Abstract
Background
B-type natriuretic peptide (BNP) has prognostic significance in heart failure (HF), and reductions in BNP may predict clinical improvement. However, there are limited data regarding the prognostic value of BNP during short-term follow-up. The aim of this study was to evaluate the relationship between short-term follow-up BNP and mortality after discharge in patients with HF.
Methods
We analyzed 427 patients hospitalized with HF from the Wonju Severance Christian Hospital Heart Failure Registry from April 2011 to December 2013, with a planned follow-up period through February 2016. Of the 427 patients, 240 (mean age, 75 years; 102 males, 42.5%) had BNP measured on admission and within the short-term follow-up period (3 months). We compared all-cause mortality during the clinical follow-up period (median length of follow-up, 709.5 days) according to the median value of BNP on admission (as a baseline value) and over a short-term follow-up period after discharge.
Results
Median BNP at admission was 816.5 pg/ml, and median follow-up BNP was 369.7 pg/ml. Multivariate analysis revealed a positive association between risk of death and high BNP. High BNP during follow-up was significantly associated with a greater risk of all-cause mortality compared to low BNP (P < 0.001). Initial BNP was not significantly associated with all-cause mortality. A multivariate model showed that follow-up BNP and percent change in BNP were independently associated with all-cause mortality after adjustment for covariates. Of the 3 BNP measurement strategies, BNP after discharge (IDI of 0.072, P < .0001 and NRI of 0.707, P < .0001) and percent change in BNP (IDI of 0.113, P < .0001 and NRI of 0.782, P < .0001) demonstrated the greatest increase in discrimination and net reclassification for mortality. Unfortunately, we did not find any significant value with initial BNP. Kaplan-Meier survival analysis was performed to assess mortality stratified by BNP according to the median value, high median of follow-up BNP and percent change in BNP were associated with significantly higher mortality compared to the below median (log-rank, p < 0.001).
Conclusions
Short-term follow-up BNP and percent change in BNP level are significant prognostic factors of all-cause mortality. These values will be clinically useful when evaluating prognosis in hospitalized patients with heart failure.
Keywords: B-type natriuretic peptide, Heart failure, Prognosis
Background
Heart failure (HF) is a global public health concern, especially in countries with aging populations where diagnosis, treatment, and prevention of re-hospitalization are challenging [1]. Unfortunately, repeated hospitalization exerts a huge cost on national healthcare budgets and diminishes quality of life [2]. It is important to predict a patient’s clinical course as early as possible by selecting evidence-based management strategies that improve the care of patients with acute HF. Risk stratification in these patients is challenging [3].The use of natriuretic peptides in the diagnosis of acute HF is well established [4]. Moreover, a peptide that correlates with intra-cardiac pressure is expected to reflect prognosis and predict both short- and long-term outcomes of HF [5]. According to the guidelines of the European Society of Cardiology (ESC) and American College of Cardiology Foundation/American Heart Association (ACCF/AHA), the biomarker B-type natriuretic peptide (BNP) is the most reliable tool for diagnosing HF, establishing prognosis or disease severity, and guiding treatment planning by indicating the need for treatment intensification [6, 7]. Natriuretic peptides such as BNP are counter-regulatory hormones involved in volume homeostasis and cardiovascular remodeling; they have also become promising cardiac markers in various HF settings, especially since the advent of rapid assays [8, 9]. Serial changes in BNP can act as surrogate markers in patients with progressive HF, and these values give incremental prognostic information and help track therapeutic response [10, 11]. A change in BNP during hospitalization appears to predict outcomes in patients with acute decompensated HF (ADHF), providing incremental prognostic value beyond baseline measurement [12]. Also, understanding BNP levels through the early period after discharge may help expedite treatment initiation and allow lower-risk patients to transit more rapidly through the system. However, most studies have evaluated patients only during hospitalization [13, 14]. Variation in BNP level during short-term follow-up is associated with both the degree of congestive status and clinical outcomes [15]. Therefore, this study aimed to evaluate the prognostic value of short-term follow-up BNP and the change in BNP after discharge for predicting mortality of hospitalized patients with HF.
Methods
Study population
This study used a subset of data from a larger cohort study, the Korean Heart Failure (KorAHF) registry [16]. We used prospectively collected data for retrospective study analysis. We have only considered same inclusion criteria and registry for sub-set data collection by following the reference. This is the part of Korean HF registry. We performed a single-center cohort study using these data. Patients were diagnosed with acute HF and were admitted to Wonju Severance Christian Hospital (Wonju, Korea).
