Abstract
Aims
Previous studies demonstrated poor public awareness of heart failure (HF) compared with myocardial infarction and stroke. With respect to several activities to improve HF awareness in recent years, we present data on the development of HF awareness and information sources in Germany over 8 years.
Methods and results
In 2007, 2012, and 2015, respectively, 2531, 359, and 171 respondents answered questions about causes, presentation, prognosis, and treatment of HF from a survey developed by the German Competence Network HF. Relationships between respondents' sociodemographic data and their HF knowledge were explored and changes in knowledge and use of information sources analysed. Sixty‐eight per cent of respondents knew HF as ‘weakness of the heart’. Seventy‐nine per cent knew shortness of breath, 74% reduced exercise tolerance, and 52% knew leg edema as symptoms. Only 40% knew all three symptoms. Although up to 34% of the respondents were directly or indirectly affected by HF, they demonstrated poor knowledge about severity and prognosis. Between 2007 and 2015, overall HF awareness has not changed; awareness about treatment has dropped significantly. Younger respondents used all media, especially internet, for information about health; older respondents preferred printed/verbal media and their physician.
Conclusions
We found rather insufficient public knowledge on HF etiology and symptoms but especially about management, severity, and prognosis, which is essential for good self‐care and adherence of patients. Heart failure awareness has not improved even though awareness campaigns were held over the years. It seems that especially older patients should be much more approached by their family physicians.
Keywords: Heart failure, Awareness, Prognosis, Health survey, Health literacy, Cardiovascular risk
Introduction
Heart failure (HF) is the fourth leading cause of death and the most common diagnosis leading to hospitalization in Germany.1 However, according to representative surveys, although 76–85% of the German population had heard of HF and many were able to identify symptoms of HF when presented separately (50–70%),2, 3, 4, 5 only about 3% could identify it from a description of typical symptoms (shortness of breath, fatigue, and swollen ankles) and showed better awareness about other severe diseases such as angina/myocardial infarction and transient ischemic attack/stroke.2 Furthermore, most respondents thought it had a better prognosis than cancer, and roughly 30% thought it was a natural part of the aging process.2 In 2013, 3086 beneficiaries of the German public health insurance provider DAK‐Gesundheit did not even rank HF among the top 10 diseases they feared most, with cancer, dementia, and stroke at the top.6 The disparity between the burden of disease and the public perception of it can lead to delays in diagnosis and appropriate care of HF. Indeed, symptoms are often present several years before the diagnosis of HF is made.7 Half of all patients have NYHA class III–IV symptoms at the time of first diagnosis and are referred to specialist care or hospitalized within one month.8 Higher NYHA class and hospitalization for HF are both markers of worse prognosis;9, 10 therefore, early detection and treatment are paramount. However, according to registry data from the United States, HF was previously undiagnosed in as many as a quarter of patients hospitalized for acute decompensation.11 This demonstrates the need to improve the awareness of HF among the general public. The above cited surveys showing that awareness was low did not however examine the factors associated with low awareness.
Therefore, the first main objective of the current study was to better characterize the impact of factors like educational and professional background, presence of HF in person or family, age, and gender on the level of HF awareness among a large population.
Second, as several efforts were made to improve HF awareness during recent years, we followed the development of HF awareness and the use of different information sources over this period starting in 2007 and investigated whether awareness campaigns have brought general improvement in HF awareness.
The results may guide future awareness campaigns and patient education efforts.
Methods
Study sample and data collection
Study participants came from a convenient random sample of visitors attending the national ‘Health Research Day’ of the German Federal Ministry of Education and Research in Berlin, Marburg, Essen, Hannover, Göttingen, Heidelberg, and Lübeck on 25 February 2007, and the ‘Long night of the Sciences’ at the Charité Medical University in Berlin in 2012 and 2015. Thus, participants were a sample of people who are most probably interested in health issues. They were approached by study personnel and filled out the paper‐based 22‐item survey about HF. Participation was voluntary, confidential, and anonymous. Inclusion criteria were being adult (≥18 years of age) and proficient in German, as judged by study personnel. The questionnaire was developed using expert consensus by the German Competence Network HF based on the experience with a questionnaire on knowledge about cardiovascular emergencies in Berlin by Baumann et al.; it has not been additionally validated.12 The survey took 3–5 min to complete. It contained five demographic items to characterize the study population and determine generalizability but no identifying information, five dichotomous (Yes/No) questions to ascertain the subject's previous experience with the medical profession and heart disease, particularly HF, one categorical question to determine how subjects obtain information about health issues, and 10 multiple‐choice questions about HF (seven about epidemiology, symptoms, and causes and three about treatment and prognosis).
