Abstract
Background
More than one-third of lung cancer worldwide occurring in China. However, the clinical profiles of lung cancer patients in the mainland of China are rarely reported and largely unknown. The objective of this study is to analyze the characteristics and time trends of newly diagnosed lung cancer cases during the past 5 years in East China.
Methods
The data came from an academic tertiary care hospital of East China. Patients who were newly diagnosed as lung cancer from 2011 to 2015 were enrolled. All new cases got pathological supports by lung biopsy or surgery. Tumor staging was performed according to the seventh edition of the tumor node metastasis (TNM) classification of malignant tumors. The patients’ disease information was collected from the database of the hospital information system (HIS).
Results
From 2011 to 2015, aggregately 5,779 patients, including 3,719 males and 2,060 females, were diagnosed as lung cancer. The major histologic subtypes of lung cancer were adenocarcinoma (ADC, 60.0%), squamous cell carcinoma (SCC, 25.6%), small cell lung cancer (SCLC, 8.5%), large cell carcinoma (0.6%), adenosquamous carcinoma (1%), other non-small cell carcinoma (1.6%) and unclassified or rare carcinoma (2.8%). ADC proportion of female was much higher than that of male. A higher proportion of advanced stage (stage IIIB, IV) of lung cancer existed in patients who were admitted to hospital due to respiratory or cancer related symptoms (RCRS) than those without RCRS. Smoking rate in male patients reached 80.2%, while it was only 2.7% in females. EGFR mutation existed in 66% of female and 37% of male patients with ADC.
Conclusions
This study demonstrates the clinicopathologic characteristics of lung cancer patients from East China, including histologic composition, staging proportion, smoking prevalence and gene mutation status. During the past 5 years, the proportion of ADC has increased gradually whereas SCC decreased.
Keywords: Lung cancer, China, profiles
Introduction
Lung cancer has become the most commonly diagnosed cancer and the leading cause of cancer death in China. There are an estimated 733,300 new cases and 610,200 deaths of lung cancer in China in 2015 (1). Regrettably, since the incomplete registration of case information, the clinical profiles of lung cancer patients in the mainland of China, such as histologic composition, staging proportion, smoking prevalence and gene mutation profiles, are rarely reported and largely unknown. On the other hand, in China, the estimated mortality of lung cancer is higher than the world average (2), which may be related to the neglect of early finding and diagnosis. It is reported that approximately two-thirds of patients are diagnosed at the advanced stage (3,4). During the past 5 years, a rising Chinese population, especially people in East China, is covered by medical insurance and routine physical examinations. Thus, more patients with early-stage lung cancer can be found. In this study, we analyzed the characteristics and variation trends of newly diagnosed lung cancer cases during the past 5 years in an academic tertiary care hospital of East China, and aimed to demonstrate some clinical profiles of Chinese lung cancer.
Methods
Study subjects
The cases of current study came from an academic tertiary care hospital of East China, the Second Affiliated Hospital of Zhejiang University (SAHZU). This is a general hospital with multiple departments including thoracic surgery, pulmonary medicine and oncology. From Jan 2011 to Dec 2015, there were 5,779 patients diagnosed as lung cancer in SAHZU. All patients were pathologically confirmed as lung cancer by bronchoscopy, thoracoscopy, needle biopsy, surgical resection or pleural effusion examination. Tumor staging was performed according to the seventh edition of the tumor node metastasis (TNM) classification of malignant tumors (5).
The retrospective study was approved by the Institutional ethics committee of SAHZU (2017-031).
Data collection
The patients’ demographic information and clinical characteristics, including gender, age at diagnosis, smoking history, symptoms, pathological results, imaging results, TNM staging, EGFR mutation, were collected from the database of the hospital information system (HIS). Tumor staging was confirmed by two researchers.
Statistical methods
Our data were analyzed by SPSS statistical software 20.0 (SPSS, Inc., an IBM Company, Chicago, IL, USA). Discrete variables were presented with absolute and relative frequencies. Continuous variables were presented as mean and standard deviation. Chi-square test was used for the comparison of proportions. Differences were considered significant when two-sided P values were less than 0.05.