Data related to in-hospital outcomes and one-year follow-up mortality of 427 consecutive patients who were hospitalized with an episode of acute HF were prospectively collected between April 2011 and December 2013, with a planned follow-up period through February 2016. Data collection, study management, and data validation were performed according to the methods of the KorAHF registry [16]. Study data were obtained for patients with HF if one of the following criteria was met: (i) lung congestion or (ii) findings indicative of LV systolic dysfunction or structural heart disease. Lung congestion was defined as congestion on chest X-ray or as detection of rales on medical examination. Written informed consent was obtained from each patient. If patients were unable to provide consent due to disease severity or other reasons, informed consent was obtained from relatives or a legal guardian. Follow-up data were collected from patients by the attending physician, who completed a web-based case report form. Data were stored in the Clinical Data Management System (iCReaT) under the Korea National Institute of Health (NIH) with the assistance of a clinical research coordinator. In-hospital mortality has been decided by an independent event committee. Mortality data for patients who were lost to follow-up was collected from the National Death Records [16]. The endpoint of the present investigation was defined as all-cause mortality, and the study participants were followed for 730 days from the time they were admitted to the hospital or until death if it occurred earlier. Mortality data were obtained from the National Death Records. All 240 patients underwent follow-up. Variables included demographic and baseline characteristics, medical history, clinical presentation, laboratory tests, hospital course, and clinical outcomes during admission and after one-year of follow-up. We performed echocardiography 1 or 2 days after admission according to the patient’s condition. Initial echocardiographic measurements obtained during index admission were also collected. We evaluated LV end-diastolic volume (LVEDV), LV end-systolic volume (LVESV) and LV ejection fraction (LVEF) parameters using a modified version of Simpson’s method. We did not evaluate echocardiography after 3 months.
Measurement of BNP
In this study, we selected all the patients that included only BNP level. Plasma BNP level was measured at admission and at the first visit to the outpatient clinic after discharge for short-term follow-up of acute HF. The second blood collection for BNP measurement was performed within 92 days of admission. The median time to second collection was 22 (16 to 33) days. We selected 3 months as the endpoint for the short-term follow-up BNP. All plasma samples were obtained in plastic tubes containing potassium ethylene diamine tetra-acetic acid (Becton Dickinson, Franklin Lakes, NJ, USA) in amounts that ranged from 3 to 5 ml. All samples were centrifuged, and plasma was tested for BNP using the Biosite Triage assay, a point-of-care device that uses a fluorescence immunoassay technique (Biosite, San Diego, CA, USA). The total coefficient of variation at different levels of plasma BNP was reported to be <7% using the control samples provided by the manufacturer. The sensitivity for BNP of these measurements ranged from 5 pg/ml to 5000 pg/ml [17].
Statistical analysis
Baseline characteristics between the alive and dead group were compared with Mann-Whitney test for continuous variables. Categorical variables are presented as frequency (percentage) and were analyzed via Chi-square test. The prognostic value of the biomarkers was assessed by investigating the relationship with mortality using logistic regression analysis. We categorized the baseline and follow-up biomarker values by median. We used a crude model and models with degrees of adjustment. First, we performed an age- and sex-adjusted analysis (model 1). Second, we adjusted model 1 by including clinical characteristics for hypertension, diabetes, ischemic heart disease chronic obstructive pulmonary disease, chronic kidney disease (CKD), and stroke (model 2). Finally, we adjusted model 2 by including sodium (Na), creatinine (Cr), hemoglobin (Hb) and echocardiographic LVEF (model 3). The increased discriminative value of these biomarkers was examined by calculation of AUC, NRI and IDI. All-cause mortality was estimated with the Kaplan-Meier method and compared using the log-rank test. Statistical significance was set at p < 0.05 for all comparisons. All analyses were performed using SAS statistical software (version 9.0; SAS Institute Inc., Cary, NC).
Results
Demographic characteristics and clinical profiles
This study enrolled 427 HF patients who had both initial and follow-up BNP data. Patients who died in the hospital and those without follow-up BNP were excluded.
We used several exclusion criteria. BNP value is usually increased in CKD patients, so we excluded patients with a creatinine value >2 (43 nos). Those patients who died in hospital after admission were also excluded (20 nos). Those for whom BNP (follow-up = 53 nos), LVEF (14 nos), or clinical outcome data (i.e., mortality) (3 nos) were not available were also excluded. The short-term follow-up period was defined as within 3 months of discharge. Those for whom the BNP value was measured after more than 3 months (54 nos) were not considered (Fig. 1).
Fig. 1.
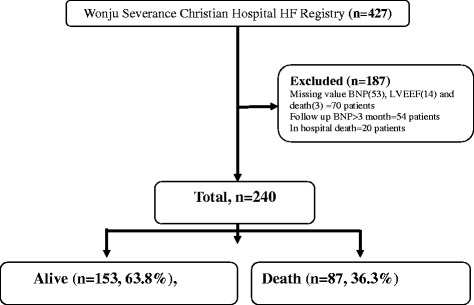
Selection of the study population. This study enrolled 427 patients. We excluded those patients with a creatinine value >2; those who died in-hospital; those for whom the BNP, LVEF, or clinical outcome value (i.e., mortality) was not available; and those for whom the BNP value was measured after more than 3 months. Finally, we analyzed 240 patients, including 153 (63.8%) with alive and 87 (36.3%) with death
The median length of follow-up was 709.5 days (range, 10 to 1477 days). During the follow-up period, 87 (36.3%) patients died. One-year mortality was 47 (19.6%). The median age of the study population was 75 years, and 42.5% of patients were male. Median BNP was 816.5 pg/ml at admission and 369.7 pg/ml on follow-up (median BNP follow-up duration, 22 days).
