Abstract
Reference isolates of Candida parapsilosis (n = 8), Candida metapsilosis (n = 6), Candida orthopsilosis (n = 7), and Lodderomyces elongisporus (n = 11) were analyzed to gain insight into their pathobiology and virulence mechanisms. Initial evaluation using BBL Chromagar Candida medium misidentified L. elongisporus isolates as C. albicans. Polymerase chain reaction analysis of isolate MTL idiomorphs revealed that all C. parapsilosis isolates were MTLa homozygous and no MTL α1, α2, a1, or a2 gene was detected in L. elongisporus isolates. For C. orthopsilosis, two isolates were MTLa homozygous and five were MTL-heterozygous. Similarly, one C. metapsilosis isolate was MTLα homozygous whereas five were MTL-heterozygous. Isolate phenotypic switching analysis revealed potential phenotypic switching in the MTLα homozygous C. metapsilosis isolate, resulting in concomitant elongated cell formation. Minimum inhibitory concentrations of fluconazole (FLC) and FK506, alone or in combination, were determined by checkerboard assay, with data analyzed using the fractional inhibitory concentration index model. Synergistic or additive effects of these compounds were commonly observed in C. parapsilosis and L. elongisporus isolates. No killer activity was observed in the studied isolates, as determined phenotypically. No significant difference in virulence was seen for the four species in a Galleria mellonella model (P > 0.05). In conclusion, our results demonstrated phenotypic switching of C. metapsilosis CBS 2315 and that FLC and FK506 represent a promising drug combination against C. parapsilosis and L. elongisporus. The findings of the present study contribute to our understanding of the biology, diagnosis, and new possible treatments of the C. parapsilosis species group and L. elongisporus.
Introduction
The Candida parapsilosis group of species belonging to the human commensal mycoflora comprises three closely related taxa, C. parapsilosis, C. orthopsilosis, and C. metapsilosis [1]. C. parapsilosis is the most common pathogen within the group and is considered the most virulent. Candida metapsilosis is the least virulent species, with a low prevalence in human infections [2–4]. Thus, given the significant differences between species, it is not recommended to refer to a "species complex" for C. parapsilosis and its relatives [5]. Infections caused by C. parapsilosis and C. orthopsilosis are mainly described in severely ill patients from intensive care units, in low-birth-weight neonates, and in those receiving parenteral nutrition [6,7]. However, during the last decade, antifungal resistance to azoles and caspofungin has markedly increased worldwide among the entire group [8,9], which may contribute to increased prevalence.
Lodderomyces elongisporus was initially thought to represent the asexual state of C. parapsilosis [10]; however, subsequent small subunit rRNA gene sequencing revealed it to be a closely related but distinct species [11]. In a phylogenetic analysis, Riccombeni et al. [12] showed that L. elongisporus was classified within a clade of the C. parapsilosis species group and C. albicans, C. dubliniensis, and C. tropicalis, although in that clade, L. elongisporus is the only species that is able to produce ascospores [13,14]. Using large subunit rRNA gene sequencing, Lockhart et al. [15] described the first human L. elongisporus infections, which mostly occurred in patients from Mexico; notably, these isolates had initially been misidentified physiologically by the Vitek yeast identification system as C. parapsilosis. More recently, L. elongisporus has been shown to be globally distributed and human infections have been reported from the Middle East [16,17], Spain [18], and Japan [19]. However, compared to that in C. parapsilosis, antifungal resistance is fairly low in L. elongisporus [15–18].
Whereas mating has not yet been reported for the C. parapsilosis species group, C. albicans has been reported to have a parasexual cycle [20–23]. The mating-type like (MTL) locus of C. albicans is present as two idiomorphs: MTLa and MTLα [24–26]. In contrast, only a single MTL idiomorph, MTLa, has been identified in C. parapsilosis [27]. In comparison, L. elongisporus is reported to be in a homothallic sexual state, producing asci and ascospores in solo culture [13].
Switching between morphological phenotypes is common in pathogenic fungi and is hypothesized to be important in adapting to different environmental conditions [28]. C. albicans efficiently switches and is known to be present as yeast, hyphae, pseudohyphae, chlamydospores, and several yeast-like phases such as white, opaque, grey, and GUT phenotypes that have different virulence potentials and assist in the successful adaptation to different host niches [29]. The opaque phase also constitutes the mating-specialized form of C. albicans [30]. These are elongated and absorb phloxine B, producing pink colonies [31]. C. parapsilosis has also been reported to have different cell and colony morphologies, which exhibit different biofilm formation and agar invasion capabilities [32].
"Killer" characteristics were first observed in laboratory strains of Saccharomyces cerevisiae by Makower and Bevan [33], who defined the yeast phenotypes as killer, sensitive, and neutral. Killer yeasts secrete proteinaceous toxins that are lethal to sensitive strains, but to which the killer strains themselves are immune [34,35]. To date, killer yeasts have been reported in several genera, although the most widely studied killer systems are those of S. cerevisiae and Kluyveromyces lactis, with toxins that are RNA and DNA plasmid-encoded, respectively [36,37]. Growth inhibition evoked in sensitive strains by killer yeasts and their toxins has been proposed as a means of biotyping pathogenic Candida and Cryptococcus strains [38]. The killer system also enables species recognition within the C. parapsilosis species group, as only C. metapsilosis strains were shown to exhibit killer activity, in contrast to C. parapsilosis and C. orthopsilosis [39].
Published studies strongly suggest that Galleria mellonella provides a good alternative model for studying virulence in several fungi, including the major human fungal pathogens Aspergillus spp. [40], Candida spp. [41], and Cryptococcus spp. [42]. As the emerging resistance in the entire group of C. parapsilosis has led to difficult-to-treat infections [8,9], it is therefore important to understand the virulence potential of C. parapsilosis and its relatives. Furthermore, the development of drug combinations to address emerging antifungal resistance is critical for the management of patients, particularly in the case of invasive diseases [43–48]. Accordingly, Sun et al. [43] suggested the antifungal potential of a combination therapy with calcineurin pathway inhibitors (i.e., FK506, also known as tacrolimus) as a replacement for the activity of several azoles to combat azole resistance in C. albicans.
In the present study, we analyzed C. parapsilosis and its relatives to further characterize (i) the accuracy of their identification on BBL Chromagar Candida medium, (ii) their MTL genotypes and the occurrence of phenotypic switching, (iii) their killer activity and virulence in the G. mellonella model, and (iv) the ability of FK506 to enhance the isolate susceptibility to fluconazole (FLC).
Materials and methods
Isolates
The strains used in this study, i.e., C. metapsilosis (n = 6), C. orthopsilosis (n = 7), C. parapsilosis (n = 8), and L. elongisporus (n = 11), as well as their origin, identification number, and place of origin, are listed in S1 Table. C. parapsilosis species group isolates were provided by the culture collection of Centraalbureau voor Schimmelcultures (housed at Westerdijk Fungal Biodiversity Institute, Utrecht, the Netherlands) and L. elongisporus isolates were from the collection of the Molecular Genetics and Microbiology Department (Duke University, Durham, NC). All strains were subcultured on yeast extract-peptone dextrose agar (YEPD; Difco, Detroit, MI), at 37°C for 3 d, prior to analysis. The identities of all strains were verified prior to this study by sequencing the internal transcribed spacer region.
