Abstract
Existing research that studies individual health behaviors and conceive of behaviors as simplistically reflecting narrow intentions toward health may obscure the social organization of health behaviors. Instead, we examine how eight health behaviors group together to form distinct health behavior niches. Using nationally-representative data from U.S. adults aged 18 and over from the 2004–2009 National Health Interview Survey (NHIS), we use Latent Class Analysis to identify classes of behavior based on smoking status, alcohol use, physical activity, physician visits, and flu vaccination. We identify 7 distinct health behavior classes including concordant health promoting (44%), concordant health compromising (26%), and discordant classes (30%). We find significant race/ethnic, sex, regional, and age differences in class membership. We show that health behavior classes are associated with prospective mortality, suggesting that they are valid representations of health lifestyles. We discuss the implications of our results for sociological theories of health behaviors, as well as for multiple behavior interventions seeking to improve population health.
Keywords: Health behaviors, Health lifestyle, Mortality, Latent class analysis, United States
Highlights
-
•
We document 7 distinct health lifestyle typologies comprised of 8 health behaviors.
-
•
Health behavior classes included both concordant and discordant behaviors.
-
•
We find significant membership patterns by race, sex, region, and age.
-
•
Health behavior classes have valid relationships with all-cause mortality.
1. Introduction
Unhealthy behaviors are implicated in up to 40% of premature deaths in the U.S. (Mokdad, Marks, Stroup, & Gerberding, 2004) and contribute to persistent disparities in health (U.S. Department of Health and Human Services, 2015). But public health and behavioral research routinely focuses on single behaviors or small subsets of behaviors with shared functional meanings (e.g., both drinking and smoking to alleviate stress). Health lifestyle theories suggest that focusing on single behaviors or small subsets of either risky or low-risk behaviors offer limited insight into the organization of meaningful health behavior patterns that reflect broader social forces (Frohlich, Corin, & Potvin, 2001). From an applied standpoint, interventions that target single behaviors may do little to create enduring changes in broader health behavior patterns or in related health outcomes (Spring, Moller, & Coons, 2011). Indeed, the Institute of Medicine (2001) suggests the need for models and interventions that consider multiple behaviors simultaneously, as a strategy for creating larger and more enduring behavioral changes.
We advance existing research by drawing on health lifestyle theories that link broad patterns of health behaviors to social conditions, and using nationally representative data on diverse health behaviors among U.S. adults to identify typologies of health-related behavior that encompass both healthy and unhealthy behaviors. A detailed description of major health behavior typologies among U.S. adults is a necessary first step in addressing disease prevention and health promotion. In addition, we examine how health behavior typologies are associated with sociodemographic characteristics (i.e., age, race/ethnicity, sex, and region) and test a link with prospective mortality as a measure of the predictive criterion validity of including both healthy and unhealthy behaviors in typologies.
1.1. Health lifestyles
Health lifestyles are broad and potentially unobservable orientations that organize patterns of behaviors that derive from knowledge and norms about what constitutes healthy, stress relieving, or pleasurable behaviors (Bourdieu, 1984, Cockerham, 2005). Health lifestyle perspectives emphasize that individual choices about health behaviors are influenced by the social, cultural, and economic forces that frame and constrain individual choices (Bourdieu, 1984, Cockerham, 2000a). For example, cultural diffusion and cultural preferences (Pampel, 2005, Saint Onge and Krueger, 2011), racial and economic stratification (Harris, 2010, Krueger et al., 2011), and geopolitical forces (Cockerham et al., 2006, Krueger et al., 2009) have been linked to the organization of health behavior patterns. In contrast, frequently used behavioral theories such as the Health Belief Model or the Theory of Planned Behavior focus narrowly on individuals and offer little insight into how behaviors are shaped by broader social contexts (see Abel and Frohlich (2012) for further discussion). According to Bourdieu (1984:77), lifestyles are “most marked in the ordinary choices of everyday existence.” By emphasizing patterns of behaviors rather than single behaviors, we gain insight into the various ways that ordinary behaviors coalesce into meaningful patterns, and how those patterns reflect behavioral niches that are structured by social positions including age, race/ethnicity, sex, and geographic region.
Our first aim is to examine how individuals practice distinctive “health lifestyles” as indicated by meaningful typologies in a diverse array of health behaviors. We advance prior research in three ways. First, we consider health behaviors from multiple domains, including what are traditionally considered “lifestyle” variables (e.g., smoking, drinking, exercise), as well as preventive health care behaviors (e.g., influenza vaccinations, receipt of dental care, eye exams). Prior research on health behavior patterns generally focuses on behaviors in narrow domains (e.g., the combination of drinking and smoking), and sometimes conflates behaviors with the antecedents or outcomes of those behaviors (e.g., including mental distress along with measures of drinking and smoking). By including behaviors from multiple domains, we present a more comprehensive picture of health behaviors among U.S. adults.
Second, we consider behaviors that reflect diverse intentions toward health. Much public health and even sociological research implies that, ceteris paribus, people treat the pursuit of health and the enactment of healthy behaviors as though they should be the most important objective for all individuals (Frohlich, Corin, & Potvin, 2001). In contrast, health lifestyle theories recognize that individuals cultivate diverse motivations—including seeking pleasure, managing time for work and family obligations, alleviating stress, and expressing age, gender, socioeconomic, regional, and race/ethnic identities —that can compete with motives to pursue health (Jackson et al., 2010, Pampel, 2012, Saint Onge and Krueger, 2011). Although some behaviors are likely undertaken with health “in mind” (e.g., influenza vaccinations, doctor visits), other behaviors are routinely undertaken or avoided for non-health related reasons (e.g., exercise, alcohol consumption, sleep duration).
Because we consider health behaviors from multiple domains that have diverse implications for health, and that reflect diverse intentions toward health, we expect to identify some health behavior typologies that are “discordant” and that include some combination of both healthy and unhealthy behaviors. In contrast, public health research often imposes a “concordant” structure on health behaviors (i.e., where behavior patterns are uniformly healthy or unhealthy), by using additive scales to count the number of health recommendations or risk criteria (Coups et al., 2004, de Vries et al., 2008, Fine et al., 2004). Limited research has documented that between 10% and 20% of adults fall into discordant health behavior patterns (Patterson et al., 1994, Pronk et al., 2004), with little to no discussion of these discordant patterns. Fine and colleagues (2004) results show that 11.5% of their nationally-representative sample fall into discordant categories including drinkers who are physically active, smokers and drinkers who are physically active, and overweight or obese drinkers who are physically active. Further, 19% of a different sample fall into discordant categories, with only 16.5% of the total sample either meeting all or none of the healthy recommendation guidelines (Pronk et al., 2004). Studies that fail to consider health behaviors from multiple domains that reflect diverse intentions toward health, may underestimate the prevalence of discordant health behavior patterns in the U.S. Understanding the distribution and correlates of discordant health behavior patterns provides insight into the origins of those patterns and suggest how multiple-behavior interventions might be tailored to specific groups.
Third, we consider the criterion validity of our health lifestyles, in terms of their associations with prospective mortality. We classify individuals based on broad patterns of health behaviors that capture multiple domains of health, imply diverse intentions toward health, and have established associations with mortality (e.g., smoking, heavy drinking), promote early detection of potential health problems (e.g., visits to dentists or eye exams), or prevent future morbidity or mortality (e.g., influenza vaccinations, exercise). Thus, we expect our health lifestyle measure to have emergent properties that may reflect attitudes, behaviors, or tastes that are correlated with patterns among our observed items and that may be associated with the risk of death, even though they are unmeasured in our data. That is, our health lifestyles should remain associated with mortality, even after adjusting for the specific items used to identify our health lifestyle typologies. If our expectation is correct, then our findings will extend prior research that shows that multiple risky health behaviors are negatively related with mortality (Kvaavik et al., 2010, Saint Onge et al., 2014), and combinations of low-risk behaviors reduce the likelihood of death (Khaw et al., 2008, Spencer et al., 2005, Ford et al., 2011).