Baseline characteristics of patients are summarized in Table 1. Age, creatinine level, and the incidence of diabetes (42.5%), hypertension (81.6%), CKD (10.3%), and stroke (25.3%) were significantly higher in patients who died during follow-up compared to those who lived. However, de novo HF (74.5%) was significantly more common among patients who lived than patients who died. In contrast, hemoglobin and sodium were similar between the two groups, and echocardiographic measurements also did not differ significantly.
Table 1.
Baseline characteristics between the alive and death group
| Alive (n = 153) | Death (n = 87) | P value | |
|---|---|---|---|
| Age (years) | 73(63 to 80) | 78(71 to 82) | <0.001 |
| Males | 63 (41.2) | 39 (44.8) | 0.582 |
| BMI (kg/m2) | 22.8(20.5 to 24.8) | 22.5(20.2 to 25.5) | 0.418 |
| Medical history: | |||
| DM | 40 (26.1) | 37 (42.5) | 0.009 |
| HTN | 89 (58.2) | 71 (81.6) | <0.001 |
| Congestion | 131 (85.6) | 72 (82.8) | 0.555 |
| De novo HF | 114 (74.5) | 47 (54) | 0.001 |
| COPD | 20 (13.1) | 17 (19.5) | 0.182 |
| CKD | 5 (3.3) | 9 (10.3) | 0.025 |
| IHD | 35(22.9) | 33(37.9) | 0.013 |
| Stroke | 16 (10.5) | 22 (25.3) | 0.002 |
| AF | 28 (18.3) | 20 (23) | 0.383 |
| SBP | 140(120.5 to 158) | 135(119.5 to 157) | 0.352 |
| Echocardiography | |||
| LVESV (mL) | 99(57 to 144.5) | 82(53 to 137) | 0.195 |
| LVEDV (mL) | 183(142 to 236.5) | 169(129 to 214) | 0.072 |
| LVEF (%) | 41(32 to 53) | 44(32 to 55) | 0.388 |
| Laboratory findings | |||
| Hs-CRP (mg/dL) | 0.5(0.2 to 2.4) | 1.1(0.3 to 2.5) | 0.143 |
| Hb (g/dL) | 12.8(11.6 to 14.2) | 12.8(10.4 to 12.9) | <0.001 |
| Cr (mg/dL) | 0.900(0.8 to 1.2) | 1.1(0.8 to 1.3) | 0.002 |
| Na (mmol/L) | 139(137 to 141) | 138(135 to 140) | <0.001 |
| Initial BNP (pg/mL) | 808.4(497.9 to 1325.3) | 872.1(571.3 to 1587.9) | 0.165 |
| Follow up BNP (pg/mL) | 282.5(136.2 to 487.3) | 617.7(319.1 to 1260) | <0.001 |
| (%) Changes of BNP | −66.1(−81.3 to −37.4) | −31.1(−57 to 36.2) | <0.001 |
Values are expressed as median (25th to 75th) or n (%). BMI body mass index, DM diabetes mellitus, HTN hypertension, HF heart failure, COPD chronic obstructive pulmonary disease, CKD chronic kidney disease, IHD ischemic heart disease, left bundle branch block, AF atrial fibrillation, SBP systolic blood pressure, LV left ventricular, ESV end-systolic volume, EDV end-diastolic volume, EF ejection fraction, Hs-CRP high-sensitivity C-reactive protein, Hb Hemoglobin, Cr creatinine, Na sodium, BNP brain natriuretic peptide
The change in median BNP at admission or initial was not significantly different between the two groups (dead: 872.1 (571.3 to 1587.9) pg/ml; alive: 808.4 (497.9 to 1325.3) pg/ml, p = 0.165). However, follow-up BNP was significantly greater in patients who died 617.7 (319.1 to 1260) pg/ml compared to those who lived 282.5 (136.2 to 487.3) pg/ml, p < 0.001). Moreover, the median percent change in BNP differed significantly between the two groups (alive: −66.1 (−81.3 to −37.4) %; dead: −31.1 (−57 to 36.2) %, p < 0.001) (Table 1).
Association between BNP and mortality
Logistic regression analysis demonstrated that in the crude model, follow-up BNP and percent change in BNP were significantly associated with mortality. Additionally, when some selective baseline variables (e.g., age, sex, clinical characteristics, Hb, Na and echocardiographic LVEF) were adjusted in the multiple logistic regression model, whereas mortality was the dependent variable; we also found similar results for BNP after discharge and percent change in BNP, which could independently predict primary outcome. However, we did not find any significant association between initial BNP and mortality (Table 2).
Table 2.
