest infection, ARDS, and mortality) among the two groups were analyzed using chi-square test. For continuous variables, Student t-test (i.e., hospital LOS, ICU LOS, and ventilator days) was used and nonparametric Mann-Whitney U test was performed for skewed variables. A two-tailed p value of <0.05 was considered significant.
A multiple linear regression analysis was performed for continuous in-hospital outcomes i.e., hospital LOS, ICU LOS, and ventilator days after adjusting for age, CTCV, PaO2/FiO2 ratio, chest AIS, chest infection, chest tube insertion, bilateral contusion, polytrauma, injury severity score (ISS) and ARDS. Another regression analysis was performed for the development of ARDS after adjusting for the potential confounders (age, PF ratio, chest AIS, chest infection, polytrauma, pulmonary contusion volume, bilateral contusion, and ISS). Data analysis was carried out using the Statistical Package for the Social Sciences version 18 (SPSS, Inc., Chicago, IL USA). Post hoc power analysis was conducted using the software package G*Power 3.0.10 for multiple regression analysis.
Results
Overall patients characteristics
Of the total 500 blunt chest trauma patients admitted to HGH, 226 (45.2%) were identified to have pulmonary contusion by thoracic CT scan (CTCV) with a mean age of 35.2±13.1 years and 93% of them were males (Table 1). Motor vehicle crash (54.4%), fall from height (16.4%), and pedestrian-traffic accidents (15.5%) were the most frequent mechanisms of injury. One hundred eighty-four patients (81.4%) sustained polytrauma and 79 (35.3%) had long bone fractures. None of the patient underwent thoracotomy. The mean ISS was 20.5±10.4 and chest AIS was 2.97±0.95. Transfusion of packed red blood cells was needed in 76 (33.6%) cases and chest tube was placed in 77 (34.4%) patients.
Table 1.
Demographics, presentation and outcome of chest injury patients with lung contusion (n=226).
| Variable | Data |
|---|---|
| Age (mean ±SD) | 35.2±13.1 |
| Males (%) | 211 (93.4%) |
| Oxygen saturation, PO2 | 173±109 |
| PaO2/FiO2 ratio | 253.8±150.4 |
| Lactate (mean ±SD) | 3.2±1.8 |
| Base deficit (mean ±SD) | 5.16±3.8 |
| Intubation (%) | 100 (44.2%) |
| Chest Abbreviated Injury Score (AIS) (mean ±SD) | 2.97±0.95 |
| Long bone fracture (%) | 79 (35.3%) |
| Chest tube insertion | 77 (34.4%) |
| Polytrauma | 184 (81.4%) |
| Blood transfusion (%) | 76 (33.6%) |
| Lung contusion | |
| Right-side | 44 (19.5%) |
| Left-side | 43 (19.0%) |
| Bilateral | 139 (61.5%) |
| Lung contusion volume (%) | 7.1 (0.2–59.5) |
| Injury severity score (mean±SD) | 20.5±10.4 |
| Chest infection | 49 (21.7%) |
| Acute respiratory distress syndrome | 28 (12.4%) |
| Ventilatory day (median, range) | 8 (1–32) |
| Intensive care unit stay in days, (median, range) | 7 (1–57) |
| Hospital stay (days) | 10 (1–144) |
| Mortality | 15 (6.6%) |
Intubation and mechanical ventilation was required in 100 (44.2%) subjects, of them 68 had severe head injury, 10 had respiratory distress with oxygen desaturation despite supplemental oxygen, 14 required general anesthesia for abdominal surgery or orthopedic procedures, and 8 were intubated for airway protection for maxillofacial injuries.
On CT evaluation, 61.5% of cases showed bilateral lung contusion, 19.5% identified with right-sided contusion, and 19% had left-sided contusion. The median percentage of CTCV was 7.1 (0.2–59.5) and 42 (18.6%) cases had critical contusion volume (CTCV ≥20%). The median mechanical ventilation was 8 (1–32) days, ICU stay was 7 (1–57) days and the hospital stay was 10 (1–144) days.
