Abstract
Study Design:
Retrospective cohort study.
Objective:
To compare perioperative characteristics of stand-alone cages and anterior cervical plates used for anterior cervical discectomy and fusion (ACDF).
Methods:
We reviewed 40 adult patients who received a stand-alone cage for elective ACDF and matched them with 40 patients who received an anterior cervical plate. We statistically compared operative time, length of stay, proportion of ambulatory cases, overall complications necessitating a trip to the ED, readmission, or reoperation related to index procedure.
Results:
There were 21 women and 19 men in the plate cohort with average ages of 53 years ± 12 and 20 women and 20 men in the stand-alone group with an average age of 52 years ± 11. With no statistical difference in total number, the plate group experienced 4 short-term (within 90 days of discharge) complications, including 3 patients who visited the emergency department for dysphagia and 1 who visited the emergency department for severe back pain, while the stand-alone group experienced 0 complications. There was no significant difference in operative time between the stand-alone group (75.35 min) and the plate group (81.35 min; P = .37). There was a significant difference between the proportion of ambulatory cases in the stand-alone group (25) and the plate group (6; P < .0001).
Conclusion:
Our results demonstrate that stand-alone cages have fewer complications compared to anterior plating, with a lower trend of incidence of postoperative dysphagia. Stand-alone cages may offer the advantage of sending patients home ambulatory after ACDF surgery.
Keywords: anterior cervical surgery, cervical fusion, stand-alone device, zero-profile device, dysphagia, cervical plating
Introduction
Anterior cervical discectomy and fusion (ACDF) was developed by Smith and Robinson in 1958 for the treatment of neurologic deficits and symptoms associated with cervical spine degeneration.1,2 The anterior approach affords access to the entire cervical spine through an intermuscular plane. This muscle-sparing interval is generally better tolerated by patients and has been shown to lead to fewer procedure-related complications than the posterior approach.3 First described for use in cervical trauma, the advent of anterior plating has become a popular adaptation of the procedure to improve postoperative segmental stability and has been shown to drastically increase fusion rates following ACDF.4-6
Despite its effectiveness, anterior plating is associated with a number of potential drawbacks. Apart from the initial design and application flaws that lead to higher incidence of adjacent level disease,7-9 some literature suggests that soft tissue injury and dysphagia are among the most common complications linked to plating.10-12 Though the underlying cause of plate-related dysphagia is not well understood, plate design does seem to have an effect on dysphagia incidence. Not surprisingly, plate size and shape has been implicated in development of postoperative dysphagia; wider and thicker plates have been shown to have a significantly higher incidence of postoperative dysphagia.13
Stand-alone cages were developed as a means to mitigate the complications associated with anterior plating. These devices employ screws to anchor an interbody spacer directly into the adjacent endplates and do not use any additional internal fixation or plating. This design provides a smoother and more anatomic juxtaposition for the esophagus on the anterior cervical spine. Stand-alone cages afford comparable mechanical stability and efficacy compared to anterior plating, but current literature is polarizing with regard to their complication incidence.14-17 Additionally, no studies have directly compared cases performed utilizing a plate or stand-alone cage with respect to length of hospital stay or ability to send patients home the same day of surgery.18
The objective of this retrospective cohort analysis was to expand on operative and perioperative characteristics, with an emphasis on length of stay, safety of ambulatory status, and dysphagia- or airway-related complications following ACDF surgery performed with either a stand-alone cage or an anterior plate by direct comparison of 2 matched cohorts. As a secondary goal, we aim to establish the safety profile of same-day discharge after such procedures.
Methods
Patient Cohorts
The institutional review board approved this retrospective cohort study of patients who underwent ACDF surgery for radiculopathy or cervical spondylotic myelopathy that did not respond to conservative measures by a single surgeon at a single center between 2012 and 2016. The surgeon began using stand-alone devices sparingly in 2012, and exclusively began using them for ACDF in 2015. We included single- and multilevel primary procedures. Any cases with prior instrumentation of the cervical spine were excluded. A total of 153 cases were performed during this time period. Of these, 52 were treated with stand-alone devices of which 12 were excluded for having prior instrumentation. Of the 12 excluded cases, 4 cases fell into the first 26 of these procedures performed by the lead surgeon while 8 cases of the last 26 procedures were excluded, all due to prior instrumentation to the operative levels. The 40 remaining primary fusions treated with stand-alone devices were matched using a logistic regression–based matching algorithm available within IBM SPSS (Armonk, NY) to 40 patients treated with an anterior cervical plate for a primary fusion. Matching was based on number of operative levels, gender, age, Charlson Comorbidity Index, smoking status, hypertension, and body mass indexd.19 A summary of the patient characteristics for the matched cohorts is presented in Table 1.