Our second aim is to examine how these meaningful health behavior typologies vary across sociodemographic factors including race/ethnicity, age, gender, and geographic region. Those sociodemographic factors reflect structural positions that shape the practice of health behaviors (Cockerham, 2005). Indeed, sociodemographic circumstances may define settings within which behavioral niches can develop and provide norms and resources that support specific types of health lifestyles.
We expect that health lifestyles typologies will be associated with sociodemographic factors. We remain agnostic about how specific behaviors will cluster with others, or how the resulting lifestyles will be associated with specific sociodemographic factors. But research that focuses on single behaviors suggests that we should expect to see disparities in health lifestyles by race/ethnicity, age, gender, and region. For example, although non-Hispanic blacks are slightly less likely than non-Hispanic whites to smoke and tend to smoke at lower levels (NCHS, 2013), they are more likely than whites to either binge drink or abstain, while whites are more likely to drink in moderation (Dawson, 1998). Compared to whites, Hispanics are less likely to be current frequent drinkers, but also have lower levels of physical activity and are less likely to receive regular medical exams (Schiller, Lucas, Ward, & Peregoy, 2012). Gender differences can be equally challenging. For instance, counts of low-risk behaviors do not show differences by gender (Ford et al., 2011), although examination of specific behaviors shows potential discordance, with women consistently drinking less than men, but also exercising less than men (NCHS, 2013).
While aging may coalesce behaviors into more static and potentially less-risky patterns (i.e., concordance), the social and biological process of aging may also influence discordant behaviors. Most adults who currently smoke began smoking in early adulthood, and alcohol consumption at older ages is related to drinking earlier in life (Bobo, Greek, Klepinger, & Herting, 2013). Biologically, exercise becomes more difficult with age as cardiovascular function and balance decline, and the prevalence of joint problems increases. The utilization of medical care may also increase with age as the prevalence of chronic conditions increases. But social factors are also important. Middle aged adults may have higher health care utilization than younger adults, because they are more likely to have jobs that provide high quality health care, have more health recommendations, or have access to health insurance through Medicare.
Regional variations and heterogeneity in health behaviors are substantial. The U.S. South is marked by increasing mortality rates among women over time, lower levels of physical activity, and elevated rates of chronic conditions including diabetes and stroke (Centers for Disease Control and Prevention, 2014, Kindig and Cheng, 2013). Regional differences in health behaviors partially result from socioeconomic factors (i.e., poverty, low education), but also result from cultural norms, structural limitations, and disparities in health care access. Yet, inconsistency in Southern disadvantage is also apparent—adults in the South are least likely to be current drinkers and are most likely to report lifetime abstention from alcohol consumption (Schoenborn, Adams, & Peregoy, 2013). In contrast, adults living in the West may indicate a different form of discordance – individual indicators suggest that they are more likely to sleep 7 to 8 h on average, less likely to be current smokers, and most likely to meet leisure-time physical activity guidelines than adults in other regions of the U.S. (Schoenborn, Adams, & Peregoy, 2013).
Research tends to focus on how high risk behaviors are clustered and most prevalent in more disadvantaged segments of the population, emphasizing how efforts to improve conditions will improve health behaviors across multiple domains. But rather than focusing on how risky populations (e.g., minority, elderly, Southerners, men) engage in risky or low-risk behaviors, we aim to understand how key sociodemographic factors are associated with patterns of behaviors that may be healthy, unhealthy, or neither.
2. Material and methods
Our data come from the 2004–2009 waves of the National Health Interview Survey (NHIS)-Sample Adult File (SAM). The NHIS is a large, nationally representative, cross-sectional survey that tracks the health of the non-institutionalized U.S. population, and has a response rate of 89% or higher for sampled households. The SAM is a supplemental file that collects detailed health and health behavior data on a randomly-sampled adult from each family in the NHIS. We draw the NHIS-SAM data from the Integrated Health Interview Series (IHIS) database, which collates the NHIS data and ensures the consistency of those data over multiple years (Minnesota Population Center, 2010).
We also use the NHIS-SAF files linked to mortality records through the end of 2009 that have been recorded in the National Death Index, the Social Security Administration, and the Centers for Medicare & Medicaid Services as provided in the NHIS public-use linked mortality files (NCHS, 2015). Due to missing information on the criteria that are used to match NHIS-SAF records to death records, 4.1% of records are considered ineligible to be linked to vital status. We follow the recommendations of staff at the National Center for Health Statistics and exclude those individuals from our survival analyses and use corrected weights to address their exclusion from our data (NCHS, 2015). Removing ineligible records (6621) for the mortality data analysis leaves an analytic sample of 152,500. This study was approved by the Institutional Review Board at the University of Kansas (#20786).
2.1. Variables
All data are self-reported by survey respondents. Health behaviors include cigarette smoking, alcohol use, physical activity, and sleep duration. We classify variables in ways that preserve meaningful variation in the data and that reflect differential associations with mortality in prior studies (Pampel, Krueger, & Denney, 2010). Cigarette smoking is measured categorically as never smoker (never smoked 100 cigarettes in lifetime), former smoker, current light smoker (0–14 cigarettes per day), current moderate smoker (15–24 cigarettes per day), and current heavy smoker (greater than 24 cigarettes per day). Alcohol consumption is assessed categorically as lifetime abstainer, former drinker (no drinks in past year), current moderate drinker (12+ drinks in past year but not current heavy drinker), or current heavy drinker (>14 drinks per week in past year for men; >7 drinks per week for women). Whereas moderate drinking may promote health, heavy drinking, non-drinking, and former drinking are generally considered a health compromising behavior (Dawson, 2011, Rogers et al., 2013). Sleep duration indicates the usual number of hours that respondents sleep each day and is categorized as less than 7 h, 7 to 8 h, and more than 8 h. High and low levels of sleep duration are associated with both poor health and premature mortality (Krueger et al., 2011, Singh et al., 2005).
Moderate leisure time physical activity is measured as the number of times per week that respondents participate in leisure time activities that result in light sweating or slight to moderate increases in breathing or heart rate for at least 10 min. Vigorous leisure time physical activity is measured as the number of times per week that respondents participate in leisure time activities that result in heavy sweating or large increases in breathing or heart rate for at least 10 min. Both moderate and vigorous activities are top-coded as 9 or more bouts per week, which represents less than 2% of the sample. Health guidelines emphasize the importance of addressing both moderate and vigorous activity (Haskell et al., 2007).
Flu vaccination, comprehensive eye exams, and regular dental care are each the focus of public health efforts aimed at primary and preventive care. Receipt of influenza vaccine (either as a shot or nasal spray) in the past year, receipt of preventive dental care in the past year, and receipt of preventive eye care (including visits to an optometrist, ophthalmologist, or other eye doctor) in the last year are all coded dichotomously. National public health goals aim to increase the current vaccination rates from approximately 30% of adults aged 18 to 64 years to 80%, with a goal of 90% vaccination for those over the age of 65 (U.S. Department of Health and Human Services, 2015). Eye exams are generally recommended every two years for low-risk, young adults and every one year for older adults with vision problems or risk factors with U.S. national objectives aiming to increase this proportion of comprehensive eye exams to 60.5% of the population (U.S. Department of Health and Human Services, 2015). Oral health is a leading public health indicator, serving as a potential screener of disease with established links between periodontal disease and chronic conditons (Garcia, Henshaw, & Krall, 2000).
Our sociodemographic variables include age, sex, race/ethnicity, and region of residence—distal factors that are linked to individual health behaviors, health conditions, and mortality, and that signal important disparities in the population. Age is measured as a continuous variable that ranges from 18 to 85 or older. We include a quadratic term for age in the best-fitting multivariate models to account for nonlinear associations between age and class membership. Sex is measured dichotomously with women as the reference category. We code race/ethnicity as non-Hispanic whites (referent), non-Hispanic blacks, Hispanics, and other race. The Census region of residence is coded categorically as Midwest (referent), Northeast, South, and West.
2.2. Latent class analysis (LCA)
We use latent class analysis (LCA) in Mplus software to predict membership in latent (i.e., unobserved) groups that share similar health behavior patterns. LCA is an inductive statistical technique that estimates the number and composition of health behavior classes (i.e., typologies) directly from the data. LCA is a model based procedure that uses information on the eight health behavior variables to probabilistically classify respondents such that the similarity of combinations of health behaviors within each class is maximized. See Table 1 for the distribution proportions of health behaviors for the analysis sample.
