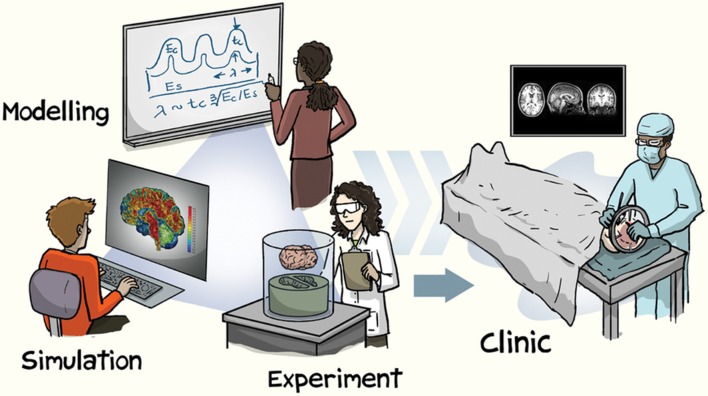
Until recently, neuroimaging data for a research study needed to be collected within one's own lab. However, when studying inter-individual differences in brain structure, a large sample of participants is necessary. Given the financial costs involved in collecting neuroimaging data from hundreds or thousands of participants, large-scale studies of brain morphology could previously only be conducted by well-funded laboratories with access to MRI facilities and to large samples of participants. With the advent of broad open-access data-sharing initiatives, this has recently changed–here the primary goal of the study is to collect large datasets to be shared, rather than sharing of the data as an afterthought. This paradigm shift is evident as increase in the pace of discovery, leading to a rapid rate of advances in our characterization of brain structure. The utility of open-access brain morphology data is numerous, ranging from observing novel patterns of age-related differences in subcortical structures to the development of more robust cortical parcellation atlases, with these advances being translatable to improved methods for characterizing clinical disorders (see Figure 1 for an illustration). Moreover, structural MRIs are generally more robust than functional MRIs, relative to potential artifacts and in being not task-dependent, resulting in large potential yields. While the benefits of open-access data have been discussed more broadly within the field of cognitive neuroscience elsewhere (Van Horn and Gazzaniga, 2013; Poldrack and Gorgolewski, 2014; Van Horn and Toga, 2014; Vogelstein et al., 2016; Voytek, 2016; Gilmore et al., 2017), as well as in other fields (Choudhury et al., 2014; Ascoli et al., 2017; Davies et al., 2017), this opinion paper is focused specifically on the implications of open data to brain morphology research.
Figure 1.
Illustration of approaches involved in brain morphology research. Reprinted with permission from Kuhl (2016), created by Jorge Cham. Copyright 2016, Nature Publishing Group.
Why brain morphology?
Brain morphology is the study of the structural measures of the brain, e.g., volume and shape. Usually these measures are derived from T1 volumes, but other sequences such as T2 and FLAIR can also be useful. When comparing brains of individuals from patient populations with healthy controls, brain morphology can be used to identify differences in brain structure associated with the related medical condition (e.g., Alzheimer's disease or schizophrenia). Brain morphology can also be used to gain a better understanding normative brain development and aging (Frisoni et al., 2011; Falk et al., 2013; Fjell et al., 2014; Lee et al., 2014; Somerville, 2016; Lerch et al., 2017). Furthermore, brain morphology can beneficial in studying cognition, through an individual differences approach (Kanai and Rees, 2011).
As an example of studying memory using brain morphology, one could examine the relationship between behavioral measures of memory performance and structural measures such as hippocampal volume across a large number of individuals or as differences between participant groups (e.g., den Heijer et al., 2012; Ferreira et al., 2017; Olsen et al., 2017; Ritter et al., 2017). In contrast, researchers using fMRI to assess memory would examine differences in brain activity related to memory during encoding or retrieval tasks (i.e., subsequent memory effect [SME] or retrieval success [RS], respectively), looking for temporal fluctuations in regional activation in within-subject contrasts (e.g., Reagh and Yassa, 2014; Richter et al., 2016; Chen et al., 2017; de Chastelaine et al., 2017; Madan et al., 2017). Generally, both of these approaches can be useful, particularly when used as convergent approaches. For instance, while fMRI can provide within-subject estimates of regional brain activity, it is also influenced by age-related differences in BOLD signal variability (Grady and Garrett, 2013; Geerligs et al., 2017; Liu et al., 2017; Nomi et al., 2017), which can be at least partially attributed to effects of aging on neurovasculature (Thomas et al., 2014; Tsvetanov et al., 2015). In addition to aging, it has also been shown that genetic risk factors such as APOE can also be influence BOLD signal estimates (Filippini et al., 2009; Trachtenberg et al., 2012). Nonetheless, differences in brain morphology can, however, correspond to a myriad of inter-individual differences, including personality traits (Bjørnebekk et al., 2013; Holmes et al., 2016; Riccelli et al., 2017), genetic risk factors (Mormino et al., 2014; Strike et al., 2015; Chang et al., 2016), and age-related differences (Sowell et al., 2003; Allen et al., 2005; Fjell et al., 2009; Walhovd et al., 2011; Hogstrom et al., 2013; McKay et al., 2014; Madan and Kensinger, 2016; Cao et al., 2017). Generally, since brain morphology and fMRI studies are susceptible to different confounding factors, the use of both approaches as complementary methods is worth pursuing.
Overview of available datasets
A number of datasets have been organized to advance the broad goal of improving our understanding of human brain structure. Two of the first well-used open-access datasets are Information eXtraction from Images (IXI) and Open Access Series of Imaging Studies (OASIS) (Marcus et al., 2007b, 2010). Briefly, the IXI dataset includes T1, T2, DTI, PD, and MRA data from nearly 581 healthy adults across the adult lifespan (20–86 years old). There are two OASIS datasets, one cross-sectional and one longitudinal. The OASIS cross-sectional dataset consists of T1 scans from 416 adults, aged 18–96, including over 100 adults that have been clinically diagnosed with Alzheimer's disease. The OASIS longitudinal dataset consists of T1 scans from 150 adults, aged 60–96, with at least two visits each and visits separated by at least 1 year; 64 adults were characterized as having dementia at their initial visit.
