Abstract
Background
To explore the effectiveness of transcutaneous electrical acupoint stimulation (TEAS) approach on cancer-related fatigue (CRF) in non-small cell lung cancer (NSCLC) chemotherapy patients.
Methods
A total of 162 participants who treated with gemcitabine combined with platinum-based drugs (GP chemotherapy) were randomly assigned to three groups: Control (Group A, n=56), Sham TEAS (Group B, n=49), and TEAS (Group C, n=57). The following acupoints were used in this study: Qihai (CV6), Keshu (UB17), and Zusanli (ST36). The Revised Piper Fatigue Scale (RPFS) were used to measure CRF on the day before chemotherapy (P1), days 8 (P2) and 28 (P3) separately. The Differences among three groups were analyzed.
Results
At the 28th day, the outcomes of the fatigue scores for Group C, Group B and Group A were 2.06±0.90, 2.80±1.34, 3.00±1.29 respectively. There were significantly different among three groups (F=9.784, P<0.01). At the 28th day, the outcomes of the affective fatigue (F=8.161, P<0.01), sensory fatigue (F=3.06, P=0.05) and cognitive fatigue (F=8.06, P<0.01) for Group C, Group B and Group A were significantly different among three groups.
Conclusions
Chemotherapy may increase the fatigue from P1 to P2 and P3 in NSCLC patients. And TEAS could help to relived CRF, especially at P3.
Keywords: Cancer-related fatigue (CRF), transcutaneous electrical acupoint stimulation (TEAS), lung cancer
Introduction
Lung cancer is the leading cause of cancer related mortality worldwide, which accounts for about 19.4% of all cancer-related deaths (1). In 2010 to 2012, the incidence of lung cancer was approximately 30 people per 10 million in Global (2). 80% to 85% of all lung cancer patients’ diagnosis as non-small cell lung cancer (NSCLC).
Chemotherapy remains the primary treatment method for NSCLC patients, and gemcitabine combined with platinum-based drugs (GP regimen) is common used (3,4). Although GP regimen reduces the mortality of NSCLC patients significantly, majority patients could not endure the adverse reactions of chemotherapy. The fatigue is recognized as one of the most prevalent negative effects of the GP regimen (5,6). Up to 40% of cancer patients report fatigue at the time of diagnosis, and 80% of patients report fatigue at some point during chemotherapy (7). In 2014, National Comprehensive Cancer Network (NCCN) defined Cancer-related fatigue (CRF) as a distressing persistent tiredness with physical, emotional, and cognitive effects caused by cancer or chemotherapy (8). Fatigue is not only a prevalent adverse reaction, but a long-term problem. In the National Comprehensive Cancer Network (NCCN) guideline for Cancer-Ralted Fatigue (9), approximately one third of cancer patients who have completed their primary treatment for more than 6 years, still have certain levels of fatigue. As health professionals, however, the current fatigue after chemotherapy did not cause enough attention. It is hard to reduce the fatigue of cancer patients due to no standard guideline of fatigue intervention (10). Mitchell et al. (5) have suggested that exercise is an effective method to relieve cancerous fatigue, and scientific care interventions could improve the quality of life and treatment compliance of cancer patients with fatigue. However, Phillips et al. (6) demonstrated exercise is not associated with improved cancerous fatigue. Aerobic exercise caused by the cardiovascular system and skeletal muscle system adaptation is not permanent. After stop training for some time, the cardiovascular system function and skeletal muscle metabolism will gradually decline (11).
Currently, Traditional Chinese Medicine (TCM) has been the focus of increasing research activity. In a phase II trial, after acupuncture Zusanli (ST36), Qihai (CV6), Guanyuan (CV4) twice a week, 31.1% patient undergoing chemotherapy improve fatigue level (12). Guo CH showed that stimulating CV4, CV6, ST36, Shenque (CV8), Keshu (UB17) with moxibustion is another TCM method to ameliorate fatigue in esophagus cancer patients (13). However, the interventions are still limited, and acupuncture is an invasive method. Patients experience pain. In additional, moxibustion is not adapted to lung cancer patients caused by producing smoking.