Chest infection was observed in 49 (21.7%) cases. Sputum culture revealed gram-negative microorganisms in 41 cases (11 cases had Klebsiella pneumoniae, three case has Enerobacter cloacaents, two had Pseudomonas, seven had Hemophilus influenza, six had Acinetobacter baumannii, four had Moraxella catarrhalis and eight had other infectious agents) and gram-positive cocci were identified in eight cases (six had Staphylococcus and two had Streptococcus).
In-hospital outcomes
ARDS developed in 28 (12.4%) patients and the mortality rate was 6.6% (15 patients) which mainly constituted head injury (13 cases) and multiorgan failure (2 cases). Table 2 demonstrates a univariate correlation analysis for in-hospital outcomes. With respect to CTCV, a significant positive correlation was observed with ISS whereas, CTCV had a negative correlations with PF ratio (r=–0.283, p=0.001) and age (−0.187, p=0.005).
Table 2.
Univariate correlation analysis for in-hospital outcomes.
| Parameters | Pearson’s correlation (r) | p-value |
|---|---|---|
| CTCV vs. age | −0.187 | 0.005 |
| CTCV vs. injury severity score | 0.210 | 0.002 |
| CTCV vs. PF ratio | −0.283 | 0.001 |
| CTCV vs. intensive care LOS | 0.167 | 0.060 |
| CTCV vs. hospital LOS | 0.074 | 0.277 |
| CTCV vs. ventilatory days | 0.154 | 0.140 |
| PF ratio vs. injury severity score | −0.320 | 0.001 |
| PF ratio vs. intensive care LOS | −0.348 | 0.001 |
| PF ratio vs. hospital LOS | −0.242 | 0.002 |
| PF ratio vs. ventilatory days | −0.251 | 0.023 |
| ISS vs. intensive care LOS | 0.348 | 0.001 |
| ISS vs. hospital stay | 0.367 | 0.001 |
CTCV – computed tomography based contusion volume; LOS – length of stay; PF ratio – PaO2/FiO2 ratio.
Moreover, ISS, ventilatory days, ICU and hospital LOS showed significant negative correlation with PF ratio (p<0.05 for all). Mean ISS had significant positive correlation with ICU and hospital LOS (p=0.001).
The mean CTCV was highest in patients with severe PF ratio (15.6, range 1.9–59.5, p=0.001) as compared to moderate PF ratio (8.5, range 1.6–40.2) and mild PF ratio (5.8, range 0.2–55.9), p=0.001 (Figure 2). CTCV was significantly higher in patients who developed complications (chest infection, ARDS and/or mortality): [10 (range 0.5–59.5) vs. 6.3 (range 0.2–52.3); p=0.02] than those who did not have complications (Figure 3).
Figure 2.
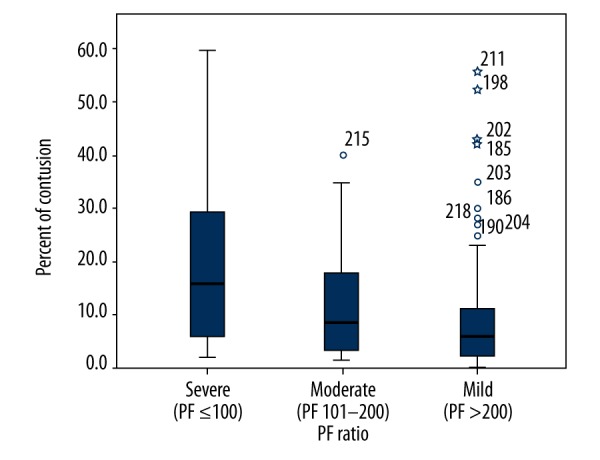
Lung contusion volume (CTCV) and severity of PF ratio (p=0.001).
Figure 3.