Table 1.
Proportions and means for Health Behaviors, Sociodemographic Variables, and Mortality, by Health Classes for U.S Adults Ages 18 and Over, 2004–2009 NHIS.
|
Health Behavior Classes |
||||||||
|---|---|---|---|---|---|---|---|---|
|
Overall |
1 |
2 |
3 |
4 |
5 |
6 |
7 |
|
| % | Concordant, Health Promoting | Concordant, Health Compromising | Discordant | |||||
| Health Behaviors | ||||||||
| Regular nightly hours of sleep | ||||||||
| <7 | 0.28 | 0.20 | 0.27 | 0.28 | 0.34 | 0.21 | 0.33 | 0.35 |
| 7–8 | 0.63 | 0.76 | 0.63 | 0.65 | 0.54 | 0.69 | 0.60 | 0.57 |
| 9+ | 0.09 | 0.04 | 0.10 | 0.06 | 0.12 | 0.09 | 0.07 | 0.07 |
| Alcohol consumption | ||||||||
| Abstainer | 0.23 | 0.13 | 0.21 | 0.19 | 0.09 | 0.81 | 0.12 | 0.14 |
| Former | 0.15 | 0.09 | 0.17 | 0.10 | 0.28 | 0.00 | 0.09 | 0.11 |
| Moderate drinker | 0.58 | 0.75 | 0.59 | 0.65 | 0.57 | 0.18 | 0.71 | 0.65 |
| Heavy drinker | 0.05 | 0.03 | 0.04 | 0.06 | 0.06 | 0.00 | 0.08 | 0.10 |
| Moderate physical activity per week (mean) | 2.78 | 5.22 | 4.92 | 0.00 | 0.00 | 0.00 | 2.63 | 6.92 |
| Vigorous activity per week (mean) | 1.81 | 4.30 | 0.00 | 4.61 | 0.00 | 0.00 | 2.30 | 5.70 |
| Smoking status | ||||||||
| Never | 0.58 | 0.68 | 0.56 | 0.62 | 0.33 | 1.00 | 0.57 | 0.52 |
| Former | 0.22 | 0.30 | 0.25 | 0.20 | 0.30 | 0.00 | 0.16 | 0.15 |
| Light (<14 cigs. / day) | 0.11 | 0.02 | 0.10 | 0.11 | 0.17 | 0.00 | 0.16 | 0.19 |
| Moderate (15–24 cigs. / day) | 0.07 | 0.00 | 0.07 | 0.05 | 0.15 | 0.00 | 0.09 | 0.11 |
| Heavy (25+ cigs. / day) | 0.02 | 0.00 | 0.02 | 0.02 | 0.05 | 0.00 | 0.03 | 0.03 |
| Dental exam in past year [yes] | 0.62 | 0.95 | 0.64 | 0.68 | 0.47 | 0.59 | 0.55 | 0.51 |
| Eye exam in past year [yes] | 0.37 | 0.64 | 0.42 | 0.35 | 0.36 | 0.24 | 0.24 | 0.19 |
| Flu vaccine in past year [yes] | 0.29 | 0.48 | 0.36 | 0.25 | 0.31 | 0.24 | 0.11 | 0.10 |
| Sociodemographic characteristics | ||||||||
| Age (Mean) | 45.76 | 45.06 | 49.87 | 40.11 | 49.72 | 46.13 | 37.73 | 38.05 |
| Age Categories | ||||||||
| 18–24 | 0.13 | 0.12 | 0.09 | 0.20 | 0.08 | 0.16 | 0.18 | 0.20 |
| 25–34 | 0.18 | 0.17 | 0.14 | 0.22 | 0.15 | 0.18 | 0.27 | 0.26 |
| 35–64 | 0.53 | 0.58 | 0.55 | 0.49 | 0.55 | 0.46 | 0.51 | 0.50 |
| ≥65 | 0.16 | 0.13 | 0.22 | 0.08 | 0.22 | 0.21 | 0.03 | 0.04 |
| Sex | ||||||||
| Men | 0.48 | 0.48 | 0.40 | 0.59 | 0.53 | 0.33 | 0.60 | 0.57 |
| Race/ethnicity | ||||||||
| Non-Hispanic White | 0.69 | 0.81 | 0.73 | 0.65 | 0.69 | 0.51 | 0.73 | 0.74 |
| Non-Hispanic Black | 0.11 | 0.07 | 0.09 | 0.13 | 0.13 | 0.17 | 0.10 | 0.10 |
| Hispanic | 0.13 | 0.07 | 0.11 | 0.15 | 0.13 | 0.22 | 0.10 | 0.10 |
| Other race | 0.06 | 0.06 | 0.07 | 0.08 | 0.05 | 0.09 | 0.07 | 0.06 |
| Region | ||||||||
| Northeast | 0.18 | 0.19 | 0.18 | 0.20 | 0.18 | 0.16 | 0.15 | 0.16 |
| North Central/Midwest | 0.24 | 0.27 | 0.25 | 0.23 | 0.23 | 0.19 | 0.30 | 0.26 |
| South | 0.36 | 0.31 | 0.33 | 0.34 | 0.41 | 0.44 | 0.33 | 0.35 |
| West | 0.22 | 0.24 | 0.23 | 0.23 | 0.18 | 0.21 | 0.22 | 0.23 |
| Mortality | ||||||||
| Deaths by year 2011 | 0.05 | 0.02 | 0.05 | 0.01 | 0.09 | 0.06 | 0.01 | 0.02 |
| Age at death (mean) | 72.38 | 70.76 | 73.78 | 64.92 | 72.82 | 75.73 | 58.05 | 58.03 |
| % of total | 100.00 | 14.13 | 22.18 | 8.59 | 25.1 | 12.41 | 6.66 | 10.93 |
| unweighted n | 152,500 | 19,615 | 34,463 | 12,469 | 40,113 | 20,966 | 9,307 | 15,567 |
All values include sample weights and adjust for complex survey design
We sought to accurately describe the distribution of health behavior typologies among U.S. adults without over-specifying the number of classes or sacrificing interpretive value. Because the “true” number and composition of health behavior typologies in the population is unknown, we estimated models that allowed for between one and fifteen classes and compared the models with various model fit statistics. To arrive at the best number of classes, we balanced the practical usefulness of our results against quantitative measures of model fit (Munthen, 2003).
Appendix A summarizes the quantitative measures of model fit for models with one through 10 classes. Smaller values of the Akaiki Information Criterion (AIC), Bayesian Information Criterion (BIC) and Sample Adjusted Bayesian Information Criterion (SBIC) indicate improved model fit (Vermunt & Magidson, 2004). Ancillary model criterion also included examination of the Lo-Mendell-Rubin likelihood ratio test. The included goodness of fit measures are comparative measures of log-likelihood that integrate number of model parameters (AIC) and number of observations (BIC and SBIC). The AIC, BIC, and SBIC decline rapidly until reaching the seven-class model, and then fall more slowly with the inclusion of each additional class. Entropy can range from 0 to 1, with higher values indicating higher certainty that individuals belong in their assigned classes (Muthén & Muthén, 2007). In our case, the entropy is relatively uninformative with similar values for the 4 to 10 class models.
We evaluated the practical usefulness of our results in two ways. First, we gave preference to models that identify as many unique classes as possible, without identifying substantively similar but smaller classes. For example, moving from the 6 class to 7 class model resulted in the identification of a new class that is qualitatively unlike any of those estimated from the 6 class model. Second, we gave preference to models that identified classes that included meaningful numbers of people, both because we wanted to find the most common health lifestyle patterns among U.S. adults and because LCA models are prone to over-fitting (finding trivial and meaningless patterns) in large data. Models that identified 8 or more classes found smaller, less distinct, and less interpretable classes (see Appendix A). For example, moving from a seven-class to an eight-class model primarily split Class 3 into similar, smaller categories where one included slightly more non-smokers. Ancillary analyses indicated nearly identical risks of mortality for these two classes. Taken together, our fit statistics and practical criteria suggest the 7 class model solution as the most parsimonious and substantively sound. Individuals were assigned to classes based on estimated posterior class probabilities with an overall average latent class probability of 0.81 (standard deviation; sd 0.15), ranging from a low mean probability of 0.71 (sd 0.17) for Class 1 to a high mean probability of 0.92 (sd 0.09) for membership in Class 3.