Logistic analysis of BNP at admission, after discharge and (%) changes of BNP (according to the median value) for predicting mortality
| BNP | Model | OR (95% CI) | p-value | |
|---|---|---|---|---|
| Initial BNP | Crude model | <816.5 | 1 | 0.6871 |
| ≥816.5 | 1.114 (0.658 ~ 1.887) | |||
| Model 1 | <816.5 | 1 | 0.4891 | |
| ≥816.5 | 1.215 (0.70 ~ 2.107) | |||
| Model 2 | <816.5 | 1 | 0.5791 | |
| ≥816.5 | 1.184 (0.652 ~ 2.152) | |||
| Model 3 | <816.5 | 1 | 0.8117 | |
| ≥816.5 | 0.920 (0.465 ~ 1.822) | |||
| Follow up BNP | Crude model | <370 | 1 | <.0001 |
| ≥370 | 4.30 (2.426 ~ 7.621) | |||
| Model 1 | <370 | 1 | <.0001 | |
| ≥370 | 4.373 (2.406 ~ 7.946) | |||
| Model 2 | <370 | 1 | <.0001 | |
| ≥370 | 4.438 (2.331 ~ 8.450) | |||
| Model 3 | <370 | 1 | <.0001 | |
| ≥370 | 4.703 (2.360 ~ 9.374) | |||
| (%) Changes of BNP | Crude model | <−0.52 | 1 | <.0001 |
| ≥ − 0.52 | 5.118 (2.852 ~ 9.184) | |||
| Model 1 | <−0.52 | 1 | <.0001 | |
| ≥ − 0.52 | 6.331 (3.353 ~ 11.954) | |||
| Model 2 | <−0.52 | 1 | <.0001 | |
| ≥ − 0.52 | 6.838 (3.418 ~ 13.68) | |||
| Model 3 | <−0.52 | 1 | <.0001 | |
| ≥ − 0.52 | 7.344 (3.518 ~ 15.331) | |||
Model 1 = Age and sex
Model 2 = Model 1+ diabetes mellitus, hypertension, ischemic heart disease, chronic obstructive pulmonary disease, chronic kidney disease and stroke
Model 3 = Model 2 + sodium (Na), creatinine (Cr), hemoglobin (Hb) and EF
Kaplan-Meier survival analysis was performed to assess mortality stratified by BNP according to the median value. This analysis revealed that the high median of follow-up BNP and percent change in BNP were associated with significantly higher mortality compared to the below median (log-rank, p < 0.001) (Fig. 2).
Fig. 2.
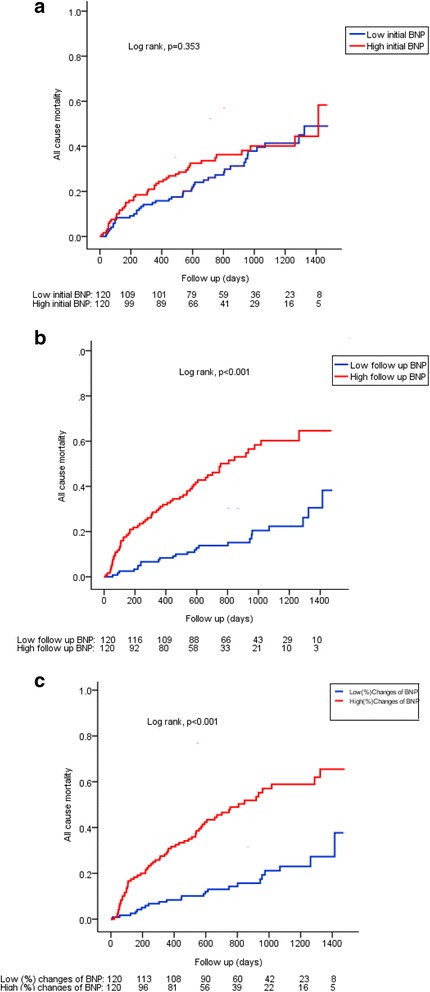
Kaplan-Meier analysis displaying mortality stratified by median value of initial BNP (a), follow-up BNP (b) and (%) changes of BNP (c). High follow up BNP and percent changes of BNP were associated with a higher mortality as compared to low median value (Log-rank, p = <0.001)
Incremental discrimination
The AUC was 0.782 (0.722 ~ 0.842) for the traditional model, which was constructed by using selective baseline variables including age, sex, diabetes mellitus, hypertension, ischemic heart disease, chronic obstructive pulmonary disease, CKD, stroke, Na, Cr, Hb and EF. When we added BNP to the traditional model, we found an AUC of 0.828 (0.777 ~ 0.879) (P = 0.0205) for follow-up BNP and 0.852 (0.805 ~ 0.899) (P = 0.0023) for percent change in BNP. Furthermore, we compared the discrimination and NRI for each measurement of BNP level in the 240 patients with both admission and discharge BNP data available (Table 3). Of the 3 BNP measurement strategies, BNP after discharge (IDI of 0.072, P < .0001 and NRI of 0.707, P < .0001) and percent change in BNP (IDI of 0.113, P < .0001 and NRI of 0.782, P < .0001) provided the greatest increase in discrimination and net reclassification for mortality. There were no significant associations with initial BNP.
Table 3.