The aim of this research was to explore the effects of TEAS on CRF in NSCLC chemotherapy patients. TEAS is a therapeutic approach based on transcutaneous electrical nerve stimulation (TENS) (14). TEAS incorporates the use of an electrode into traditional Chinese acupuncture therapy to stimulate specific acupuncture points in order to relieve symptoms and rehabilitate (14). According to TCM channel and collateral theory, TEAS would be introduced to relieve fatigue at ST36, CV6, UB17. Combined effects of the three acupoints have not been studied yet, even the literature indicates no incompatibility between it.
Methods
Study design
This study was conducted with a prospective experimental design from July, 2014 to July, 2015.This research was a single-center, randomized trial last for 28 days. A research assistant collected the outcome surveys at baseline before the chemotherapy (P1), at day 8 (P2), and at day 28 of the program (P3). To recruit suitable patients, the investigators explained the purpose of the research and provided a confidentiality agreement to each participant. The research protocol for the retrospective analysis was approved by the ethics committee of the Shanghai Pulmonary Hospital, China (No. K14-170). The Clinical Trial Number of this research is NCT02663492.
Setting and subjects
All participants were recruited from the oncology ward of a specialist pulmonary hospital in Shanghai. Those patients were selected for inclusion in the study who (I) had been diagnosed with NSCLC; (II) were aged between 20 and 80 years; (III) were in the first cycle of-GP chemotherapy after diagnosis; (IV) had been prescribed the doses of GP regimen are Gemcitabine 1,000 mg/m2 combine with Cisplatin 75 mg/m2 or carboplatin AUC 5–7; (V) had no surgery within 3 months; (VI) were expected to survive more than 3 months based on a score ≥60 points on the Karnofsky Performance Status (KPS); and (VII) were able to understand and speak Mandarin. Patients who were pregnant, mentally ill, or unable to communicate were excluded.
According to the results of the pre-experiment, the calculated sample size formula was used to obtain at least 47 samples (including 20% of the sample wastage rate). The formula is . The power was 90% and α was 5%. To minimize the infection between the TEAS group, the sham TEAS group and the control group, the subjects were physically isolated from the wards until the longitudinal study was carried out.
The patients who met all the selection criteria were randomized to the study groups as follows: Control group (Group A), Sham TEAS group (intervention group, Group B), and TEAS group (Group C). To assign the patients to the study groups, the letters “A”, “B”, and “C” were each written on 3 pieces of paper for each ward in the hospital. Then, all of the papers were placed in a container, and the participants were instructed to choose one piece of paper randomly from the container before the study began, then replace the paper in the container. The participants were not told which treatment the letters corresponded to, and the nurses who assisted the participants were not involved in the investigation.
Intervention
All the participants received routine cancer care at the time of hospitalization in terms of disease observation, dietary care, and psychological care.
For the control group, participants received routine nursing care, in terms of strict observation of the changes in condition, dietary care, vein embolic protection, routine use of antiemetic and gastroprotective agents.
In the TEAS group, patients received TEAS. After training the intensity, frequency of TEAS program by a Traditional Chinese Medicine clinical experts. TEAS was applied to three acupoints: bilateral Zusanli (ST36), bilateral Keshu (UB17), and unilateral Qihai (CV6). These acupoints were located based on Chinese anatomical locations (Table 1). In this research, TEAS was applied on the 1st, 2nd, 3rd, 5th, 8th, 11th, 14th, and 28th days. TEAS was used the G6805-II (Shanghai Medical Equipment Technology Co. Ltd., Shanghai, China) with a dense-disperse frequency of 30/100 Hz and an intensity of 6–15 V. Each session performed 30 minutes. The optimal intensity was adjusted to remain a slight twitching of the regional muscle according to individual maximum tolerance. Participants should record each acupoint stimulation session, involving date of session, frequency, intensity. If there are complications, inform the doctors timely. After each session, participants made appointment for the next session. A total 57 patients of the TEAS group had no adverse reactions.
Table 1. Location of acupuncture sites for the TEAS program.
| Acupoints | Location |
|---|---|
| Qihai (CV6) | Lower abdomen, located at the anterior median line, 1.5 inches below the navel |
| Keshu (UB17) | Located at the thoracic vertebra spinous process of the back, 1.5 inches away from the midline |
| Zusanli (ST36) | Located on the lateral side of each lower leg, 3 inches under Dubi (S 35), in the line of Dubi and Jiexi (ST 41) |
For the sham TEAS group, the procedure and duration of TEAS were same as those in the TEAS group, but the treatment was applied at nearby non-acupoint sites. The five sham points, located on each side of the belly button, the shin bone, and the scapula of the back, were selected. Those five sham points were either in similar dermatome regions as the five selected acupoints, or they were unknown with regard to their effects on fatigue (15). The sham TEAS group was used to explore whether TEAS influenced the psychological status of the participants.