Currently, the most notable include Alzheimer's Disease Neuroimaging Initiative (ADNI) (Mueller et al., 2005; Jack et al., 2008, 2015; Weiner et al., 2015a), ADHD-200 Consortium (ADHD-200 Consortium, 2012; Bellec et al., 2017), Autism Brain Imaging Data Exchange (ABIDE) (Di Martino et al., 2014), SchizConnect (Ambite et al., 2015; Wang et al., 2016a), 1,000 Functional Connectomes Project (FCP) (Mennes et al., 2013), and the UK Biobank (Miller et al., 2016; Alfaro-Almagro et al., 2017). It is also important to acknowledge the data storage and computation infrastructure developed to manage this unprecedented amount of neuroimaging data, including software such as XNAT (Marcus et al., 2007a), COINS (Scott et al., 2011; Landis et al., 2016), INDI (Mennes et al., 2013; Kennedy et al., 2016), and LORIS/CBRAIN (Das et al., 2012; Sherif et al., 2014; Das et al., 2016), among others (Keator et al., 2009; Redolfi et al., 2009; Crawford et al., 2016).
For those particularly interested in relationships between brain structure and behavior in healthy individuals, the most relevant datasets are the the Human Connectome Project (HCP) (Van Essen et al., 2013; Glasser et al., 2016), Nathan Kline Institute - Rockland Sample (NKI-RS) (Nooner et al., 2012), Brain Genome Superstruct Project (GSP) (Holmes et al., 2015), and Cambridge Centre for Aging and Neuroscience (Cam-CAN) (Shafto et al., 2014; Taylor et al., 2017). Several large-scale developmental studies are also in-progress, including the Developing Human Connectome Project (dHCP) (Makropoulos et al., 2017) Adolescent Brain Cognitive Development (ABCD) study (https://abcdstudy.org), and Healthy Brain Network (Alexander et al., 2017). Additionally, a newly funded project, Lifebrain (http://www.lifebrain.uio.no), will be harmonizing data across eleven large-scale, brain imaging European cohorts, with data collection spanning seven countries and over 6,000 participants.
I currently maintain a list of open-access datasets of structural MRIs that includes further details of these datasets, along with additional datasets not described here, https://github.com/cMadan/openMorph.
Working with open data
Benefits
Apart from the obvious benefit of readily having access to datasets with sample sizes in the hundreds or more, several related benefits and cautions are also important to consider. An important consideration when collecting data for a study is financial cost (Guo et al., 2012; Mar et al., 2013; Poldrack and Gorgolewski, 2014). In this regard, the benefit of using open-access data is simple–the data has already been collected and is free to use. More related to the goals of a particular research question, open-access data can allow for access to populations that may otherwise be unfeasible to recruit–such as middle-age adults, patients, and individuals from other geographic regions. Many studies of aging often recruit young and older adults, but not middle-age adults. While a study's hypothesis may only bear on this comparison, it is also true that middle-age adults are more difficult to recruit (Lachman, 2015). Open-access datasets of aging often take a lifespan approach and do recruit middle-age adults, providing a continuous view of age-related differences in brain morphology. A population that is even harder to recruit from, at least for those without the relevant collaborators, is patient populations. Moreover, when patients are being recruited for a study, additional skills are necessary to appropriately characterize the patient's health and cognitive state–making the sharing of this data particularly valuable for further research, albeit with additional considerations related to the sharing of patient data (see Brakewood and Poldrack, 2013). Data sharing can also be viewed as minimizing the burden on participants, as a single MRI scan can be analyzed by multiple labs, rather than having multiple MRI scans of the same individual. More broadly, since many factors are known to influence brain morphology, it may be desirable to replicate analyses in other samples. Researchers are constrained in where they can recruit participants, but are also often located in areas where there is a so-called WEIRD (Western, Educated, Industrialized, Rich, and Democratic) demographic (Henrich et al., 2010). As such, it is important to also investigate the potential role of education (Kim et al., 2015; Steffener et al., 2016), socioeconomic status (Brito and Noble, 2014; Brito et al., 2017) and cultural backgrounds (Chee et al., 2011). However, this issue of recruitment can be circumvented by sharing data; for instance, many of the datasets included in the Consortium for Reliability and Reproducibility (CoRR) (Zuo et al., 2014) are from participants in China, which can enable researchers in western countries to reproduce their analyses using data from an East Asian sample.
Large open-access datasets, particularly those that are larger than would be commonly collected by a research lab, can further facilitate knowledge discovery by allowing for increased statistical sensitivity to assess distributional properties within samples. For instance, open-access data of patients with Alzheimer's disease has facilitated identifying heterogeneity within patient samples, allowing for the characterization of disease subtypes (Zhang et al., 2016; Dong et al., 2017), while other open-access data has helped establish consistent differences in brain morphology associated with schizophrenia (Moberget et al., 2017). These distribution-related insights are not limited to only characterizing patient populations, as recent findings have also demonstrated sex differences in the volume of many brain structures (Ritchie et al., 2017; Wierenga et al., 2017), with greater variability being found across males than females.
Beyond the discovery of new results directly, the sharing of open-access data is also beneficial to the development of reproducible research methods. In this regard, if everyone has access to the same data, researchers can more readily assess the influence of different analysis pipelines and approaches om morphological results. For instance, cortical thickness estimates produced by different software packages or the correspondence between manually traced structures relative to automated segmentation algorithms.
Cautions and considerations
While the use of open-access data carries many benefits, they should not be used exclusively and to the detriment of future data collection. If specific datasets are solely used to characterize particular samples of individuals, this may result in over-fitting to that particular sample (e.g., if the findings of too many studies are based on a specific dataset). Relatedly, if care is not taken to assess the generalizability of findings, sample biases may become even more pronounced than before–e.g., instead of many researchers sampling participants from WEIRD demographics, they may be studying individuals from a specific location and set of inclusion criteria, despite the researchers themselves being located around the world.
It is also important to consider the metadata collected along with the structural MRI data. While age and sex demographic data will undoubtedly be included, some datasets stop here. If more data is collected, the secondary researcher needs to consider which datasets may be most suitable for the desired research question, as additional metadata–often cognitive or genetic data–will vary between dataests. Furthermore, many factors influence brain morphology estimates, such as head motion (Alexander-Bloch et al., 2016; Pardoe et al., 2016; Savalia et al., 2017) and circadian cycles (Nakamura et al., 2015), and additional consideration is needed to ensure that analyses are conducted appropriately, since the researchers using open data were not involved in data collection process.
