Abstract
In conventional fundus imaging devices, transpupillary illumination is used for illuminating the inside of the eye. In this method, the illumination light is directed into the posterior segment of the eye through the cornea and passes the pupillary area. As a result of sharing the pupillary area for the illumination beam and observation path, pupil dilation is typically necessary for wide-angle fundus examination, and the field of view is inherently limited. An alternative approach is to deliver light from the sclera. It is possible to image a wider retinal area with transcleral-illumination. However, the requirement of physical contact between the illumination probe and the sclera is a drawback of this method. We report here trans-palpebral illumination as a new method to deliver the light through the upper eyelid (palpebra). For this study, we used a 1.5 mm diameter fiber with a warm white LED light source. To illuminate the inside of the eye, the fiber illuminator was placed at the location corresponding to the pars plana region. A custom designed optical system was attached to a digital camera for retinal imaging. The optical system contained a 90 diopter ophthalmic lens and a 25 diopter relay lens. The ophthalmic lens collected light coming from the posterior of the eye and formed an aerial image between the ophthalmic and relay lenses. The aerial image was captured by the camera through the relay lens. An adequate illumination level was obtained to capture wide angle fundus images within ocular safety limits, defined by the ISO 15004-2: 2007 standard. This novel trans-palpebral illumination approach enables wide-angle fundus photography without eyeball contact and pupil dilation.
Keywords: Fundus examination, ophthalmoscopy, retinal imaging, wide-field, fundus camera, transscleral illumination, pars plana
1. INTRODUCTION
It is known that wide angle fundus photography is essential for screening, diagnosis and treatment evaluation of eye diseases such as diabetic retinopathy, retinopathy of prematurity, intraorbital neoplasms, and choroidal dystrophies. Wide field fundus photography can also be readily used in telemedicine consultation. [1–5]. However, it is technically difficult to construct wide angle fundus imagers, due to the complication of illumination and imaging mechanisms. In conventional fundus imaging devices, illuminating the inside of the eye is performed with a transpupillary illumination method [4]. In this method, the light source is directed into the posterior segment of the eye through the cornea and passes the pupillary area and crystalline lens and vitreous of the eye. As first described by Gullstrand, the ray bundles used for illumination and observation should be separated on the cornea and on the first surface of the crystalline lens in the transpupillary illumination method. Otherwise, it is impossible to observe the retina because of light reflection and scattering from these areas [6]. The widest retinal area captured in a single photograph by transpupillary illumination is limited due to the nature of the technique. In this technique, a ring shaped peripheral corneal area is used by the illumination light. The remaining central corneal area is used for observing the retina. The border of the central cornea limits the amount of capture of the incident retinal rays to form an image. Rays coming from the peripheral retina cannot be captured by imaging optics because the corresponding corneal area is occupied by the illuminating ring [7]. In fact, transpupillary illumination uses nearly half of the pupil area and corresponding corneal and crystalline lens layers. Therefore, pupil dilation is typically required for transpupillary illumination to ensure the necessary field of view.
Instead of flood transpupillary illumination, Optos Camera (Optos, PLC, Dunfermline, UK) uses a single-point light scanning approach to achieve wide angle photography. Optos can image 200 degrees of the retina using a confocal scanning laser and ellipsoid mirror system. Optos uses two laser wavelengths (532 nm and 633 nm) to create a color image. The high cost of the Optos limits its access in rural and underserved areas [8]. Low posterior pole resolution and peripheral distortion of the image make it difficult for reliabel assessment of disease assocated morphological changes in these areas.