Area under curve (AUC), net reclassification improvement (NRI) and integrated discrimination improvement (IDI).for specific models using the 240 Patients with BNP at admission, after discharge and (%) changes of BNP
| BNP | death | ||
|---|---|---|---|
| value | p-value | ||
| Initial BNP | AUC (95% CI) | ||
| Traditional model | 0.782 (0.722 ~ 0.842) | - | |
| Traditional model + BNP at admission | 0.783 (0.724 ~ 0.843) | 0.4683 | |
| NRI (95% CI) | 0.014 (−0.25 ~ 0.278) | 0.9183 | |
| IDI (95% CI) | 0.00013 (−0.002 ~ 0.002) | 0.8909 | |
| Follow up BNP | AUC (95% CI) | ||
| Traditional model | 0.782 (0.722 ~ 0.842) | - | |
| Traditional model + BNP at discharge | 0.828 (0.777 ~ 0.879) | 0.0205 | |
| NRI (95% CI) | 0.707 (0.465 ~ 0.949) | <.0001 | |
| IDI (95% CI) | 0.072 (0.037 ~ 0.106) | <.0001 | |
| (%) Changes of BNP | AUC (95% CI) | ||
| Traditional model | 0.782 (0.722 ~ 0.842) | - | |
| Traditional model + BNP change | 0.852 (0.805 ~ 0.899) | 0.0023 | |
| NRI (95% CI) | 0.782 (0.544 ~ 1.021) | <.0001 | |
| IDI (95% CI) | 0.113 (0.071 ~ 0.155) | <.0001 | |
Traditional model: Age, sex, diabetes mellitus, hypertension, ischemic heart disease, chronic obstructive pulmonary disease, chronic kidney disease, stroke, sodium (Na), creatinine (Cr), hemoglobin (Hb) and EF
Discussion
We found that both short-term follow-up BNP after discharge and percent change in BNP between admission and follow-up were powerful prognostic markers of mortality in hospitalized patients with HF. In contrast, BNP at admission was not associated with mortality risk. Furthermore, we observed that the high median of follow-up BNP after discharge and percent change in BNP was associated with higher mortality than the below median. This association persisted after adjustment for potential confounders. BNP after discharge and percent change in BNP were independent predictors of mortality.
Many studies have found that BNP level at admission provides useful information for the diagnosis of HF, the assessment of HF severity, and the prognosis of high-risk patients during the early follow-up period [10, 18]. One study that used data from the KorAHF registry found a difference in risk stratification pattern, especially in patients with low NT-proBNP levels [19]. In general, patients with low BNP usually have better prognoses than those with high BNP [19].
Patients hospitalized for HF who are identified as high risk could be scheduled for earlier outpatient visits with a physician and may require follow-up appointments for better outcomes [20]. As expected, BNP concentration 1 month after hospital discharge was the strongest prognostic factor. Another study suggested that HF patients with the highest percentage decrease in BNP 4 months after discharge have the lowest mortality and morbidity [5]. However, no randomized controlled trials have tested whether such data can be used to improve outcomes or have determined the best time for BNP follow-up [18]. In the current study, we found the best cut-off value for monitoring the prognosis of HF to be 294.01 pg/ml for short-term follow-up BNP (within 3 months of discharge; median, 22 days). Median BNP level decreased from 816.5 pg/ml to 369.7 pg/ml (median percent change in BNP, −52.2%) over the 3-month follow-up period. Moreover, short-term follow-up BNP after discharge and percent change in BNP from admission to discharge were associated with mortality. These data may motivate clinicians to measure BNP after discharge to monitor patient outcomes [21]. In Asian countries, including Korea, China, and Japan, the prevalence of HF in the population has increased due to aging of the population and adoption of a Western lifestyle [22]. A few studies have been performed in Asian populations and have revealed that BNP at admission is the most powerful prognostic factor of mortality in patients with HF, and that high levels of BNP are significantly associated with poor outcomes [19, 23]. Most of the studies were designed to investigate the significance of admission BNP for HF patients. Very few studies have explored short-term follow-up BNP. In this study, we mainly focused on Korean HF patients and the effects of short term (90-day) follow-up BNP on prognosis. We also compared the prognostic value of admission BNP, follow-up BNP and percent change in BNP. We measured BNP at admission and at the first follow-up visit to the outpatient clinic after discharge. During the 90-day short term follow-up period after discharge, many patients were lost to follow-up. Thus, unfortunately, our study population is small. However, we analyzed BNP at admission and after discharge and the percent change in BNP and found that the high median for both follow-up BNP and percent change in BNP after short-term follow-up were associated with greater mortality than the below median. We did not find any association between BNP at admission and mortality. After adjustment for covariates of age, sex, clinical characteristics, Hb, Na, and echocardiographic measurement, short-term BNP after discharge and percent change in BNP still predicted mortality. In previous studies, various factors have limited the standard time for evaluating plasma BNP in the prediction of long-term outcomes after discharge [24]. A number of studies have been conducted at single centers or with small sample sizes, limiting the evaluation of the relationship between BNP and other important clinical characteristics; other studies have had variable follow-up times and heterogeneous endpoints [24]. Among those studies that explored the prognostic value of BNP at admission and after discharge, several have also concluded that measurement of BNP at discharge was a strong prognostic marker in HF [25, 26]. One well-designed prospective cohort study of patients with acute HF found that the pre-discharge BNP and percent change in BNP provided conclusive prognostic information and predicted mortality and readmission [27]. Another large, single-center study revealed that high pre-discharge BNP is the most significant predictor of 6-month outcomes and is a more relevant predictor than change in BNP during acute care [2]. However, those studies had small sample sizes, which limited their ability to adjust for covariates [2]. Other studies have found that the percent reduction in natriuretic peptide during HF admission is a powerful predictor of outcome, but the sample sizes were relatively small (less than 200 patients), limiting their ability to control for confounding variables [13, 28]. In the Valsartan Heart Failure Trial (Val-HeFT), BNP was measured at randomization and at the fourth month in patients with chronic HF. The results suggested that percent change in neurohormones such as BNP is associated with mortality and morbidity, thus supporting their role as important surrogate markers in HF [29, 30]. Although there is currently no standard follow-up duration after discharge, our results suggest that short-term follow-up BNP and change in BNP are important metrics for predicting mortality and morbidity in patients with HF. Baseline BNP reflects hemodynamic stress regardless of cause or severity, while follow-up BNP and change in BNP reflect treatment response and hemodynamic status after treatment. Therefore, follow-up BNP and change in BNP are more powerful than baseline BNP for predicting morality or morbidity [18, 31].