When conducting analyses involving multiple datasets, or using data from a multi-site study, caution is also necessary in ‘harmonizing’ data across sites. It is well-established that scanner effects can influence brain morphology estimates (Han et al., 2006; Jovicich et al., 2009, 2013; Iscan et al., 2015; Potvin et al., 2016; Madan and Kensinger, 2017b). Less obvious, however, are considerations related to the sample composition itself. For instance, studies may differ in their inclusion criteria–the presence of Axis-I disorder would result in exclusion for some datasets (e.g., HCP, GSP), but not others (e.g., NKI-RS). In other cases, the proportion of patients to controls may differ between studies, such as between ADNI and AIBL (Australian Imaging Biomarkers and Lifestyle Study of Aging) (Ellis et al., 2009).
Recent advances
Beyond describing existing datasets and their related considerations, some examples of the utility of open-access datasets may be beneficial. The use of large open-access datasets have provided insights into differences in brain structure related to development (Mills et al., 2016) and aging (Cox et al., 2016; Madan and Kensinger, 2016, 2017a; Potvin et al., 2016, 2017; Wang et al., 2016b; DuPre and Spreng, 2017), as well as patient populations (relative to healthy controls) (Franke and Gaser, 2012; Gaser et al., 2013; Cole et al., 2015). These advances have been particularly evident for Alzheimer's disease, where the ADNI dataset has greatly contributed to our understanding of both healthy aging and dementia (Fjell et al., 2012; Zhang et al., 2012; Tamnes et al., 2013; Mormino et al., 2014; Wachinger et al., 2015; Weiner et al., 2015a,b; Wachinger et al., 2016; Coutu et al., 2017).
Providing more nuanced examples of the application of these datasets, they have also been used to develop an improved cortical parcellation atlas based on neuroanatomical landmarks (Klein and Tourville, 2012), as well as computational methods of estimating cortical parcellation and subcortical segmentation structure (Tustison et al., 2014; Redolfi et al., 2015; Wachinger et al., 2015, 2016; Madan and Kensinger, 2016, 2017a; Klein et al., 2017; Saygin et al., 2017). Datasets can also be used to measure the validity of standard morphological methods, such as the test-retest reliability of estimates of brain morphology (Madan and Kensinger, 2017b) and effects of head motion (Pardoe et al., 2016). Moreover, open-access data can be beneficial in methods development for tools designed for quality control and annotation (Heuer et al., 2016; Keshavan et al., 2017).
Despite a number of challenges involved in data sharing (Longo and Drazen, 2016; Mbuagbaw et al., 2017), open-access data is reshaping the field of neuroscience, as well as scientific research as a whole. The advent of open-access neuroimaging data suitable for brain morphology has recently and rapidly begun to move the field forward. In the coming years, I expect our understanding of the relationship between brain structure and inter-individual differences to increase drastically and meaningfully, supported by high-powered studies and the development of improved data analyses methods.
Author contributions
The author confirms being the sole contributor of this work and approved it for publication.
Conflict of interest statement
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
I would like to thank Elizabeth Kensinger and Dan Lurie for feedback on an earlier draft of the manuscript.
Footnotes
Funding. CRM is supported by a fellowship from the Canadian Institutes of Health Research (FRN-146793).
References
- ADHD-200 Consortium (2012). The ADHD-200 consortium: a model to advance the translational potential of neuroimaging in clinical neuroscience. Front. Syst. Neurosci. 6:62 10.3389/fnsys.2012.00062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander L. M., Escalera J., Ai L., Andreotti C., Febre K., Mangone A., et al. (2017). The healthy brain network biobank: an open resource for transdiagnostic research in pediatric mental health and learning disorders. bioRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander-Bloch A., Clasen L., Stockman M., Ronan L., Lalonde F., Giedd J., et al. (2016). Subtle in-scanner motion biases automated measurement of brain anatomy from in vivo MRI. Hum. Brain Mapp. 37, 2385–2397. 10.1002/hbm.23180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfaro-Almagro F., Jenkinson M., Bangerter N. K., Andersson J. L., Griffanti L., Douaud G., et al. (2017). Image processing and quality control for the first 10,000 brain imaging datasets from UK Biobank. bioRxiv. 10.1101/130385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen J. S., Bruss J., Brown C. K., Damasio H. (2005). Normal neuroanatomical variation due to age: the major lobes and a parcellation of the temporal region. Neurobiol. Aging 26, 1245–1260. 10.1016/j.neurobiolaging.2005.05.023 [DOI] [PubMed] [Google Scholar]
- Ambite J. L., Tallis M., Alpert K., Keator D. B., King M., Landis D., et al. (2015). SchizConnect: virtual data integration in neuroimaging. Lect. Notes Comput. Sci. 9162, 37–51. 10.1007/978-3-319-21843-4_4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ascoli G. A., Maraver P., Nanda S., Polavaram S., Armañanzas R. (2017). Win–win data sharing in neuroscience. Nat. Methods 14, 112–116. 10.1038/nmeth.4152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellec P., Chu C., Chouinard-Decorte F., Benhajali Y., Margulies D. S., Craddock R. C. (2017). The neuro bureau ADHD-200 preprocessed repository. NeuroImage 144, 275–286. 10.1016/j.neuroimage.2016.06.034 [DOI] [PubMed] [Google Scholar]
- Bjørnebekk A., Fjell A. M., Walhovd K. B., Grydeland H., Torgersen S., Westlye L. T. (2013). Neuronal correlates of the five factor model (FFM) of human personality: multimodal imaging in a large healthy sample. NeuroImage 65, 194–208. 10.1016/j.neuroimage.2012.10.009 [DOI] [PubMed] [Google Scholar]
- Brakewood B., Poldrack R. A. (2013). The ethics of secondary data analysis: considering the application of Belmont principles to the sharing of neuroimaging data. NeuroImage 82, 671–676. 10.1016/j.neuroimage.2013.02.040 [DOI] [PubMed] [Google Scholar]
