Both MUC1 and CK19 PCR‐based detection of circulating tumor cells (CTC) have been reported in breast cancer patients (Xenidis et al., 2006; Felton et al., 2004), but their respective long term prognostic value has not been compared. Moreover, immunomagnetic selection of epithelial cells followed by a double detection technique improves the specificity of the analysis. From October 1996 to October 1998, we have prospectively analyzed blood samples of 94 breast cancer patients for the presence of CTC, by means of MUC1 RT‐qPCR and CK19 RT‐nested‐PCR. Patients had stage I (n=21), stage II (n=25), stage III (n=25) and stage IV (metastatic, n=23) breast cancers. CTC were isolated from whole peripheral blood with BerEP4‐coated immunomagnetic beads. Total RNA was extracted and reverse transcribed before analysis by real‐time PCR of a MUC1‐specific cDNA sequence (de Cremoux et al., 2000) and nested‐PCR CK19 detection of a specific cDNA sequence (Denis et al., 1997). False positive detection rates were assessed on 28 patients with benign breast disease and were 11 and 3%, respectively (nonsignificant). None of the control group was positive for both CK19 and MUC1, in contrast to nine of the 14 patients with metastatic breast cancer who were positive for at least one marker. CTC detection was strongly associated with tumor stage for both MUC1 and CK19 markers (p=0.02 and p=0.001, respectively, chi‐square) and was independent of other prognostic factors like age, pT, pN, tumor grade or hormonal receptor status. At a median follow up of 9 years (111 months), presence of CTC, detected by CK19 or MUC1 expression, was associated with poor overall survival in the whole population of breast cancer patients (p=0.02, log rank). This prognosis impact of CTC detection was seen in high risk patients, namely locally advanced (stage III) and metastatic (stage IV) (p=D;0.002, log rank) but was not significant in poor risk, localized, breast cancer patients (Figures 1 and 2). This finding is in accordance with the results obtained by an automatized immunocytostaining method in a large cohort of stage IV breast cancer patients (Cristofanilli et al., 2004). Interestingly, we found no relevant difference between prognosis issues (overall survival) of MUC1 and/or CK19, MUC1 only and CK19 only based detection. The double criteria MUC1 and CK19 did not show valuable prognostic significance in any subgroup. Although our study has been conducted in a small cohort, these results show that CTC keep a significant prognosis value at long term on high risk breast cancer patients, that MUC1 and CK19 have similar long term impact, and that a double detection does not improve the prognostic value of CTC.
Figure 1.
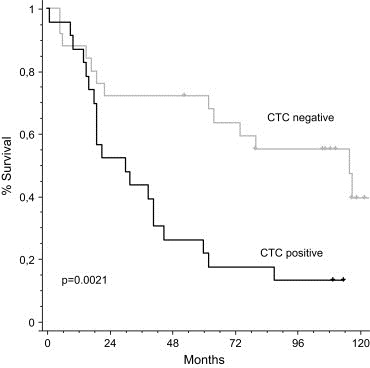
Overall survival in high risk breast cancer patients (stages III and IV, n=48) according to CTC status (MUC1 and/or CK19 positive).
Figure 2.
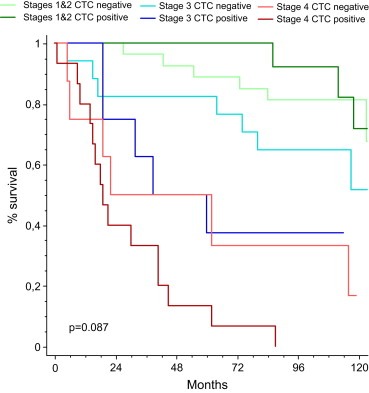
Overall survival in stages I and II, III and IV breast cancer patients (n=94) according to CTC detection.
Supporting information
Supplementary data
Acknowledgments
We thank Drs E. Bourstyn, K.B. Clough, C. Nos (Surgery Department) and Dr B. Asselain (Biostatistics Department).
Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.molonc.2007.09.005.
Pierga J.-Y., Bidard F.-C., Denis M.G., de Cremoux P., (2007), Prognostic value of peripheral blood double detection of CK19 and MUC1 mRNA positive cells detected by RT‐quantitative PCR in 94 breast cancer patients with a follow up of 9 years, Molecular Oncology, 1, doi: 10.1016/j.molonc.2007.09.005.
References
- Cristofanilli, M. , Budd, G.T. , Ellis, M.J. , Stopeck, A. , Matera, J. , Miller, M.C. , Reuben, J.M. , Doyle, G.V. , Allard, W.J. , Terstappen, L.W. , 2004. Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N. Engl. J. Med.. 351, 781–791. [DOI] [PubMed] [Google Scholar]
- de Cremoux, P. , Extra, J.M. , Denis, M.G. , Pierga, J.Y. , Bourstyn, E. , Nos, C. , Clough, K.B. , Boudou, E. , Martin, E.C. , Muller, A. , 2000. Detection of MUC1-expressing mammary carcinoma cells in the peripheral blood of breast cancer patients by real-time polymerase chain reaction. Clin. Cancer Res.. 6, 3117–3122. [PubMed] [Google Scholar]
- Denis, M.G. , Lipart, C. , Leborgne, J. , LeHur, P.A. , Galmiche, J.P. , Denis, M. , Ruud, E. , Truchaud, A. , Lustenberger, P. , 1997. Detection of disseminated tumor cells in peripheral blood of colorectal cancer patients. Int. J. Cancer. 74, 540–544. [DOI] [PubMed] [Google Scholar]
- Felton, T. , Harris, G.C. , Pinder, S.E. , Snead, D.R. , Carter, G.I. , Bell, J.A. , Haines, A. , Kollias, J. , Robertson, J.F. , Elston, C.W. , 2004. Identification of carcinoma cells in peripheral blood samples of patients with advanced breast carcinoma using RT-PCR amplification of CK7 and MUC1. Breast. 13, 35–41. [DOI] [PubMed] [Google Scholar]
- Xenidis, N. , Perraki, M. , Kafousi, M. , Apostolaki, S. , Bolonaki, I. , Stathopoulou, A. , Kalbakis, K. , Androulakis, N. , Kouroussis, C. , Pallis, T. , 2006. Predictive and prognostic value of peripheral blood cytokeratin-19 mRNA-positive cells detected by real-time polymerase chain reaction in node-negative breast cancer patients. J. Clin. Oncol.. 24, 3756–3762. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data


