Abstract
Psychological distress is common in patients with diabetes. Little is known about the impact of Mindfulness Based Stress Reduction (MBSR), a non-traditional, cognitive behavioural intervention designed to improve stress management skills, in patients with diabetes.
The purpose of this retrospective analysis was to evaluate the impact of MBSR training on mood states in 25 individuals with diabetes. All participants completed the Profile of Mood States Short Form (POMS-SF) at baseline and following eight weeks of MBSR. Overall psychological distress measured by the total mood score (TMS) and six subscales – including tension/anxiety, depression/dejection, anger/hostility, fatigue/inertia, confusion/bewilderment and vigour/activity – were assessed.
Overall mood, measured by the TMS, as well as all subscale mood measurements improved significantly from baseline following MBSR training. Compared to population means, those with diabetes had higher distress at baseline and similar levels of distress following MBSR training. The primary reason participants reported for enrolling in the MBSR course was to improve stress management skills.
It was concluded that MBSR training is a promising, group-based intervention that can be used to decrease psychological distress in individuals with diabetes who perceive a need for training in stress management.
Keywords: diabetes distress, mindfulness meditation
Introduction
Emotional distress is common among patients with diabetes mellitus, though techniques for its management remain unproven.1 Mindfulness, described as attending to present moment experiences without judgement, improves psychological health, increases emotional flexibility and promotes the development of effective coping skills.2,3 A popular approach used to cultivate mindfulness is Mindfulness Based Stress Reduction (MBSR).4,5 Little is known about the efficacy of MBSR in patients with diabetes, although a small, uncontrolled trial demonstrated trends in psychological symptom reduction following MBSR training in subjects with type 2 diabetes.6 We sought to gain an enhanced perspective on the psychological impact of MBSR in individuals with diabetes by examining the effects of this intervention on specific mood states.
Research design and methods
The Penn Program for Stress Management offers training in MBSR throughout greater Philadelphia. MBSR is a group-based intervention designed to provide basic instruction on mindfulness techniques including meditation and mindful movement. Based upon the MBSR programme developed at the University of Massachusetts, the course includes eight weekly classes of 2.5 hours with an all-day retreat between weeks seven and eight.5 Outside of class, participants are asked to practise mindfulness exercises daily for 30–45 minutes.
Course participants are asked to complete the Profile of Mood States Short Form (POMS-SF) at baseline and at week eight of training. The POMS-SF is a 30-item, self-assessment of emotional distress with scores ranging from -20 (no distress) to 100 (high distress).7 In addition to an overall measure of emotional distress, termed the total mood score (TMS), there are six subscale scores which include: tension/anxiety, depression/dejection, anger/hostility, fatigue/inertia, confusion/bewilderment and vigour/activity. Lower scores indicate a more positive mood state except for vigour/activity, where higher scores reflect a more positive mood.
We performed a retrospective analysis of data collected between September 2003 and March 2008. Within the database, we identified 25 individuals with a self-reported diagnosis of diabetes who provided complete demographic and pre-/post-questionnaire data. For each outcome, data are expressed as the median and interquartile range; paired Wilcoxon signed-ranks test was used to compare pre- and post-MBSR POMS-SF scores. Unpaired t-tests were used to compare baseline and post-MBSR POMS-SF scores in the diabetes participants compared to population normative values.7 Outcome expectancy was assessed by the reasons cited for enrolment by the participants prior to beginning the MBSR training. SPSS version 15.0 was used for data analyses. Institutional Review Board approval from the University of Pennsylvania was obtained.
Results
The mean age was 56±10 years. Sixty percent of the cohort were female. Forty-four percent had type 2 diabetes, 12% had type 1 diabetes and 44% did not specify diabetes type.
The TMS was significantly improved at the end of the programme (pre 23.7 [14–51]/post 8 [1–14], p<0.001). Improvement in each of the POMS-SF mood subscales was also observed: tension/anxiety (pre 7 [5–10]/post 4 [2–6]); depression/dejection (pre 6 [3–11.5}/post 3 [0.5-6]); anger/hostility (pre 6 [1.5–9]/post 2 [0.5–4]); fatigue/inertia (pre 12 [5.5–15]/post 5 [3–7]); confusion/bewilderment (pre 6 [3–10]/post 4 [2–5]); vigour/activity (pre 7 [3.5–10.5]/post 12 [8–14]). The p-value was <0.001 for all pre-post comparisons except for confusion, where p=0.003.
Compared to population values, individuals with diabetes had higher distress at baseline and similar levels of distress following MBSR training (Figure 1). After training, vigour was significantly higher than that of the general population.