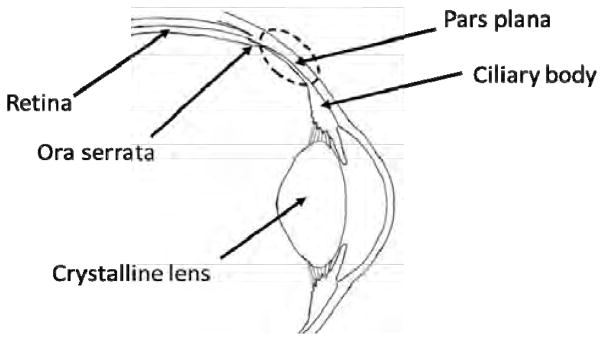
Transscleral illumination is an alternative approach to achieve wide angle photography. The ciliary body extends forward from the anterior end of the choroid to the root of the iris. It consists of a corrugated anterior zone, the pars plicata, and a flattened posterior zone, the pars plana (Figure 1). The pars plana extends anteriorly from the ora serrata. The ora serrata is the serrated peripheral margin where the retina ends [9]. Light transmission of the pars plana and adjacent sclera is better than any other scleral part of the eye. In other words, it is nearly impossible to obtain a natural image of the retina by illumination from other parts of the sclera instead of the pars plana. Transscleral illumination was first presented by Pomerantzeff in 1975. He showed that fiber optic bundle placement in the pars plana region of the sclera provides uniform, diffuse and adequate illumination for examining and photographing the interior of the eye. He emphasized the significantly high optical transmission of light from the pars plana compared to other scleral regions and preferred this area to illuminate the inside of the eye [10]. In 2002, a wide field retinal imaging system, based on trans-scleral illumination, called Panoret-1000, was put on the market. It produced excellent images of the retina with high resolution and natural color. Panoret was able to image the retina from the optic disc to the ora serrata in a single-shot measurement. With the advantage of trans-scleral illumination, it was possible to image the retina of patients with small pupils, cataracts, or an intraocular lens implant. Although the Panoret-1000 has been used successfully in ocular centers, it is no longer commercially available. Its clinical deployment failed due to the logistics of obtaining the retinal image. The camera and light system were apart from each other in the Panoret-1000. To capture a retinal image, one hand was used to hold the camera and the other hand was used to hold the light at the same time. The need to simultaneously use both hands results in difficult operation of the device [3]. The requirement of physical contact between the illumination system and sclera is another drawback of this method.
Figure 1.
Anatomical illustration of the pars plana
In this study, we developed a new technique by delivering light through the upper eyelid (palpebra) for wide angle fundus photography [11]. This novel trans-palpebral illumination approach enables wide-angle fundus photography without eyeball contact and pupil dilation.
2. MATERIALS AND METHODS
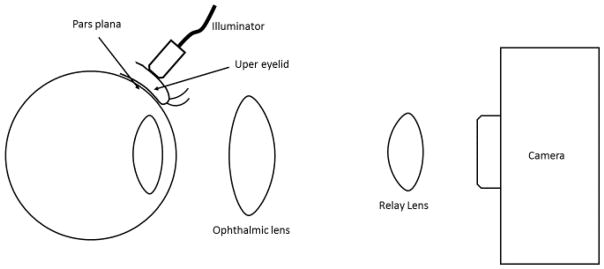
This study was approved by the Institutional Review Board of the University of Illinois at Chicago and was in compliance with the Declaration of Helsinki. Figure 2 shows a schematic diagram of the trans-palpebral illumination imaging system. A custom made adaptor was attached to a Sony Alpha a5100 mirrorless digital camera. The adaptor consists of one ophthalmic lens (Volk 90D, Volk Optical Inc) and one relay lens (25D achromatic doublets, Thorlabs) housed in the tube system. The ophthalmic lens collects light coming from the eye and forms an aerial image between the ophthalmic and relay lenses. The aerial image is captured by the camera through the relay lens. The focusing system of the camera lens was set to the manual focusing mode. The photographs were captured when the optic disc and central retinal area were optimally focused. During the experiment, the eye was illuminated with a warm white LED light (Thorlabs Inc.) through the palpebra. A 1.5 mm diameter fiber was used to illuminate the palpebra. The field of view of the imaging system was calculated based on ISO 10940:2009 [12]. A target placed at 1 m from the imaging device was used to measure the corresponding external angle of the imaging system.
Figure 2.
Schematic diagram of the trans-palpebral illumination imaging system
3. RESULTS
Figure 3 shows a fundus image captured from a subject who had no ocular pathology. The optic disc, including both cup and disc, was clearly identified in the image. Similarly, the macula and blood vessels were unambiguously observed. Retinal arteries that have a maximum diameter of 80 μm near the optic disc and 50 μm at midperiphery of the retina were unambiguously observed.
Figure 3.