Results
Histological composition and variation tendency of lung cancer in Chinese people
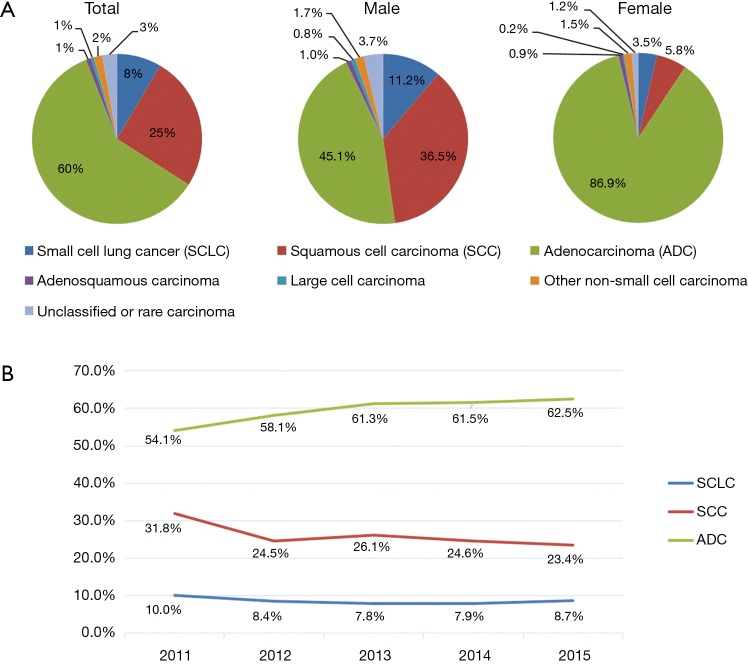
From 2011 to 2015, aggregately 5,779 patients, including 3,719 males and 2,060 females, were diagnosed as lung cancer. The most common histological subtype was adenocarcinoma (ADC, 60.0%), followed by squamous cell carcinoma (SCC, 25.6%), small cell lung cancer (SCLC, 8.5%), large cell carcinoma (LCC, 0.6%), adenosquamous carcinoma (1%), other non-small cell carcinoma (1.6%) and unclassified or rare carcinoma (2.8%). Of note, there was a significant difference of histological proportion between male and female. In male population, the percentage of ADC, SCC, and SCLC was 45.1%, 36.5% and 11.2% respectively. However, in female population, ADC accounted for 86.9% of the proportion to be the majority of histological subtype (Figure 1A). During the past 5 years, the proportion of ADC increased gradually from 54.1% to 62.5%, whereas SCC decreased from 31.8% to 23.4% (Figure 1B).
Figure 1.
Histological composition and variation tendency of lung cancer during 2011 to 2015.
Respiratory or cancer related symptoms (RCRS) of lung cancer patients
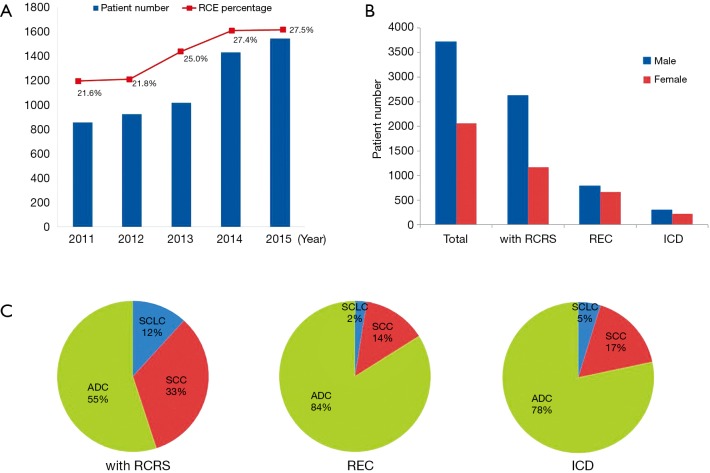
According to the reasons for admission, patients were divided into three types: admitted to hospital because of RCRS, diagnosed by routine chest examination (RCE) of asymptomatic lung cancers, or detected by incidental chest discovery (ICD) of asymptomatic lung cancers when imaging studies were performed for other reasons. Both RCE and ICD patients were considered without RCRS. Our study showed that the proportion of RCE group rose gradually from 21.6% to 27.5% during the past 5 years (Figure 2A). The number of male patients with RCRS was much more than that of female patients (2,623 vs. 1,168); however, the number in RCE and ICD groups was similar (Figure 2B). Further analysis showed that the proportions of three major subtypes of ADC, SCC, and SCLC were different between groups with or without RCRS. Almost 80% cases were ADC in the group without RCRS, whereas only 55% were in those with RCRS (Figure 2C).