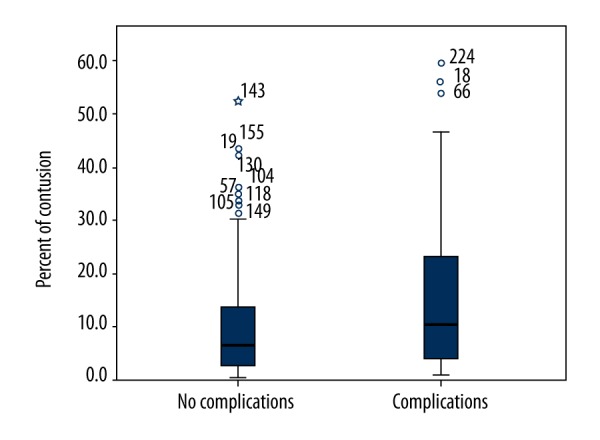
Comparison of lung contusion volumes (CTCV) with outcomes (chest infection, ARDS and/or mortality) in chest trauma patients.
A multiple linear regression analysis was performed for continuous in-hospital outcomes i.e., hospital LOS, ICU LOS, and ventilator days after adjusting for age, CTCV, PaO2/FiO2 ratio, chest AIS, chest infection, polytrauma, ISS, and ARDS (Table 3). A model using ARDS, chest infection, ISS, and polytrauma correlated with total hospital LOS (r2=0.251, p=0.001), ICU LOS (R2=0.524, p=0.001) and ventilator days (R2=0.434, p=0.001) (Table 3).
Table 3.
Multiple regression analysis* for the predictors of in-hospital outcomes.
| Significant predictors | p values | R2 | |
|---|---|---|---|
| Hospital LOS | Chest infection | 0.002 | 0.251 (P=0.001) |
| ISS | 0.013 | ||
| Hospital LOS=7.24+16.48 (chest infection) +0.58 (ISS) | |||
| Intensive care unit (ICU) LOS | Chest infection | 0.001 | 0.524(P=0.001) |
| ISS | 0.011 | ||
| Polytrauma | 0.034 | ||
| ICU LOS=15.24+10.13 (chest infection) –11.29 (polytrauma) +0.29 (ISS) | |||
| Ventilatory days | Chest infection | 0.001 | 0.434 (P=0.001) |
| ARDS | 0.014 | ||
| Ventilatory days=8.96+6.04 (chest infection) +4.85 (ARDS) | |||
ISS – injury severity score; ARDS – acute respiratory distress syndrome; LOS – length of stay; R – multiple correlation coefficient;
A multiple linear regression was performed for continuous in-hospital outcomes i.e. hospital LOS, ICU LOS, and ventilator days after adjusting for age, CTCV, PaO2/FiO2 ratio, chest AIS, chest infection, chest tube insertion, bilateral contusion, polytrauma, ISS and ARDS.
Lung contusion volume, chest infection, and ISS were predictors of the development of ARDS in another logistic regression analysis (Table 4).
Table 4.
Multivariate analysis for the predictors of ARDS in chest trauma patients.
| Variables | Odd ratio | 95% CI | p-value |
|---|---|---|---|
| Age | 1.02 | 0.96–1.04 | 0.44 |
| PF ratio | 1.00 | 0.99–1.00 | 0.37 |
| Chest abbreviated injury scores | 0.53 | 0.17–1.66 | 0.28 |
| Chest infection | 25.0 | 4.02–155.4 | 0.001 |
| Polytrauma | 0.66 | 0.05–7.90 | 0.75 |
| Pulmonary contusion volume | 1.08 | 1.02–1.14 | 0.006 |
| Bilateral contusion | 1.52 | 0.21–10.87 | 0.67 |
| Injury Severity score | 1.09 | 1.01–1.19 | 0.02 |
Table 5 shows the subgroup analysis for the association of CTCV with the outcomes measures. Development of ARDS (28.6% vs. 8.7%; p=0.001) and blood transfusion administration (52.4% vs. 29.3%; p=0.004) were significantly higher in patients with critical contusion volume (CTCV ≥20%) than those with CTCV <20%. Similarly, prolonged mechanical ventilation was needed in patients with CTCV ≥20% [13 (range 1–25) vs. 7 (range 1–32); p=0.04].
Table 5.