HFpEF, defined as symptomatic HF with a normal or almost normal ejection fraction and diastolic dysfunction, accounts for about one-half of patients hospitalized for acute HF [5, 32, 33]. HFpEF patients have comorbidities that can drive myocardial dysfunction and concentric remodeling due to progressive loss of cardiomyocytes with increased relative wall thickness and a relatively preserved LV diameter, resulting in a high ratio of mass to volume. Patients with HFrEF have an enlarged LV cavity but fairly normal LV wall thickness, and exchange of dead cardiomyocytes by collagen creates patchy areas of fibrosis [34, 35]. BNP is a cardiac neurohormone that is primarily exudated from the ventricles in response to increases in wall tension and volume overload [36]. Patients with HFpEF who have lower wall tension thus have lower natriuretic peptide levels than those with HFrEF [37]. The KorAHF registry revealed that the plasma level of natriuretic peptide at baseline or at admission is the most powerful prognostic factor in both HFpEF and HFrEF, and it is also useful for risk-stratifying patients with HF [19]. We used similar inclusion criteria for patients from the same registry; however, we selected whole acute HF patient without any differentiation; interestingly, we found no relationship between BNP at admission and mortality. These differences might be due to the role of baseline BNP in reflecting baseline hemodynamic change, regardless of the cause of HF and severity of underlying disease. Moreover, multiple factors affect the BNP level [18]. Furthermore, when we used new statistical analysis methods (NRI and IDI), we found that BNP after discharge (IDI of 0.072, P < .0001 and NRI of 0.707, P < .0001) and percent change in BNP (IDI of 0.113, P < .0001 and NRI of 0.782, P < .0001) demonstrated the greatest increase in discrimination and net reclassification for mortality. This study was limited by a small population. Though the sample size was small but the study was chosen as a cohort study and most of the analytic data set had able to give significance in both FU-BNP and percent changes BNP with little variations. Moreover, a greater decrease in the percent change of BNP from admission to discharge increased the survival rate.
Study limitations
First, this was a cohort study, so the study design had several inherent limitations, including selection bias and uncontrolled confounding factors. Second, discharge medications and a measure of functional status were not available; therefore, we could not adjust for the use of evidence-based medical therapy or NYHA functional class. Finally, we did not analyze re-hospitalization by HF, so we could not determine whether BNP was a significant predictor of composite mortality and morbidity.
Conclusion
Short-term follow-up BNP after discharge and percent change in BNP are significant prognostic markers of mortality for hospitalized patients with HF. These values are clinically useful for the evaluation of patient prognosis.
Acknowledgements
None.
Funding
This research received no funding from any agency in the public, commercial or not-for-profit sectors.
Availability of data and materials
According to hospital regulations it is prohibited to publicly release datasets. Data release would cause concern from local ethical committees based on current institution regulations. Data are available from the “Wonju Severance Christian Hospital” Institutional Data Access/Ethics Committee for researchers who meet the criteria for access to confidential data. The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- AF
Atrial fibrillation
- BMI
Body mass index
- BNP
Brain natriuretic peptide
- CKD
Chronic kidney disease
- Cr
Creatinine
- DM
Diabetes mellitus
- EDV
End-diastolic volume
- EF
Ejection fraction
- ESV
End-systolic volume
- Hb
Hemoglobin
- HF
Heart failure
- HFpEF
Heart failure with preserved ejection faction
- HFrEF
Heart failure with reduced ejection faction
- Hs-CRP
High-sensitivity C-reactive protein
- HTN
Hypertension
- LV
Left ventricular
- Na
Sodium
- SBP
Systolic blood pressure
Authors’ contributions
SSK had full access to, interpreted, statistical analysis, validation of datasets, and drafting the manuscript, BSY and SSK provided the conception and design of the study, performed data collection and drafting of the manuscript, and take responsibility for the integrity of the data and the accuracy of data analysis. JWS provided validation and analysis of the data, SSK, JWS, JWL, YJY, JHY, SHL, JYK, SGA, MSA, and BSY performed data collection and revised the manuscript. BSY provided the conception of the study and critical review of the manuscript. BSY supported the administrative and technical materials. All authors supervised the study, reviewed the manuscript for important intellectual content, and read and approved the final manuscript.
Ethics approval and consent to participate
This study was approved by the ethics/institutional review board committee of the Heart Failure Cohort (Board Number: CR311003) at Wonju Severance Christian Hospital in Wonju, South Korea. According to the regulations of the ethics/IRB committee a prospective cohort study was conducted and data collection, study management, and data validation were performed according to the methods of the KorAHF (Korean Acute Heart failure) registry. The period of registration was from April 2011 to December 2013. All personal information was recorded prior to data analysis in accordance with the Declaration of Helsinki and South Korean ethics. Written informed consent was obtained from each patient. If patients were unable to provide consent due to disease severity or other reasons, informed consent was obtained from relatives or a legal guardian.