Figure 2.
Respiratory or cancer related symptoms of lung cancer patients. (A) The proportion of RCE group rose gradually during past 5 years; (B) male patients with RCRS were much more than female patients; (C) ADC proportion was higher in patients without RCRS than that with RCRS. RCRS, Respiratory or cancer related symptoms.
Staging distribution of lung cancer with or without RCRS
Of 5,779 patients, ADC, SCC and SCLC accounted for 94%. Except for 172 cases that could not be staged because of uncompleted data, the rest 5,263 cases with definite staging were analyzed in this study. All the patients analyzed were divided into two groups on the basis of whether they were accompanied with RCRS at the time of diagnosis or not. The group without RCRS included RCE and ICD patients. Staging proportions were shown in Table 1. For non-small cell lung cancer (NSCLC), mainly including ADC and SCC, stage IIIB and IV were considered as advanced stage that could not be radically resected. In this study, we found patients with RCRS have a higher proportion of advanced stage than those without RCRS (SCC, 39.9% vs. 22.7%; ADC, 54.4% vs. 19.8%). Notably, for patients without RCRS, 57.5% of ADC patients were in stage I. For SCLC, stage I (T1-2aN0M0) can receive a radical operation; otherwise, chemotherapy and radiotherapy are major managements. This study showed that patients without RCRS accounted for 12.3% of the stage I SCLC, relevant to 4.3% in the group with RCRS.
Table 1. Staging proportion in different subtypes of lung cancer.
| Variable | RCRS | Number | Stage (%) | |||||
|---|---|---|---|---|---|---|---|---|
| 0 | I | II | IIIA | IIIB | IV | |||
| Total | Yes | 3,408 | 0.4 | 19.9 | 9.0 | 20.0 | 8.3 | 42.4 |
| No | 1,855 | 2.8 | 53.8 | 8.5 | 13.5 | 4.4 | 17.0 | |
| SCLC | Yes | 401 | 0.0 | 4.2 | 5.5 | 26.4 | 13.0 | 50.9 |
| No | 57 | 0.0 | 12.3 | 8.8 | 19.3 | 14.0 | 45.6 | |
| SCC | Yes | 1,132 | 0.1 | 15.9 | 13.7 | 30.4 | 11.5 | 28.4 |
| No | 268 | 0.0 | 41.4 | 14.6 | 21.3 | 6.3 | 16.4 | |
| ADC | Yes | 1,875 | 0.7 | 25.6 | 6.9 | 12.4 | 5.3 | 49.1 |
| No | 1,530 | 3.4 | 57.5 | 7.4 | 12.0 | 3.7 | 16.1 | |
RCRS, respiratory or cancer related symptoms; SCLC, small cell lung cancer; SCC, squamous cell carcinoma; ADC, adenocarcinoma.
Smoking prevalence in Chinese lung cancer patients
There were 5,702 patients, including 3,666 males and 2,036 females who provided smoking history. As shown in Table 2, smoking rate in male patients reached 80.2%, compared to 2.7% in females. Further analysis showed that, for male patients, the smoking rate in SCC and SCLC was much higher than that in ADC.