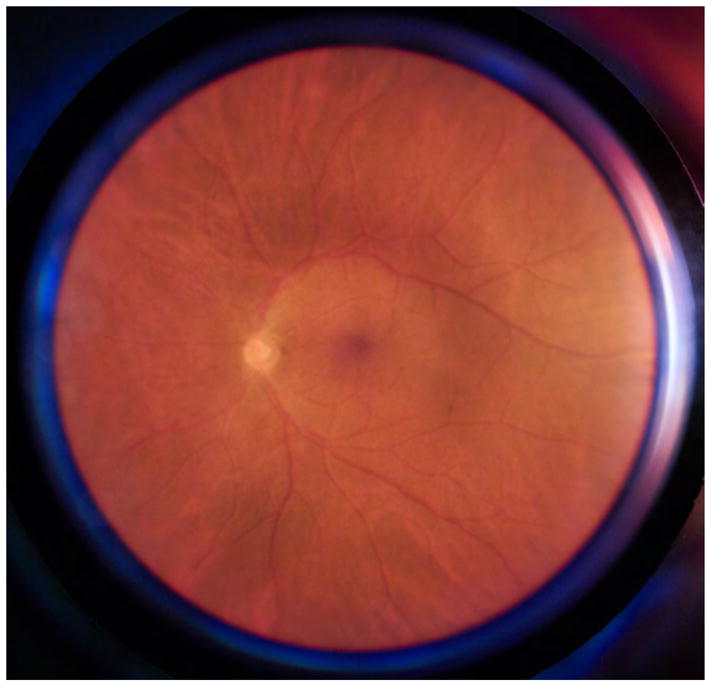
Fundus image captured from a subject who had no ocular pathology
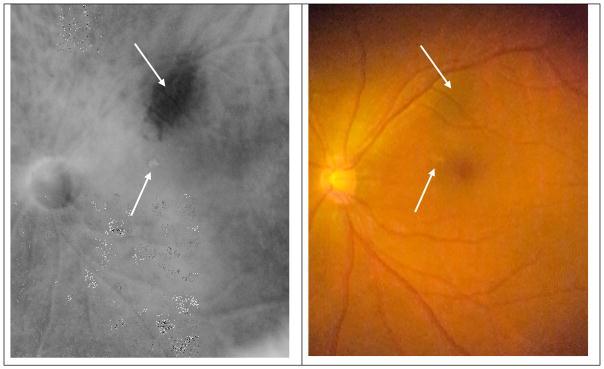
Figure 4a is a near infrared fundus image captured from a subject who had a choroidal nevus with drusen. Figure 4b is the color fundus image of the same patient captured by our imaging system with the transpalpebral illumination method.
Figure 4.
Near infrared (a) and color (b) fundus images captured from a subject who had a choroidal nevus with drusen.
The field of view based on the external angle was equal to 103°. However, current wide-field fundus cameras, such as a Retcam and Optos, typically use a spherical center (i.e., interior angle) to specify the view angle. For the 103° external angle, the corresponding interior angle was estimated at 0.74 × 2 × θ external [13]; i.e., 152°.
The radiant power at the fiber endpoint; i.e., the contact point with the eyelid was 70 mW/cm2, was ten times below the threshold of 700 mW/cm2 that was allowed for continuous illumination without thermal hazard concern. The light delivered by the illuminator was 1.5 lm luminous flux, which was lower than that of a xenon illumination system for vitreoretinal surgery [14]. The estimated irradiance at the retina was calculated to be 0.49 mW/cm2, which enabled 5.7 hours of continuous safe observing time according to the ISO 15004-2: 2007 standard [15]. Therefore, the trans-palpebral illumination is a safe and feasible method to pursue wide-angle fundus imaging.
4. DISCUSSION
The relatively avascular and thin structure of the pars plana allows a unique opportunity to transmit light to the inside of the eye. The anterior adjacent tissue pars plicata is a thick and vascularized structure that does not permit enough light to enter the eye. Outside of the pars plana, the choroid tissue becomes thicker sharply. The choroid is comprised of blood vessels, melanocytes, and other structures. Melanosomes and the high vascularization of the choroid results in blocking the light transmission into the inside of the eye [16].
Here we report a new approach for wide-angle fundus photography by illuminating the retina through the eyelid. Without pupil dilation, we were able to achieve a 152° view in a single-shot image, exceeding the 130° [8] maximum in a single-shot fundus image captured by the RetCam 3 (Clarity Medical Systems). Wide-angle fundus cameras, such as Retcam and Optos, are only available at limited clinical centers of urban hospitals because of their high cost due to expensive requirements for the sophisticated illuminating and imaging systems. The transpalpebral illumination method might help to provide a low-cost alternative to achieve wide angle fundus photography.