Comparison of pulmonary contusion volume and complications.
| CTCV <20% (n=184) | CTCV ≥20% (n=42) | p-value | |
|---|---|---|---|
| Blood transfusion | 54 (29.3%) | 22 (52.4%) | 0.004 |
| Chest infection | 37 (20.1%) | 12 (28.6%) | 0.23 |
| ARDS | 16 (8.7%) | 12 (28.6%) | 0.001 |
| Hospital LOS | 10 (1–144) | 12.5 (1–126) | 0.43 |
| Intensive care LOS | 6.5 (1–57) | 11 (1–57) | 0.25 |
| Ventilatory days | 7 (1–32) | 13 (1–25) | 0.04 |
| Mortality | 11 (6.0%) | 4 (9.5%) | 0.40 |
CTCV – computed tomography based contusion volume; ARDS – acute respiratory distress syndrome; LOS – length of stay.
Discussion
This is a unique study from the Arab Middle East region that focuses on the clinical correlation of PC measurement with the outcome in patients with BCT. The key finding of the present study is the positive correlation between CTCV, injury severity, and complications. This finding is consistent with an earlier study which observed that patients with higher CTCV were at an increased risk of short term complications [9]. PC secondary to BCT occurs frequently in polytrauma patients, which leads to adverse hospital outcomes [16]. Identification of high-risk patients for pulmonary complications in terms of pneumonia and ARDS after thoracic trauma is crucial for early risk-stratification, preventive measures and management. In this regard, early accurate quantification of PC has a clinical favorable implication in severe BCT [9,16,17].
Wang et al. [16] demonstrated that the admission PaO2/FiO2 and CTCV could reflect the PC degree and overall injury severity. In our series, CTCV showed a negative correlation with PaO2/FiO2 ratio. Based on these findings, lower PaO2/FiO2 ratio and higher CTCV percentage are proportional to the severity of injury. In addition, we observed a negative correlation of PaO2/FiO2 ratio with ISS, mechanical ventilation, and ICU stay which highlights the association of a lower PaO2/FiO2 ratio with a higher ISS and worse hospital outcomes.
In our study, 61.5% cases had bilateral contusion and the median CTCV was significantly higher in patients who developed hospital complications. CTCV alone was not an independent predictor of in-hospital outcomes. In contrast, an earlier study demonstrated a significant correlation of contusion volume with prolonged ICU stay on multivariate analysis [9]. These authors observed that the complications such as pneumonia and ARDS had a significant additive effect on the multivariate model. In our series, chest infection and injury severity score played a contributory role to increase hospital length of stay on the multivariate model. It has been suggested that in spite of advanced pulmonary management in ICU, PC is often associated with increased morbidity and morbidity due to associated polytrauma [13].
We also identified chest infection, injury severity score, and polytrauma to be associated with ICU length of stay. These results indicated that appropriate management of trauma patients together with active measures to prevent pulmonary complications may have a significant impact in reducing ICU stays which result in better utilization of hospital resources [18].
Only a few published studies have evaluated the association of CTCV and in-hospital outcomes in chest trauma patients. Miller et al. [10] reported that patients with CTCV >20% had four-fold higher rate of ARDS, suggesting that volumetric analysis of thoracic CT scans may allow identification of patients at high-risk for respiratory decompensation. Similarly, Strumwasser et al. [9] reported that the higher CTCV scores predicted prolonged ICU stay across all sizes of PC and also CTCV greater than 20% of total lung volume specifically identified patients at risk for developing complications. Consistent with these reports, our findings suggested that in addition to prolonged mechanical ventilation, patients who have CTCV >20% are at increased risk of developing ARDS. Moreover, PaO2/FiO2 ratios were lower in the severe contusion group. In addition, there was a significant increase in the frequency of ARDS at CTCV >20% which could be related to the degree of parenchymal disruption and subsequent shunt. With improvement in the understanding of the role of inflammatory mediators in PC, it has become clear that pulmonary dysfunction could be associated with cytokine release as well as mechanical damage to the lungs. This could explain in part the relationship between PC and ARDS, which has been well described. It could be speculated that the sharp increase in ARDS with CTCV >20% could be a function of cytokine release reaching a threshold level necessary to cause ARDS.