- Brito N. H., Noble K. G. (2014). Socioeconomic status and structural brain development. Front. Neurosci. 8:276. 10.3389/fnins.2014.00276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brito N. H., Piccolo L. R., Noble K. G. (2017). Associations between cortical thickness and neurocognitive skills during childhood vary by family socioeconomic factors. Brain Cogn. 116, 54–62. 10.1016/j.bandc.2017.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao B., Mwangi B., Passos I. C., Wu M.-J., Keser Z., Zunta-Soares G. B., et al. (2017). Lifespan gyrification trajectories of human brain in healthy individuals and patients with major psychiatric disorders. Sci. Rep. 7:511. 10.1038/s41598-017-00582-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang L., Douet V., Bloss C., Lee K., Pritchett A., Jernigan T. L., et al. (2016). Gray matter maturation and cognition in children with different APOEϵ genotypes. Neurology 87, 585–594. 10.1212/wnl.0000000000002939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chee M. W. L., Zheng H., Goh J. O. S., Park D., Sutton B. P. (2011). Brain structure in young and old East Asians and Westerners: comparisons of structural volume and cortical thickness. J. Cogn. Neurosci. 23, 1065–1079. 10.1162/jocn.2010.21513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H.-Y., Gilmore A. W., Nelson S. M., McDermott K. B. (2017). Are there multiple kinds of episodic memory? an fMRI investigation comparing autobiographical and recognition memory tasks. J. Neurosci. 37, 2764–2775. 10.1523/JNEUROSCI.1534-16.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choudhury S., Fishman J. R., McGowan M. L., Juengst E. T. (2014). Big data, open science and the brain: lessons learned from genomics. Front. Hum. Neurosci. 8:239. 10.3389/fnhum.2014.00239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole J. H., Leech R., Sharp D. J. (2015). Prediction of brain age suggests accelerated atrophy after traumatic brain injury. Ann. Neurol. 77, 571–581. 10.1002/ana.24367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coutu J.-P., Lindemer E. R., Konukoglu E., Salat D. H. (2017). Two distinct classes of degenerative change are independently linked to clinical progression in mild cognitive impairment. Neurobiol. Aging 54, 1–9. 10.1016/j.neurobiolaging.2017.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox S. R., Ritchie S. J., Tucker-Drob E. M., Liewald D. C., Hagenaars S. P., Davies G., et al. (2016). Ageing and brain white matter structure in 3,513 UK Biobank participants. Nat. Commun. 7:13629. 10.1038/ncomms13629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford K. L., Neu S. C., Toga A. W. (2016). The image and data archive at the laboratory of neuro imaging. NeuroImage 124, 1080–1083. 10.1016/j.neuroimage.2015.04.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das S., Glatard T., MacIntyre L. C., Madjar C., Rogers C., Rousseau M.-E., et al. (2016). The MNI data-sharing and processing ecosystem. NeuroImage 124, 1188–1195. 10.1016/j.neuroimage.2015.08.076 [DOI] [PubMed] [Google Scholar]
- Das S., Zijdenbos A. P., Harlap J., Vins D., Evans A. C. (2012). LORIS: a web-based data management system for multi-center studies. Front. Neuroinform. 5:37. 10.3389/fninf.2011.00037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies T. G., Rahman I. A., Lautenschlager S., Cunningham J. A., Asher R. J., Barrett P. M., et al. (2017). Open data and digital morphology. Proc. R. Soc. B Biol. Sci. 284:20170194. 10.1098/rspb.2017.0194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Chastelaine M., Mattson J. T., Wang T. H., Donley B. E., Rugg M. D. (2017). Independent contributions of fMRI familiarity and novelty effects to recognition memory and their stability across the adult lifespan. NeuroImage 156, 340–351. 10.1016/j.neuroimage.2017.05.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- den Heijer T., van der Lijn F., Vernooij M. W., de Groot M., Koudstaal P. J., van der Lugt A., et al. (2012). Structural and diffusion MRI measures of the hippocampus and memory performance. NeuroImage 63, 1782–1789. 10.1016/j.neuroimage.2012.08.067 [DOI] [PubMed] [Google Scholar]
- Di Martino A., Yan C.-G., Li Q., Denio E., Castellanos F. X., Alaerts K., et al. (2014). The autism brain imaging data exchange: towards a large-scale evaluation of the intrinsic brain architecture in autism. Mol. Psychiatry 19, 659–667. 10.1038/mp.2013.78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong A., Toledo J. B., Honnorat N., Doshi J., Varol E., Sotiras A., et al. (2017). Heterogeneity of neuroanatomical patterns in prodromal Alzheimer's disease: links to cognition, progression and biomarkers. Brain 140, 735–747. 10.1093/brain/aww319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuPre E., Spreng R. N. (2017). Structural covariance networks across the lifespan, from 6-94 years of age. Network Neurosci. [Epub ahead of print]. 10.1162/NETN_a_00016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis K. A., Bush A. I., Darby D., Fazio D. D., Foster J., Hudson P., et al. (2009). The Australian Imaging, Biomarkers and Lifestyle (AIBL) study of aging: methodology and baseline characteristics of 1112 individuals recruited for a longitudinal study of Alzheimer's disease. Int. Psychogeriatr. 21:672. 10.1017/S1041610209009405 [DOI] [PubMed] [Google Scholar]
- Falk E. B., Hyde L. W., Mitchell C., Faul J., Gonzalez R., Heitzeg M. M., et al. (2013). What is a representative brain? neuroscience meets population science. Proc. Natl. Acad. Sci. U.S.A. 110, 17615–17622. 10.1073/pnas.1310134110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira D., Hansson O., Barroso J., Molina Y., Machado A., Hernández-Cabrera J. A., et al. (2017). The interactive effect of demographic and clinical factors on hippocampal volume: a multicohort study on 1958 cognitively normal individuals. Hippocampus 27, 653–667. 10.1002/hipo.22721 [DOI] [PubMed] [Google Scholar]