Measures and instruments
The instruments included the demographic status and the Revised Piper Fatigue Scale (RPFS).
The demographic status was assessed based on the participants’ age, gender, financial status, family history, body mass index (BMI), body temperature, heart rate, respiratory rate, systolic pressure, diastolic pressure, cancer type, cancer staging and KPS.
The RPFS is a 22-item multidimensional self-report scale that assesses patient’s overall fatigue status based on four dimensions, including behavioral fatigue, sensory fatigue, affective fatigue, and cognitive fatigue (16). Scores on the RPFS range from 0 to 10 for each item, and a higher score is associated with worse fatigue (17). The RPFS is classified into four categories as follows: a score of 0 represents no fatigue; a score of 1–3 indicates mild fatigue; a score of 4–6 represents moderate fatigue; and a score of 7–10 indicates severe fatigue (16). The total score on the RPFS is given as the mean score of all items, and the score for each dimension is also calculated. The RPFS has documented validity and reliability in many countries (18), and it has been translated into Chinese and applied to measure the fatigue status of cancer patients in various studies (17). The inter-rater reliability and consistency were shown to be 0.97 (19).
Data analysis
SPSS, version 19.0 (SPSS Inc., Chicago, IL, USA) was used to analyze the data in this study. Descriptive statistics were used, including the means, standard deviations, and percentages. Analysis of variance (ANOVA) and a t-test were applied to analyze the effectiveness of TEAS. Chi-squared test was used to evaluate the differences in the outcomes and the demographic data among the three groups in the case of categorical variables. Additionally, the ANOVA was performed to compare the differences in continuous variables. A P value less than 0.05 was considered statistically significant.
Results
Patients’ demographic characteristics
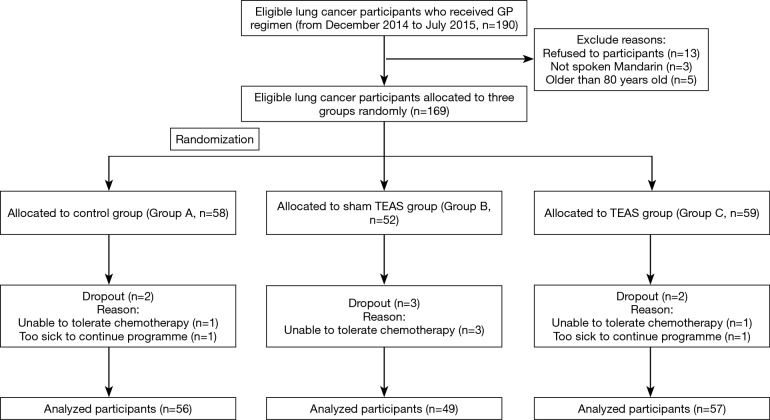
Initially, 169 participants from Shanghai pulmonary hospital in China were randomized into three groups: Group A (n=58) was a control group, Group B (n=52) received sham TEAS, and Group C (n=59) received TEAS. During the study, 7 participants dropped out because they were too sick to continue the program or they could not tolerate chemotherapy. Finally, 162 participants completed the study (Figure 1).
Figure 1.
Flow chart of allocation and dropouts of participants.
The baseline characteristics of the participants are presented in Tables 2 and 3. There was no significant difference among three groups (P>0.05). The KPS did not differ significantly between the three groups (P=0.089), and all participants were expected to live more than six months (20). There was no significant difference in the baseline characteristics between the dropouts and those who completed the study (P>0.05).