Hamrick et al. [19] found that the need for mechanical ventilation and duration of ventilator support correlated with the contusion volume >20% of total lung volume and could be used to identify high-risk patients required early ventilatory support for improved hospital outcomes. An earlier study by Tyburski et al. [20] quantified the PC and identified factors which were correlated with the size of PC. The authors observed that severe PC scoring (i.e., 10–18 scores) correlated with lower PaO2: FiO2 ratio, prolonged hospital length of stay, and higher ISS. In contrast, our study showed that contusion volume did not independently predict total hospital LOS, ICU LOS, or ventilator days suggesting that outcomes for polytrauma patients with BCT are multifactorial in nature. This could be explained by the fact that pulmonary contusion is an evolving lesion and initial measurements of CTCV only describes the disease at a single time point. Wang et al. [16] analyzed the implications of PC volume measurement with three-dimensional CT in the detection of ARDS at early stage. The authors identified PaO2/FiO2 ratio and the percentage of CTCV to be the independent predictors of developing ARDS in patients with BCT. In our series, lung contusion volume, chest infection, and ISS were independently associated with the development of ARDS. In addition, PaO2/FiO2 ratio was not an independent predictor of ARDS development in our series.
Study limitations
A limitation of the present study was its retrospective nature. Furthermore, aspiration risk and pneumonia were not well defined in our records. Also, the measurement of pulmonary contusion might have introduced some subjectivity into the findings of our study. To overcome this variation, experienced radiologists were involved to identify the volume of pulmonary contusion from the thoracic CT imaging. Furthermore, we believe that the lack of atelectasis quantification might prevent distinguishing an effect of CTCV in intubated patient in our series, which is another limitation of our study. Post hoc power analysis showed a power=1; however, further prospective studies with larger sample size are needed to address the validity of CTCV in the patients care and to demonstrate a dose-response curve for CTCV and adverse outcomes.
Conclusions
Pulmonary contusion is a common clinical entity in BCT with a significant risk of morbidity and mortality. Pulmonary contusion volume has a significant correlation with injury severity. Moreover, quantifying pulmonary contusion volumes could allow identification of patients at high-risk of ARDS development and CTCV >20% are more likely to be associated with prolonged mechanical ventilation. This could have important implication for clinical prognostication as well as targeting of appropriate patients for the proven therapies. Accurate measurements of PC volume on admission by chest CT scan can lead to early intervention such as selective ventilatory support with lung protective strategies, chest physiotherapy, nasotracheal suction, and pain relief which may be important in prevention of pulmonary complications. However, contusion volume was not found to be independently associated with pooled in-hospital outcomes suggesting that outcomes of BCT are influenced by multiple factors.
Acknowledgments
The authors would like to thank the entire registry database team in the section of trauma surgery. The Medical Research Center (IRB# 13331/13) at Hamad Medical Corporation, Doha, Qatar, has approved the study.
Footnotes
This study was presented in part at London trauma conference December 8th–11th, 2015, London, U.K.
Conflict of interest
None.