Growth on chromogenic medium
All strains were inoculated in parallel onto BBL Chromagar Candida medium (Becton Dickinson and Company, Sparks, MD) and Sabouraud dextrose agar (SDA; Merck, Darmstadt, Germany), and incubated at 37°C for 72 h [15]. Following the incubation period, the isolates were evaluated on the basis of colony color. C. albicans SC5314 and C. tropicalis YJM57 were used as control strains.
Genomic DNA isolation, polymerase chain reaction (PCR) amplification, and DNA sequencing
For genomic DNA isolation, all strains were collected directly from YEPD plates after 2 d of growth. Genomic DNA isolation was performed using the MasterPure Yeast DNA Purification Kit (Epicentre Biotechnologies, Madison, WI) according to the manufacturer’s instructions.
All PCR assays were conducted in a PTC-200 automated thermal cycler (BioRad, Hercules, CA); 300 ng DNA was used as a template for amplification in a 25 0μL reaction mixture containing 10 pM of each primer, 2 mM of each nucleotide (dATP, dCTP, dGTP, and dTTP), 2.5 μL 10 × Ex Taq buffer, 0.125 mL ExTaq polymerase (TaKaRa, Shiga, Japan), and an appropriate volume of distilled water. The primers and their sequences are specified in S2 Table.
The following conditions were used for standard PCR amplification: an initial 5 min denaturation at 94°C; followed by 36 cycles of denaturation for 1 min at 94°C, annealing for 1 min at 57°C, and an extension for 1 min at 72°C. The amplification was completed with a final extension period of 10 min at 72°C. For amplification using degenerate primers, a touchdown protocol was applied (5 min at 94°C; 24 cycles of 45 s at 94°C, 45 s at 66°C–54°C step-down at 0.5°C every cycle, 1 min at 72°C; 16 cycles of 45 s at 94°C, 45 s at 54°C, 1 min at 72°C, and a final extension step of 10 min at 72°C). Sterile water instead of DNA served as a negative control in each assay. PCR products were analyzed on 1% agarose gels.
Amplicons to be sequenced were purified using the QIAquick PCR Purification Kit (Qiagen, Germantown, MD) as recommended by the manufacturer. Both strands of PCR products were sequenced using BigDye Terminator version 3.1 cycle sequencing ready reaction mix (Applied Biosystems, Foster City, CA). Sequencing products were resolved using an ABI 3130 automated sequencer (Applied Biosystems) and the sequences were assembled using Sequencher 4.8. software (Gene Code Corporation, Ann Arbor, MI).
Switching test
To examine the occurrence of phenotypic switching, the isolates were grown on plates of supplemented Lee’s agar medium for 5 d and then plated on synthetic complete (SC) medium containing 5 μg/mL phloxine B; they were then further grown for 7 d at 26°C and 30°C [30]. C. albicans WO-1 white and C. albicans WO-1 white opaque strains obtained from the Duke University Molecular Genetics and Microbiology Department collection were used as control strains.
Killer activity/sensitivity assay
C. parapsilosis species group and L. elongisporus isolates were assayed to determine their killer/sensitivity phenotypes. The killer sensitivity of C. parapsilosis species group and L. elongisporus strains was assayed by mixing each isolate with YEPD-MB agar [0.3% yeast extract, 0.3% malt extract, 0.5% peptone, 2% glucose, 2% agar, and 0.003% methylene blue (MB); adjusted to pH 4.5 with 0.1 M citrate-phosphate buffer] to a final concentration of 106 cells/mL and by streaking the known killer and sensitive isolates on the surface of plates. The plates were incubated at 26°C for up to 72 h. The sensitivity test was considered positive if killer strains showed a clear inhibition zone surrounded by a blue halo [39]. RNA extraction was performed using TRIzol reagent (Thermo Fisher Scientific, Waltham, MA) according to a protocol provided by the manufacturer. S. cerevisiae strains were used as controls. Products were analyzed on 1% agarose gels.
Evaluation of virulence using the G. mellonella model
Isolates were pre-grown on YPD agar for 24 h at 37°C and then harvested by gentle scraping of the colony surfaces with plastic loops and washed three times in sterile phosphate-buffered-saline (PBS). Cell suspensions were counted using a hemocytometer, and cell density adjusted to 106 cells/μL with sterile PBS. The virulence of each isolate was tested in 15 G. mellonella larvae. Cell suspensions in sterile PBS (4 μL) were injected via the last left rear proleg, using a 100 μL Hamilton syringe with dispenser. The syringe was rinsed several times with 70% ethanol, followed by a PBS rinse, prior to injecting each larva. The control group of larvae was inoculated with sterile PBS. Inoculated larvae were incubated at 37°C and the number of dead animals was monitored daily [4].
Determination of antimicrobial drug resistance
FLC (Sigma, St. Louis, MO) and FK506 (Sigma) were diluted in sterile water according to the Clinical and Laboratory Standards Institute (CLSI) protocol [49]. Serial two-fold dilutions of each drug were prepared in RPMI 1640. Synergy testing of FLC and FK506 against C. parapsilosis species group and L. elongisporus strains was assessed by the checkerboard method [50]. The test was performed as a microdilution assay, in duplicate for each fungal strain. The minimum inhibitory concentrations (MIC) were interpreted according to the CLSI guidelines [49]. To evaluate the effect of the combinations of FLC and FK506, the fractional inhibitory concentration (FIC) was calculated for each antifungal agent in every combination. The following formulas were used to calculate the FIC index: FIC of drug A, MIC (drug A in combination)/MIC (drug A alone); FIC of drug B, MIC (drug B in combination)/MIC (drug B alone); FIC index, sum of FIC of drug A and FIC of drug B. Antifungal combinations were evaluated based on FIC index ranges, as follows: synergistic, if ≤ 0.5; additive, if > 0.5 but < 1; no effect, if ≥ 1 but < 4; and antagonistic if ≥ 4 [51,52].
Statistical analysis
The Kaplan-Meier test was performed to assess the statistical significance of differences in survival among groups. Survival curves were analyzed using Minitab v. 16.1 software with the log-rank (Mantel-Cox) test; P < 0.05 was considered statistically significant.
Results and discussions
In this study, the identifying characteristics, MTL genotypes, phenotypic switching, and susceptibility profiles of C. parapsilosis species group and L. elongisporus reference isolates were analyzed to gain insight into their pathobiology and virulence mechanisms.