Table 2. Demographic values for categorical variables by group.
| Categorical variables | Group A (n=56), n (%) | Group B (n=49), n (%) | Group C (n=57), n (%) | Chi-squared test | P |
|---|---|---|---|---|---|
| Gender | 2.54 | 0.97 | |||
| Male | 46 (82.1) | 34.(69.4) | 42 (73.7) | ||
| Female | 10 (17.9) | 15 (30.6) | 15 (26.3) | ||
| Financial status | 0.46 | 0.53 | |||
| Pension | 32 (57.1) | 26 (53.1) | 29 (50.9) | ||
| Non-pension | 24 (42.9) | 23 (46.9) | 28 (49.1) | ||
| Family history | 0.40 | 0.98 | |||
| Yes | 1 (1.8) | 1 (2.0) | 2 (3.5) | ||
| No | 55 (98.2) | 48 (98.0) | 55 (96.55) | ||
| Cancer type | 0.70 | 0.91 | |||
| Adenocarcinoma | 30 (53.6) | 24 (49.0) | 29 (50.9) | ||
| Squamous carcinoma | 18 (32.1) | 15 (30.6) | 18 (31.6) | ||
| Others | 8 (14.3) | 10 (20.4) | 10 (17.5) | ||
| Cancer staging | 0.28 | 0.83 | |||
| I–III | 52 (92.9) | 46 (93.9) | 52 (91.2) | ||
| IV | 4 (7.1) | 3 (6.1) | 5 (8.8) |
Table 3. Baseline values for continuous variables by group.
| Continuous variables | Group A (n=56), mean ± SD | Group B (n=49), mean ± SD | Group C (n=57), mean ± SD | F-test | P |
|---|---|---|---|---|---|
| Age | 58.27±10.57 | 54.44±10.48 | 58.06±8.42 | 2.660 | 0.062 |
| BMI | 22.97±2.55 | 22.18±3.43 | 23.23±2.56 | 2.638 | 0.071 |
| Body temperature | 36.06±0.30 | 36.77±0.22 | 36.57±0.29 | 0.198 | 0.922 |
| Heart rate | 81.77±5.35 | 82.45±2.66 | 82.58±7.17 | 0.324 | 0.727 |
| Respiratory rate | 21.00±11.90 | 19.27±0.81 | 20.96±6.55 | 0.613 | 0.572 |
| Systolic pressure | 125.46±15.42 | 119.75±14.00 | 121.62±14.83 | 2.006 | 0.205 |
| Diastolic pressure | 78.83±6.38 | 75.69±9.04 | 75.83±9.73 | 2.312 | 0.098 |
| KPS | 85.02±4.98 | 83.31±4.77 | 83.31±4.77 | 2.328 | 0.103 |
Effects of TEAS on CRF
Table 4 summarizes the results of the RPFS. At P1 and P2, there was no statistically significant difference between the three groups (P>0.05, Table 4). However, the outcomes showed statistically significant differences among the three groups at P3 (P<0.01, Table 4).
Table 4. Results of RPFS among the groups at P1, P2 and P3.
| Groups | P1, mean ± SD | P2, mean ± SD | P3, mean ± SD |
|---|---|---|---|
| Group A, n=56 | 1.49±1.58 | 2.68±1.36 | 3.00±1.29 |
| Group B, n=49 | 1.91±1.37 | 2.59±1.18 | 2.80±1.34 |
| Group C, n=57 | 1.68±1.57 | 2.85±1.62 | 2.06±0.90 |
| Total, n=162 | 1.69±1.52 | 1.69±1.52 | 2.61±1.25 |
| F-test | 1.091 | 0.488 | 9.784 |
| P | 0.338 | 0.615 | <0.01 |
| Multiple comparison: P | |||
| Group A vs. Group B | 0.142* | 0.724* | 0.821** |
| Group A vs. Group C | 0.490* | 0.526* | <0.01** |
| Group B vs. Group C | 0.419* | 0.334* | 0.005** |
*, refers to LSD-test; **, refers to Tamhane-test. P1, before chemotherapy; P2, day 8 after chemotherapy; P3, day 28 after chemotherapy.
Effects of TEAS on the dimensions of the RPFS at P3
The outcome measures of the four dimensions of the RPFS at P3 are summarized in Table 5. Based on the results, all he dimension indicated statistically significant differences, with the exception of sensory fatigue (P=0.50). However, Group C (Mean =2.48) had a lower sensory fatigue score than Group A or Group B (Mean =3.20 and Mean =2.72, respectively, Table 5).