- Filippini N., MacIntosh B. J., Hough M. G., Goodwin G. M., Frisoni G. B., Smith S. M., et al. (2009). Distinct patterns of brain activity in young carriers of the APOE-ϵ4 allele. Proc. Natl. Acad. Sci. U.S.A. 106, 7209–7214. 10.1073/pnas.0811879106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fjell A. M., McEvoy L., Holland D., Dale A. M., Walhovd K. B. (2014). What is normal in normal aging? effects of aging, amyloid and Alzheimer's disease on the cerebral cortex and the hippocampus. Prog. Neurobiol. 117, 20–40. 10.1016/j.pneurobio.2014.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fjell A. M., Westlye L. T., Amlien I., Espeseth T., Reinvang I., Raz N., et al. (2009). High consistency of regional cortical thinning in aging across multiple samples. Cereb. Cortex 19, 2001–2012. 10.1093/cercor/bhn232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fjell A. M., Westlye L. T., Grydeland H., Amlien I., Espeseth T., Reinvang I., et al. (2012). Accelerating cortical thinning: unique to dementia or universal in aging? Cereb. Cortex 24, 919–934. 10.1093/cercor/bhs379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franke K., Gaser C. (2012). Longitudinal changes in individual BrainAGE in healthy aging, mild cognitive impairment, and Alzheimer's disease. GeroPsych 25, 235–245. 10.1024/1662-9647/a000074 [DOI] [Google Scholar]
- Frisoni G. B., Redolfi A., Manset D., Rousseau M.-É., Toga A., Evans A. C. (2011). Virtual imaging laboratories for marker discovery in neurodegenerative diseases. Nat. Rev. Neurol. 7, 429–438. 10.1038/nrneurol.2011.99 [DOI] [PubMed] [Google Scholar]
- Gaser C., Franke K., Klöppel S., Koutsouleris N., Sauer H. (2013). BrainAGE in mild cognitive impaired patients: predicting the conversion to Alzheimer's disease. PLoS ONE 8:e67346. 10.1371/journal.pone.0067346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geerligs L., Tsvetanov K. A., Cam-CAN, Henson R. N. (2017). Challenges in measuring individual differences in functional connectivity using fMRI: the case of healthy aging. Hum. Brain Mapp. 38, 4125–4156. 10.1002/hbm.23653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore R. O., Diaz M. T., Wyble B. A., Yarkoni T. (2017). Progress toward openness, transparency, and reproducibility in cognitive neuroscience. Ann. N. Y. Acad. Sci. 1396, 5–18. 10.1111/nyas.13325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasser M. F., Smith S. M., Marcus D. S., Andersson J. L. R., Auerbach E. J., Behrens T. E. J., et al. (2016). The Human Connectome Project's neuroimaging approach. Nat. Neurosci. 19, 1175–1187. 10.1038/nn.4361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grady C. L., Garrett D. D. (2013). Understanding variability in the BOLD signal and why it matters for aging. Brain Imaging Behav. 8, 274–283. 10.1007/s11682-013-9253-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Q., Hall G., McKinnon M., Thabane L., Goeree R., Pullenayegum E. (2012). Setting sample size using cost efficiency in fMRI studies. Open Access Med. Stat. 2, 33–41. 10.2147/OAMS.S30830 [DOI] [Google Scholar]
- Han X., Jovicich J., Salat D., van der Kouwe A., Quinn B., Czanner S., et al. (2006). Reliability of MRI-derived measurements of human cerebral cortical thickness: the effects of field strength, scanner upgrade and manufacturer. NeuroImage 32, 180–194. 10.1016/j.neuroimage.2006.02.051 [DOI] [PubMed] [Google Scholar]
- Henrich J., Heine S. J., Norenzayan A. (2010). The weirdest people in the world? Behav. Brain Sci. 33, 61–83. 10.1017/S0140525X0999152X [DOI] [PubMed] [Google Scholar]
- Heuer K., Ghosh S., Sterling A. R., Toro R. (2016). Open neuroimaging laboratory. Res. Ideas Outcomes 2:e9113 10.3897/rio.2.e9113 [DOI] [Google Scholar]
- Hogstrom L. J., Westlye L. T., Walhovd K. B., Fjell A. M. (2013). The structure of the cerebral cortex across adult life: age-related patterns of surface area, thickness, and gyrification. Cereb. Cortex 23, 2521–2530. 10.1093/cercor/bhs231 [DOI] [PubMed] [Google Scholar]
- Holmes A. J., Hollinshead M. O., O'Keefe T. M., Petrov V. I., Fariello G. R., Wald L. L., et al. (2015). Brain genomics superstruct project initial data release with structural, functional, and behavioral measures. Sci. Data 2:150031. 10.1038/sdata.2015.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes A. J., Hollinshead M. O., Roffman J. L., Smoller J. W., Buckner R. L. (2016). Individual differences in cognitive control circuit anatomy link sensation seeking, impulsivity, and substance use. J. Neurosci. 36, 4038–4049. 10.1523/JNEUROSCI.3206-15.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iscan Z., Jin T. B., Kendrick A., Szeglin B., Lu H., Trivedi M., et al. (2015). Test-retest reliability of FreeSurfer measurements within and between sites: effects of visual approval process. Hum. Brain Mapp. 36, 3472–3485. 10.1002/hbm.22856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack C. R., Barnes J., Bernstein M. A., Borowski B. J., Brewer J., Clegg S., et al. (2015). Magnetic resonance imaging in Alzheimer's Disease Neuroimaging Initiative. Alzheimer's Dement. 11, 740–756. 10.1016/j.jalz.2015.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack C. R., Bernstein M. A., Fox N. C., Thompson P., Alexander G., Harvey D., et al. (2008). The Alzheimer's disease neuroimaging initiative (ADNI): MRI methods. J. Magn. Reson. Imaging 27, 685–691. 10.1002/jmri.21049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jovicich J., Czanner S., Han X., Salat D., van der Kouwe A., Quinn B., et al. (2009). MRI-derived measurements of human subcortical, ventricular and intracranial brain volumes: reliability effects of scan sessions, acquisition sequences, data analyses, scanner upgrade, scanner vendors and field strengths. NeuroImage 46, 177–192. 10.1016/j.neuroimage.2009.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jovicich J., Marizzoni M., Sala-Llonch R., Bosch B., Bartrés-Faz D., Arnold J., et al. (2013). Brain morphometry reproducibility in multi-center 3T MRI studies: a comparison of cross-sectional and longitudinal segmentations. NeuroImage 83, 472–484. 10.1016/j.neuroimage.2013.05.007 [DOI] [PubMed] [Google Scholar]
- Kanai R., Rees G. (2011). The structural basis of inter-individual differences in human behaviour and cognition. Nat. Rev. Neurosci. 12, 231–242. 10.1038/nrn3000 [DOI] [PubMed] [Google Scholar]
- Keator D., Wei D., Gadde S., Bockholt H., Grethe J., Marcus D., et al. (2009). Derived data storage and exchange workflow for large-scale neuroimaging analyses on the BIRN grid. Front. Neuroinform. 3:30. 10.3389/neuro.11.030.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy D. N., Haselgrove C., Riehl J., Preuss N., Buccigrossi R. (2016). The NITRC image repository. NeuroImage 124, 1069–1073. 10.1016/j.neuroimage.2015.05.074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keshavan A., Datta E., McDonough I. M., Madan C. R., Jordan K., Henry R. G. (2017). Mindcontrol: a web application for brain segmentation quality control. NeuroImage. [Epub ahead of print]. 10.1016/j.neuroimage.2017.03.055 [DOI] [PubMed] [Google Scholar]