2.3. Predicting class membership
We use multinomial logistic regression models (Long, 1997), to examine the association between age, sex, race/ethnicity, and region of residence and membership in classes (Class 2 as the reference category) that mark distinct health behavior patterns. To simplify our presentation of the results, we present predicted probabilities across values of our predictor variables. The regression coefficients are exponentiated and presented as relative risk ratios (RRR) in Appendix B. All models incorporate sample weights and correct the standard errors for the complex sampling frame employed by the NHIS.
2.4. Mortality analyses
We use Cox proportional hazard models to examine the association between health behavior typologies and the risk of all-cause mortality. Test of the proportional-hazards assumption assured appropriate model specification. We use age as the time-to-event, because age is the fundamental driver of mortality rates (Korn, Graubard, & Midthune, 1997).
3. Results
The first column of Table 1 presents means and proportions for all study variables. Adults in our sample typically sleep 7 to 8 h, are current drinkers, and have about 3 bouts of moderate physical activity and 2 bouts of vigorous physical activity in the last week. Nearly 60% of adults in our sample never smoke, but almost 20% are light, moderate, or heavy smokers. In the past year, over 60% of our sample had a dental visit, 37% had an eye exam, and 29% received a flu vaccine.
3.1. Health behavior classes
The remaining columns of Table 1 show the distribution of variables across classes. The first three classes represent concordant health promoting classes that jointly account for 44% of the population. Class 1 is marked by a relatively higher share of adults who sleep 7–8 h than in the general population, high levels of current moderate drinking but low levels of heavy drinking, high levels of moderate and vigorous activity, below average levels of current smoking, and above average levels of receipt of dental care, eye care, or influenza vaccine.
Classes 2 and 3 are generally concordant, health promoting behavior typologies that differ in terms of physical activity. Class 2 is marked by high levels of moderate activity and low levels of vigorous activity, and Class 3 is marked by low levels of moderate activity and high levels of vigorous activity. Both classes mirror the population in terms of the distribution of sleep duration and dental exams. Class 2 has somewhat higher levels of eye exams and influenza vaccinations than the population average. Class 2 has a distribution of alcohol use that mirrors the population averages, whereas Class 3 is marked by somewhat lower levels of abstaining and former drinking, and higher levels of moderate drinking than the population. Both classes 2 and 3 exhibit a distribution of smoking behaviors similar to the population average.
Class 4 is marked by concordant but health compromising behaviors, and accounts for about 25% of the population. Class 4 is marked by disproportionately high levels of both short and long sleep duration, no moderate or vigorous activity, and the highest levels of heavy smoking of any of the classes identified. Moreover, Class 4 is also marked by relatively high levels of former drinking (which, in the context of the other behaviors, may indicate a history of problem drinking), and the lowest levels of dental exams.
Classes 5, 6, and 7 are discordant and comprise 12.4%, 6.7% and 10.9% of the population, respectively. Class 5 is characterized by an over-representation of sleep durations of 7–8 h, and relatively few adults who sleep less than 7-h, compared to the population average. Class 5 is also marked by very high levels of abstaining from alcohol consumption and virtually universal non-smoking, but also the absence of vigorous or moderate physical activity, and low levels of optometry visits.
Class 6 is marked by a modest over-representation of adults who sleep less than 7 h, and a modest under-representation of adults who sleep 7–8 h, compared to the population average. Class 6 is also characterized by relatively high levels of moderate drinking, vigorous activity, and light or moderate smoking levels, but reduced levels of dental exams, eye exams, and influenza vaccination. Class 7 includes the largest share of adults who sleep less than 7 h. Moreover, Class 7 is marked by high levels of moderate and heavy drinking, high levels of light and moderate smoking, and low levels of receipt of dental exams, eye exams, and influenza vaccination, compared to the average population. Despite being characterized by so many unhealthy behaviors, adults in Class 7 also have among the highest levels of moderate and vigorous physical activity of any of the classes examined.
3.2. Demographic characteristics and class membership
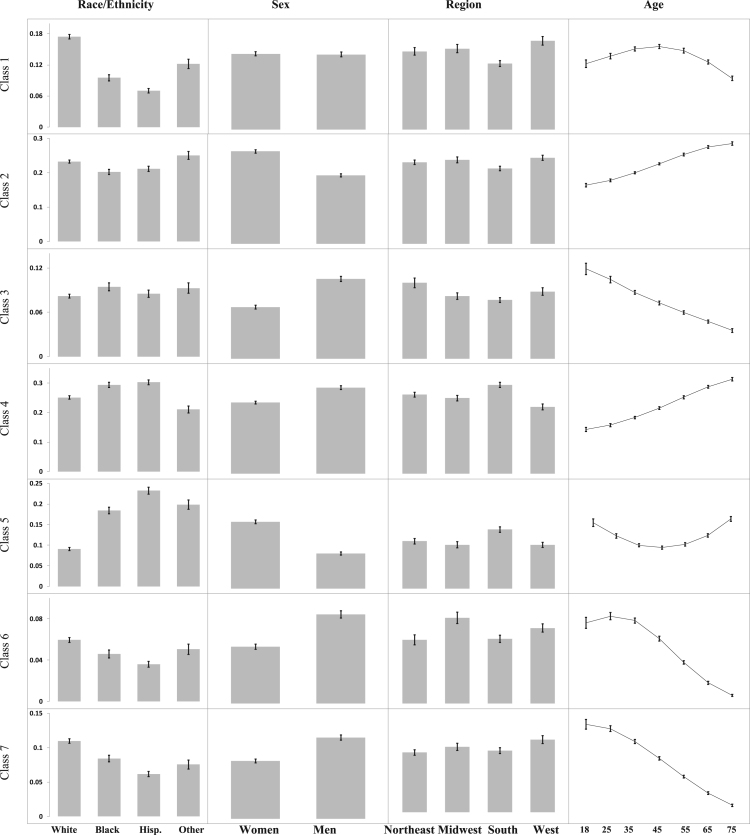
Fig. 1 presents the predicted probabilities of class membership by race/ethnicity, sex, region, and age (Appendix B shows the multinomial logistic regression model from which these estimates are derived, with Class 2 serving as the reference category). The vertical scale is the same within each row to permit comparisons of the magnitude of each sociodemographic variable within a given class. However, we allow the vertical scale to differ across rows. Otherwise, differences in the proportion of people in each class would overwhelm sociodemographic differences within classes, thereby obscuring disparities.
Fig. 1.
Adjusted Predicted Probabilites of Sociodemographic Categories on Class Membership. Predicted probabilities and 95% confidence intervals from multinomial logistic regression including race/ethnicity, sex, region, age, and age2. *Note: Vertical axis scales vary by row.
Classes 1 through 3 are marked by concordant, health promoting behaviors. Class 1 exhibited elevated levels of all healthy behaviors and reduced levels of all unhealthy behaviors. The probability of membership in Class 1 is higher among whites than blacks or Hispanics, is higher among those who live in the West than the South, and is higher in midlife than among younger or older adults. Men and women have similar probabilities of membership in Class 1. Classes 2 and 3 were also concordant, health promoting classes, where Class 2 exhibited high levels of moderate physical activity, and Class 3 exhibited high levels of vigorous physical activity. The probability of belonging to Class 2 is relatively similar across race/ethnic groups and by geographic region. However, women and older adults have a higher probability of belonging to Class 2 than men or younger adults, respectively. In contrast, the probability of membership in Class 3 is higher among men than among women, and declines with age. Blacks and Northeasterners have a somewhat higher probability of belonging to Class 3 than whites or residents of other regions, respectively.