Statistical analysis
Baseline variables are presented as frequencies and percentages for nominal variables, or means and standard deviations for continuous variables. For longitudinal analysis, data were adjusted for age, sex, education level, medical profession, and presence of HF total (i.e. respondent or family member), as these factors differed between years. Adjusted scores were normalized based on per cent rank transformation with a mean of 100 and standard deviation of 15 (comparable to IQ scaling). An ordinal logistic regression was calculated with the baseline data from 2007 for the scores that can be deduced from the answers to the questions shown in Table 2.
All variables found to be relevant at baseline showed significant variation between surveys at the different time points. Thus, any difference between years could have reflected real increase/decrease in knowledge or changes in sample composition. Therefore, scores were adjusted in a multivariate linear model adjusting for age, sex, education level, medical profession, and presence of HF total.
All analyses were considered exploratory; thus, no adjustments were made for multiple testing. Statistical analysis was performed with IBM SPSS Statistics software version 20.
Results
Sample characteristics at baseline
In 2007, 2531 respondents [53% women; median age 54 (quartiles: 38/66) years, 29% ≥65 years] completed the HF awareness survey. Seventeen per cent of respondents worked in the medical profession, 31% had a university education, and 34% of respondents were directly or indirectly (i.e. a family member was) affected by HF (Table 1). Participants above 65 years of age (P = 0.001), male (P = 0.001), without an academic degree (P = 0.011), or not employed in a medical field (P = 0.001) were significantly more likely to be affected by HF themselves. Respondents with HF were also significantly more likely to have family members affected by HF (P = 0.001) (data not shown).
Table 1.
Sample characteristics at baseline (2007)
| Variable | Levels | Total in n (%) n = 2531 (100%) |
|---|---|---|
| Age | <65 years | 1791 (71%) |
| ≥65 years | 740 (29%) | |
| Gender | Men | 1191 (47%) |
| Women | 1324 (53%) | |
| Education level | University graduate | 734 (31%) |
| Non‐academic | 1598 (69%) | |
| Place of origin | Former FRG | 1626 (67%) |
| Former GDR | 703 (29%) | |
| Other | 98 (4%) | |
| Hannover | 265 | |
| Göttingen | 581 | |
| Heidelberg | 28 | |
| Essen | 61 | |
| Berlin | 1386 | |
| Marburg | 76 | |
| Lübeck | 134 | |
| Medical profession | Yes | 416 (17%) |
| No | 2010 (83%) | |
| Presence of HF in respondent | Yes | 742 (29%) |
| No | 1662 (66%) | |
| Don't know | 127 (5%) | |
| Presence of HF in family member | Yes | 573 (23%) |
| No | 1733 (69%) | |
| Don't know | 211 (8%) | |
| Presence of HF total | Yes | 864 (34%) |
| No/Don't know | 1659 (66%) |
FRG, Federal Republic of Germany; GDR, German Democratic Republic; HF, heart failure.
Awareness about heart failure
As shown in Table 2, 73% of respondents knew HF, and 68% knew that it was a failure of the heart. Regarding the symptoms of HF, 79% identified shortness of breath, 74% identified reduced effort tolerance, and 52% identified leg edema. All three symptoms were identified by 40% of participants. The fact that HF is one of the most common diseases in internal medicine was familiar to 67% of respondents, and 57% knew that HF is most common among adults above 65 years. Respondents knew more about HF treatment than about its prognosis: 74% of respondents knew that lifelong treatment with medicines is necessary in most cases, 19% thought HF was healed after at least one month of treatment, 30% thought HF could only be healed through surgery, and 24% did not know about the course of HF. The correct statement that HF is as bad as malignant cancer was identified by 25% of participants. Eighty per cent of respondents were aware that a healthy lifestyle could reduce their risk of HF (Table 2).