Table 5. Results for the four dimensions of the RPFS among the groups at P3.
| Outcome measures (P3) | Behavioral fatigue, mean ± SD | Affective fatigue**, mean ± SD | Sensory fatigue, mean ± SD | Cognitive fatigue, mean ± SD |
|---|---|---|---|---|
| Group A, n=56 | 2.497±1.105 | 3.039±1.524 | 3.20±1.79 | 3.31±2.12 |
| Group B, n=49 | 2.36±1.25 | 3.216±1.731 | 2.72±1.63 | 2.96±2.24 |
| Group C, n=57 | 1.80±0.89 | 2.143±1.198 | 2.48±1.30 | 1.91±1.37 |
| F-test | 6.471 | 8.161 | 3.060 | 8.060 |
| P | 0.002 | <0.01 | 0.050 | <0.01 |
| Multiple comparison: P | ||||
| Group A vs. Group B | 0.919** | 0.927** | 0.122* | 0.795** |
| Group A vs. Group C | 0.001** | 0.002** | 0.016* | <0.01** |
| Group B vs. Group C | 0.031** | 0.001** | 0.428* | 0.016** |
*, refers to LSD-test; **, refers to Tamhane-test. RPFS, Revised Piper Fatigue Scale; P3, day 28 after chemotherapy.
Discussion
According to the results, this study of the implementation of TEAS intervention to verify long-term use can relieve lung cancer chemotherapy in patients with CRF. This is associated with some previous literature. Studies have shown that percutaneous electrical stimulation of cancer patients with CRF has a certain mitigation effect (18). Another study in the UK concluded that 36% of patients were significantly improved fatigue after 14 days of acupuncture (21).
Based on the findings, the fatigue level of most lung cancer patients increased slightly during chemotherapy. Lung cancer patients undergoing chemotherapy experience physical and psychological stress for a long period of time (22). During process of treatments, the accumulation of chemotherapeutic drugs and products of cellular causes impairment to the body and brain cells, thereby affecting the patients’ fatigue level through both physical and psychological mechanisms (23). Jones et al. (24) discovered the longer the patient’s chemotherapy, the heavier the level of fatigue.
This study demonstrates that the three major acupoints (ST36, CV6, UB17) used in this research positively influence fatigue level. In Chinese medicine, fatigue is considered to represent a series of physiological dysfunctions caused by spleen deficiency (25). And ST 36 in the stomach meridian is commonly used to improve spleen-deficiency syndrome (26). CV 6 adjusts the viscera Chi of the body to enhance the flow of Chi and soothe the organs so that body can rest (15,27). UB 17 is usually targeted to relieve vomiting, hiccups, and backaches. Symptom control is an important strategy to alleviate patients’ physical fatigue (28). Meanwhile, the fatigue score of the sham TEAS group (Group B) is higher than the TEAS group (Group C) at day 28, which means participants experienced an improvement in their fatigue level through electrical stimulation of the three acupoints rather than psychological factors.
Based on the results in this research, the majority of the patients had a moderate fatigue status for sensory fatigue, affective fatigue and cognitive fatigue, but there was variability in the scores for the behavioral dimension. In other words, fatigue causes a varying degree of damage in lung cancer patients, in terms of daily activities, physical health, emotional status, and cognitive function. The sensory dimension showed less improvement than the other dimensions. Sun believed that the insufficient high-energy foods, such as protein, fat, and sugar, give rise to fatigue (29). In addition, accumulation of chemotherapy metabolites in the body could increase the level of sensory fatigue. Finally, most lung cancer patients are at old age with the onset of disease at mean age of 76.9 years old. With aging, decreased physical function leads to intensification of the experience of fatigue (26).
This research has a few limitations. First, all the patients were in the first cycle of GP chemotherapy treatment after diagnosis. However, CRF might be increased during later cycles of chemotherapy (7). Thus, subsequent studies should recruit participants in other lines of chemotherapy to explore the effects of TEAS on CRF. Secondly, the daily activities of the participants may have affected their fatigue level (30). In this research, the level of physical activity of the participants was variable and might have influenced the results. Further studies are needed to address the effects of exercise on the effectiveness of TEAS. Third, only three times data collection during 28 days might increase memorizing bias, which could affect the results. For the further research, data collection would be more frequently in order to avoid memorizing bias, Additionally, this study only included lung cancer patients undergoing chemotherapy, and the findings cannot be generalized to cancer patients who receive other forms of treatment, such as radiotherapy, surgery, or targeted therapy. Future studies should consider different cancer diagnoses and treatments to increase generalizability. Finally, appropriate frequency and duration of TEAS for each participant could be analyzed more precisely in future studies.