Chromogenic medium
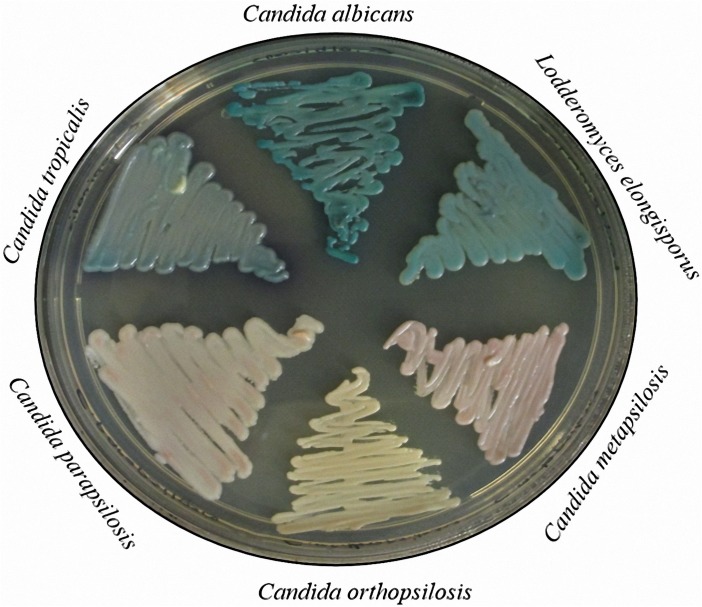
The adequacy of BBL Chromagar Candida medium for the initial identification of reference strains was evaluated. All C. parapsilosis and C. metapsilosis isolates formed light pink colonies; C. orthopsilosis formed ivory colonies; and L. elongisporus formed blue/green colonies similar to C. tropicalis and C. albicans on this medium. Representative colonies on the chromogenic medium are shown in Fig 1.
Fig 1. Candida albicans SC 5314, Candida tropicalis YJM 57, Lodderomyces elongisporus 7660, Candida metapsilosis CBS 2315, Candida orthopsilosis CBS 107.41, and Candida parapsilosis CBS 2315 were grown on BBL Chromagar Candida medium at 37°C for 3 d and photographed.
The utility of chromogenic media for the screening and initial identification of yeasts in polyfungal clinical materials is well established [53–56]. C. parapsilosis characteristically produces pink or lavender colonies on BBL CHROMagar Candida medium, whereas L. elongisporus isolates were reported to form colonies with a distinct turquoise color [15]. However, C. parapsilosis and C. metapsilosis isolates formed light pink colonies, rendering their presumptive identification problematic.
Determination of MTL genotypes
Sexual reproduction is important in the evolution of fungal pathogens. In particular, pathogenic fungi are hypothesized to restrict sexual reproduction so as not to disrupt well-adapted pathogenic genotypes; however, they maintain the potential for sexual reproduction to cope with stressful conditions such as antimicrobial therapy [57]. The MTL locus is responsible for the determination of cell identity and regulation of mating in C. albicans and related species [25]. In C. albicans, there are two versions of MTL: MTLa which harbors the transcription factor genes a1 and a2; and MTLα, which encodes the α1 and α2 regulatory elements [24–26]. Both idiomorphs also possess a or α versions of additional genes that have no known function in mating, such as PAB, OBP, and PIK [20]. In C. albicans, α1 and a2 activate the α- and a-specific genes, respectively; the a1/α2 heterodimer plays a role both in the regulation of mating and in white/opaque switching, by repressing mating and limiting switching to the opaque phase in a/α cells by inhibiting White-opaque regulator 1 (WOR1), which is regulated by other factors as well [29,58,59]. In comparison, C. orthopsilosis has an MTL locus very similar to that of C. albicans and harbors both MTLa and MTLα idiomorphs, whereas only the MTLa idiomorph has been identified to date in C. parapsilosis [27].
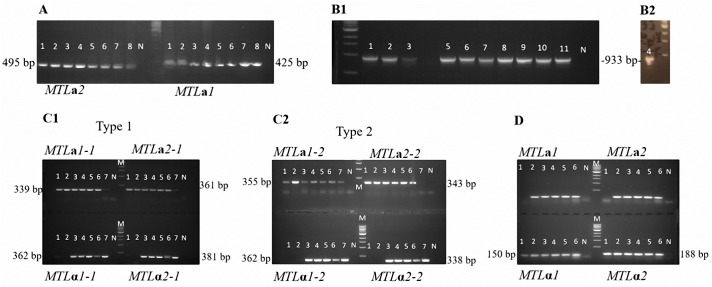
Mating type genes of the isolates were determined by PCR. As no MTL α1, α2, a1, or a2 genes have been detected in L. elongisporus to date and no C. parapsilosis MTLα idiomorph is known, degenerate primers to amplify the MTL transcription factor genes a1, a2, α1, and α2 were designed to search for the presence of these genes. In addition, specific primers were designed to amplify the a2 gene and a1 pseudogene in C. parapsilosis. PCR screening of eight C. parapsilosis isolates revealed only the presence of a1 and a2 genes (Fig 2A), indicating that these isolates all bear the MTLa idiomorph. An MTLα idiomorph was not detected using the degenerate primers.
Fig 2.
Determination of the MTL genotypes by PCR, (a) Candida parapsilosis isolates (1–8 referring to CBS 8836, CBS 7248, CBS 2915, CBS 604, CBS 2216, CBS 8181, CBS 125.41, and CBS 1954), the 425 bp MTLa1 and the 495 bp MTLa2 products were obtained for all isolates; (b1 and b2) Lodderomyces elongisporus isolates (1–11 referring to the isolates 7660, 7661, 7663, 7665, 7666, 7668, 7669, 7670, 7672, 7673, and 7675), the 933 bp PCR product obtained for all isolates indicates the absence of any MTL transcription factor gene in between PIKa and orf19.3202; (c) Candida orthopsilosis isolates (1–7 referring to CBS 107.41, CBS 107.42, CBS 109.06, CBS 8825, CBS 107.43, CBS 9894, and CBS 2212) were screened with primers designed based on C. orthopsilosis type 1 (c1) and type 2 MTL sequences (c2); both primer pairs worked for the isolates although band brightness’ varied owing to differences among type 1 and type 2 sequences. With CBS 107.41 and CBS 107.42, only MTLa1 and MTLa2 PCR products were obtained indicating that these isolates are MTLa homozygotes; the other isolates were found to be heterozygous for MTL; (d) Candida metapsilosis isolates (1–6 referring to CBS 2315, CBS 107.47, CBS 109.07, CBS 111.27, CBS 1046, and CBS 2916), whereas only MTLα1 (150 bp) and MTLα2 (188 bp) PCR products were obtained with CBS 2315 indicating MTLα homozygosity; all MTL gene products were obtained for the other isolates showing that they are MTL heterozygous. M, Marker; NC, Negative control.
L. elongisporus is the only close relative of C. parapsilosis reported to exhibit a homothallic sexual state [13]. However, in the sequenced strain and in seven additional isolates of L. elongisporus, a genomic region that is syntenic to the MTL locus of other Candida species only has the MTLa versions of PAB, OBP, and PIK genes, and does not contain any transcription factor genes [25]. Considering the genome analysis and molecular data, it was suggested that L. elongisporus might not have a sexual cycle or the sexual cycle might function in a manner independent of MTL [25].