Consent for publication
We obtained consent from the patient, or in the case of children, their parent or legal guardian. We used an institutional form to record consent. We preserved all consent documents and copies can be provided upon request.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sayma Sabrina Khanam, Email: saymaditi@gmail.com.
Jung-Woo Son, Email: soneycar@gmail.com.
Jun-Won Lee, Email: ljwcardio@yonsei.ac.kr.
Young Jin Youn, Email: younyj@yonsei.ac.kr.
Junghan Yoon, Email: jyoon@yonsei.ac.kr.
Seung-Hwan Lee, Email: carshlee@yonsei.ac.kr.
Jang-Young Kim, Email: kimjy@yonsei.ac.kr.
Sung Gyun Ahn, Email: sgahn@yonsei.ac.kr.
Min-Soo Ahn, Email: heartsaver@yonsei.ac.kr.
Byung-Su Yoo, Email: yubs@yonsei.ac.kr.
References
- 1.Bosseau C, Galli E, Donal E. Prognostic value of BNP in heart failure with preserved or reduced ejection fraction. Heart. 2015;101(23):1881–8. [DOI] [PubMed]
- 2.Logeart D, et al. Predischarge B-type natriuretic peptide assay for identifying patients at high risk of re-admission after decompensated heart failure. J Am Coll Cardiol. 2004;43(4):635–641. doi: 10.1016/j.jacc.2003.09.044. [DOI] [PubMed] [Google Scholar]
- 3.Noveanu M, et al. Direct comparison of serial B-type natriuretic peptide and NT-proBNP levels for prediction of short- and long-term outcome in acute decompensated heart failure. Crit Care. 2011;15(1):R1. doi: 10.1186/cc9398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maisel AS, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347(3):161–167. doi: 10.1056/NEJMoa020233. [DOI] [PubMed] [Google Scholar]
- 5.Wright GA, Struthers AD. Natriuretic peptides as a prognostic marker and therapeutic target in heart failure. Heart. 2006;92(2):149–151. doi: 10.1136/hrt.2003.018325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ponikowski P, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the heart failure association (HFA) of the ESC. Eur J Heart Fail, 2016. 2016;18(8):891–975. doi: 10.1002/ejhf.592. [DOI] [PubMed] [Google Scholar]
- 7.Yancy CW, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2013;62(16):e147–e239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 8.Yoo B-S. Biomarkers in heart failure: focus on B-type Natriuretic peptide. Korean J Med. 2012;82(6):647. doi: 10.3904/kjm.2012.82.6.647. [DOI] [Google Scholar]
- 9.Fonarow GC, et al. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol. 2007;49(19):1943–1950. doi: 10.1016/j.jacc.2007.02.037. [DOI] [PubMed] [Google Scholar]
- 10.Ho KK, et al. Survival after the onset of congestive heart failure in Framingham heart study subjects. Circulation. 1993;88(1):107–115. doi: 10.1161/01.CIR.88.1.107. [DOI] [PubMed] [Google Scholar]
- 11.Latini R, et al. Incremental prognostic value of changes in B-type natriuretic peptide in heart failure. Am J Med. 2006;119(1):70. doi: 10.1016/j.amjmed.2005.08.041. [DOI] [PubMed] [Google Scholar]
- 12.Januzzi JL, Jr, et al. Natriuretic peptide testing for predicting adverse events following heart failure hospitalization. Congest Heart Fail. 2012;18(Suppl 1):S9–s13. doi: 10.1111/j.1751-7133.2012.00306.x. [DOI] [PubMed] [Google Scholar]
- 13.Bettencourt P, et al. N-terminal-pro-brain natriuretic peptide predicts outcome after hospital discharge in heart failure patients. Circulation. 2004;110(15):2168–2174. doi: 10.1161/01.CIR.0000144310.04433.BE. [DOI] [PubMed] [Google Scholar]
- 14.Bayes-Genis A, et al. N-terminal probrain natriuretic peptide (NT-proBNP) in the emergency diagnosis and in-hospital monitoring of patients with dyspnoea and ventricular dysfunction. Eur J Heart Fail. 2004;6(3):301–308. doi: 10.1016/j.ejheart.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 15.Chung I-H, et al. The relationship between the early follow-up BNP level and congestive status or prognosis in acute heart failure. Korean Circulation J. 2006;36:200–207. doi: 10.4070/kcj.2006.36.3.200. [DOI] [Google Scholar]
- 16.Lee SE, et al. A multicentre cohort study of acute heart failure syndromes in Korea: rationale, design, and interim observations of the Korean acute heart failure (KorAHF) registry. Eur J Heart Fail. 2014;16(6):700–708. doi: 10.1002/ejhf.91. [DOI] [PubMed] [Google Scholar]
- 17.Choi H, et al. The optimal time of B-type natriuretic peptide sampling associated with post-myocardial infarction remodelling after primary percutaneous coronary intervention. Cardiovasc J Afr. 2013;24(5):165–170. doi: 10.5830/CVJA-2013-024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahn M-S, Yoo B-S. Serial monitoring of B-type Natriuretic peptide in heart failure patients. Korean Circ J 2007. 2007;37:393–398. doi: 10.4070/kcj.2007.37.9.393. [DOI] [Google Scholar]
- 19.Kang SH, et al. Prognostic value of NT-proBNP in heart failure with preserved versus reduced EF. Heart. 2015;101(23):1881–1888. doi: 10.1136/heartjnl-2015-307782. [DOI] [PubMed] [Google Scholar]