Conclusions
In conclusion, the results of this research support the hypothesis that CRF in patients with lung cancer undergoing GP chemotherapy could be relieved by TEAS. It is feasible to provide TEAS and to implement the program in chemotherapy patients. This study demonstrates the effectiveness of the TEAS, although additional studies are needed to determine the appliance of the TEAS in other chemotherapy regimens and other lines of chemotherapy to alleviate CRF in Chinese patients. Future studies should aim to improve the generalizability of the sample, develop an intervention that is easier to implement, and utilize stronger study designs.
Acknowledgements
We acknowledge the efforts of the staff of Medical Record Room in the record retrieval.
Funding: The study was supported by a grant from the National Nature and Science Foundation of China (Grant No. Nur81202750). The funding agency has no involvement with the design of the study and collection, analysis, interpretation of data and writing the manuscript.
Ethical Statement: Ethical approval was given by the ethics committee of the Shanghai Pulmonary Hospital, China (No. K14-170). Individual consent was not required as this was a secondary data study using a pseudo-anonymised database extract.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.WHO. World Cancer Report 2014. (2014-02-03) [2017-05-9]. Available online: http://www.iarc.fr/en/media-centre/pr/2014/pdfs/pr224_E.pdf
- 2.Jemal A, Bray F, Center M, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69-90. 10.3322/caac.20107 [DOI] [PubMed] [Google Scholar]
- 3.Curt G, Johnston G. Cancer fatigue: the way forward. Oncologist 2003;8:27-30. 10.1634/theoncologist.8-suppl_1-27 [DOI] [PubMed] [Google Scholar]
- 4.Wang S, Peng L, Li J, et al. A Trial-Based Cost-Effectiveness Analysis of Erlotinib Alone versus Platinum-Based Doublet Chemotherapy as First-Line Therapy for Eastern Asian Non squamous Non–Small-Cell Lung Cancer. Plos One 2013;8:e55917. 10.1371/journal.pone.0055917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mitchell SA, Beck SL, Hood LE, et al. Putting evidence into practice: evidence-based interventions for fatigue during and following cancer and its treatment. Clin J Oncol Nurs 2007;11:99-113. 10.1188/07.CJON.99-113 [DOI] [PubMed] [Google Scholar]
- 6.Phillips SM, McAuley E. Physical activity and fatigue in breast cancer survivors: a panel model examining the role of self-efficacy and depression. Cancer Epidemiol Biomarkers Prev 2013;22:773-81. 10.1158/1055-9965.EPI-12-0983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang XS, Woodruff JF. Cancer-related and treatment-related fatigue. Gynecol Oncol 2015;136:446-52. 10.1016/j.ygyno.2014.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hotta K, Matsuo K, Ueoka H, et al. Addition of platinum compounds to a new agent in patients with advanced non-small-cell lung cancer: a literature based meta-analysis of randomized trials. Ann Oncol 2004;15:1782-9. 10.1093/annonc/mdh476 [DOI] [PubMed] [Google Scholar]
- 9.Notional Comprehensive Cancer Network. Cancer-Related Fatigue, 2014, version 1. (2014-02-03)[2017-05-9] Available online: https://www.nccn.org/professionals/physician_gls/pdf/fatigue.pdf
- 10.Koornstra RH, Peters M, Donofrio S, et al. Management of fatigue in patients with cancer -- a practical overview. Cancer Treat Rev 2014;40:791-9. 10.1016/j.ctrv.2014.01.004 [DOI] [PubMed] [Google Scholar]
- 11.Stone PC, Minton O. Cancer-related fatigue. Eur J Cancer 2008;44:1097-104. 10.1016/j.ejca.2008.02.037 [DOI] [PubMed] [Google Scholar]
- 12.Yang J, Ding M. Research of intervention on patients with cancer related fatigue (Chinese). Chinese General Practice 2012;15:593-5. [Google Scholar]