In this study, for L. elongisporus, primers were designed to bind within PIKa and orf19.3202 (encoding a hypothetical protein ortholog of C. albicans CAALFM_C501730WA, located just outside the MTL locus in C. albicans and other closely related species), respectively [25], to check for the presence of mating genes between these sites. In the absence of any such genes, a 933 bp PCR product was predicted, as in the sequenced isolate [25]. All L. elongisporus isolates yielded 933 bp amplicons, indicating the absence of an MTL idiomorph (Fig 2B1 and 2B2). Furthermore, neither an a nor α gene was detected in the isolates using degenerate primers.
In C. orthopsilosis, α1, α2, a1, and a2 genes were screened using specific primers. Only a1- and a2-specific PCR product bands were obtained from isolates CBS 107.41 and CBS 107.42; all the expected gene PCR product bands were obtained from the remaining five isolates. This indicated a/a homozygosity of the former two isolates and a/α heterozygosity of the remainder (Fig 2C1 and 2C2). In comparison, in a study by Sai et al. [27], only two of 16 C. orthopsilosis isolates were found to be MTL heterozygous, whereas nine were MTLa homozygous, and five were MTLα homozygous.
According to Pryszcz et al. [60], the MTLα locus of C. metapsilosis is very similar to that of C. albicans in structure, encoding the genes MTLα1, MTLα2, OBPα, PIKα, and PAPα. The MTLa locus, however, harbors MTLα2, OBPα, and PIKα in addition to the a-specific genes MTLa1 and MTLa2. For C. metapsilosis isolates, primers designed by Pryszcz et al. [60] were used to amplify the α1, α2, a1, and a2 genes. Whereas PCR products for each gene were obtained from five C. metapsilosis isolates, only the α1 and α2 products were obtained from CBS 2315. Thus, CBS 2315 carried the α/α genotype and the other five isolates were a/α (Fig 2D). Similarly, 10 out of 11 C. metapsilosis isolates analyzed by Pryszcz et al. [60] were MTL heterozygous.
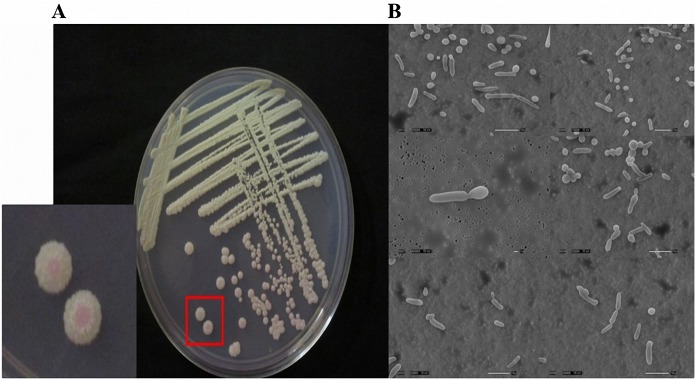
Phenotypic switching within the isolate set
Previous studies have identified different colony and cell morphologies of Candida spp., especially C. albicans and C. parapsilosis isolates. Although pseudohyphae formation has been observed in C. parapsilosis and C. albicans as well as in C. orthopsilosis, it was not observed in C. metapsilosis [4,61,62]. In contrast, in the present study we detected phenotypic switching in C. metapsilosis CBS 2315, the isolate carrying the MTLα/MTLα genotype, at 37°C. The switching led to the formation of pink colonies in the presence of phyloxine B, which contained elongated cells revealed by scanning electron microscopy (Fig 3).
Fig 3. Phenotypic switching test with Candida metapsilosis CBS 2315 (MAT α/α).
(a) Pink colonies indicating phenotypic switching (red box), grown at 30°C for 7 d on SC medium containing 5 μg/mL phloxine B; (b) elongated cells analyzed by scanning electron microscopy (Scale bar, 10 μm).
Killer activity of the isolates
A total of 32 isolates were analyzed by the killer/sensitivity phenotype test. Briefly, 22 out of 32 isolates produced weak blue halos around their colonies; nine isolates did not produce such halos. C. parapsilosis CBS 2915 produced a weak blue halo around both the killer and sensitive strains. However, no RNA band was observed on a 1% agarose gel, indicating the absence of killer activity due to a dsRNA virus.
C. parapsilosis has been reported to be a killer yeast [63], although killer strains were reported to represent less than 3% of clinical isolates of the species [64]. Killer activity was found to be expressed at 25°C, whereas isolates of C. parapsilosis and C. orthopsilosis did not show this activity at 25°C [62]. Because the killer toxin is thermolabile [34], wild-type killers exhibit very little killing activity at 30°C and are normally tested at 20°C. Therefore, in the present study, the isolates were analyzed at 26°C, 30°C, and 37°C; however, no killer activity was detected.
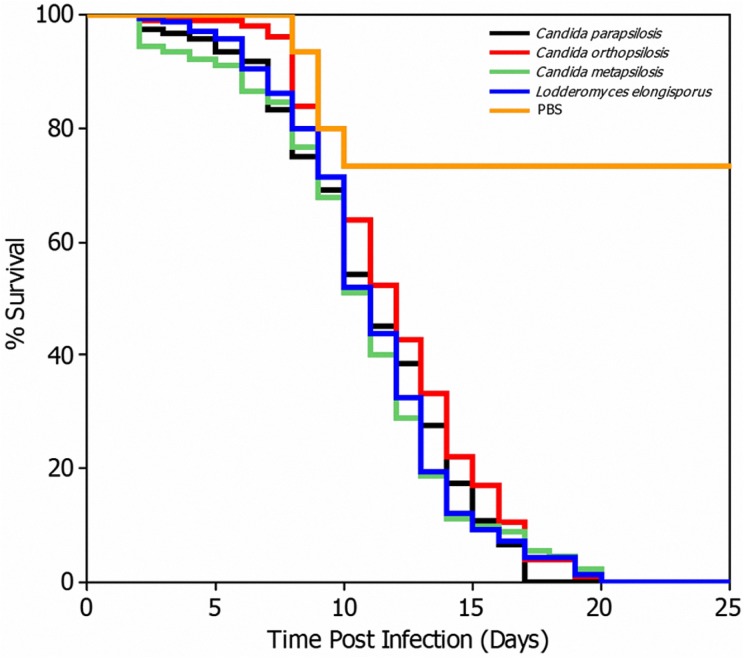
Virulence of the isolates in the G. mellonella model
Virulence of the 32 study isolates was compared using the G. mellonella model (S3 Table). We observed no significant differences among the C. parapsilosis species group and their closely related species L. elongisporus (P > 0.05); however, significant differences were detected with the PBS control group (P < 0.05; Fig 4).
Fig 4. Galleria mellonella survival curves after larval infection with the indicated Candida parapsilosis (blue line), Candida orthopsilosis (green line), Candida metapsilosis (purple line), and Lodderomyces elongisporus (turquoise line) species, or with PBS as a control (red line).