Figure 1. Pre- and post-POMS (Profile of Mood States) scores compared to population normative values.
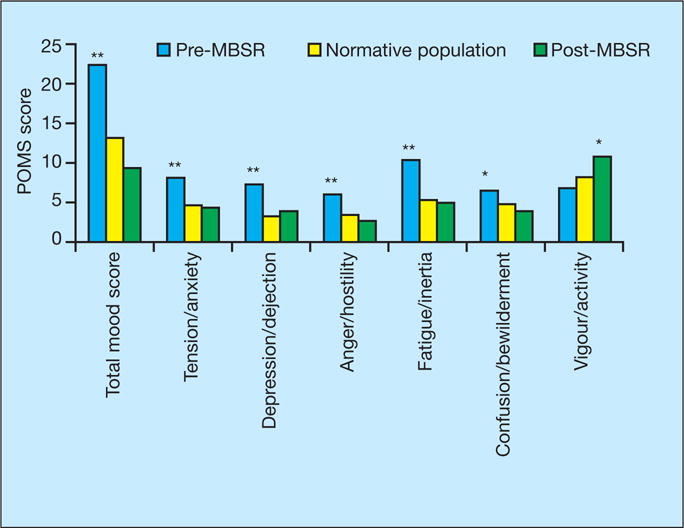
Comparisons are of mood scores (1) pre-MBSR vs normative population, and (2) post-MBSR vs normative population; *p<0.05; **p<0.001.
Reasons cited for enrolment in the MBSR course included improvement of the following: stress management (24%), anxiety (20%), focus/concentration (20%), weight (16%), hypertension (16%), worry/obsessive thinking/guilt (12%), pain control (12%), anger (12%), sleep (8%), overall health (8%), energy (4%), depression (4%) and diabetes (4%).
Discussion
Prior to training, participants with diabetes had elevated levels of psychological distress compared to population norms, decreasing to that of the general population after MBSR training. This improvement was statistically significant for all measures of a validated mood scale and resulted in increased vigour and activity compared to the general population. Most enrolled in the MBSR course with the desire to develop effective stress management skills. Few had preconceived beliefs that participation would improve mood or increase energy, thereby making these observed psychological improvements less attributable to expectancy of benefit.
The continual physical and psychological demands that accompany living with diabetes can lead to significant emotional distress.8 The most effective means for dealing with this distress remain unanswered. Based upon traditional cognitive behavioural therapy theory, the overarching goal of previous stress management interventions has been to increase logical thinking through the judgement and suppression of irrational thoughts, assumptions, and beliefs.9,10 Eliminating distressful thoughts may not be a realistic strategy in patients with diabetes. Avoidance of negative thoughts and feelings related to diabetes is associated with poorer quality of life, higher degrees of depressive thoughts and lower adherence to self-care regimens.11,12 Acceptance of diabetes and diabetes-related thoughts is associated with improved glycaemic control and may be a more realistic approach.13,14 Mechanistically, living mindfully facilitates the perception of thoughts, feelings, emotions and experiences in a less judgemental, more accepting way. Successful incorporation of mindfulness into daily living improves coping skills, promotes emotional flexibility and optimises self-regulation, ultimately leading to decreased psychological distress.15 It is important to highlight that the population of subjects we studied were self-selected and enrolled in the MBSR course seeking specific training in stress management. We conclude that MBSR may be beneficial for those with diabetes who perceive a need for training in stress management and who are committed to participating fully in this type of programme. Our findings add to a small body of evidence that suggests training in mindfulness may have beneficial psychological effects in those with diabetes, although to date sample sizes have been small and studies uncontrolled.6,14
Improvements in fatigue and vigour are intriguing and have particular relevance in diabetes. Although Rosenzweig et al.6 reported no change in exercise patterns in subjects with diabetes who completed MBSR training, our findings suggest that individuals experience an enhancement in vigour and a decline in fatigue. Capitalising on these changes could lead to more favourable daily physical activity patterns, a cornerstone of successful diabetes management.
Our findings should be regarded as preliminary – due to the small sample size, lack of metabolic measurements, incomplete classification of diabetes by type, potential for variation in the delivery of the programme based upon the MBSR instructor and retrospective, uncontrolled design. Since the degree and type of emotional distress vary by type of diabetes, it is important to highlight our inability to comment on differences in the utility of this intervention between patients with type 1 and type 2 diabetes.1 However, with the ever increasing burden of diabetes worldwide, innovative and accessible adjunctive therapies are urgently needed to promote healthy coping for those with this chronic disease. Our data support the need for randomised, controlled studies to determine if decreased psychological distress achieved through mindfulness can be sustained over time and/or contribute to decreased diabetes-related morbidity and mortality.