Class 4 is marked by concordant but heath compromising behaviors. The probability of membership in Class 4 is higher among Hispanics and blacks than among whites, and is higher among men than among women. Further, the probability of belonging to Class 4 is highest among those who live in the South and lowest among those who live in the West, with intermediate probabilities among residents of the Northeast and Midwest. The probability of membership in Class 4 increases steadily with age.
Classes 5 through 7 are discordant, and include some combination of health promoting and health compromising behaviors. Class 5 includes low levels of physical activity, smoking, and alcohol use, but also low levels of preventive health care utilization. The probability of belonging to Class 5 is substantially higher among Hispanics than among whites, with blacks falling in the middle. Women and Southerners have a higher probability of belonging to Class 5 than men or residents of other areas. The probability of belonging to Class 5 is highest for young and old adults, and lowest for middle-aged adults.
Class 6 and 7 are both marked by elevated levels of alcohol consumption and smoking, reduced levels of preventive health care utilization. Class 6 exhibits modest levels of vigorous activity, whereas Class 7 exhibits higher levels of both moderate and vigorous physical activity. Despite these differences, they exhibit similar socioedemographic differences. The probability of membership in Classes 6 or 7 is higher among whites and men than among blacks, Hispanics, or women, respectively. Compared to residents of other regions, the probability of membership in Class 6 is somewhat higher among Midwesterners, and the probability of membership in Class 7 is somewhat higher among Westerners. The probability of membership on both classes declines by age.
3.3. Class membership and survival
The average age of death in the sample was 72.4 years of age, with differences in mean age of death by each health behavior typology. Notably, Class 6 and 7 each have lower average age of death, indicative of the younger age composition of these groups. Table 2 examines whether the health behavior typologies are valid predictors of subsequent mortality. Model 1 shows age-adjusted associations between health behavior types and all-cause mortality. Compared to those in Class 2, adults in Class 1 and 3 have 39% lower risks of death, which is similar to a meta-analysis that found a relative risk of 0.34 for three healthy factors (Loef & Walach, 2012). While each of these typologies are similar in terms of behaviors, Class 2 has lower levels of non-smokers, which may explain part of these differences. Model 1 also shows that Classes 4–6 have elevated risks of death. Model 2 further adjusts for the demographic variables and finds that they do little to explain the association between health behavior typologies and mortality. Finally, Model 3 further adjusts for each of the individual health behaviors—the health behavior typologies identified in our analyses have emergent properties and remained associated with mortality even when adjusting for the health behavior items that comprise those classes.
Table 2.
Cox Proportional Hazard Ratios (95% Confidence Intervals) for the Relationships among Sociodemographic factors, Health Behavior Classes, Health Behaviors, and the Risk of All-Cause Mortality, U.S. Adults 18 Years and Older, 2004–2009.
|
1 |
2 |
3 |
||||
|---|---|---|---|---|---|---|
| (Class only model) | (+ sociodemographice) | (+ health behaviorse,f) | ||||
| Class (Referent: Class 2) | ||||||
| Class 1 | 0.61 | *** | 0.59 | *** | 0.64 | *** |
| (0.53 - 0.68) | (0.52 - 0.67) | (0.52 - 0.78) | ||||
| Class 3 | 0.61 | *** | 0.58 | *** | 0.74 | * |
| (0.51 - 0.71) | (0.49 - 0.68) | (0.56 - 0.96) | ||||
| Class 4 | 1.79 | *** | 1.72 | *** | 1.65 | *** |
| (1.68 - 1.91) | (1.61 - 1.84) | (1.43 - 1.91) | ||||
| Class 5 | 1.12 | ** | 1.20 | *** | 1.63 | *** |
| (1.03 - 1.22) | (1.10 - 1.30) | (1.37 - 1.93) | ||||
| Class 6 | 0.78 | * | 0.73 | ** | 0.73 | * |
| (0.63 - 0.97) | (0.59 - 0.90) | (0.57 - 0.95) | ||||
| Class 7 | 0.94 | 0.88 | † | 0.77 | * | |
| (0.80 - 1.09) | (0.75 - 1.02) | (0.61 - 0.97) | ||||
| n | 151,847 | 151,689 | 129,432 | |||
| χ2 (df) | 684.5 (6) | 1064.2 (13) | 17,076.8 (27) |
No. of deaths: 7, 980.
p<0.001.
p<0.01.
p<0.05.
p<0.10.
Sociodemographic (sex, race/ethnicity, region).
Health behaviors: (hours of sleep, alcohol status, moderate activity, vigorous activity, smoking status, dental visits, optometry visits, flu vaccine).
4. Discussion
We use eight health behaviors to identify seven distinct health behavior typologies in a nationally representative sample of U.S. adults. We use health behaviors that have established associations with mortality and morbidity, and that have diverse functional meanings (Cockerham, 2000b). By including both health promoting and health compromising behaviors, our health behavior typologies can distinguish among those who actively pursue health and those who simply avoid unhealthy behaviors. We also highlight the predictive validity of including typologies over individual-level behaviors and show how key sociodemographic characteristics are associated with these meaningful health behavior typologies.
We advance prior research by using inductive latent class analysis methods to identify concordant health promoting, concordant health compromising, and discordant health behavior typologies in our data. Three concordant health behavior typologies jointly include about 44% of the population and are marked by consistently health promoting behaviors. An additional concordant typology is marked by uniformly unhealthy behaviors and accounts for 26% of the population. The remaining 30% of the population falls into one of three discordant typologies marked by some combination of health promoting and health compromising behaviors.
There are three major implications of our analyses. First, we identify diverse classes of behavior that are associated with prospective mortality. Additive scales of healthy/unhealthy behaviors may be useful summary scales for understanding broad patterns of investment (or disinvestment) in health, but they have limited value for identifying points of intervention to be maintained indefinitely (Spring, Moller, & Coons, 2012). Behavior interventions that target broadly unhealthy behavior patterns—as opposed to single behaviors—might benefit from identifying sustainable health promoting behavior patterns as destinations for subjects of those interventions.
To illustrate, Class 4 is concordant and health compromising with an elevated risk of death, wherein individuals are unlikely to sleep 7–8 h, to be never smokers, to receive preventive health care, or to undertake any physical activity, although they are relatively likely to be former or current smokers. Interventions that seek to promote physical activity may be unlikely to succeed if those individuals are limited by smoking, lack energy due to their short sleep hours, or suffer lasting effects of alcohol. Further, the low levels of participation in preventive behaviors may indicate a lack of interest in other forms of health promotion or the presence of social or economic barriers to health promotion. Interventions that seek to promote a more holistic set of behavior changes may pose greater challenges, but might be more likely to persist over time (Institute of Medicine, 2001).
The second implication of our analyses suggests the importance of sociodemographic and structural characteristics, in shaping “behavioral niches” that individuals inhabit and that may shape the organization of health lifestyles. Individual dispositions appear to be grounded in a collective framework that goes beyond individual responsibility. Health behaviors are not simply individual choices, but instead relate directly to important structural contexts that can affect opportunities for sets of behaviors suggesting the importance of considering theoretical models of health lifestyles when designing models of health behavior intervention (Abel & Frohlich, 2012).
For example, Class 7 includes discordant health behaviors that suggests a “work hard, play hard” lifestyle marked by very high levels of moderate and vigorous physical activity, as well as relatively short sleep hours, high levels of moderate and heavy alcohol consumption, relatively high levels of light and moderate smoking, and low levels of preventive health behaviors. The probability of membership in Class 7 is highest among young, white men who live in the Western U.S. Younger men may use smoking or drinking to facilitate social interactions, yet they may not have been smokers or drinkers long enough to experience the deleterious consequences of those behaviors, as evidenced in the mortality results. But, this relationship with mortality may be different for older individuals who remain in this behavioral pattern.
In contrast, Class 5 includes discordant health behaviors that suggests a “do nothing” lifestyle marked by abstaining from both alcohol consumption and smoking, but also relatively low levels of physical activity and preventive health behaviors. Members of Class 5 appear to do very little to promote good health, but also do very few actively health compromising behaviors. Members of Class 5 are relatively likely to be Hispanic or black rather than white, to be women rather than men, to live in the South rather than other regions, and to be young or old rather than middle-aged. The South offers relatively few opportunities to pursue better health (Krueger, Bhaloo, & Rosenau, 2009), and what few opportunities are available may be difficult for racial/ethnic minorities, women, and young or old adults to utilize.