Acknowledgments
THIS RESEARCH WAS SUPPORTED IN PART BY NIH GRANTS R01 EY023522, R01 EY024628, P30 EY001792; BY NSF GRANT CBET-1055889; by Richard and Loan Hill endowment.
References
- 1.Pugh JA, Jacobson JM, Van Heuven WA, Watters JA, Tuley MR, Lairson DR, Lorimor RJ, Kapadia AS, Velez R. Screening for diabetic retinopathy. The wide-angle retinal camera. Diabetes care. 1993;16(6):889–95. doi: 10.2337/diacare.16.6.889. [DOI] [PubMed] [Google Scholar]
- 2.Wang SK, Callaway NF, Wallenstein MB, Henderson MT, Leng T, Moshfeghi DM. SUNDROP: six years of screening for retinopathy of prematurity with telemedicine. Canadian Journal of Ophthalmology / Journal Canadien d’Ophtalmologie. 2015;50(2):101–106. doi: 10.1016/j.jcjo.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 3.Shields CL, Materin M, Shields JA. Panoramic Imaging of the Ocular Fundus. Archives of Ophthalmology. 2003;121(11):1603. doi: 10.1001/archopht.121.11.1603. [DOI] [PubMed] [Google Scholar]
- 4.Schalenbourg A, Zografos L. Pitfalls in colour photography of choroidal tumours. Eye (London, England) 2013;27(2):224–9. doi: 10.1038/eye.2012.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yuan A, Kaines A, Jain A, Reddy S, Schwartz SD, Sarraf D. Ultra-wide-field and autofluorescence imaging of choroidal dystrophies. Ophthalmic surgery, lasers & imaging : the official journal of the International Society for Imaging in the Eye. 2010:e1–5. doi: 10.3928/15428877-20101025-10. 41 Online. [DOI] [PubMed] [Google Scholar]
- 6.Pomerantzeff O, Webb RH, Delori FC. Image formation in fundus cameras. Investigative ophthalmology & visual science. 1979;18(6):630–7. [PubMed] [Google Scholar]
- 7.DeHoog E, Schwiegerling J. Optimal parameters for retinal illumination and imaging in fundus cameras. Applied optics. 2008;47(36):6769–77. doi: 10.1364/ao.47.006769. [DOI] [PubMed] [Google Scholar]
- 8.Witmer MT, Kiss S. Wide-field imaging of the retina. Survey of ophthalmology. 2013;58(2):143–54. doi: 10.1016/j.survophthal.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 9.Riordan-Eva P, Cunningham E. Vaughan & Asbury’s General Ophthalmology. McGraw Hill Professional; London: 2011. pp. 10–14. [Google Scholar]
- 10.Pomerantzeff O. Equator-plus camera. Investigative ophthalmology. 1975;14(5):401–6. [PubMed] [Google Scholar]
- 11.Toslak D, Thapa D, Chen Y, Erol MK, Paul Chan RV, Yao X. Trans-palpebral illumination: an approach for wide-angle fundus photography without the need for pupil dilation. Optics letters. 2016;41(12):2688–91. doi: 10.1364/OL.41.002688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ophthalmic instruments-Fundus cameras-International standard (ISO 10940: 2009).
- 13.Atkinson A, Mazo C. [3 Jan 2017];Imaged Area of the Retina. https://www.optos.com/globalassets/documents/casestudies_imagedareaoftheretina.pdf.
- 14.Dithmar S, Hoeh AE, Amberger R, Ruppenstein M, Ach T. Light-emitting diode technology in vitreoretinal surgery. Retina (Philadelphia, Pa) 2011;31(5):924–7. doi: 10.1097/IAE.0b013e3181f44269. [DOI] [PubMed] [Google Scholar]
- 15.Ophthalmic instruments-Fundamental requirements and test methods-Part 2: Light hazard protection (ISO 15004-2: 2007).
- 16.Remington LA. Clinical anatomy and physiology of the visual system. Elsevier Health Sciences; St.Louis: 2012. pp. 48–49. [Google Scholar]