Table 1.
Patient Characteristics Between ACDF Cases Performed With Either a Stand-Alone Cage or Anterior Cervical Platea.
| Stand-Alone, n = 40 | Plate, n = 40 | P | |
|---|---|---|---|
| Male | 20 | 19 | 1.0000 |
| Female | 20 | 21 | |
| Age (years) | 52 ± 11 | 53 ± 12 | .8240 |
| Hypertension | 10 | 11 | .7847 |
| Charlson Comorbidity Index | 1.32 ± 1.49 | 1.57 ± 1.39 | .4390 |
| Smoker | 6 | 5 | 1.0000 |
| Body mass index | 27.53 ± 5.03 | 28.47 ± 5.62 | .5364 |
| Time since surgery (weeks) | 50.01 ± 39.94 | 141.80 ± 44.69 | <.0001 |
Abbreviation: ACDF, anterior cervical discectomy and fusion.
aContinuous values reported as mean ± SD.
Chart Review and Decisions of Discharge
Patient charts were accessed through the electronic medical record to obtain all demographic and perioperative data. Age is reported as age at the time of surgery. Length of stay was calculated as day of surgery to the day of discharge from the orthopedic spine service. Patients that were discharged on postoperative day 0 (day of surgery) were considered ambulatory. Discharge on day of surgery required an operating room time <2 hours, surgeon and ambulatory staff evaluation, as well as passing of a speech and swallow test with no potential signs of complication such as difficulty breathing, neurologic disturbances, or recurrence/worsening of preoperative symptomatology. Additionally, patients were required to undergo a minimum of 4 hours of observation in the post-anesthesia care unit, which involved a focused physical examination every hour. In order to be considered for same-day discharge, the patient had to meet institutional criteria, which included the aforementioned milestones in addition to a soft, palpable neck around the incision, dry dressing, and thin liquid and solid PO tolerance. Once clearing this protocol, the decision was made on a case-by-case basis by the surgeon, ancillary staff, and patient regarding disposition. Ambulatory patients were removed from calculations involving length of stay. Complications were determined from any patient readmissions or emergency department (ED) visits within 90 days of discharge, from operative reports for related complications within 90 days of discharge, and from office follow-up notes within 90 days of discharge. Chart review aimed to identify any and all complications related to the procedure including residual pain that necessitated readmission or an ED encounter, symptoms related to dysphagia, dysphonia, or airway compromise that required readmission or an ED encounter, or any case of reoperation related to index procedure during that time frame. Operative time was determined from the anesthesia report for each procedure.
Statistical Analysis
All analyses were performed with Prism GraphPad V6 (La Jolla, CA). Continuous variables between groups were compared with a paired t test, with the exception of length of stay and time since operation, which were compared with an unpaired t test. Contingent variables between groups were compared with a Fisher’s exact test. Statistical significance was considered to be P < .05.
Results
Patient Cohorts
All patients received ACDF for segmental cervical spondylosis resulting in either radiculopathy or myelopathy. There was a statistical difference (P = <.0001) with respect to weeks since operation between the stand-alone (50.01 ± 39.94) and plate groups (141.80 ± 44.69).
Operative Characteristics
A breakdown of the operative levels is presented in Table 2. There were a total of 50 levels operated on in each group. Of the 40 stand-alone patients, 1 received a Synthes Zero-P stand-alone device (DePuy Synthes Spine, Inc, Raynham, MA), 3 received a Biomet zero-profile interbody device (Zimmer Biomet, Warsaw, IN), and 36 received a Stryker Anchor C device (Stryker Spine, Allendale, NJ). Of the 40 patients who received machined allograft and anterior cervical plating, 20 received Medtronic Venture (Medtronic, Minneapolis, MN), 7 received Atlantis Elite (Medtronic, Minneapolis, MN), 5 received Biomet MaxAn (Zimmer Biomet, Warsaw, IN), 4 received Stryker Reflex Hybrid (Stryker Spine, Allendale, NJ), 3 received Stryker Aviator (Stryker Spine, Allendale, NJ), and 1 received DePuy CSLP (DePuy Synthes Spine, Inc, Raynham, MA). Anterior cervical plating was used in all cases of allograft and anterior cervical plating procedures, including single-level ACDF, as this is the protocol of the lead surgeon.