- Kim J. P., Seo S. W., Shin H. Y., Ye B. S., Yang J.-J., Kim C., et al. (2015). Effects of education on aging-related cortical thinning among cognitively normal individuals. Neurology 85, 806–812. 10.1212/WNL.0000000000001884 [DOI] [PubMed] [Google Scholar]
- Klein A., Ghosh S. S., Bao F. S., Giard J., Häme Y., Stavsky E., et al. (2017). Mindboggling morphometry of human brains. PLoS Comput. Biol. 13:e1005350. 10.1371/journal.pcbi.1005350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein A., Tourville J. (2012). 101 labeled brain images and a consistent human cortical labeling protocol. Front. Neurosci. 6:171. 10.3389/fnins.2012.00171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhl E. (2016). Unfolding the brain. Nat. Phys. 12, 533–534. 10.1038/nphys3641 [DOI] [Google Scholar]
- Lachman M. E. (2015). Mind the gap in the middle: a call to study midlife. Res. Hum. Dev. 12, 327–334. 10.1080/15427609.2015.1068048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landis D., Courtney W., Dieringer C., Kelly R., King M., Miller B., et al. (2016). COINS data exchange: an open platform for compiling, curating, and disseminating neuroimaging data. NeuroImage 124, 1084–1088. 10.1016/j.neuroimage.2015.05.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee F. S., Heimer H., Giedd J. N., Lein E. S., Šestan N., Weinberger D. R., et al. (2014). Adolescent mental health–opportunity and obligation. Science 346, 547–549. 10.1126/science.1260497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerch J. P., van der Kouwe A. J. W., Raznahan A., Paus T., Johansen-Berg H., Miller K. L., et al. (2017). Studying neuroanatomy using MRI. Nat. Neurosci. 20, 314–326. 10.1038/nn.4501 [DOI] [PubMed] [Google Scholar]
- Liu X., Gerraty R. T., Grinband J., Parker D., Razlighi Q. R. (2017). Brain atrophy can introduce age-related differences in BOLD response. Hum. Brain Mapp. 38, 3402–3414. 10.1002/hbm.23597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longo D. L., Drazen J. M. (2016). Data sharing. New Engl. J. Med. 374, 276–277. 10.1056/NEJMe1516564 [DOI] [PubMed] [Google Scholar]
- Madan C. R., Fujiwara E., Caplan J. B., Sommer T. (2017). Emotional arousal impairs association-memory: roles of amygdala and hippocampus. NeuroImage 156, 14–28. 10.1016/j.neuroimage.2017.04.065 [DOI] [PubMed] [Google Scholar]
- Madan C. R., Kensinger E. A. (2016). Cortical complexity as a measure of age-related brain atrophy. NeuroImage 134, 617–629. 10.1016/j.neuroimage.2016.04.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madan C. R., Kensinger E. A. (2017a). Age-related differences in the structural complexity of subcortical and ventricular structures. Neurobiol. Aging 50, 87–95. 10.1016/j.neurobiolaging.2016.10.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madan C. R., Kensinger E. A. (2017b). Test–retest reliability of brain morphology estimates. Brain Inform. 4, 107–121. 10.1007/s40708-016-0060-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makropoulos A., Robinson E. C., Schuh A., Wright R., Fitzgibbon S., Bozek J., et al. (2017). The developing human connectome project: a minimal processing pipeline for neonatal cortical surface reconstruction. bioRxiv. 10.1101/125526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mar R. A., Spreng R. N., DeYoung C. G. (2013). How to produce personality neuroscience research with high statistical power and low additional cost. Cogn. Affect. Behav. Neurosci. 13, 674–685. 10.3758/s13415-013-0202-6 [DOI] [PubMed] [Google Scholar]
- Marcus D. S., Fotenos A. F., Csernansky J. G., Morris J. C., Buckner R. L. (2010). Open Access Series of Imaging Studies: longitudinal MRI data in nondemented and demented older adults. J. Cogn. Neurosci. 22, 2677–2684. 10.1162/jocn.2009.21407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus D. S., Olsen T. R., Ramaratnam M., Buckner R. L. (2007a). The extensible neuroimaging archive toolkit. Neuroinformatics 5, 11–33. 10.1385/NI:5:1:11 [DOI] [PubMed] [Google Scholar]
- Marcus D. S., Wang T. H., Parker J., Csernansky J. G., Morris J. C., Buckner R. L. (2007b). Open Access Series of Imaging Studies (OASIS): cross-sectional MRI data in young, middle aged, nondemented, and demented older adults. J. Cogn. Neurosci. 19, 1498–1507. 10.1162/jocn.2007.19.9.1498 [DOI] [PubMed] [Google Scholar]
- Mbuagbaw L., Foster G., Cheng J., Thabane L. (2017). Challenges to complete and useful data sharing. Trials 18:71. 10.1186/s13063-017-1816-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay D. R., Knowles E. E. M., Winkler A. A. M., Sprooten E., Kochunov P., Olvera R. L., et al. (2014). Influence of age, sex and genetic factors on the human brain. Brain Imaging Behav. 8, 143–152. 10.1007/s11682-013-9277-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennes M., Biswal B. B., Castellanos F. X., Milham M. P. (2013). Making data sharing work: the FCP/INDI experience. NeuroImage 82, 683–691. 10.1016/j.neuroimage.2012.10.064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller K. L., Alfaro-Almagro F., Bangerter N. K., Thomas D. L., Yacoub E., Xu J., et al. (2016). Multimodal population brain imaging in the UK Biobank prospective epidemiological study. Nat. Neurosci. 19, 1523–1536. 10.1038/nn.4393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills K. L., Goddings A.-L., Herting M. M., Meuwese R., Blakemore S.-J., Crone E. A., et al. (2016). Structural brain development between childhood and adulthood: convergence across four longitudinal samples. NeuroImage 141, 273–281. 10.1016/j.neuroimage.2016.07.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moberget T., Doan N. T., Alnæs D., Kaufmann T., Córdova-Palomera A., Lagerberg T. V., et al. (2017). Cerebellar volume and cerebellocerebral structural covariance in schizophrenia: a multisite mega-analysis of 983 patients and 1349 healthy controls. Mol. Psychiatry. [Epub ahead of prnt]. 10.1038/mp.2017.106 [DOI] [PubMed] [Google Scholar]