Table 2. Smoking prevalence in lung cancer patients.
| Variable | Smoke | Non-smoke | ||
|---|---|---|---|---|
| Case number (%) | Smoking history (pack-year) | Case number (%) | ||
| Male | 2,941 (80.2) | 725 (19.8) | ||
| SCLC | 363 (88.3) | 44.6±27.8# | 48 (11.7) | |
| SCC | 1,199 (89.5) | 48.1±27.9# | 140 (10.5) | |
| ADC | 1,167 (70.5) | 36.6±25.5 | 488 (29.5) | |
| Female | 54 (2.7) | 1,982 (97.3) | ||
| SCLC | 6 (8.2) | 22.2±18.2 | 67 (91.8) | |
| SCC | 16 (13.8) | 31.0±15.6 | 100 (86.2) | |
| ADC | 31 (1.8) | 23.3±28.3 | 1,739 (98.2) | |
#, P<0.05 compared to ADC group. SCLC, small cell lung cancer; SCC, squamous cell carcinoma; ADC, adenocarcinoma.
Age distribution in Chinese lung cancer patients
The average age of male patients in our study was 62.7 years, with female patients being 59.7 years. The U.S. Preventive Services Task Force (USPSTF) recommends annual screening for lung cancer with low-dose computed tomography in American adults aging from 55 to 80 years, who are current or ever smokers with a smoking history of 30 pack year and have only quit smoking within the past 15 years. In our study, among 1,459 RCE patients, only 22.5% meets this criterion.
EGFR mutation in Chinese lung cancer patients
In our study, we found that 501 patients, including 440 ADC (161 smokers and 279 non-smokers) and 61 SCC received EGFR mutation test. As shown in Table 3, EGFR mutation existed in 66% female and 37% male patients of ADC. A higher mutation rate was found in non-smokers (62%) than smokers (34%). Exon21 L858R and Exon19 DEL were the most common mutation types, which consisted of 91% in female and 88% in male among all mutation types. However, EGFR mutation was very rare in SCC patients. Of all the 61 SCC patients who took gene detection, only one case was proved positive for EGFR mutation.
Table 3. EGFR mutation in lung cancer patients.
| Variable | Female [%] | Male [%] |
|---|---|---|
| ADC (total cases) | 229 | 211 |
| Wild | 79 [34] | 133 [63] |
| 19 DEL | 57 [25] | 32 [15] |
| 21 L858R | 79 [34] | 37 [18] |
| 20 ins | 3 [1] | 3 [1] |
| 18 G719X | 4 [2] | 2 [1] |
| 21 L861Q | 5 [2] | 1 [0] |
| 20 S768I | 0 [0] | 1 [0] |
| Multi-mutation | 2 [1] | 2 [1] |
| SCC (total cases) | 5 | 56 |
| Wild | 5 [100] | 55 [98] |
| 20 S768I | 0 | 1 [2] |
ADC, adenocarcinoma; SCC, squamous cell carcinoma.
Discussion
China is a great nation with 1.37 billion people. Over one-third lung cancer worldwide occurs in China. Different from developed countries, the information record and statistics of lung cancer in China are incomplete, and the clinical profiles about Chinese lung cancer are rarely reported and largely unknown. There were only several reports from a Hong Kong hospital describing the clinical profiles of Chinese lung cancer decades ago (6-8). Another paper representing the histological characteristics of lung cancer of males was based on the data from a hospital in North China (9). So far, there are no definite statistics data about the proportion of lung cancer categories in Chinese people. According to the statistics from USA, the proportions of different categories of lung cancer are showed as follows: SCLC (13.6%) and NSCLC (85.3% of the total lung cancer cases). NSCLC are further classified as ADC (40.8% of the total lung cancer cases), SCC and transitional cell carcinoma (21.4%), LCC (2.6%), and other non–small cell carcinoma (20.4%) (10). Our data showed that there was a larger proportion of ADC patients in China (60%), especially in female patients (86.9%).