Table 2.
Awareness about HF as answers to the different questions (number and percentage of all respondents in 2007), bold = correct
| Question | Frequency in n (%) |
|---|---|
| Which of the following diseases do you know? | |
| AIDS | 2327 (92%) |
| Heart failure (HF) | 1843 (73%) |
| Coronary heart disease (CHD) | 1768 (70%) |
| Bronchial carcinoma | 1523 (60%) |
| None | 57 (2%) |
| What is the meaning of HF? | |
| Disturbed blood flow in the heart muscle | 671 (27%) |
| Defect of the heart valves | 355 (14%) |
| Failure of the heart | 1726 (68%) |
| Elevated blood pressure | 313 (12%) |
| I don't know | 283 (11%) |
| Which disease/diseases can lead to HF? | |
| Heart attack | 1394 (55%) |
| Defect of the heart valves | 1361 (54%) |
| Elevated blood pressure | 1719 (68%) |
| Stroke | 695 (27%) |
| I don't know | 191 (8%) |
| What are typical symptoms or signs of HF? | |
| Shortness of breath under strain | 1987 (79%) |
| Accumulation of water in the legs | 1314 (52%) |
| Weakness of physical performance | 1866 (74%) |
| Pain in right upper arm | 490 (19%) |
| I don't know | 175 (7%) |
| Which is the most common cause for HF? | |
| Disease of the heart's coronary blood vessels with disturbed blood flow | 1801 (71%) |
| Lack of sleep | 60 (2%) |
| Genetic endowments | 347 (14%) |
| Weight loss | 53 (2%) |
| I don't know | 258 (10%) |
| How is HF caused? | |
| By a pumping failure of the heart | 1535 (61%) |
| By the blockage of a brain vessel with a blood clot | 142 (6%) |
| By the blockage of a venous valve | 296 (12%) |
| By overweight | 276 (11%) |
| I don't know | 275 (11%) |
| What is the frequency of HF in the population? | |
| There are only single cases | 101 (4%) |
| It is very rare (less than 0.1%) | 116 (5%) |
| It is one of the most common diseases in internal medicine | 1685 (67%) |
| Almost everyone will be affected in the course of life | 309 (12%) |
| I don't know | 307 (12%) |
| Which age group is especially affected by HF? | |
| Children of up to 12 years | 46 (2%) |
| Adolescents of up to 18 years | 35 (1%) |
| Adults of up to 50 years | 808 (32%) |
| Adults above 65 years | 1435 (57%) |
| I don't know | 206 (8%) |
| How is the course of HF? | |
| HF mostly goes away by itself | 52 (2%) |
| It is healed after at least one month of treatment | 486 (19%) |
| It is about as bad as malignant cancer diseases | 629 (25%) |
| It can only be healed through surgery | 754 (30%) |
| I don't know | 594 (24%) |
| What can I do to reduce my risk of developing HF? | |
| Healthy diet | 152 (6%) |
| Sufficient physical exercises | 165 (7%) |
| Not smoke | 122 (5%) |
| All the above measures | 2027 (80%) |
| I don't know | 59 (2%) |
| What are the treatment options for HF? | |
| There is no treatment | 60 (2%) |
| Always strict bed rest for several months | 57 (2%) |
| Diet | 212 (9%) |
| Mostly, lifelong treatment with medicines | 1844 (74%) |
| I don't know | 318 (13%) |
Factors influencing awareness
In the linear model, most grouping variables had a consistent impact on the knowledge scores even when each was corrected for the impact of all others. Table 3 presents how the variables influence the three overall scores for awareness about HF causes and treatment specifically and awareness in total. Female respondents, respondents with a university degree, those who worked in the medical field, and respondents affected directly or indirectly by HF showed significantly higher scores for total awareness as well as for causes and treatment separately (P < 0.023).