A total of 1 × 106 cells were used to infect the larvae and animal survival was observed at 37°C. All study isolates were tested.
C. orthopsilosis was reported by Gago et al. [4] to represent the most virulent species of the C. parapsilosis species group in the G. mellonella model, followed by C. parapsilosis and C. metapsilosis, with a median survival time of 2.3, 2.6, and 4.5 d, respectively. It has been previously suggested that these scores could not be related to the growth rate of Candida spp. [65]. Notably, however, C. metapsilosis strains were more effectively phagocytosed by G. mellonella hemocytes than in C. parapsilosis and C. orthopsilosis (P < 0.05) [4]. Furthermore, hyphae or pseudohyphae formation was less frequent in C. metapsilosis isolates than in C. parapsilosis and C. orthopsilosis (P < 0.05) [4]. In another study, one oral and one systemic isolate of C. parapsilosis, both susceptible to FLC and amphotericin B, killed the G. mellonella larvae within 18 h and 21 h, respectively, which suggested that the clinical origin of the strain is not important for virulence (P = 0.6) [4]. However, in contrast to these previous reports [4,65], which did not differ with respect to inoculum size in comparison with the present study (1 × 106 cells/larvae), we did not observe a difference in virulence using this model among the studied fungi.
Antimicrobial resistance of the isolates
MIC values of FLC and FK506 were determined in synergy tests using the checkerboard assay (Table 1). FIC indices were calculated by considering all combinations of drugs where no visible growth was observed. The results were as follows: for C. metapsilosis, 33.3% synergy and 66.7% indifferent effect; for C. orthopsilosis, 14.3% synergy, 14.3% additive effect, and 71.4% indifferent effect; for C. parapsilosis, 25% synergy, 62.5% additive effect, and 12.5% indifferent; and for L. elongisporus, 36.4% synergy, 45.4% additive effect, and 18.2% indifferent effect.
Table 1. Synergy testing of fluconazole (FLU) and FK506 against Candida parapsilosis species group and Lodderomyces elongisporus strains.
| Taxon Name | Reference no | Minimum inhibitory concentrations (MIC; μg/ml) | Fractional inhibitory Outcome concentration (FIC) Index |
||||
|---|---|---|---|---|---|---|---|
| Best Combined | |||||||
| FLU | FK506 | FLU | FK506 | ||||
| C.metapsilosis | CBS 2315 | 1 | >16 | 1 | 0.03125 | 1.0019 | Indifferent |
| CBS 107.47 | 1 | >16 | 1 | 0.125 | 1.007 | Indifferent | |
| CBS 109.07* | 4 | >16 | 1 | 2 | 0.375 | Synergy | |
| CBS 111.27 | 16 | >16 | 8 | 8 | 1 | Indifferent | |
| CBS 107.46 | 8 | >16 | 2 | 0.125 | 0.2578 | Synergy | |
| CBS 2916 | 16 | >16 | 16 | 8 | 1.5 | Indifferent | |
| C.orthopsilosis | CBS 107.41 | 1 | >16 | 1 | 0.03125 | 1.0019 | Indifferent |
| CBS 107.42 | 4 | >16 | 1 | 0.125 | 0.2578 | Synergy | |
| CBS 109.06* | 2 | >16 | 2 | 0.25 | 1.015 | Indifferent | |
| CBS 8825 | 1 | >16 | 2 | 0.125 | 2.0078 | Indifferent | |
| CBS 107.43 | 16 | >16 | 16 | 0.125 | 1.0078 | Indifferent | |
| CBS 9894 | 4 | >16 | 4 | 0.0625 | 1.0039 | Indifferent | |
| CBS 2212 | 8 | >16 | 4 | 0.125 | 0.5078 | Additive | |
| C.parapsilosis | CBS 8836 | 1 | >16 | 0.5 | 0.03125 | 0.5019 | Additive |
| CBS 7248 | 0.5 | >16 | 0.25 | 0.125 | 0.507 | Additive | |
| CBS 2915 | 1 | >16 | 2 | 0.15625 | 2.0098 | Indifferent | |
| CBS 604 | 4 | >16 | 2 | 0.03125 | 0.5019 | Additive | |
| CBS 2216 | 1 | >16 | 0.25 | 1 | 0.3125 | Synergy | |
| CBS 8181 | 4 | >16 | 1 | 0.03125 | 0.2519 | Synergy | |
| CBS 125.41 | 2 | >16 | 1 | 0.03125 | 0.5019 | Additive | |
| CBS 1954* | 4 | >16 | 2 | 0.03125 | 0.5019 | Additive | |
| L.elongisporus | 7660 | 1 | >16 | 0.5 | 0.03125 | 0.5019 | Additive |
| 7661 | 1 | >16 | 0.5 | 0.03125 | 0.5019 | Additive | |
| 7663 | 1 | >16 | 0.25 | 0.0625 | 0.2539 | Synergy | |
| 7665 | 1 | >16 | 1 | 0.0625 | 1.0039 | Indifferent | |
| 7666 | 1 | >16 | 0.5 | 4 | 0.75 | Additive | |
| 7668 | 1 | >16 | 0.5 | 0.03125 | 0.50195 | Additive | |
| 7669 | 1 | >16 | 1 | 0.015625 | 1.00098 | Indifferent | |
| 7670 | 2 | >16 | 0.5 | 0.0625 | 0.2539 | Synergy | |
| 7672 | 2 | >16 | 0.5 | 0.03125 | 0.2519 | Synergy | |
| 7673 | 2 | >16 | 0.25 | 4 | 0.375 | Synergy | |
| 7675 | 1 | >16 | 0.5 | 1 | 0.5625 | Additive | |
CBS, Centraalbureau voor Schimmelcultures.
*, Type strain.
The intrinsic antifungal resistance of Candida spp. constitutes a major issue related to the therapeutic management of infections and has required the utilization of combinatorial therapy, such as with FK506. For example, Chen et al. [44] reported that posaconazole exhibits an in vitro and in vivo synergistic antifungal activity with caspofungin or FK506 against C. albicans isolates. Cruz et al. [45] also observed that FK506 was synergistic with FLC against azole-resistant C. albicans mutants, against other Candida species, or when combined with different azoles. Notably, Li et al. [46] observed that a combination of FLC and FK506 might represent a promising approach toward overcoming the intrinsic resistance of Candida krusei to FLC. Denardi et al. [47] also investigated the in vitro interaction of FK506 and four azole compounds against 30 clinical FLC-susceptible or FLC-resistant Candida glabrata isolates using the microdilution checkerboard method. In particular, they detected a promising synergistic effect against FLC-resistant C. glabrata isolates of FK506 combined with ketoconazole (77%), itraconazole (73%), voriconazole (63%), and FLC (60%). In contrast, FK506 showed no activity against 30 clinical FLC-susceptible and FLC-resistant Trichosporon asahii isolates, with MICs ≥ 64 μg/ml. However, a pronounced synergistic interaction of FK506 in combination with amphotericin B (96.7%) and caspofungin (73.3%) was observed, although low rates of synergism were observed with FLU (40%) and itraconazole (10%) [48].