Table 2.
Breakdown of Total Levels Fused and Number of Vertebral Levels per Operation for ACDF Cases Performed With Either a Stand-Alone Cage or Anterior Cervical Platea.
| Stand-Alone, n = 40 | Plate, n = 40 | P | |
|---|---|---|---|
| Total number of vertebral levels | 50 | 50 | |
| Number of vertebral levels per operation | 1.25 ± 0.44 | 1.25 ± 0.44 | >.9999 |
| One-level fusion | 30 | 30 | |
| Two-level fusion | 10 | 10 | |
| Radiculopathy | 15 | 13 | .8149 |
| Myelopathy | 25 | 27 |
Abbreviation: ACDF, anterior cervical discectomy and fusion.
aRadiculopathy or cervical spondylotic myelopathy as an indication are also reported.
Total Complications and Emergency Department Visits
There were a total of 4 short-term (within 90 days of discharge) complications in the anterior plating group, and no complications in the stand-alone cage group (Table 3). Each of the 4 complications for the plate group occurred within 7 days of discharge and necessitated an ED visit, though none required readmission to the hospital. Three of the complications were related to dysphagia and the fourth was for severe neck and shoulder pain. Three of the complaints of dysphagia and the complaint of severe neck and shoulder pain occurred following single-level procedures. All of the complications occurred in patients treated with a Medtronic Venture plate. All of the patients were discharged from the ED the same day after pain control and reassurance. None of the stand-alone patients were readmitted to the ED or hospital within 90 days of discharge.
Table 3.
Comparison of Short-Term (90 Day) Complications Between ACDF Cases Performed With a Plate or Stand-Alone Cage. Type of Complication and Significance Indicated.
| Stand-Alone, n = 40 | Plate, n = 40 | P | |
|---|---|---|---|
| Total complications | 0 | 4 | .1156 |
| Dysphagia | 0 | 3 | .2405 |
| Severe pain | 0 | 1 | 1.0000 |
Abbreviation: ACDF, anterior cervical discectomy and fusion.
Operative Time
The average operative time for stand-alone group was 75.35 ± 27.82 minutes, and the average operative time for the plate group was 81.35 ± 28.01 minutes. There was no statistical difference between the average operative times (P = .37).
Length of Stay and Ambulatory Versus Day of Admission Surgery Cases
A total of 25 patients in the stand-alone group and 6 patients in the plate group were ambulatory. This finding was statistically significant with the proportion of ambulatory cases between the 2 groups yielding a P value of <.0001 (Figure 1). For nonambulatory cases, the average length of stay for the stand-alone group was 1.88 ± 1.36 days compared to 1.35 ± 0.69 days for the plate group, which trended toward but failed to reach significance (P = .08).
Figure 1.
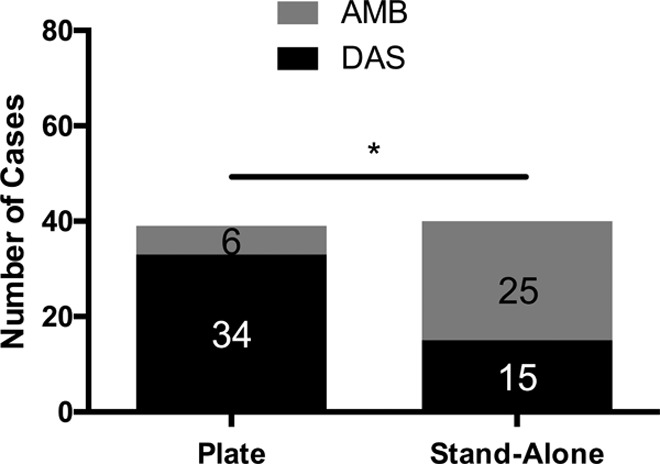
Comparison of the proportion of ambulatory (AMB) and day of admission surgery (DAS) between the 2 groups. The asterisk (*) indicates a significant difference in the proportions between the 2 groups.