- Mormino E. C., Betensky R. A., Hedden T., Schultz A. P., Ward A., Huijbers W., et al. (2014). Amyloid and APOE ϵ4 interact to influence short-term decline in preclinical Alzheimer disease. Neurology 82, 1760–1767. 10.1212/WNL.0000000000000431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller S. G., Weiner M. W., Thal L. J., Petersen R. C., Jack C. R., Jagust W., et al. (2005). Ways toward an early diagnosis in Alzheimer's disease: the Alzheimer's Disease Neuroimaging Initiative (ADNI). Alzheimer's Dement. 1, 55–66. 10.1016/j.jalz.2005.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura K., Brown R. A., Narayanan S., Collins D. L., Arnold D. L. (2015). Diurnal fluctuations in brain volume: Statistical analyses of MRI from large populations. NeuroImage 118, 126–132. 10.1016/j.neuroimage.2015.05.077 [DOI] [PubMed] [Google Scholar]
- Nomi J. S., Bolt T. S., Ezie C. C., Uddin L. Q., Heller A. S. (2017). Moment-to-moment BOLD signal variability reflects regional changes in neural flexibility across the lifespan. J. Neurosci. 37, 5539–5548. 10.1523/JNEUROSCI.3408-16.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nooner K. B., Colcombe S. J., Tobe R. H., Mennes M., Benedict M. M., Moreno A. L., et al. (2012). The NKI-Rockland sample: a model for accelerating the pace of discovery science in psychiatry. Front. Neurosci. 6:152. 10.3389/fnins.2012.00152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen R. K., Yeung L.-K., Noly-Gandon A., D'Angelo M. C., Kacollja A., Smith V. M., et al. (2017). Human anterolateral entorhinal cortex volumes are associated with cognitive decline in aging prior to clinical diagnosis. Neurobiol. Aging 57, 195–205. 10.1016/j.neurobiolaging.2017.04.025 [DOI] [PubMed] [Google Scholar]
- Pardoe H. R., Hiess R. K., Kuzniecky R. (2016). Motion and morphometry in clinical and nonclinical populations. NeuroImage 135, 177–185. 10.1016/j.neuroimage.2016.05.005 [DOI] [PubMed] [Google Scholar]
- Poldrack R. A., Gorgolewski K. J. (2014). Making big data open: data sharing in neuroimaging. Nat. Neurosci. 17, 1510–1517. 10.1038/nn.3818 [DOI] [PubMed] [Google Scholar]
- Potvin O., Dieumegarde L., Duchesne S. (2017). FreeSurfer cortical normative data for adults using Desikan-Killiany-Tourville and ex vivo protocols. NeuroImage 156, 43–64. 10.1016/j.neuroimage.2017.04.035 [DOI] [PubMed] [Google Scholar]
- Potvin O., Mouiha A., Dieumegarde L., Duchesne S. (2016). Normative data for subcortical regional volumes over the lifetime of the adult human brain. NeuroImage 137, 9–20. 10.1016/j.neuroimage.2016.05.016 [DOI] [PubMed] [Google Scholar]
- Reagh Z. M., Yassa M. A. (2014). Object and spatial mnemonic interference differentially engage lateral and medial entorhinal cortex in humans. Proc. Natl. Acad. Sci. U.S.A. 111, E4264–E4273. 10.1073/pnas.1411250111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redolfi A., Manset D., Barkhof F., Wahlund L.-O., Glatard T., Mangin J.-F., et al. (2015). Head-to-head comparison of two popular cortical thickness extraction algorithms: a cross-sectional and longitudinal study. PLoS ONE 10:e0117692. 10.1371/journal.pone.0117692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redolfi A., McClatchey R., Anjum A., Zijdenbos A., Manset D., Barkhof F., et al. (2009). Grid infrastructures for computational neuroscience: the neuGRID example. Future Neurol. 4, 703–722. 10.2217/fnl.09.53 [DOI] [Google Scholar]
- Riccelli R., Toschi N., Nigro S., Terracciano A., Passamonti L. (2017). Surface-based morphometry reveals the neuroanatomical basis of the five-factor model of personality. Soc. Cogn. Affect. Neurosci. 12, 671–684. 10.1093/scan/nsw175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter F. R., Cooper R. A., Bays P. M., Simons J. S. (2016). Distinct neural mechanisms underlie the success, precision, and vividness of episodic memory. eLife 5:e18260. 10.7554/eLife.18260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritchie S. J., Cox S. R., Shen X., Lombardo M. V., Reus L. M., Alloza C., et al. (2017). Sex differences in the adult human brain: evidence from 5,216 UK Biobank participants. bioRxiv. 10.1101/123729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritter A., Hawley N., Banks S. J., Miller J. B. (2017). The association between montreal cognitive assessment memory scores and hippocampal volume in a neurodegenerative disease sample. J. Alzheimer's Dis. 58, 695–699. 10.3233/JAD-161241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savalia N. K., Agres P. F., Chan M. Y., Feczko E. J., Kennedy K. M., Wig G. S. (2017). Motion-related artifacts in structural brain images revealed with independent estimates of in-scanner head motion. Hum. Brain Mapp. 38, 472–492. 10.1002/hbm.23397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saygin Z. M., Kliemann D., Iglesias J. E., van der Kouwe A. J. W., Boyd E., Reuter M., et al. (2017). High-resolution magnetic resonance imaging reveals nuclei of the human amygdala: manual segmentation to automatic atlas. NeuroImage 155, 370-382. 10.1016/j.neuroimage.2017.04.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott A., Courtney W., Wood D., de la Garza R., Lane S., King M., et al. (2011). COINS: an innovative informatics and neuroimaging tool suite built for large heterogeneous datasets. Front. Neuroinform. 5:33. 10.3389/fninf.2011.00033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafto M. A., Tyler L. K., Dixon M., Taylor J. R., Rowe J. B., Cusack R., et al. (2014). The cambridge centre for ageing and neuroscience (Cam-CAN) study protocol: a cross-sectional, lifespan, multidisciplinary examination of healthy cognitive ageing. BMC Neurol. 14:204. 10.1186/s12883-014-0204-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherif T., Rioux P., Rousseau M.-E., Kassis N., Beck N., Adalat R., et al. (2014). CBRAIN: a web-based, distributed computing platform for collaborative neuroimaging research. Front. Neuroinform. 8:54. 10.3389/fninf.2014.00054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerville L. H. (2016). Searching for signatures of brain maturity: what are we searching for? Neuron 92, 1164–1167. 10.1016/j.neuron.2016.10.059 [DOI] [PubMed] [Google Scholar]
- Sowell E. R., Peterson B. S., Thompson P. M., Welcome S. E., Henkenius A. L., Toga A. W. (2003). Mapping cortical change across the human life span. Nat. Neurosci. 6, 309–315. 10.1038/nn1008 [DOI] [PubMed] [Google Scholar]