The third implication of our analyses is that compliance with preventive health behaviors (i.e., influenza vaccinations, eye exams, dental exams) might best be understood in the context of broader sets of health behaviors that may not always be undertaken with health “in mind” For example, Class 1 is the most consistently health promoting (lowest risk of mortality) as observed in our data, and the preventive health care utilization behaviors fit in consistently with the other behaviors.
Classes 6 and 7, on the other hand, are discordant typologies. Consistent with existing analyses of single behaviors (American Lung Association, 2001, National Center for Health Statistics, 2013), both classes are disproportionately represented among young white men, for whom high levels of physical activity appears to “contradict” a broader pattern of somewhat unhealthy behaviors. In a sense, these discordant behaviors suggest that engaging in high levels of healthy behaviors may lead to overconfidence that limit other areas of health-oriented action. For example, a strong cultural emphasis on personal responsibility may lead members of these groups to focus less on primary prevention or influence their decisions to carry health insurance (Cantiello, Fottler, Oetjen, & Zhang, 2015).
4.1. Strengths and limitations
A major strength of our research is our focus on multiple health related behaviors, from multiple domains, in a large, population-based sample. Further, we use inductive LCA methods to identify qualitatively distinct health behavior classes, rather than focusing on narrower linear associations among variables (Berrigan et al., 2003, Reeves and Rafferty, 2005). In doing so, we can empirically identify subgroups who share distinct health behavior typologies predictive of mortality, without making strong a priori assumptions about how behaviors are related and theoretically consider the importance of collective health lifestyles.
Several limitations of our analyses warrant mention. First, our baseline health behavior data are cross-sectional and cannot parse age and cohort changes in health behavior typologies. While we are unable to determine if groups “age-out” of certain classes, health behaviors often begin early in life and set the stage for later life behaviors, and we find that the typologies remain important across age groups. Indeed, while the typologies comprised of younger individuals (e.g., Class 6 and Class 7) are more weakly associated with mortality (perhaps because health lifestyles may shift throughout early adulthood), we continue to find robust relationships thereby setting the stage for future, longitudinal research focused on age and health lifestyles.
Second, we lack information about key behaviors such as diet, illicit substance use, or other behaviors that may also have diverse implications for health. Indeed, we are limited by the institutional a priori assumptions of a national data collection that determines the most “important” health behaviors to be monitored and we are unable to capture the full breath of “real” health lifestyles within a population. For instance, a Latent Class Analysis of college students in the U.S. showed a similar pattern of behaviors to Class 7, but also included drunk driving, poor stress management, and intoxicated sex, for males (Laska, Pasch, Lust, Story, & Ehlinger, 2009). Additional behavior variables would potentially allow for more complete insight into the social structuring of health behavior patterns.
Finally, our research offers little insight into the constellations of meanings. By focusing on stable demographic factors, we highlight how social structure may translate into everyday practices that may legitimate social inequalities (Bourdieu, 1977), but are unable to understand why people engage in these typologies. Further work needs to move beyond demographic factors to consider how dynamic structural factors such as living conditions, family relationships, health care access, and support networks, influence opportunities or motivations to undertake behaviors. Also, while more proximate factors such as education, income, or employment also have major implications for health behavior typologies and established “practices” (Mollborn et al., 2014, Skalamera and Hummer, 2016, Christensen and Carpiano, 2014), the unique relationships, selection issues, and theoretical explanations are beyond the scope of this analysis and require a focused exploration (see Mirowsky & Ross, 2015).
5. Conclusions
Our results suggest that individual behaviors tend to group together by health behavior typologies into meaningful health lifestyles that are anchored in social circumstances (Cockerham, 2005). We find that health behaviors conceptually and empirically lend themselves to theories of symbolic distinction (Christensen and Carpiano, 2014, Pampel, 2012, Saint Onge and Krueger, 2011). Indeed, individuals do not appear to undertake one behavior independently of whether they undertake other behaviors. Research that focuses on single health behaviors—detached from social context—can at best provide narrow insights into the practice of health in the U.S. Our findings also bolster research that suggests that multiple behavior interventions aimed at behavioral niches may be fruitful for creating cost -effective and enduring changes in health behaviors, but also for targeting disparities that are linked to distinct health behavior typologies (Orleans, 2004). A renewed focus on the social contexts that shape health behavior typologies may help to counter the preponderance of interventions that focus on individuals and individual behaviors, and that treat health behaviors as somehow detached from broadly meaningful behavior patterns.
Acknowledgements
Research reported in this publication was supported by the National Institute On Aging of the National Institutes of Health under Award number R03AG033331. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix A
See Appendix Table A1.
Table A1.
Fit Statistics for LCA Models with 1 through 10 Classes.
| Number of classes: | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| AIC | 3,217,801 | 3,118,674 | 3,074,641 | 3,066,825 | 3,032,764 | 3,028,037 | 3,014,272 | 3,009,949 | 3,010,067 | 3,007,668 |
| BIC | 3,217,963 | 3,118,989 | 3,075,108 | 3,067,443 | 3,033,534 | 3,028,959 | 3,015,346 | 3,011,175 | 3,011,445 | 3,009,198 |
| Sample Adjusted BIC | 3,217,912 | 3,118,890 | 3,074,961 | 3,067,249 | 3,033,293 | 3,028,670 | 3,015,009 | 3,010,791 | 3,011,013 | 3,008,718 |
| Entropy | n/a | 0.89 | 0.88 | 0.76 | 0.83 | 0.82 | 0.78 | 0.77 | 0.80 | 0.77 |
| Percent in smallest class | 100 | 38.5 | 22.5 | 14.4 | 8.3 | 8.3 | 6.1 | 3.7 | 5.2 | 1.6 |
| Number of parameters | 16 | 31 | 46 | 61 | 76 | 91 | 106 | 121 | 136 | 151 |
Appendix B
See Appendix Table B1.
Table B1.
Multinomial Logistic Regression.
| Referent (Class 2) | 1 | 3 | 4 | 5 | 6 | 7 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 1.01 | ** | 0.96 | *** | 0.99 | * | 0.92 | *** | 1.04 | *** | 1.00 | |
| (1.00 - 1.02) | (0.96 - 0.97) | (0.99 - 1.00) | (0.91 - 0.93) | (1.02 - 1.05) | (0.99 - 1.00) | |||||||
| Age * Age | 1.00 | *** | 1.000 | 1.00 | *** | 1.00 | *** | 1.00 | *** | 1.00 | *** | |
| (1.00 - 1.00) | (1.00 - 1.00) | (1.00 - 1.00) | (1.00 - 1.00) | (1.00 - 1.00) | (1.00 - 1.00) | |||||||
| Sex (Referent: Women) | ||||||||||||
| Men | 1.34 | *** | 2.09 | *** | 1.63 | *** | 0.71 | *** | 2.12 | *** | 1.90 | *** |
| (1.28 - 1.40) | (1.98 - 2.21) | (1.58 - 1.69) | (0.68 - 0.75) | (2.00 - 2.24) | (1.81 - 2.00) | |||||||
| Race/ethnicity (Referent: Non-Hispanic White) | ||||||||||||
| Non-Hispanic Black | 0.63 | *** | 1.33 | *** | 1.35 | *** | 2.33 | *** | 0.89 | * | 0.88 | *** |
| (0.58 - 0.68) | (1.23 - 1.44) | (1.27 - 1.43) | (2.18 - 2.51) | (0.80 - 0.99) | (0.82 - 0.95) | |||||||
| Hispanic | 0.44 | *** | 1.15 | ** | 1.33 | *** | 2.82 | *** | 0.67 | *** | 0.62 | *** |
| (0.41 - 0.48) | (1.06 - 1.24) | (1.25 - 1.41) | (2.62 - 3.03) | (0.61 - 0.73) | (0.57 - 0.67) | |||||||
| Other race | 0.65 | *** | 1.053 | 0.78 | *** | 2.03 | *** | 0.79 | *** | 0.64 | *** | |
| (0.59 - 0.72) | (0.95 - 1.16) | (0.71 - 0.85) | (1.85 - 2.23) | (0.70 - 0.89) | (0.58 - 0.71) | |||||||
| Region (Referent: Northcentral/midwest) | ||||||||||||
| Northeast | 1.00 | 1.25 | *** | 1.08 | * | 1.12 | † | 0.77 | *** | 0.94 | ||
| (0.93 - 1.08) | (1.13 - 1.39) | (1.00 - 1.16) | (1.00 - 1.25) | (0.69 - 0.86) | (0.86 - 1.03) | |||||||
| South | 0.91 | * | 1.05 | 1.31 | *** | 1.50 | *** | 0.84 | *** | 1.05 | ||
| (0.84 - 0.99) | (0.96 - 1.14) | (1.21 - 1.41) | (1.35 - 1.67) | (0.76 - 0.93) | (0.98 - 1.15) | |||||||
| West | 1.10 | 1.05 | 0.85 | *** | 0.98 | 0.86 | ** | 1.08 | ||||
| (0.97 - 1.17) | (0.95 - 1.16) | (0.80 - 0.94) | (0.87 - 1.09) | (0.78 - 0.95) | (0.98 - 1.20) | |||||||
| Constant | 0.82 | † | 1.12 | 0.90 | 2.82 | *** | 0.40 | *** | 1.23 | * | ||
| (0.67 - 1.01) | (0.90 - 1.40) | (0.77 - 1.04) | (2.32 - 3.42) | (0.31 - 0.52) | (1.01 - 1.50) |
All values include sample weights and adjust for complex survey design.