By analyzing the variation trends of histological composition during past 5 years, we found that the ADC proportion kept increasing but the SCC decreased which was consistent with several other reports (11-14). One major reason contributing to this variation is that a rising number of Chinese people nowadays receive the RCE of CT scan, by which more early-stage ADC was detected. Our study showed that from 2011 to 2015, the proportion of RCE group rose from 20.9% to 27.5%. For RCE patients, the ADC proportion reached 84%, which was much higher than that of patients with RCRS. This implies that more ADC patients were found in China due to the routine CT scan. In western countries, the cigarette control may also contribute to the ADC increase. However, in our study, we did not find any change trends of smoking rate in both male and female.
Smoking is a well-known risk factor of lung cancer. Globally, an estimated 15% of men and 53% of women with lung cancer are never-smokers (15). In our study, 80.2% of men with lung cancer are smokers, which is similar to the global average level. Especially for SCC and SCLC males, both smoking rate and smoking quantity (pack year) are more than those of ADC patients. This suggests that smoking habit is most likely related to SCC and SCLC incidence. Of note, the smoking rate of Chinese women is very low, with only 2.7% in lung cancer females. Our study showed that ADC proportion in female reached 86.9%, while SCC only counted 5.8%. We thought the pathological constitution was related to this very low smoking rate of Chinese women. Different from lung cancer patients in western countries, Chinese ADC patients have much higher EGFR mutation rate. Our study showed that EGFR mutation rate reached 66% in ADC females and 37% in ADC males. This data was similar with the results of other studies (16-18).
It is reported that a majority of lung cancers are diagnosed at an advanced stage. For these patients, few can survive beyond 1–2 years. Only a minority of patients with lung cancer are diagnosed with localized lesion. In the absence of screening, those diagnoses are mostly made because of incidental discovery of asymptomatic lung cancers when imaging examinations are performed for other reasons. Our study showed that 70.7% of lung cancer patients complaining of respiratory symptoms were diagnosed at an advanced stage (stage IIIB & IV). In contrast, screening can detect 65.1% of the early-staged patients. During the past 5 years, the proportion of local stage of lung cancer kept increasing due to the popularization of routine physical examinations.
Chest CT scan, especially low-dose CT (LDCT) screening is an effective method to detect early-stage lung cancers (19). However, considering the adverse effects of radiation exposure, screening is only recommended for those at high risks. In late 2013, the USPSTF provided its lung cancer screening recommendation as following: “The USPSTF recommends annual screening for lung cancer with low-dose computed tomography in adults aging from 55 to 80 years who have a 30 pack-year smoking history and currently smoke or have quit within the past 15 years. Screening should be discontinued once a person has not smoked for 15 years”. However, our study showed that only 22.5% of newly diagnosed lung cancer patients meet this standard. This suggests that USPSTF recommendation may not be suitable for Chinese population. Because Chinese smoking rates, environmental factors, ethnicity and mutation status are different from those in western countries, the age range of patients for LDCT for lung cancer may be adjusted according local factors. Several LDCT lung cancer-screening trials are being carried out in China (20).
In conclusion, this study demonstrated the clinical profiles of lung cancer patients in the mainland of China. However, this single institute study may not fully represent the lung cancer status of the whole region in China.
Acknowledgements
Funding: This work was supported by the General Project (81470212 and U1609220) from the National Natural Science Foundation of China, the Distinguished Young Investigator Award (LR14H010001) and Key Science Project (2015C03043) from Natural Science Foundation of Zhejiang Province.
Ethical Statement: The study was approved by the Institutional ethics committee of SAHZU (2017-031).