In the present study, we observed synergistic and additive, or indifferent, effects of FLC and FK506 against C. parapsilosis and related species including L. elongisporus; however, antagonistic activity was not observed. Previously, nine human L. elongisporus isolates were tested against FLC, amphotericin B, caspofungin, anidulafungin, and micafungin, all of which exhibited low MICs, as determined by the CLSI microdilution method [15]. Consistent with these findings [15], we observed low FLC MICs for L. elongisporus, for which no established breakpoint values are currently available. The present study also demonstrated that synergistic and additive effects of FLC and FK506 were more apparent against C. parapsilosis (87.5%) and L. elongisporus (81.8%) than other isolates, and that the combination was likely to have no effect against C. orthopsilosis (71.4%) and C. metapsilosis (66.7%). However, a limitation of the present study is that only a small number of isolates was tested. Hence, no universal conclusion may be reached regarding the data obtained herein.
In conclusion, we determined the MTL genotypes of a set of reference isolates of the C. parapsilosis species group and detected an MTLα homozygous C. metapsilosis isolate that underwent phenotypic switching and produced elongated cells. Furthermore, we observed no significant difference in virulence among the four species, using a G. mellonella model. We suggest that the FLC/FK506 combination may be promising as a therapeutic strategy against L. elongisporus and C. parapsilosis isolates, but not against C. orthopsilosis and C. metapsilosis. In vitro assessment in an experimental model is required to verify the efficacy of this drug combination. Overall, these new data may be used to guide strategies for combating these pathogens in the clinic.
Supporting information
(DOC)
(DOCX)
(XLSX)
Acknowledgments
The authors are grateful to Shawn Lockhart, PhD, for kindly providing L. elongisporus strains. We thank Valerie Knowlton, Research Assistant, at the Center for Electron Microscopy (North Carolina State University, Raleigh, NC) for her expert help with the electron microscopy experiments. The authors also acknowledge the valuable assistance of members of the Heitman laboratory at the Department of Molecular Genetics and Microbiology, Duke University, Durham, NC, with laboratory analyses.
Data Availability
Our data are all contained within the paper and/or Supporting Information.
Funding Statement
This work was supported by NIH/NIAID R37 MERIT Award AI39115-19, and NIH/NIAID R01 AI50113-13 provided support to J.H.
References
- 1. Tavanti A, Davidson AD, Gow NAR, Maiden MCJ, Odds FC. Candida orthopsilosis and Candida metapsilosis spp. nov. to replace Candida parapsilosis groups II and III. J Clin Microbiol. 2005; 43: 284–292. doi: 10.1128/JCM.43.1.284-292.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lockhart SR, Messer SA, Pfaller MA, Diekema DJ. Geographic distribution and antifungal susceptibility of the newly described species Candida orthopsilosis and Candida metapsilosis in comparison to the closely related species Candida parapsilosis. J Clin Microbiol. 2008; 46: 2659–2664. doi: 10.1128/JCM.00803-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cantón E, Pemán J, Quindós G, Eraso E, Miranda-Zapico I, Álvarez M, et al. ; FUNGEMYCA Study Group. Prospective multicenter study of the epidemiology, molecular identification, and antifungal susceptibility of Candida parapsilosis, Candida orthopsilosis, and Candida metapsilosis isolated from patients with candidemia. Antimicrob Agents Chemother. 2011; 55: 5590–5596. doi: 10.1128/AAC.00466-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gago S, García-Rodas R, Cuesta I, Mellado E, Alastruey-Izquierdo A. Candida parapsilosis, Candida orthopsilosis, and Candida metapsilosis virulence in the non-conventional host Galleria mellonella. Virulence. 2014; 5: 278–285. doi: 10.4161/viru.26973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen M, Zeng J, de Hoog GS, Stielow B, Gerrits van den Ende AH, Liao W, et al. The "species complex" issue in clinically relevant fungi: A case study in Scedosporium apiospermum. Fungal Biol. 2016; 120: 137–146. See comment in PubMed Commons below doi: 10.1016/j.funbio.2015.09.003 [DOI] [PubMed] [Google Scholar]
- 6.Nosek J, Holesova Z, Kosa P, Gacser A, Tomaska L. Biology and genetics of the pathogenic yeast Candida parapsilosis. Curr Genet. 2009; 55: 497–509. doi: 10.1007/s00294-009-0268-4 [DOI] [PubMed] [Google Scholar]
- 7.van Asbeck EC, Clemons KV, Stevens DA. Candida parapsilosis: a review of its epidemiology, pathogenesis, clinical aspects, typing and antimicrobial susceptibility. Crit Rev Microbiol. 2009; 35: 283–309. doi: 10.3109/10408410903213393 [DOI] [PubMed] [Google Scholar]
- 8.Bonfietti LX, Martins M dos A, Szeszs MW, Pukiskas SB, Purisco SU, Pimentel FC, et al. Prevalence, distribution and antifungal susceptibility profiles of Candida parapsilosis, Candida orthopsilosis and Candida metapsilosis bloodstream isolates. J Med Microbiol. 2012; 61: 1003–1008. doi: 10.1099/jmm.0.037812-0 [DOI] [PubMed] [Google Scholar]
- 9.Bonfietti LX, Szeszs MW, Chang MR, Martins MA, Pukinskas SR, Nunes MO, et al. Ten-year study of species distribution and antifungal susceptibilities of Candida bloodstream isolates at a Brazilian tertiary hospital. Mycopathologia. 2012; 174: 389–396. doi: 10.1007/s11046-012-9566-3 [DOI] [PubMed] [Google Scholar]
- 10.Hamajima K, Nishikawa A, Shinoda T, Fukazawa Y. Deoxyribonucleic acid base composition and its homology between two forms of Candida parapsilosis and Lodderomyces elongisporus. J Gen Appl Microbiol. 1987; 33: 299–302. [Google Scholar]
- 11.James SA, Collins MD, Roberts IN. The genetic relationship of Lodderomyces elongisporus to other ascomycete yeast species as revealed by small subunit rRNA gene sequences. Lett Appl Microbiol. 1994; 19: 308–311. [DOI] [PubMed] [Google Scholar]
- 12.Riccombeni A, Vidanes G, Proux-Wera E, Wolfe KH, Butler G. Sequence and analysis of the genome of the pathogenic yeast Candida orthopsilosis. PLOS One. 2012; 7: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van der Walt JP. Lodderomyces, a new genus of the Saccharomycetaceae. Antonie van Leeuwenhoek. 1966; 32: 1–5. [DOI] [PubMed] [Google Scholar]