- 20.Hernandez AF, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303(17):1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 21.Flint KM, et al. B-type natriuretic peptide predicts 30-day readmission for heart failure but not readmission for other causes. J Am Heart Assoc. 2014;3(3):e000806. doi: 10.1161/JAHA.114.000806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee JH, et al. Epidemiology of heart failure in Korea: present and future. Korean Circ J. 2016;46(5):658–664. doi: 10.4070/kcj.2016.46.5.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krim SR, et al. Racial/ethnic differences in B-type natriuretic peptide levels and their association with care and outcomes among patients hospitalized with heart failure: findings from get with the guidelines-heart failure. JACC Heart Fail. 2013;1(4):345–352. doi: 10.1016/j.jchf.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 24.Kociol RD, et al. Admission, discharge, or change in B-type natriuretic peptide and long-term outcomes: data from organized program to initiate lifesaving treatment in hospitalized patients with heart failure (OPTIMIZE-HF) linked to Medicare claims. Circ Heart Fail. 2011;4(5):628–636. doi: 10.1161/CIRCHEARTFAILURE.111.962290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cheng V, et al. A rapid bedside test for B-type peptide predicts treatment outcomes in patients admitted for decompensated heart failure: a pilot study. J Am Coll Cardiol. 2001;37(2):386–391. doi: 10.1016/S0735-1097(00)01157-8. [DOI] [PubMed] [Google Scholar]
- 26.Verdiani V, et al. Pre-discharge B-type natriuretic peptide predicts early recurrence of decompensated heart failure in patients admitted to a general medical unit. Eur J Heart Fail. 2005;7(4):566–571. doi: 10.1016/j.ejheart.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 27.Cournot M, et al. Optimization of the use of B-type natriuretic peptide levels for risk stratification at discharge in elderly patients with decompensated heart failure. Am Heart J. 2008;155(6):986–991. doi: 10.1016/j.ahj.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 28.Bayes-Genis A, et al. NT-ProBNP reduction percentage during admission for acutely decompensated heart failure predicts long-term cardiovascular mortality. J Card Fail. 2005;11(5 Suppl):S3–S8. doi: 10.1016/j.cardfail.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 29.Anand IS, Florea VG, Fisher L. Surrogate end points in heart failure. J Am Coll Cardiol. 2002;39(9):1414–1421. doi: 10.1016/S0735-1097(02)01773-4. [DOI] [PubMed] [Google Scholar]
- 30.Anand IS, et al. Changes in brain natriuretic peptide and norepinephrine over time and mortality and morbidity in the Valsartan heart failure trial (Val-HeFT) Circulation. 2003;107(9):1278–1283. doi: 10.1161/01.CIR.0000054164.99881.00. [DOI] [PubMed] [Google Scholar]
- 31.Yoo BS. Clinical significance of B-type Natriuretic peptide in heart failure. J Lifestyle Med. 2014;4(1):34–38. doi: 10.15280/jlm.2014.4.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Owan TE, et al. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355(3):251–259. doi: 10.1056/NEJMoa052256. [DOI] [PubMed] [Google Scholar]
- 33.Bhatia RS, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med. 2006;355(3):260–269. doi: 10.1056/NEJMoa051530. [DOI] [PubMed] [Google Scholar]
- 34.Aurigemma GP, Zile MR, Gaasch WH. Contractile behavior of the left ventricle in diastolic heart failure: with emphasis on regional systolic function. Circulation. 2006;113(2):296–304. doi: 10.1161/CIRCULATIONAHA.104.481465. [DOI] [PubMed] [Google Scholar]
- 35.Paulus WJ, Tschope C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol. 2013;62(4):263–271. doi: 10.1016/j.jacc.2013.02.092. [DOI] [PubMed] [Google Scholar]
- 36.Nakagawa O, et al. Rapid transcriptional activation and early mRNA turnover of brain natriuretic peptide in cardiocyte hypertrophy. Evidence for brain natriuretic peptide as an “emergency” cardiac hormone against ventricular overload. J Clin Invest. 1995;96(3):1280–1287. doi: 10.1172/JCI118162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maisel AS, et al. Bedside B-type natriuretic peptide in the emergency diagnosis of heart failure with reduced or preserved ejection fraction. Results from the breathing not properly multinational study. J Am Coll Cardiol. 2003;41(11):2010–2017. doi: 10.1016/S0735-1097(03)00405-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
According to hospital regulations it is prohibited to publicly release datasets. Data release would cause concern from local ethical committees based on current institution regulations. Data are available from the “Wonju Severance Christian Hospital” Institutional Data Access/Ethics Committee for researchers who meet the criteria for access to confidential data. The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.