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115-32. 10.3322/caac.21338 [DOI] [PubMed] [Google Scholar]
- 2.She J, Yang P, Hong Q, et al. Lung cancer in China: challenges and interventions. Chest 2013;143:1117-26. 10.1378/chest.11-2948 [DOI] [PubMed] [Google Scholar]
- 3.Gao Y, Gao F, Ma JL, et al. Analysis of the characteristics and prognosis of advanced non-small-cell lung cancer in older patients. Patient Prefer Adherence 2015;9:1189-94. 10.2147/PPA.S87069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hong QY, Wu GM, Qian GS, et al. Prevention and management of lung cancer in China. Cancer 2015;121 Suppl 17:3080-8. 10.1002/cncr.29584 [DOI] [PubMed] [Google Scholar]
- 5.Goldstraw P, Crowley J, Chansky K, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol 2007;2:706-14. 10.1097/JTO.0b013e31812f3c1a [DOI] [PubMed] [Google Scholar]
- 6.Lee SH, Ts'o TO. Histological typing of lung cancers in Hong Kong. Br J Cancer 1963;17:37-40. 10.1038/bjc.1963.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan WC, MacLennan R. Lung cancer in Hong Kong Chinese: mortality and histological types, 1960-1972. Br J Cancer 1977;35:226-31. 10.1038/bjc.1977.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kung IT, So KF, Lam TH. Lung cancer in Hong Kong Chinese: mortality and histological types, 1973-1982. Br J Cancer 1984;50:381-8. 10.1038/bjc.1984.187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zou XN, Lin D, Chao A, et al. Histological subtypes of lung cancer in Chinese women from 2000 to 2012. Thorac Cancer 2014;5:447-54. 10.1111/1759-7714.12121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Howlader N, Noone AM, Krapcho M, et al. Bethesda (MD): National Cancer Institute; 2013. SEER cancer statistics review, 1975-2010. Available online: http://seer.cancer.gov/csr/1975_2010/
- 11.Ringer G, Smith JM, Engel AM, et al. Influence of sex on lung cancer histology, stage, and survival in a midwestern United States tumor registry. Clin Lung Cancer 2005;7:180-2. 10.3816/CLC.2005.n.033 [DOI] [PubMed] [Google Scholar]
- 12.Toyoda Y, Nakayama T, Ioka A, et al. Trends in lung cancer incidence by histological type in Osaka, Japan. Jpn J Clin Oncol 2008;38:534-9. 10.1093/jjco/hyn072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jiang X, de Groh M, Liu S, et al. Rising incidence of adenocarcinoma of the lung in Canada. Lung Cancer 2012;78:16-22. 10.1016/j.lungcan.2012.06.002 [DOI] [PubMed] [Google Scholar]
- 14.Zhang L, Li M, Wu N, et al. Time Trends in Epidemiologic Characteristics and Imaging Features of Lung Adenocarcinoma: A Population Study of 21,113 Cases in China. PLoS One 2015;10:e0136727. 10.1371/journal.pone.0136727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herceg Z, Vaissière T. Epigenetic mechanisms and cancer: an interface between the environment and the genome. Epigenetics 2011;6:804-19. 10.4161/epi.6.7.16262 [DOI] [PubMed] [Google Scholar]
- 16.Shi Y, Au JS, Thongprasert S, et al. A prospective, molecular epidemiology study of EGFR mutations in Asian patients with advanced non-small-cell lung cancer of adenocarcinoma histology (PIONEER). J Thorac Oncol 2014;9:154-62. 10.1097/JTO.0000000000000033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shi Y, Li J, Zhang S, et al. Molecular Epidemiology of EGFR Mutations in Asian Patients with Advanced Non-Small-Cell Lung Cancer of Adenocarcinoma Histology - Mainland China Subset Analysis of the PIONEER study. PLoS One 2015;10:e0143515. 10.1371/journal.pone.0143515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reck M, Hagiwara K, Han B, et al. ctDNA Determination of EGFR Mutation Status in European and Japanese Patients with Advanced NSCLC: The ASSESS Study. J Thorac Oncol 2016;11:1682-9. 10.1016/j.jtho.2016.05.036 [DOI] [PubMed] [Google Scholar]
- 19.Kovalchik SA, Tammemagi M, Berg CD, et al. Targeting of low-dose CT screening according to the risk of lung-cancer death. N Engl J Med 2013;369:245-54. 10.1056/NEJMoa1301851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhao SJ, Wu N. Early detection of lung cancer: Low-dose computed tomography screening in China. Thorac Cancer 2015;6:385-9. 10.1111/1759-7714.12253 [DOI] [PMC free article] [PubMed] [Google Scholar]