Source of support: Departmental sources
References
- 1.Huber S, Biberthaler P, Delhey P, et al. Trauma Register DGU. Predictors of poor outcomes after significant chest trauma in multiply injured patients: A retrospective analysis from the German Trauma Registry (Trauma Register DGU®) Scand J Trauma Resus Emerg Med. 2014;22:52. doi: 10.1186/s13049-014-0052-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Danelson KA, Chiles C, Thompson AB, et al. Correlating the extent of pulmonary contusion to vehicle crash parameters in near-side impacts. Ann Adv Automot Med. 2011;55:217–30. [PMC free article] [PubMed] [Google Scholar]
- 3.Hosseini M, Ghelichkhani P, Baikpour M, et al. Diagnostic accuracy of ultrasonography and radiography in detection of pulmonary contusion; A systematic review and meta-analysis. Emerg (Tehran) 2015;3:127–36. [PMC free article] [PubMed] [Google Scholar]
- 4.Amital A, Shitrit D, Fox BD, et al. Long-term pulmonary function after recovery from pulmonary contusion due to blunt chest trauma. Isr Med Assoc J. 2009;11:673–76. [PubMed] [Google Scholar]
- 5.Danelson KA, Chiles C, Thompson AB, et al. Correlating the extent of pulmonary contusion to vehicle crash parameters in near-side impacts. Ann Adv Automot Med. 2011;55:217–30. [PMC free article] [PubMed] [Google Scholar]
- 6.Cobanoglu U, Melek M, Edirne Y. Chest radiography diagnosis of pulmonary contusion is associated with increased morbidity and mortality. IJTCVS. 2010;26:24–29. [Google Scholar]
- 7.Guerrero-Lopez F, Vasquez-Mata G, Alcazar-Romero P, et al. Evaluation of the utility of computed tomography in the initial assessment of the critical care patient with chest trauma. Crit Care Med. 2000;28:1370–75. doi: 10.1097/00003246-200005000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Palas J, Matos AP, Mascarenhas V, et al. Multidetector computer tomography: Evaluation of blunt chest trauma in adults. Radiol Res Pract. 2014;2014:864369. doi: 10.1155/2014/864369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Strumwasser A, Chu E, Yeung L, et al. A novel CT volume index score correlates with outcomes in polytrauma patients with pulmonary contusion. J Surg Res. 2011;170:280–85. doi: 10.1016/j.jss.2011.03.022. [DOI] [PubMed] [Google Scholar]
- 10.Miller PR, Croce MA, Bee TK, et al. ARDS after pulmonary contusion: Accurate measurement of contusion volume identifies high-risk patients. J Trauma. 2001;51:223–28. doi: 10.1097/00005373-200108000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Pape HC, Lefering R, Butcher N, et al. The definition of polytrauma revisited: An international consensus process and proposal of the new ‘Berlin definition’. J Trauma Acute Care Surg. 2014;77:780–86. doi: 10.1097/TA.0000000000000453. [DOI] [PubMed] [Google Scholar]
- 12.ARDS Definition Task Force. Ranieri VM, Rubenfeld GD, Thompson BT, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526–33. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 13.Ganie FA, Lone H, Lone GN, et al. Lung contusion: A clinico-pathological entity with unpredictable clinical course. Bull Emerg Trauma. 2013;1:7–16. [PMC free article] [PubMed] [Google Scholar]
- 14.Donnelly LF, Klosterman LA. Subpleural sparing: A CT finding of lung contusion in children. Radiology. 1997;204(2):385–87. doi: 10.1148/radiology.204.2.9240524. [DOI] [PubMed] [Google Scholar]
- 15.Costantino M, Gosselin MV, Primack SL. The ABC’s of thoracic trauma imaging. Semin Roentgenol. 2006;41:209–25. doi: 10.1053/j.ro.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 16.Wang S, Ruan Z, Zhang J, Jin W. The value of pulmonary contusion volume measurement with three-dimensional computed tomography in predicting acute respiratory distress syndrome development. Ann Thorac Surg. 2011;92:1977–83. doi: 10.1016/j.athoracsur.2011.05.020. [DOI] [PubMed] [Google Scholar]
- 17.Deunk J, Poels TC, Brink M, et al. The clinical outcome of occult pulmonary contusion on multidetector-row computed tomography in blunt trauma patients. J Trauma. 2010;68:387–94. doi: 10.1097/TA.0b013e3181a7bdbd. [DOI] [PubMed] [Google Scholar]
- 18.Jin H, Tang LQ, Pan ZG, et al. Ten-year retrospective analysis of multiple trauma complicated by pulmonary contusion. Mil Med Res. 2014;1:7. doi: 10.1186/2054-9369-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamrick MC, Duhn RD, Ochsner MG. Critical evaluation of pulmonary contusion in the early post-traumatic period: Risk of assisted ventilation. Am Surg. 2009;75:1054–58. [PubMed] [Google Scholar]
- 20.Tyburski JG, Collinge JD, Wilson RF, Eachempati SR. Pulmonary contusions: Quantifying the lesions on chest X-ray films and the factors affecting prognosis. J Trauma. 1999;46:833–38. doi: 10.1097/00005373-199905000-00011. [DOI] [PubMed] [Google Scholar]