Table 3.
Sample characteristics and HF awareness scores depending on different variables (univariate analysis with Kruskal–Wallis test). In the linear model, most grouping variables have consistent impact on knowledge scores. Direction of effects was further explored using univariate analyses
| Group | Awareness causes | P‐value | Awareness treatment | P‐value.1 | Total score | P‐value.2 |
|---|---|---|---|---|---|---|
| Age | ||||||
| <65 years | 97 ± 13 | 0.745 | 94 ± 12.5 | 0.931 | 98 ± 13.7 | 0.388 |
| ≥65 years | 98 ± 11.9 | 93 ± 11.8 | 99 ± 12.3 | |||
| Gender | ||||||
| Men | 97 ± 12.4 | 0.007 | 93 ± 12.3 | 0.023 | 98 ± 13.0 | 0.015 |
| Women | 98 ± 12.8 | 94 ± 12.3 | 99 ± 13.5 | |||
| Educational level | ||||||
| University graduate | 100 ± 11.8 | 0.001 | 96 ± 12.3 | 0.001 | 102 ± 12.6 | 0.001 |
| Non‐academic | 96 ± 12.7 | 93 ± 12.1 | 97 ± 13.1 | |||
| Medical profession | ||||||
| Yes | 107 ± 11.2 | 0.001 | 99 ± 12.0 | 0.001 | 108 ± 12.3 | 0.001 |
| No | 96 ± 12.1 | 93 ± 12.1 | 96 ± 12.6 | |||
| Presence of HF total | ||||||
| Yes | 99 ± 11.3 | 0.001 | 95 ± 11.5 | 0.001 | 100 ± 11.8 | 0.001 |
| No/Don't know | 96 ± 13.2 | 93 ± 12.7 | 97 ± 13.9 | |||
| City | ||||||
| Berlin | 96 ± 11.8 | 94 ± 11.7 | 97 ± 12.3 | |||
| Marburg | 102 ± 12.3 | 93 ± 14.3 | 101 ± 12.7 | |||
| Hannover | 99 ± 14.0 | 92 ± 13.3 | 99 ± 14.8 | |||
| Göttingen | 98 ± 13.7 | 94 ± 12.9 | 99 ± 14.5 | |||
| Heidelberg | 93 ± 13.1 | 85 ± 11.8 | 92 ± 13.2 | |||
| Essen | 101 ± 13.4 | 96 ± 12.1 | 103 ± 14.2 | |||
| Lübeck | 103 ± 10.4 | 97 ± 12.1 | 104 ± 11.9 |
Sample characteristics in 2012 and 2015
In 2012, 359 respondents completed the HF awareness survey (60% women, 8% ≥65 years, 48% from former Western Germany, 1% from abroad, 63% with university education, 21% in medical profession). Seventy‐two per cent of respondents had heard of HF prior to the survey, and 36% knew all three main symptoms of HF as described above. Six per cent of the respondents reported having a family member with HF. Six per cent knew themselves to be affected, 90% knew not to be or did not know.
In 2015, 171 respondents completed the HF awareness survey (59% women, 8% ≥65 years, 48% from former Western Germany, 13% from abroad, 63% with university education, 29% in medical profession). Most of the respondents (79%) had heard of HF prior to the survey, and 35% knew all three symptoms of HF. Having a family member with HF was reported by 7% of respondents, 6% knew themselves to be affected, 92% knew not to be or did not know.
Changes in awareness about heart failure through the years
All variables found to be relevant at baseline showed significant variation between surveys at the different time points. Thus, any difference between years could have reflected real increase/decrease in knowledge or just changes in sample composition. Therefore, scores were adjusted in a multivariate linear model adjusting for age, gender, education level, medical profession, and presence of HF total. Figure 1 shows the development of the scores for awareness about HF causes, HF treatment, and overall awareness. The scores were normalized based on per cent rank transformation with a mean of 100 compared with the total awareness at baseline. Over time, the overall awareness and awareness about HF causes did not change significantly. The awareness about treatment of HF has worsened slightly but significantly between the years 2007 and 2015.
Figure 1.