- Steffener J., Habeck C., O'Shea D., Razlighi Q., Bherer L., Stern Y. (2016). Differences between chronological and brain age are related to education and self-reported physical activity. Neurobiol. Aging 40, 138–144. 10.1016/j.neurobiolaging.2016.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strike L. T., Couvy-Duchesne B., Hansell N. K., Cuellar-Partida G., Medland S. E., Wright M. J. (2015). Genetics and brain morphology. Neuropsychol. Rev. 25, 63–96. 10.1007/s11065-015-9281-1 [DOI] [PubMed] [Google Scholar]
- Tamnes C. K., Walhovd K. B., Dale A. M., Østby Y., Grydeland H., Richardson G., et al. (2013). Brain development and aging: overlapping and unique patterns of change. NeuroImage 68, 63–74. 10.1016/j.neuroimage.2012.11.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor J. R., Williams N., Cusack R., Auer T., Shafto M. A., Dixon M., et al. (2017). The Cambridge Centre for Ageing and Neuroscience (Cam-CAN) data repository: structural and functional MRI, MEG, and cognitive data from a cross-sectional adult lifespan sample. NeuroImage 144, 262–269. 10.1016/j.neuroimage.2015.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas B. P., Liu P., Park D. C., van Osch M. J. P., Lu H. (2014). Cerebrovascular reactivity in the brain white matter: magnitude, temporal characteristics, and age effects. J. Cere. Blood Flow Metab. 34, 242–247. 10.1038/jcbfm.2013.194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trachtenberg A. J., Filippini N., Mackay C. E. (2012). The effects of APOE-ϵ4 on the BOLD response. Neurobiol. Aging 33, 323–334. 10.1016/j.neurobiolaging.2010.03.009 [DOI] [PubMed] [Google Scholar]
- Tsvetanov K. A., Henson R. N. A., Tyler L. K., Davis S. W., Shafto M. A., Taylor J. R., et al. (2015). The effect of ageing on fMRI: Correction for the confounding effects of vascular reactivity evaluated by joint fMRI and MEG in 335 adults. Hum. Brain Mapp. 36, 2248–2269. 10.1002/hbm.22768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tustison N. J., Cook P. A., Klein A., Song G., Das S. R., Duda J. T., et al. (2014). Large-scale evaluation of ANTs and FreeSurfer cortical thickness measurements. NeuroImage 99, 166–179. 10.1016/j.neuroimage.2014.05.044 [DOI] [PubMed] [Google Scholar]
- Van Essen D. C., Smith S. M., Barch D. M., Behrens T. E. J., Yacoub E., Ugurbil K. (2013). The WU-Minn Human Connectome Project: an overview. NeuroImage 80, 62–79. 10.1016/j.neuroimage.2013.05.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Horn J. D., Gazzaniga M. S. (2013). Why share data? lessons learned from the fMRIDC. NeuroImage 82, 677–682. 10.1016/j.neuroimage.2012.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Horn J. D., Toga A. W. (2014). Human neuroimaging as a 'big data' science. Brain Imaging Behav. 8, 323–331. 10.1007/s11682-013-9255-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogelstein J. T., Mensh B., Häusser M., Spruston N., Evans A. C., Kording K., et al. (2016). To the cloud! a grassroots proposal to accelerate brain science discovery. Neuron 92, 622–627. 10.1016/j.neuron.2016.10.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voytek B. (2016). The virtuous cycle of a data ecosystem. PLoS Comput. Biol. 12:e1005037. 10.1371/journal.pcbi.1005037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wachinger C., Golland P., Kremen W., Fischl B., Reuter M. (2015). BrainPrint: a discriminative characterization of brain morphology. NeuroImage 109, 232–248. 10.1016/j.neuroimage.2015.01.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wachinger C., Salat D. H., Weiner M., Reuter M. (2016). Whole-brain analysis reveals increased neuroanatomical asymmetries in dementia for hippocampus and amygdala. Brain 139, 3253–3266. 10.1093/brain/aww243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walhovd K. B., Westlye L. T., Amlien I., Espeseth T., Reinvang I., Raz N., et al. (2011). Consistent neuroanatomical age-related volume differences across multiple samples. Neurobiol. Aging 32, 916–932. 10.1016/j.neurobiolaging.2009.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Alpert K. I., Calhoun V. D., Cobia D. J., Keator D. B., King M. D., et al. (2016a). SchizConnect: mediating neuroimaging databases on schizophrenia and related disorders for large-scale integration. NeuroImage 124, 1155–1167. 10.1016/j.neuroimage.2015.06.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Necus J., Kaiser M., Mota B. (2016b). Universality in human cortical folding in health and disease. Proc. Natl. Acad. Sci. U.S.A. 113, 12820–12825. 10.1073/pnas.1610175113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner M. W., Veitch D. P., Aisen P. S., Beckett L. A., Cairns N. J., Cedarbaum J., et al. (2015a). Impact of the Alzheimer's Disease Neuroimaging Initiative, 2004 to 2014. Alzheimer's Dement. 11, 865–884. 10.1016/j.jalz.2015.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner M. W., Veitch D. P., Aisen P. S., Beckett L. A., Cairns N. J., Cedarbaum J., et al. (2015b). 2014 update of the Alzheimer's Disease Neuroimaging Initiative: a review of papers published since its inception. Alzheimer's Dement. 11, e1–e120. 10.1016/j.jalz.2014.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wierenga L. M., Sexton J. A., Laake P., Giedd J. N., Tamnes C. K. (2017). A key characteristic of sex differences in the developing brain: greater variability in brain structure of boys than girls. Cereb. Cortex. 10.1093/cercor/bhx154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang N., Song X., Zhang Y. (2012). Combining structural brain changes improves the prediction of Alzheimer's disease and mild cognitive impairment. Dementia Geriatr. Cogn. Disord. 33, 318–326. 10.1159/000339364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Mormino E. C., Sun N., Sperling R. A., Sabuncu M. R., Yeo B. T. T. (2016). Bayesian model reveals latent atrophy factors with dissociable cognitive trajectories in alzheimer's disease. Proc. Natl. Acad. Sci. U.S.A. 113, E6535–E6544. 10.1073/pnas.1611073113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuo X.-N., Anderson J. S., Bellec P., Birn R. M., Biswal B. B., Blautzik J., et al. (2014). An open science resource for establishing reliability and reproducibility in functional connectomics. Sci. Data 1:140049. 10.1038/sdata.2014.49 [DOI] [PMC free article] [PubMed] [Google Scholar]