Key points.
MBSR offers individuals with diabetes who perceive a need for training in stress management, a cost-effective, non-pharmacological, adjunctive treatment for improving their psychological well-being
Improvements on the mood subscales for depression, fatigue and vigour are interesting and have particular relevance for patients with diabetes
Acknowledgments
This project was funded through training grant NIDDK T32007314.
Footnotes
Conflict of interest statement
There are no conflicts of interest.
Contributor Information
Laura A Young, Clinical Associate, Endocrinology, Diabetes and Metabolism, NRSA Post-doctoral Research Fellow, Department of Internal Medicine, Division of Endocrinology and Metabolism, University of Pennsylvania, USA.
Anne R Cappola, Assistant Professor of Medicine and Epidemiology, Department of Internal Medicine, Division of Endocrinology and Metabolism, University of Pennsylvania, USA.
Michael J Baime, Assistant Professor, Department of Internal Medicine, University of Pennsylvania; Director, Penn Program for Stress Management, University of Pennsylvania, USA.
References
- 1.Peyrot M, Rubin RR, Lauritzen T, et al. Psychosocial problems and barriers to improved diabetes management: results of the Cross-National Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diabet Med. 2005;22(10):1379–1385. doi: 10.1111/j.1464-5491.2005.01644.x. [DOI] [PubMed] [Google Scholar]
- 2.Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 3.Grossman P, Niemann L, Schmidt S, et al. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 4.Ludwig DS, Kabat-Zinn J. Mindfulness in Medicine. JAMA. 2008;300(11):1350–1352. doi: 10.1001/jama.300.11.1350. [DOI] [PubMed] [Google Scholar]
- 5.Kabat-Zinn J. Full catastrophe living Using the wisdom of your body and mind to face stress, pain and illness. New York: Bantam Doubleday Dell Publishing; 1990. [Google Scholar]
- 6.Rosenzweig S, Reibel DK, Greeson JM, et al. Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: a pilot study. Altern Ther Health Med. 2007;13(5):36–38. [PubMed] [Google Scholar]
- 7.McNair DM, Lorr M, Droppelman LF. POMS profile of mood states manual. Toronto, Ontario: 1992. [Google Scholar]
- 8.Fisher L, Skaff MM, Mullan JT, et al. Clinical depression versus distress among patients with type 2 diabetes: not just a question of semantics. Diabetes Care. 2007;30(3):542–548. doi: 10.2337/dc06-1614. [DOI] [PubMed] [Google Scholar]
- 9.Surwit RS, van Tilburg MAL, Zucker N, et al. Stress management improves long-term glycemic control in type 2 diabetes. Diabetes Care. 2002;25(1):30–34. doi: 10.2337/diacare.25.1.30. [DOI] [PubMed] [Google Scholar]
- 10.Henry J, Wilson P, Bruce D, et al. Cognitive-behavioural stress management for patients with non-insulin dependent diabetes mellitus. Psychol Health Med. 1997;2:109–118. [Google Scholar]
- 11.Boey K. Adaptation to type II diabetes mellitus: Depression and related factors. Int Medical J. 1999;6:125–132. [Google Scholar]
- 12.Coelho R, Amorim I, Prata J. Coping styles and quality of life in patients with non-insulin-dependent diabetes mellitus. Psychosomatics. 2003;44(4):312–318. doi: 10.1176/appi.psy.44.4.312. [DOI] [PubMed] [Google Scholar]
- 13.Richardson A, Adner N, Nordstrom G. Persons with insulin-dependent diabetes mellitus: acceptance and coping ability. J Adv Nurs. 2001;33(6):758–763. doi: 10.1046/j.1365-2648.2001.01717.x. [DOI] [PubMed] [Google Scholar]
- 14.Gregg JA, Callaghan GM, Hayes SC, et al. Improving diabetes self-management through acceptance, mindfulness, and values: a randomized controlled trial. J Consult Clin Psychol. 2007;75(2):336–343. doi: 10.1037/0022-006X.75.2.336. [DOI] [PubMed] [Google Scholar]
- 15.Reibel D, Greeson J, Brainard G, et al. Mindfulness-based stress reduction and health-related quality of life in a heterogeneous patient population. Gen Hosp Psychiatry. 2001;23(3):183–192. doi: 10.1016/s0163-8343(01)00149-9. [DOI] [PubMed] [Google Scholar]