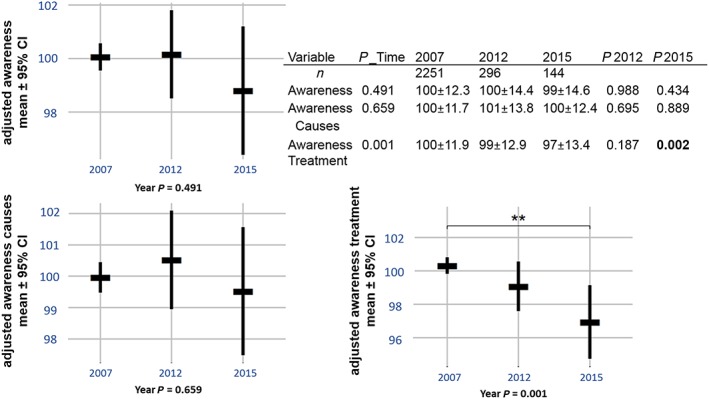
Development of the three awareness scores over time after adjustment for age, gender, education, medical profession, and presence of HF total. Due to adjustment, the n have been reduced to the numbers given in the figure. P‐values are given for development of scores overall (P_Time) and for changes between 2007 vs. 2012 (P2012) and 2007 vs. 2015 (P2015). ** P < 0.01.
Sources of information about health and cardiovascular risk
Figure 2 shows to which extent the respondents used different media at different time points. In 2007, the most common sources of information about health and cardiovascular risk were printed media, i.e. magazines and newspapers (54%), and TV/radio (51%). Forty‐one per cent of respondents gained information from their general practitioner. Friends and family as well as the Internet followed with 26% each. This behaviour drastically changed over the years. The Internet has become the top information source by 2015 (50%), and the use of print media and TV/radio dropped to around 45% after 2012. Whereas in 2007, the family doctor had been an important source for 41% of respondents, in 2012 and 2015, only around 31% got their information there. Information seeking from friends and family increased by 11% since 2007.
Figure 2.
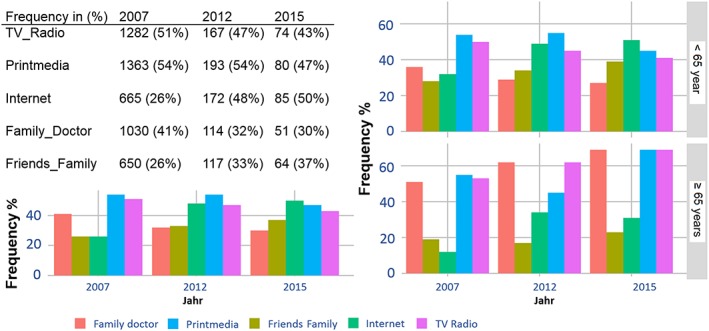
Sources of information in %. The left panel shows the overall information seeking behaviour; the right panel shows the differences between people <65 years and ≥65 years.
The information sources were used with very different frequencies by the two age groups <65 years and ≥65 years, and this discrepancy increased over the years. In 2015, respondents over 65 relied on TV/radio, printed media, and on their family doctor (69% for each); they used the internet much less than the younger respondents (31%) and were less reliant on friends and family (23%). The younger respondents used the information sources with more evenly distributed frequencies: internet at 51%, friends and family 39%, printed media 45%, TV/radio 41%, and their general practitioner at 27%.
In 2007, almost all respondents (86%) agreed that more public education efforts about HF are needed.
Discussion
This largest German survey on HF awareness to date aimed to better characterize the knowledge about HF symptoms, causes, treatment, and prognosis, to follow its development over a period of several years with awareness campaigns and to examine the information sources used by the participants.
Our study revealed a fair amount of knowledge about causes, risks, prevention and treatment strategies of HF, and poor knowledge about the prognosis and severity of HF. These results were comparable to earlier studies,2, 4 although the percentage of respondents, who knew all three main symptoms of HF, has strongly increased from only 3% reported for the 912 Germans from the population‐based survey study SHAPE conducted in 20022 to 39% in our study. This huge increase in percentage may also partially stem from a selection bias, as people in the present study can be suspected to be interested in health issues and were picked on a health information event at a university. However, 39% still seems to be a very low number for the awareness of a major disease.