Discussion
ACDF, first developed by Smith and Robinson in 1958, has undergone an intricate evolution to enhance fusion, alignment, and patient satisfaction. The addition of anterior plating almost 30 years ago has afforded an expansion in indications for the procedure, as well as improved clinical success, with increased fusion rates in as many as 3 consecutive fused levels.20
While its advantage of a stable construct with decreased subsidence and graft extrusion rates are unquestioned,21 anterior plating has also been criticized for its prevalent physical profile abutting the anterior cervical spine.7-13 Literature has shown that some plate designs are associated with increased esophageal injury and irritation, dysphagia, overhang leading to adjacent segment disease, and adhesions to the plate causing neck pain.12,22,23 In order to mitigate these potential complications, while maintaining the stability necessary to achieve solid fusion, zero-profile stand-alone cages were invented.
Success of the design of such stand-alone cages hinges on fixation of the interbody cage to the adjacent vertebral bodies. Several variations of the design exist today, though all prototypes rely on fixed angle screws through the adjacent endplates’ dense subchondral bone, anchoring the implant in the intervertebral space. Since the first Food and Drug Administration–approved stand-alone device was made available in 2008, several studies have sought to evaluate the implant and compare it to ACDF with anterior plating. Many studies have shown equivalent radiographic and clinical results as well as a lower incidence of postoperative dysphagia.24-30 However, no study has directly compared the 2 groups with regard to length of stay, ambulatory versus inpatient status, and overall complication profiles, leading many skeptics to question the safety of stand-alone cages.
Our results show that stand-alone cages resulted in a trend toward fewer total short-term complications along with a statistically significant greater number of patients being transitioned to ambulatory status. The decision of whether a patient was released on the day of surgery or admitted was multifaceted and employed a multidisciplined approach. We required patients to pass a series of tests including a speech and swallow assessment as well as evaluation by several medical personnel. This follows a “safety first” paradigm, while also decreasing the economic burden of the procedure. McGirt et al expanded on the safety and cost-saving potential of ambulatory ACDF comparing it to the traditional inpatient postoperative track.31 Their group found no difference in rate of adverse events from the immediate postoperative period until 90 days out with a significant decrease in 3-month total cost in the ambulatory group.31 These findings have been reproduced throughout the literature, validating ambulatory ACDF as safe and efficacious means to reduce hospital stays and their associated economic burdens to the health care system.32-36 However, these studies were all performed utilizing anterior cervical plating methods, suggesting same-day discharge is safe for single- and 2-level ACDF. Our findings assist in extrapolating these results to include zero-profile implants utilized for ACDF, further validating the body of evidence for same-day discharge for single- and 2-level ACDF, regardless of implant design, as a safe practice. However, further long-term longitudinal follow-up is needed to determine longevity, subsidence, and fusion rates of zero-profile devices to better characterize their efficacy.
In addition to safely discharging ambulatory patients at high rate (25/40), our results also parallel existing literature as we report a trend toward lower rates of dysphagia after stand-alone implantation compared to the anterior plate group. While the plate group experienced a rather high incidence of tracheoesophageal complications (12.5%), no patients that received a stand-alone device necessitated treatment for such complaints. This is concordant with recent literature, including a meta-analysis by Shao et al, which reliably showed a reduction in postoperative dysphagia at several time points after stand-alone ACDF compared to anterior plating.16 And while the pathophysiology of postoperative dysphagia is still not fully understood, one must not ignore the association between anterior plating and increased rates of dysphagia that was again supported by our results.
Our study has several limitations, first being the small sample size. While 80 patients is a relatively large single surgeon comparison, larger prospective randomized studies are needed to further validate our claims. Also, while the option to discharge a patient home on the same day of surgery first required meeting several objective criterion as part of an institutional protocol as detailed in the Methods section, some subjectivity in the form of patient pain tolerance, body habitus, and overall symptom relief in a brief postoperative monitoring period may have added some uncontrollable variables that may have affected the results of the study. Additionally, though irrelevant to our study aim of comparing hospital stay and perioperative and short-term characteristics, we lack long-term longitudinal follow-up, which is needed to characterize efficacy of zero-profile devices.