+p<0.10
p<0.001.
p<0.01.
p<0.05.
References
- Abel Thomas, Frohlich Katherine L. Capitals and capabilities: linking structure and agency to reduce health inequalities. Social Science Medicine. 2012;74(2):236–244. doi: 10.1016/j.socscimed.2011.10.028. [DOI] [PubMed] [Google Scholar]
- American Lung Association . Department of Epidemiology and Statistics; New York, NY: 2001. Trends in tobacco use. [Google Scholar]
- Berrigan David, Dodd Kevin, Troiano Richard P., Krebs-Smith Susan M., Barbash Rachel B. Patterns of health behavior in Us Adults. Preventive Medicine. 2003;36(5):615–623. doi: 10.1016/s0091-7435(02)00067-1. [DOI] [PubMed] [Google Scholar]
- Bobo Janet Kay, Greek April A., Klepinger Daniel H., Herting Jerald R. Predicting 10-year alcohol use trajectories among men age 50 years and older. The American Journal of Geriatric Psychiatry. 2013;21(2):204–213. doi: 10.1016/j.jagp.2012.10.021. [DOI] [PubMed] [Google Scholar]
- Bourdieu Pierre. In: Distinction: a social critique of the judgment of taste. Nice R., editor. Harvard University Press; Cambridge, MA: 1984. [Google Scholar]
- Cantiello John, Fottler Myron D., Oetjen Dawn, Zhang Ning Jackie. The impact of demographic and perceptual variables on young adults decision to be covered by private health insurance. BMC Health Services Research. 2015;15:195. doi: 10.1186/s12913-015-0848-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2014). National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014Congress
- Christensen Vibeke T., Carpiano Richard M. Social class differences in BMI among Danish women: applying Cockerham's health lifestyles approach and Bourdieu's theory of lifestyle. Social Science Medicine. 2014;112:12–21. doi: 10.1016/j.socscimed.2014.04.017. [DOI] [PubMed] [Google Scholar]
- Cockerham William C. Health lifestyle theory and the convergence of agency and structure. Journal of Health and Social Behavior. 2005;46(1):51–67. doi: 10.1177/002214650504600105. [DOI] [PubMed] [Google Scholar]
- Cockerham William C. The sociology of health behavior and health lifestyles. In: Bird C.E., Conrad P., Fremont A.M., editors. Handbook of medical sociology. 5th Ed. Prentice Hall; Upper Saddle River, NJ: 2000. pp. 159–172. [Google Scholar]
- Cockerham William C. Health lifestyles in Russia. Social Science Medicine. 2000;51(9):1313–1324. doi: 10.1016/s0277-9536(00)00094-0. [DOI] [PubMed] [Google Scholar]
- Cockerham William C., Hinote Brian P., Cockerham Geoffrey B., Abbott Pamela. Health lifestyles and political ideology in Belarus, Russia, and Ukraine. Social Science Medicine. 2006;62(7):1799–1809. doi: 10.1016/j.socscimed.2005.08.024. [DOI] [PubMed] [Google Scholar]
- Coups Elliot J., Gaba Ayorkor, Orleans C. Tracy. Physician screening for multiple behavioral health risk factors. American Journal of Preventive Medicine. 2004;27(2 Suppl):34. doi: 10.1016/j.amepre.2004.04.021. [DOI] [PubMed] [Google Scholar]
- Dawson Deborah A. Defining risk drinking. Alcohol Research and Health. 2011;34(2):144. [PMC free article] [PubMed] [Google Scholar]
- Dawson Deborah A. Beyond black, white, and hispanic: race, ethnic origin and drinking patterns in the United States. Journal of Substance Abuse. 1998;10(4):321–339. doi: 10.1016/s0899-3289(99)00009-7. [DOI] [PubMed] [Google Scholar]
- de Vries Hein, van ‘t Reit Jonathan, Spigt Mark, Metsemakers Job, van den Akker Marjan, Vermunt Jeroen K., Kremers Stef. Clusters of lifestyle behaviros: results from the Dutch Smile study. Preventive Medicine. 2008;46:203–208. doi: 10.1016/j.ypmed.2007.08.005. [DOI] [PubMed] [Google Scholar]
- Fine Lawrence J., Philogene G.Stephane, Gramling Robert, Coups Elliot J., Sinha Sarbajit. Prevalence of multiple chronic disease risk factors: 2001 National Health Interview Survey. American Journal of Preventive Medicine. 2004 doi: 10.1016/j.amepre.2004.04.017. [DOI] [PubMed] [Google Scholar]
- Ford Earl S., Zhao Guixiang, Tsai James, Li Choyang. Low-risk behaviors and all-cause mortality: findings from the National Health and Nutrition Examination Survey III Mortality study. American Journal of Public Health. 2011;101(10):1922–1929. doi: 10.2105/AJPH.2011.300167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frohlich Katherine L., Corin Ellen, Potvin Louise. A theoretical proposal for the relationship between context and disease. Sociology of Health Illness. 2001;23(6):776–797. [Google Scholar]
- Garcia Raul I., Henshaw Michelle M., Krall Elizabet. Relationship between periodontal disease and systemic health. Periodontology. 2000;25:21–36. doi: 10.1034/j.1600-0757.2001.22250103.x. [DOI] [PubMed] [Google Scholar]
- Harris Kathleen Mullan. An integrative approach to health. Demography. 2010;47(1):1–22. doi: 10.1353/dem.0.0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haskell William L., Lee I.-Min, Pate Russell R., Powell Kenneth E., Blair Steven N., Franklin Barry A., Macera Caroline A., Heath Gregory W., Thompson Paul D., Bauman Adrian. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . National Academies Press; Washington, D.C: 2001. Health and behavior: the interplay of biological, behavioral, and societal influences. Committee on health and behavior: research, practice and policy board on neuroscience and behavioral health. [PubMed] [Google Scholar]
- Jackson James S., Knight Katherine M., Refferty Jane A. Race and unhealthy behaviors: chronic stress, the Hpa Axis, and physical and mental health disparities over the life course. American Journal of Public Health. 2010;100(5):933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindig David A., Cheng Erika R. Even as mortality fell in most U.S. counties, female mortality nonetheless rose in 42.8 percent of counties from 1992 to 2006. Health Affairs. 2013;32(3):1–8. doi: 10.1377/hlthaff.2011.0892. [DOI] [PubMed] [Google Scholar]
- Khaw Kay-Tee, Wareham Nicholas, Bingham Sheila, Welch Ailsa, Luben Robert, Day Nicholas. Combined impact of health behaviours and mortality in men and women: the EPIC-Norfolk prospective population study. PLoS Medicine. 2008;5(1):e12. doi: 10.1371/journal.pmed.0050012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korn Edward L., Graubard Barry I., Midthune Douglas. Time-to-event analysis of longitudinal follow-up of a survey: choice of the time scale. American Journal of Epidemiology. 1997;145(1):72–80. doi: 10.1093/oxfordjournals.aje.a009034. [DOI] [PubMed] [Google Scholar]
- Krueger Patrick M., Bhaloo Tajudaullah, Rosenau Pauline Vaillancourt. Vol. 90. 2009. Health lifestyles in the U.S. and Canada: are we really so different? pp. 1380–1402. (Social Science Quarterly). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger Patrick M., Saint Onge Jarron M., Chang Virginia W. Race/ethnic differences in adult mortality: the role of perceived stress and health behaviors. Social Science Medicine. 2011;73(9):1312–1322. doi: 10.1016/j.socscimed.2011.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kvaavik Elisabeth, Batty David, Giske Ursin, Huxley Rachel, Gale Catharine R. Influence of individual and combined health behaviors on total and cause-specific mortality in men and women: the United Kingdom Health and Lifestyle Survey. Archives of Internal Medicine. 2010;170(8):711–718. doi: 10.1001/archinternmed.2010.76. [DOI] [PubMed] [Google Scholar]