The SHAPE study reported an overall poor HF awareness in Europeans with one‐third of respondents believing that HF was a natural consequence of aging.2, 4 Not having asked the exact same question, still one‐third of our population thought that people under 50 years were mostly affected by HF. On the other hand, 57% knew this is actually true for people older than 65, and 67% knew that HF is one of the most common diseases in internal medicine. But only 25% of our participants knew that the course of HF is as bad as that of malignant cancer. Thus, our respondents demonstrated a similarly poor understanding of HF severity and prognosis as the SHAPE respondents, where only 29% thought it was a severe condition and two‐thirds thought the prognosis was better than cancer (patients with HF live longer). Although one in five individuals will develop HF over the course of his or her lifetime, the SHAPE respondents underestimated its prevalence with only half of them knowing that HF was more common than cancer.2, 13
Thus, HF knowledge does not seem to have improved considerably over the years.
One factor that determined which types of information sources were used to obtain information about health and cardiovascular risk was age. Younger respondents used all media, but especially the internet, more frequently than their physicians, whereas older participants relied for the most part on printed and verbal media and on their general physicians. Additionally, these differences seem to have become greater over the years and can be inferred to be important when planning any future informational activity for the public.
Although it is encouraging that working in health care or being affected by HF indicated a better HF awareness in our sample, there is reason for concern. First, all participants demonstrated poor knowledge of HF prognosis. Second, lower awareness among non‐medical, non‐diagnosed individuals may lead to late presentation and treatment of HF due to a misinterpretation of the symptoms or misunderstanding of their severity. Previous studies of HF have shown that lower anxiety scores and false interpretation of early symptoms are associated with a longer duration of dyspnea and delays in seeking care.14, 15 Similarly, a large cohort study found that low health literacy, defined as the ability to ‘obtain, understand and process basic health information’ especially in printed form, was independently associated with higher all‐cause mortality in HF.16, 17 This is pertinent because many respondents in our study relied heavily on print media, such as newspapers and magazines, for information about their health and cardiovascular risk. A recent systematic review of health literacy also found it to be consistently associated to frequent hospitalizations, greater mortality, and global health status. Furthermore, individuals with lower health literacy were less likely to exhibit health seeking behaviours, such as participation in cancer screening, scheduled immunizations, or taking medications as prescribed.18
There are some limitations to the present study. First, one limitation of the questionnaire used may be the mode of its development as expert consensus without validation. A subdivision into subscales as could, for example, be examined using factorial analysis and subsequent calculation of internal consistency, etc. was not intended. However, determination of sensitivity to change could be of interest in the present context. Second, our convenience sample does not allow generalized conclusions to be drawn about the level of public HF awareness among the German population, as a selection bias may be inherent due to the setting of the survey and the failure to obtain a response rate. Also, the comparably lower number of participants in 2015 may enter a selection bias into the current results even though a multivariate model has been used in order to exclude any influence of variables such as differing age, educational background, or gender. Other possible variables with an influence on awareness on which data were not collected can, however, not be completely excluded. Such variables could be unevenly distributed in the populations at the different time points and therefore have a stronger or slighter impact in different years' populations, biasing the results. Indeed, although similar to the German population regarding the distribution of age and gender, a greater proportion of our sample had higher education, worked in a medical profession, and were more frequently affected by HF.2, 19, 20, 21, 22, 23
As discussed above, our study and others have found these factors to be associated with greater health awareness, which makes it all the more surprising that respondents should show such poor knowledge about HF prognosis. Although Störk et al. have very recently shown that hearing about HF may lower the ‘prevalence of common misbeliefs’,4 it would seem that greater health literacy does not automatically translate into better perception about the natural course of HF and the associated high mortality risk.
Active knowledge about HF is essential for the appropriate and early recognition of symptoms and thus for earlier treatment and possibly changes of lifestyle. It can also help relatives and friends to develop more understanding for their affected loved ones and thus to be more supportive and also aware of changes regarding their health.