Conclusion
ACDF using a zero-profile stand-alone device is a safe alternative to traditional interbody with anterior plating constructs as shown through our short-term data relevant to the 90-day postoperative period. Patients in the zero-profile implant group experienced significantly higher rates of early discharge on day of surgery and trended toward less overall as well as tracheoesophageal-related complications.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Sheeraz A. Qureshi has the following disclosures: Paid consulting—Zimmer, Medtronic, Stryker, Orthofix Inc; IP royalties—Zimmer; Paid speaker—Globus Medical, Medtronic, Stryker. The other authors have no conflicts of interest to report.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40:607–624. [PubMed] [Google Scholar]
- 2. Matz PG, Holly GT, Groff MW, et al. Indications for anterior cervical decompression for the treatment of cervical degenerative radiculopathy. J Neurosurg Spine. 2009;11:174–182. [DOI] [PubMed] [Google Scholar]
- 3. Memtsoudis SG, Hughes A, Ma Y, Chiu YL, Sama AA, Girardi FP. Increased in-hospital complications after primary posterior versus primary anterior cervical fusion. Clin Orthop Relat Res. 2011;469:649–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Caspar W, Barbier DD, Klara PM. Anterior cervical fusion and Caspar plate stabilization for cervical trauma. Neurosurgery. 1989;25:491–502. [DOI] [PubMed] [Google Scholar]
- 5. Epstein NE. The management of one-level anterior cervical corpectomy with fusion using Atlantis hybrid plates: preliminary experience. J Spinal Disord. 2000;13:324–328. [DOI] [PubMed] [Google Scholar]
- 6. Anderson DG, Albert TJ. Bone grafting, implants, and plating options for anterior cervical fusions. Orthop Clin North Am. 2002;33:317–328. [DOI] [PubMed] [Google Scholar]
- 7. Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine (Phila Pa 1976). 1993;18:2167–2173. [DOI] [PubMed] [Google Scholar]
- 8. Hillibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81:519–528. [DOI] [PubMed] [Google Scholar]
- 9. Hillibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 2004;4:190S–194S. [DOI] [PubMed] [Google Scholar]
- 10. Fountas KN, Kapsalaki EZ, Nikolakakos LG, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976). 2007;32:2310–2317. [DOI] [PubMed] [Google Scholar]
- 11. Zhong ZM, Jiong JM, Qu DB, et al. Esophageal perforation related to anterior cervical spinal surgery. J Clin Neurosci. 2013;20:1402–1405. [DOI] [PubMed] [Google Scholar]
- 12. Yue WM, Brodner W, Highland TR. Persistent swallowing and voice problems after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year follow-up study. Eur Spine J. 2005;14:677–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lee MJ, Bazaz R, Furey CG, Yoo J. Influence of anterior cervical plate design on dysphagia: a 2-year prospective longitudinal follow-up study. J Spinal Disord Tech. 2005;18:406–409. [DOI] [PubMed] [Google Scholar]
- 14. Stein MI, Nayak AN, Gaskins RB, Cabezas AF, Santoni BG, Castellvi AE. Biomechanics of an integrated interbody device versus ACDF anterior locking plate in a single-level cervical spine fusion construct. Spine J. 2014;14:128–136. [DOI] [PubMed] [Google Scholar]
- 15. Yang H, Chen D, Wang X, Yang L, He H, Yuan W. Zero-profile integrated plate and spacer device reduces rate of adjacent-level ossification development and dysphagia compared to ACDF with plating and cage system. Arch Orthop Trauma Surg. 2015;135:781–787. [DOI] [PubMed] [Google Scholar]
- 16. Shao H, Chen J, Ru B, et al. Zero-profile implant versus conventional cage-plate implant in anterior cervical discectomy and fusion for the treatment of degenerative cervical spondylosis: a meta-analysis. J Orthop Surg. 2015;10:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nemoto O, Kitada A, Naitou S, Tachibana A, Ito Y, Fujikawa A. Stand-alone anchored cage versus cage with plating for single-level anterior cervical discectomy and fusion: a prospective, randomized, controlled study with a 2-year follow-up. Eur J Orthop Surg Traumatol. 2015;25(suppl 1):S127–S134. [DOI] [PubMed] [Google Scholar]