- 13.Vickers AJ, Straus DJ, Fearon B, et al. Acupuncture for postchemotherapy fatigue: a phase II study. J Clin Oncol 2004;22:1731-5. 10.1200/JCO.2004.04.102 [DOI] [PubMed] [Google Scholar]
- 14.Guo C. Treatment of 39 Cases of Esophageal Carcinogenesis with Moxibustion Combined with Acupoint (Chinese). Chinese Health Care Nutrition 2016;26:33. [Google Scholar]
- 15.Wang B, Ye X. The origin of ‘Qi’ in Traditional Chinese Medicine classics and translation analysis (Chinese). Chinese Translators Journal 2014;2:107-10. [Google Scholar]
- 16.Zhao J, Li S, Rong P, et al. Investigation on effects and mechanism of acupoints (Chinese). Modernization of Traditional Chinese Medicine and Materia Medica 2014;16:2076-82. [Google Scholar]
- 17.Zhang F, Ding Y, Han L. Reliability and validity of the Chinese version of Cancer Fatigue Scale (Chinese). Chinese Mental Health Journal 2011;25:810-3. [Google Scholar]
- 18.Dagnelie PC, Pijls-Johannesma MC, Pijpe A, et al. Psychometric properties of the revised Piper Fatigue Scale in Dutch cancer patients were satisfactory. J Clin Epidemiol 2006;59:642-9. 10.1016/j.jclinepi.2005.09.015 [DOI] [PubMed] [Google Scholar]
- 19.Xue X. Cancer-related fatigue assessment tools and the research progress of evaluation index (Chinese). Chinese Journal Nursing 2012;47:859-61. [Google Scholar]
- 20.Soo I, Gramlich L. Use of parenteral nutrition in patients with advanced cancer. Appl Physiol Nutr Metab 2008;33:102-6. 10.1139/H07-152 [DOI] [PubMed] [Google Scholar]
- 21.Dimeo FC, Stieglitz RD, Novelli-Fischer U, et al. Effects of physical activity on the fatigue and psychologic status of cancer patients during chemotherapy. Cancer 1999;85:2273-7. [DOI] [PubMed] [Google Scholar]
- 22.Molassiotis A, Sylt P, Diggins H. The management of cancer-related fatigue after chemotherapy with acupuncture and acupressure: a randomised controlled trial. Complement Ther Med 2007;15:228-37. 10.1016/j.ctim.2006.09.009 [DOI] [PubMed] [Google Scholar]
- 23.Bol Y, Duits A, Hupperts M, et al. The psychology of fatigue in patients with multiple sclerosis: a review. J Psychosom Res 2009;66:3-11. 10.1016/j.jpsychores.2008.05.003 [DOI] [PubMed] [Google Scholar]
- 24.Chou PB, Morse CA. Understanding premenstrual syndrome from a Chinese medicine perspective. J Altern Complement Med 2005;11:355-61. 10.1089/acm.2005.11.355 [DOI] [PubMed] [Google Scholar]
- 25.Jones JM, Olson K, Catton P, et al. Cancer-related fatigue and associated disability in post-treatment cancer survivors. J Cancer Surviv 2016;10:51-61. 10.1007/s11764-015-0450-2 [DOI] [PubMed] [Google Scholar]
- 26.Huang W, Kutner N, Bliwise L. A systematic review of the effects of acupuncture in treating insomnia. Sleep Med Rev 2009;13:73-104. 10.1016/j.smrv.2008.04.002 [DOI] [PubMed] [Google Scholar]
- 27.Liu L, Mills J, Rissling M, et al. Fatigue and sleep quality are associated with changes in inflammatory markers in breast cancer patients undergoing chemotherapy. Brain Behav Immun 2012;26:706-13. 10.1016/j.bbi.2012.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Giacalone A, Polesel J, De Paoli A, et al. Assessing cancer-related fatigue: the psychometric properties of the Revised Piper Fatigue Scale in Italian cancer in patients. Support Care Cancer 2010;18:1191-7. 10.1007/s00520-009-0741-0 [DOI] [PubMed] [Google Scholar]
- 29.Sun Q. Effect of transcutanclus electrical acupoint stimulation used to alleviate cancer related fatigue in cancer chemotherapy patients (Chinese). Chinese Journal of Modern Nursing 2011;7:3486-8. [Google Scholar]
- 30.Schwartz AL, Mori M, Gao R, et al. Exercise reduces daily fatigue in women with breast cancer receiving chemotherapy. Med Sci Sports Exerc 2001;33:718-23. 10.1097/00005768-200105000-00006 [DOI] [PubMed] [Google Scholar]