We recommend health education programs adjusted to the needs of older patients, for example courses about healthy lifestyle and symptoms of illnesses offered by health insurances, hospitals, adult education centres, and community centres. Further, as this is a measure of primary prevention and as such in favour of long‐term public health as well as finances, family physicians should be given the option to prescribe health education courses.
The current study has shown that the overall awareness about HF has not increased since 2007 and is overall not at a satisfactory level. This could possibly lead to delays in the timely diagnosis and treatment of this condition. Thus, it is feasible to conclude, that more educational advertising should be implemented and also tested for effectiveness. Future awareness campaigns have to use all available media channels in an age‐appropriate way. Especially older patients should be approached through print media, television and radio, and, importantly, by their family physicians in person.
Conflict of interest
None declared.
Funding
This study received financial support from the Competence Network HF, funded by the Federal Ministry of Education and Research (BMBF), FKZ 01GI0205.
Zelenak, C. , Radenovic, S. , Musial‐Bright, L. , Tahirovic, E. , Sacirovic, M. , Lee, C.‐B. , Jahandar‐Lashki, D. , Inkrot, S. , Trippel, T. D. , Busjahn, A. , Hashemi, D. , Wachter, R. , Pankuweit, S. , Störk, S. , Pieske, B. , Edelmann, F. , and Düngen, H.‐D. (2017) Heart failure awareness survey in Germany: general knowledge on heart failure remains poor. ESC Heart Failure, 4: 224–231. doi: 10.1002/ehf2.12144.
References
- 1. DESTATIS Statistisches Bundesamt . Die 10 häufigsten Todesursachen insgesamt_Sterbefälle insgesamt nach der ICD‐10 im Jahr 2014. http://www.gbe‐bund.de/oowa921‐install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=3&p_aid=92618646&nummer=516&p_sprache=D&p_indsp=4065&p_aid=97444059 (2 March 2017).
- 2. Remme WJ, McMurray JJ, Rauch B, Zannad F, Keukelaar K, Cohen‐Solal A, Lopez‐Sendon J, Hobbs FD, Grobbee DE, Boccanelli A, Cline C, Macarie C, Dietz R, Ruzyllo W. Public awareness of heart failure in Europe: first results from SHAPE. Eur Heart J 2005; 26: 2413–2421. [DOI] [PubMed] [Google Scholar]
- 3. Neumann T, Biermann J, Erbel R, Neumann A, Wasem J, Ertl G, Dietz R. Heart failure: the commonest reason for hospital admission in Germany: medical and economic perspectives. Dtsch Arztebl Int 2009; 106: 269–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Störk S, Kavoliuniene A, Vinereanu D, Ludwig R, Seferovic P, Dickstein K, Anker SD, Filippatos G, Ponikowski P, Lainscak M. What does the lay public know about heart failure? Findings from the Heart Failure Awareness Day Initiative. Eur J Heart Fail 2016; 18: 66–70. [DOI] [PubMed] [Google Scholar]
- 5. Christ M, Störk S, Dörr M, Heppner HJ, Müller C, Wachter R, Riemer U, Trend HF Germany Project . Heart failure epidemiology 2000–2013: insights from the German Federal Health Monitoring System. Eur J Heart Fail 2016; 18: 1009–1018. [DOI] [PubMed] [Google Scholar]
- 6. Forsa , Gesellschaft für Sozialforschung und statistische Analysen mbH. http://www.dak.de/dak/download/Forsa‐Umfrage_Demenz‐1331362.pdf (29 June 2017).