- 18. Tabaraee E, Ahn J, Bohl DD, et al. Comparison of surgical outcomes, narcotics utilization, and costs after an anterior cervical discectomy and fusion: stand-alone cage versus anterior plating [published online July 14, 2016]. Clin Spine Surg. doi:10.1097/BSD.0000000000000341. [DOI] [PubMed] [Google Scholar]
- 19. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 20. Fraser JF, Hartl R. Anterior approaches to fusion of the cervical spine: a meta-analysis of fusion rates. J Neurosurg Spine. 2007;6:298–303. [DOI] [PubMed] [Google Scholar]
- 21. Scholz M, Reyes PM, Schleicher P, et al. A new stand-alone cervical anterior interbody fusion device: biomechanical comparison with established anterior cervical fixation devices. Spine (Phila Pa 1976). 2009;34:156–160. [DOI] [PubMed] [Google Scholar]
- 22. Sahjpaul RL. Esophageal perforation from anterior cervical screw migration. Surg Neurol. 2007;68:209–210. [DOI] [PubMed] [Google Scholar]
- 23. Rhyne AL, 3rd, Spector LR, Schmidt GL, et al. Anatomic mapping and evaluation of the esophagus in relation to the cervical vertebral body. Eur Spine J. 2007;16:1267–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wang ZW, Jiang W, Li X, et al. The application of zero-profile anchored spacer in anterior cervical discectomy and fusion. Eur Spine J. 2015;24:148–154. [DOI] [PubMed] [Google Scholar]
- 25. Li YB, Hao D, He B, Wang X, Yan L. The efficiency of zero-profile implant in anterior cervical discectomy fusion: a prospective controlled long-term follow-up study. J Spine Discord Tech. 2013;28:398–403. [DOI] [PubMed] [Google Scholar]
- 26. Son DK, Son DW, Kim HS, Sung SK, Lee SW, Song GS. Comparative study of clinical and radiological outcomes of a zero-profile device concerning reduced postoperative dysphagia after single level anterior cervical discectomy and fusion. J Korean Neurosci. 2014;56:103–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Qi M, Chen H, Liu Y, Zhang Y, Liang L, Yuan W. The use of a zero-profile device compared with an anterior plate and cage in the treatment of patients with symptomatic cervical spondylosis: a preliminary clinical investigation. Bone Joint J B. 2013;95:543–547. [DOI] [PubMed] [Google Scholar]
- 28. Vanek P, Bradac O, Delacy P, Lacman J, Benes V. Anterior interbody fusion of the cervical spine with Zero-P spacer: prospective comparative study-clinical and radiological results at a minimum 2 years after surgery. Spine (Phila Pa 1976). 2011;38:E792–E797. [DOI] [PubMed] [Google Scholar]
- 29. Wang ZD, Zhu RF, Yang HL, et al. The application of a zero-profile implant in anterior cervical discectomy and fusion. J Clin Neurosci. 2014;21:462–466. [DOI] [PubMed] [Google Scholar]
- 30. Miao JH, Shen Y, Kuang Y, et al. Early follow-up outcomes of a new zero-profile implant used in anterior cervical discectomy and fusion. J Spinal Disord Tech. 2013;26:E193–E197. [DOI] [PubMed] [Google Scholar]
- 31. McGirt MJ, Godil SS, Adamson TE, Coric D, Dyer EH, Asher AL. Anterior cervical diskectomy and fusion in the ambulatory care setting defining its value across the acute and post-acute care episode. Neurosurgery. 2014;61:205. [Google Scholar]
- 32. Villavicencio AT, Pushchak E, Burneikiene S, Thramman JJ. The safety of instrumented outpatient anterior cervical discectomy and fusion. Spine J. 2007;7:148–153. [DOI] [PubMed] [Google Scholar]
- 33. Tally WC, Tarabadkar S, Kovalenko BC. Safety and feasibility of outpatient ACDF in an ambulatory setting: a retrospective chart review. Int J Spine Surg. 2013;7:e84–e87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wohns RR. Safety and cost-effectiveness of outpatient cervical disc arthroplasty. Surg Neurol Int. 2010;1:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Adamson T, Godil SS, Mehrlich M, et al. Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting compared with the inpatient hospital setting: analysis of 1000 consecutive cases. J Neurosurg Spine. 2016;24:878–884. [DOI] [PubMed] [Google Scholar]
- 36. Stieber JR, Brown K, Donald GD, et al. Anterior cervical decompression and fusion with plate fixation as an outpatient procedure. Spine J. 2005;5:503–507. [DOI] [PubMed] [Google Scholar]


