Dear Editor
We have read with great interest the article of C. Markello et al. entitled “Vascular pathology of medial arterial calcifications in NT5E deficiency: Implications for the role of adenosine in pseudoxanthoma elasticum” [1]. The reported case raises a new hypothesis about another rare inherited tissular calcifiying disease known as pseudo xanthoma elasticum (PXE) characterized by a deficiency in the ABCC6 transporters. Although their hypothesis is seductive, several crucial clinical signs that characterize PXE are lacking in the NT5E patient's phenotype. Based on the literature and our own comprehensive cohorts (>100 patients) with documented ultrasound imaging and CT scans, there are major differences to the NT5E case. Uni or bilateral arteriomegaly, an aneurismal-like lesion, in the distal femoral and popliteal arteries has never reported in PXE cohorts [2] (see Fig. 1) and in the Abcc6-null mice, an animal model that closely mimic the human PXE condition [3–5]. Very importantly, the basic ophthalmologic findings (angioid streaks and peau d'orange) and skin lesions that characterize the PXE phenotype [2] are lacking (or not mentioned) in the present case and others recently published [6]. Rare aneurismal lesions in PXE are restricted to the cerebral vasculature which differs histologically from the lower-limb vasculature. In addition, a reduction of the diameter of the peripheral arteries (rather than an increase), with thickening of the medial layer, and fragmentation of elastic fibers occurs in PXE, illustrate further the divergence with the present case [3–5]. Therefore, we believe that the proposed hypothesis that adenosine (or AMP) is the ABCC6 substrate responsible for the vascular manifestation in PXE is certainly premature and would require careful demonstration in large cohorts. Although it cannot be excluded that some amount of extracellular adenosine could be transported via ABCC6, other important mechanisms intervene to explain the phenotypic differences that remain unanswered.
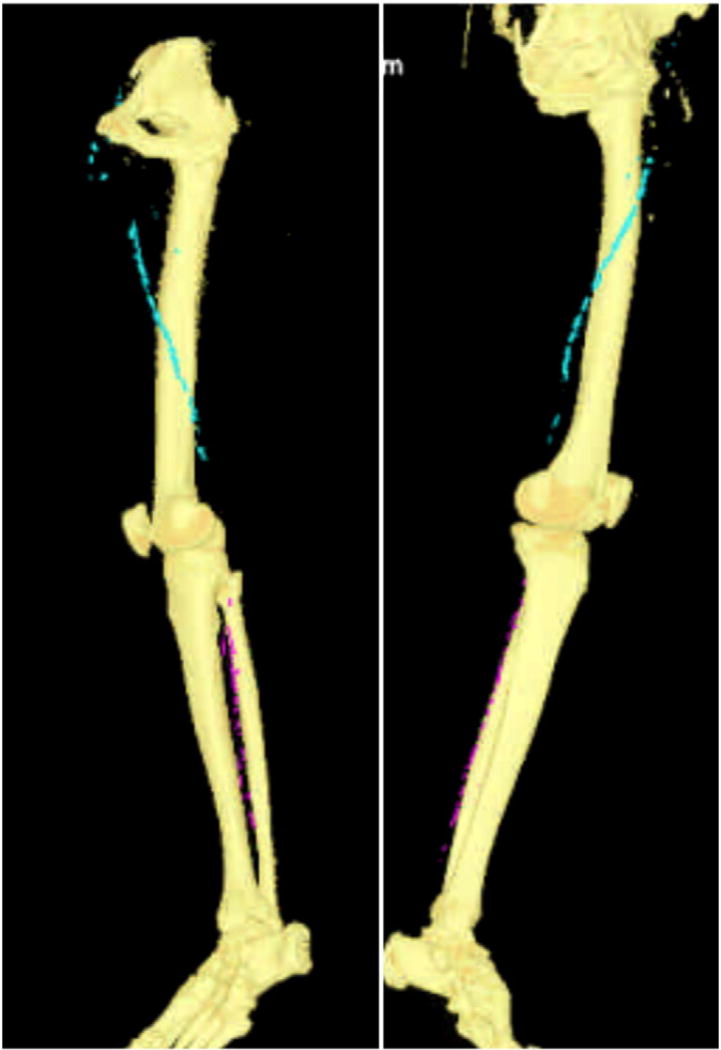
Fig. 1.
Non-opacified CT-scan of the lower legs in a patient with PXE disease (male, 59 years) showing the typical calcified proximal (blue) and distal (cyan) arteries. Note the absence of arteriomegaly. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Contributor Information
Georges Lefthériotis, University Hospital of Angers, PXE Center, France.
Olivier Vanakker, Center for Medical Genetics, Ghent University Hospital, Belgium.
Olivier Le Saux, Department of Cell and Molecular Biology, University of Hawaii, USA.
Ludovic Martin, University Hospital of Angers, PXE Center, France.
References
- 1.Markello TC, Pak LK, StHilaire C, Dorward H, Ziegler SG, Chen MY, Chaganti K, Nussbaum RL, Boehm M, Gahl WA. Vascular pathology of medial arterial calcifications in NT5E deficiency: implications for the role of adenosine in pseudoxanthoma elasticum. Mol. Genet. Metab. 2011 doi: 10.1016/j.ymgme.2011.01.018. (Electronic publication ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vanakker OM, Leroy BP, Coucke P, Bercovitch LG, Uitto J, Viljoen D, Terry SF, Van Acker P, Matthys D, Loeys B, De Paepe A. Novel clinico-molecular insights in pseudoxanthoma elasticum provide an efficient molecular screening method and a comprehensive diagnostic flowchart. Hum. Mutat. 2008;29:205. doi: 10.1002/humu.9514. [DOI] [PubMed] [Google Scholar]
- 3.Kornet L, Bergen AA, Hoeks AP, Cleutjens JP, Oostra RJ, Daemen MJ, van Soest S, Reneman RS. In patients with pseudoxanthoma elasticum a thicker and more elastic carotid artery is associated with elastin fragmentation and proteoglycans accumulation. Ultrasound Med. Biol. 2004;30:1041–1048. doi: 10.1016/j.ultrasmedbio.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Boutouyrie P, Germain DP, Tropeano AI, Laloux B, Carenzi F, Zidi M, Jeunemaitre X, Laurent S. Compressibility of the carotid artery in patients with pseudoxanthoma elasticum. Hypertension. 2001;38:1181–1184. doi: 10.1161/hy1101.096108. [DOI] [PubMed] [Google Scholar]
- 5.Germain DP, Boutouyrie P, Laloux B, Laurent S. Arterial remodeling and stiffness in patients with pseudoxanthoma elasticum. Arterioscler. Thromb. Vasc. Biol. 2003;23:836–841. doi: 10.1161/01.ATV.0000067428.19031.28. [DOI] [PubMed] [Google Scholar]
- 6.St. Hilaire C, Ziegler SG, Markello TC, Brusco A, Groden C, Gill F, Carlson-Donohoe H, Lederman RJ, Chen MY, Yang D, Siegenthaler MP, Arduino C, Mancini C, Freudenthal B, Stanescu HC, Zdebik AA, Chaganti RK, Nussbaum RL, Kleta R, Gahl WA, Boehm M. NT5E mutations and arterial calcifications. N. Engl. J. Med. 2011;364:432–442. doi: 10.1056/NEJMoa0912923. [DOI] [PMC free article] [PubMed] [Google Scholar]