- Laska Melisa Nessaon, Pasch Keryn E., Lust Katherine, Story Mary, Ehlinger Ed. Vol. 10. 2009. Latent class analysis of lifestyle characteristics and health risk behaviors among college youth. (Prevention Science). (476-386) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loef Martin, Walach Harald. The combined effects of healthy lifestyle behaviors on all-cause mortality: a systematic review and meta-analysis. Preventive Medicine. 2012;55(3):163–170. doi: 10.1016/j.ypmed.2012.06.017. [DOI] [PubMed] [Google Scholar]
- Long J. Scott. Vol. 7. Sage; Thousand Oaks, CA: 1997. (Regression models for categorical and limited dependent variables). [Google Scholar]
- Minnesota Population Center . University of Minnesota; Minneapolis: 2010. Integrated health interview series: Version 5.0. [Google Scholar]
- Mirowsky John, Ross Catherine E. Education, health, and the default American lifestyle. Journal of Health and Social Behavior. 2015;56(3):297–306. doi: 10.1177/0022146515594814. [DOI] [PubMed] [Google Scholar]
- Mokdad Ali H., Marks James S., Stroup Donna F., Gerberding Julie L. Actual causes of death in the United States, 2000. Journal of the American Medical Association. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Mollborn Stefanie, James-Hawkins Laurie, Lawrence Elizabeth, Fomby Paula. Health lifestyles in early childhood. Journal of Health and Social Behavior. 2014;55(4):386–402. doi: 10.1177/0022146514555981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munthen Bengt. Statistical and substantive checking in growth mixture modeling: comment on Bauer and Curran (2003) Psychological Methods. 2003;8(3):369–377. doi: 10.1037/1082-989X.8.3.369. [DOI] [PubMed] [Google Scholar]
- Muthén, L. and Muthén B. (2007). Mplus: Statistical Analysis with Latent Variables; User’s Guide;[Version 5]: Muthén & Muthén
- National Center for Health Statistics (NCHS) (2015). Office of Analysis and Epidemiology. Public-use Linked Mortality File, 2015. Hyeattsville, Maryland. (Available at the follwing address: 〈http://www.cdc.gov/nchs/data_access/data_linkae/mortality.htm〉)
- National Center for Health Statistics (2013). Health, United States 2012. Hyattsville, MD [PubMed]
- Orleans C.Tracy. Addressing multiple behavioral health risks in primary care. Broadening the focus of health behavior change research and practice. American Journal of Preventive Medicine. 2004;27(2 Suppl):1. doi: 10.1016/j.amepre.2004.05.001. [DOI] [PubMed] [Google Scholar]
- Pampel Fred C. Diffusion, cohort change, and social patterns of smoking. Social Science Research. 2005;34(1):117–139. doi: 10.1016/j.ssresearch.2003.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pampel Fred C. Does reading keep you thin? Leisure activities, cultural tastes, and body weight in comparative perspective. Sociology of Health Illness. 2012;34(3):396–411. doi: 10.1111/j.1467-9566.2011.01377.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pampel Fred C., Krueger Patrick M., Denney Justin T. Socioeconomic disparities in health behaviors. Annual Review of Sociology. 2010;36:349–370. doi: 10.1146/annurev.soc.012809.102529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson Ruth E., Haines Pamela S., Popkin Barry M. Health lifestyle patterns of Us aults. Preventive Medicine. 1994;23(4):453–460. doi: 10.1006/pmed.1994.1062. [DOI] [PubMed] [Google Scholar]
- Pronk Nicolaas P., Anderson Louise H., Crain A. Lauren, Martinson Brian C., O’Connor Patrick J., Sherwood Nancy E., Whitebird Robin R. Meeting recommendations for multiple healthy lifestyle factors: prevalence, clustering, and predictors among adolescent, adult, and senior health plan members. American Journal of Preventive Medicine. 2004;27(2):25–33. doi: 10.1016/j.amepre.2004.04.022. [DOI] [PubMed] [Google Scholar]
- Reeves Mathew J., Rafferty Anne P. Healthy lifestyle characteristics among adults in the United States, 2000. Archives of Internal Medicine. 2005;165(8):854–855. doi: 10.1001/archinte.165.8.854. [DOI] [PubMed] [Google Scholar]
- Rogers Richard G., Krueger Patrick M., Miech Richard, Lawrence Elizabeth M., Kemp Robert. Nondrinker mortality risk in the U.S. Population Research and Policy Review. 2013;32(3):325–352. doi: 10.1007/s11113-013-9268-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saint Onge Jarron M., Krueger Patrick M. Education and race/ethnic differences in types of exercise in the United States. Journal of Health and Social Behavior. 2011;52(2):197–211. doi: 10.1177/0022146510394862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saint Onge Jarron M., Krueger Patrick M., Rogers Richard G. The relationship between major depression and non-suicide mortality for U.S. adults: then importance of health behaviors. Journals of Gerontology. 2014;69(4):622–632. doi: 10.1093/geronb/gbu009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiller, J., Lucas J., Ward B. and Peregoy J. (2012). Summary Health Statistics for U.S. Adults: National Health Interview Survey, 2010. Congress. Vital Health Statistics 10 [PubMed]
- Schoenborn, C., Adams P. and Peregoy J. (2013). Health Behaviors of Adults: United States, 2008–2010. Congress. Vital Health Statistics10 [PubMed]
- Singh Meeta, Drake Christoper L., Roehrs Timothy, Hudgel David W., Roth Thomas. The association between obesity and short sleep duration: a population-based study. Journal of Clinical Sleep Medicine. 2005;1(4):357–363. [PubMed] [Google Scholar]
- Skalamera Julie, Hummer Robert A. Educational attainment and the clustering of health-related behavior among U.S. young adults. Preventive Medicine. 2016;84:83–89. doi: 10.1016/j.ypmed.2015.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer Carole A., Norman Paul E., Lawrence-Brown Michael. A simple lifestyle score predicts survival in healthy elderly men. Preventive Medicine. 2005;40(6):712–717. doi: 10.1016/j.ypmed.2004.09.012. [DOI] [PubMed] [Google Scholar]
- Spring Bonnie, Moller Arlen C., Coons Michael J. Multiple health behaviors: overview and implications. Journal of Public Health. 2012;34(S1):i3–i10. doi: 10.1093/pubmed/fdr111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (2015). Healthy People 2020. Washington, D.C. Washington, D.C. Retrieved February 3, 2015
- Vermunt J.K., Magidson J. Latent class analysis. In: Lewis-Beck M., Bryman A., Liao T.F., editors. The Sage encyclopedia of social sciences research methods. Sage Publications; Thousand Oakes, CA: 2004. pp. 549–553. [Google Scholar]