- 7. Steinhubl S, Sun J, Vijayakrishnan R, Byrd R, Daar Z, Gotz D, Ebadollahi S, Stewart W. A3‐2: the signs and symptoms of heart failure are frequently documented to wax and wane in the years prior to a clinical diagnosis of heart failure: data from 4,644 patients followed in primary care. Clin Med Res 2013; 11: 134–135. [Google Scholar]
- 8. Johansson S, Wallander MA, Ruigomez A, Garcia Rodriguez LA. Incidence of newly diagnosed heart failure in UK general practice. Eur J Heart Fail 2001; 3: 225–231. [DOI] [PubMed] [Google Scholar]
- 9. Ahmed A. A propensity matched study of New York Heart Association class and natural history end points in heart failure. Am J Cardiol 2007; 99: 549–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gheorghiade M, Vaduganathan M, Fonarow GC, Bonow RO. Rehospitalization for heart failure: problems and perspectives. J Am Coll Cardiol 2013; 61: 391–403. [DOI] [PubMed] [Google Scholar]
- 11. Adams KF Jr, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, Berkowitz RL, Galvao M, Horton DP, ADHERE Scientific Advisory Committee and Investigators . Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J 2005; 149: 209–216. [DOI] [PubMed] [Google Scholar]
- 12. Baumann G, Stangl V, Grohmann A, Schink T, Wernecke K‐D. What do German citizens know about cardiovascular emergencies? Results of a survey conducted among 2000 Germans concerning coronary risk factors, symptom complexes of angina pectoris and acute myocardial infarction. Intensivmed 2003; 40: 590. doi:10.1007/s00390‐003‐0443‐7.200. [Google Scholar]
- 13. Lloyd‐Jones DM, Larson MG, Leip EP, Beiser A, D'Agostino RB, Kannel WB, Murabito JM, Vasan RS, Benjamin EJ, Levy D, Framingham Heart Study . Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation 2002; 106: 3068–3072. [DOI] [PubMed] [Google Scholar]
- 14. Jurgens CY, Hoke L, Byrnes J, Riegel B. Why do elders delay responding to heart failure symptoms? Nurs Res 2009; 58: 274–282. [DOI] [PubMed] [Google Scholar]
- 15. Jurgens CY. Somatic awareness, uncertainty, and delay in care‐seeking in acute heart failure. Res Nurs Health 2006; 29: 74–86. [DOI] [PubMed] [Google Scholar]
- 16. Nielsen‐Bohlmann L., Panzer A. M., Kindig D. A., eds. Health Literacy: A Prescription to End Confusion. Institute of Medicine (US) Committee on Health Literacy; Washington (DC): National Academies Press (US); 2004. [PubMed] [Google Scholar]
- 17. Peterson PN, Shetterly SM, Clarke CL, Bekelman DB, Chan PS, Allen LA, Matlock DD, Magid DJ, Masoudi FA. Health literacy and outcomes among patients with heart failure. JAMA 2011; 305: 1695–1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011; 155: 97–107. [DOI] [PubMed] [Google Scholar]
- 19. DESTATIS Statistisches Bundesamt . https://www.destatis.de/DE/Publikationen/Thematisch/BildungForschungKultur/Bildungsstand/BildungsstandBevoelkerung5210002157004.pdf (27 May 2016).
- 20. DESTATIS Statistisches Bundesamt . Bundesamt DS (2011) Statistisches Jahrbuch Statistisches Bundesamt, Wiesbaden. https://www.destatis.de/DE/Publikationen/StatistischesJahrbuch/Jahrbuch2008.pdf (19 November 2013).
- 21. DESTATIS Statistisches Bundesamt . Bundesamt DS (2008) Bevölkerung und Erwerbstätigkeit. Mikrozensus Stand und Entwicklung der Erwerbstätigkeit Band 2: Deutschland 2007. Statistisches Bundesamt, Wiesbaden 2008. https://www.destatis.de/DE/Publikationen/Thematisch/Arbeitsmarkt/Erwerbstaetige/StandEntwicklungErwerbstaetigkeitBandII2010411077424.pdf (19 November 2013).
- 22. Tiller D, Russ M, Greiser KH, Nuding S, Ebelt H, Kluttig A, Kors JA, Thiery J, Bruegel M, Haerting J, Werdan K. Prevalence of symptomatic heart failure with reduced and with normal ejection fraction in an elderly general population—the CARLA study. PLoS One 2013; 8: e59225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Roger VL, Go AS, Lloyd‐Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. 2012; 125: e2‐e220. [DOI] [PMC free article] [PubMed] [Google Scholar]