- 14.Diezmann S, Cox CJ, Schönian G, Vilgalys RJ, Mitchell TG. Phylogeny and evolution of medical species of Candida and related taxa: a multigenic analysis. J Clin Microbiol. 2004; 42: 5624–5635. doi: 10.1128/JCM.42.12.5624-5635.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lockhart SR, Messer SA, Pfaller MA, Diekema DJ. Lodderomyces elongisporus masquerading as Candida parapsilosis as a cause of bloodstream infections. J Clin Microbiol. 2008; 46: 374–376. doi: 10.1128/JCM.01790-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ahmad S, Khan ZU, Johny M, Ashour NM, Al-Tourah WH, Joseph L, et al. Isolation of Lodderomyces elongisporus from the catheter tip of a fungemia patient in the Middle East. Case Rep Med. 2013; 2013: 560406 doi: 10.1155/2013/560406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Show full citationTaj-Aldeen SJ, AbdulWahab A, Kolecka A, Deshmukh A, Meis JF, Boekhout T. Uncommon opportunistic yeast bloodstream infections from Qatar. Med Mycol. 2014; 52: 552–556. doi: 10.1093/mmycol/myu016 [DOI] [PubMed] [Google Scholar]
- 18.Fernández-Ruiz M, Guinea J, Puig-Asensio M, Zaragoza Ó, Almirante B, Cuenca-Estrella M, et al. ; CANDIPOP Project; GEIH-GEMICOMED (SEIMC) and REIPI. Fungemia due to rare opportunistic yeasts: data from a population-based surveillance in Spain. Med Mycol. 2017; 55: 125–136. doi: 10.1093/mmy/myw055 [DOI] [PubMed] [Google Scholar]
- 19.Hatanaka S, Nakamura I, Fukushima S, Ohkusu K, Matsumoto T. Catheter-related bloodstream infection due to Lodderomyces elongisporus. Jpn J Infect Dis. 2016; 69: 520–522. doi: 10.7883/yoken.JJID.2015.307 [DOI] [PubMed] [Google Scholar]
- 20.Hull CM, Raisner RM, Johnson AD. Evidence for mating of the "asexual" yeast Candida albicans in a mammalian host. Science. 2000; 289: 307−310. [DOI] [PubMed] [Google Scholar]
- 21.Magee BB, Magee PT. Induction of mating in Candida albicans by construction of MTLa and MTLα strains. Science. 2000; 289: 310−313. [DOI] [PubMed] [Google Scholar]
- 22.Bennett RJ, Johnson AD. Completion of a parasexual cycle in Candida albicans by induced chromosome loss in tetraploid strains. EMBO J. 2003; 22: 2505‒2515. doi: 10.1093/emboj/cdg235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hickman MA, Zeng G, Forche A, Hirakawa MP, Abbey D, Harrison BD, et al. The "obligate diploid" Candida albicans forms mating-competent haploids. Nature. 2013; 494: 55‒59. doi: 10.1038/nature11865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hull CM, Johnson AD. Identification of a mating type-like locus in the asexual pathogenic yeast Candida albicans. Science. 1999; 285: 1271−1275. [DOI] [PubMed] [Google Scholar]
- 25.Butler G, Rasmussen MD, Lin MF, Santos MA, Sakthikumar S, Munro CA, et al. Evolution of pathogenicity and sexual reproduction in eight Candida genomes. Nature. 2009; 459: 657–662. doi: 10.1038/nature08064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Butler G. Fungal sex and pathogenesis. Clin Microbiol Rev. 2010; 23: 140−159. doi: 10.1128/CMR.00053-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sai S, Holland LM, McGee CF, Lynch DB, Butler G. Evolution of mating within the Candida parapsilosis species group. Eukaryot Cell. 2011; 10: 578–587. doi: 10.1128/EC.00276-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Soll DR. Why does Candida albicans switch? FEMS Yeast Res. 2009; 9: 973–989. doi: 10.1111/j.1567-1364.2009.00562.x [DOI] [PubMed] [Google Scholar]
- 29.Noble SM, Gianetti BA, Witchley JN. Candida albicans cell-type switching and functional plasticity in the mammalian host. Nature Rev Microbiol. 2017; 15: 96–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miller MG, Johnson AD. White-opaque switching in Candida albicans is controlled by mating-type locus homeodomain proteins and allows efficient mating. Cell. 2002; 110: 293–302. [DOI] [PubMed] [Google Scholar]
- 31.Anderson J, Mihalik R, Soll DR. Ultrastructure and antigenicity of the unique cell wall pimple of the Candida opaque phenotype. J Bacteriol. 1990; 172: 224–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laffrey SF, Butler G. Phenotype switching affects biofilm formation by Candida parapsilosis. Microbiology. 2005; 151: 1073‒1081. doi: 10.1099/mic.0.27739-0 [DOI] [PubMed] [Google Scholar]
- 33.Makower M, Bevan EA. The physiological basis of killer character in yeast. In: Goerts SJ, editor. Genetics Today. Proceedings of the XI International Congress on Genetics, vol 1. The Hague: MacMillan; 1963. pp. 202–203.
- 34.Woods DR, Bevan EA. Studies on the nature of the killer factor produced by Saccharomyces cerevisiae. J Gen Microbiol. 1968; 51: 115–126. doi: 10.1099/00221287-51-1-115 [DOI] [PubMed] [Google Scholar]
- 35.Bussey H. Effects of the yeast killer factor on sensitive cells. Nature New Biol. 1972; 235: 73–75. [DOI] [PubMed] [Google Scholar]
- 36.Bussey H. K1 killer toxin, a pore-forming protein from yeast. Mol Microbiol. 1991; 5: 2339–2343. [DOI] [PubMed] [Google Scholar]
- 37.Stark MJR, Boyd A, Mileham AJ, Romanos MA. The plasmid-encoded killer system of Kluyveromyces lactis: a review. Yeast. 1990; 6: 1–29. [DOI] [PubMed] [Google Scholar]
- 38.Morace G, Manzara S, Dettori G, Fanti F, Conti S, Campana L, et al. Biotyping of bacterial isolates using the killer system. Eur J Epidemiol. 1989; 5: 303–310. [DOI] [PubMed] [Google Scholar]
- 39.Robledo-Leal E, Elizondo-Zertuche M, Villarreal-Treviño L, Treviño-Rangel Rde J, García-Maldonado N, Adame-Rodríguez JM, et al. Killer behavior within the Candida parapsilosis complex. Folia Microbiol. 2014; 59: 503–506. [DOI] [PubMed] [Google Scholar]
- 40.Slater JL, Gregson L, Denning DW, Warn PA. Pathogenicity of Aspergillus fumigatus mutants assessed in Galleria mellonella matches that in mice. Med Mycol. 2011; 49 (suppl. 1): s107–113. [DOI] [PubMed] [Google Scholar]
- 41.Fuchs BB, Eby J, Nobile CJ, El Khoury JB, Mitchell AP, Mylonakis E. Role of filamentation in Galleria mellonella killing by Candida albicans. Microbes Infect. 2010; 12: 488–496. doi: 10.1016/j.micinf.2010.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mylonakis E, Moreno R, El Khoury JB, Idnurm A, Heitman J, Calderwood SB, et al. Galleria mellonella as a model system to study Cryptococcus neoformans pathogenesis. Infect Immun. 2005; 73: 3842–3850. doi: 10.1128/IAI.73.7.3842-3850.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sun S, Li Y, Guo Q, Shi C, Yu J, Ma L. In vitro interactions between tacrolimus and azoles against Candida albicans determined by different methods. Antimicrob Agents Chemother. 2008; 52: 409−417. doi: 10.1128/AAC.01070-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen YL, Lehman VN, Averette AF, Perfect JR, Heitman J. Posaconazole exhibits in vitro and in vivo synergistic antifungal activity with caspofungin or FK506 against Candida albicans. PLOS One. 2013; 8: e57672 doi: 10.1371/journal.pone.0057672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cruz MC, Goldstein AL, Blankenship JR, Del Poeta M, Davis D, Cardenas ME, et al. Calcineurin is essential for survival during membrane stress in Candida albicans. EMBO J. 2002; 21: 546–559. doi: 10.1093/emboj/21.4.546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li H, Zhang C, Chen Z, Shi W, Sun S. A promising approach of overcoming the intrinsic resistance of Candida krusei to fluconazole (FLC)-combining tacrolimus with FLC. FEMS Yeast Res. 2014; 14: 808−811. doi: 10.1111/1567-1364.12163 [DOI] [PubMed] [Google Scholar]
- 47.Denardi LB, Mario DA, Loreto ÉS, Santurio JM, Alves SH. Synergistic effects of tacrolimus and azole antifungal compounds in fluconazole-susceptible and fluconazole-resistant Candida glabrata isolates. Braz J Microbiol. 2015; 46: 125−129. doi: 10.1590/S1517-838246120120442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kubiça TF, Denardi LB, Azevedo MI, Oliveira V, Severo LC, Santurio JM, et al. Antifungal activities of tacrolimus in combination with antifungal agents against fluconazole-susceptible and fluconazole-resistant Trichosporon asahii isolates. Braz J Infect Dis. 2016; 20: 539−545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Clinical and Laboratory Standards Institute (CLSI). Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts; Approved Standard- Third Edition. CLSI document M27-A3, Wayne, Pennsylvania: Clinical and Laboratory Standards Institute, 2008.
- 50.Odds FC. Synergy, antagonism, and what the chequerboard puts between them. J Antimicrob Chemother. 2003; 52: 1 doi: 10.1093/jac/dkg301 [DOI] [PubMed] [Google Scholar]
- 51.Tascini C, Menichetti F, Bozza S, Del FA, Bistoni F. Evaluation of the activities of two-drug combinations of rifampicin, polymyxin B and ampicillin/sulbactam against Acinetobacter baumannii. J Antimicrob Chemother. 1998; 42: 270–271. [DOI] [PubMed] [Google Scholar]
- 52.Miyasaki Y, Morgan MA, Chan RC, Nichols WS, Hujer KM, Bonomo RA, et al. In vitro activity of antibiotic combinations against multidrug resistant strains of Acinetobacter baumannii and the effects of their antibiotic resistance determinants. FEMS Microbiol Lett. 2012; 328: 26–31. doi: 10.1111/j.1574-6968.2011.02480.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Odds FC, Bernaerts R. CHROMagar Candida, a new differential isolation medium for presumptive identification of clinically important Candida species. J Clin Microbiol. 1994; 32: 1923−1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pincus DH, Orenga S, Chatellier S. Yeast identification−past, present, and future methods. Med Mycol. 2007; 45: 97−121. doi: 10.1080/13693780601059936 [DOI] [PubMed] [Google Scholar]
- 55.Ozcan K, Ilkit M, Ates A, Turac-Bicer A, Demirhindi H. Performance of Chromogenic Candida agar and CHROMagar Candida in recovery and presumptive identification of monofungal and polyfungal vaginal isolates. Med Mycol. 2010; 48: 29−34. doi: 10.3109/13693780802713224 [DOI] [PubMed] [Google Scholar]
- 56.Guzel AB, Ilkit M, Akar T, Burgut R, Demir SC. Evaluation of risk factors in patients with vulvovaginal candidiasis and the value of chromID Candida agar versus CHROMagar Candida for recovery and presumptive identification of vaginal yeast species. Med Mycol. 2011; 49: 16−25. doi: 10.3109/13693786.2010.497972 [DOI] [PubMed] [Google Scholar]
- 57.Nielsen K, Heitman J. Sex and virulence of human pathogenic fungi. Adv Genet. 2007; 57: 143–173. doi: 10.1016/S0065-2660(06)57004-X [DOI] [PubMed] [Google Scholar]
- 58.Tsong AE, Miller MG, Raisner RM, Johnson AD. Evolution of a combinatorial transcriptional circuit: a case study in yeasts. Cell. 2003; 115: 389‒399. [DOI] [PubMed] [Google Scholar]
- 59.Tsong AE, Tuch BB, Li H, Johnson AD. Evolution of alternative transcriptional circuits with identical logic. Nature. 2006; 443: 415‒420. doi: 10.1038/nature05099 [DOI] [PubMed] [Google Scholar]
- 60.Pryszcz LP, Németh T, Saus E. The genomic aftermath of hybridization in the opportunistic pathogen Candida metapsilosis. PLOS Genet. 2015; 11: e1005626 doi: 10.1371/journal.pgen.1005626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Németh T1, Tóth A, Szenzenstein J, Horváth P, Nosanchuk JD, Grózer Z, et al. Characterization of virulence properties in the C. parapsilosis sensu lato species. PLOS One. 2013; 8: e68704 doi: 10.1371/journal.pone.0068704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ziccardi M, Souza LO, Gandra RM, Galdino AC, Baptista AR, Nunes AP, et al. Candida parapsilosis (sensu lato) isolated from hospitals located in the Southeast of Brazil: Species distribution, antifungal susceptibility and virulence attributes. Int J Med Microbiol. 2015; 305: 848–859. doi: 10.1016/j.ijmm.2015.08.003 [DOI] [PubMed] [Google Scholar]
- 63.Zekhnov AM, Soom YO, Nesterova GF. New test strains for detecting the antagonistic activity of yeasts. Mikrobiologiya. 1989; 58: 807–811. [Google Scholar]
- 64.Robledo-Leal E, Villarreal-Treviño L, González GM. Occurrence of killer yeasts in isolates of clinical origin. Trop Biomed. 2012; 29: 297–300. [PubMed] [Google Scholar]
- 65.Junqueira JC, Fuchs BB, Muhammed M, Coleman JJ, Suleiman JM, Vilela SF, et al. Oral Candida albicans isolates from HIV-positive individuals have similar in vitro biofilm-forming ability and pathogenicity as invasive Candida isolates. BMC Microbiol. 2011; 11: 247 doi: 10.1186/1471-2180-11-247 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
(XLSX)
Data Availability Statement
Our data are all contained within the paper and/or Supporting Information.