Abstract
Study Design:
Case-control study.
Objective:
To determine the incidence, impact, and risk factors for wound complications within 30 days following elective adult spinal deformity surgery.
Methods:
Current Procedural Terminology and International Classification of Diseases, Ninth Edition, diagnosis codes were used to query the database for adults who underwent spinal deformity surgery from 2010 to 2014. Patients were separated into groups of those with and without wound complications. Univariate analysis and multivariate logistic regression were used to analyze the influence of patient factors, operative variables, and clinical characteristics on the incidence of postoperative wound complication. This study was qualified as exempt by the Mount Sinai Hospital Institutional Review Board.
Results:
A total of 5803 patients met the criteria for this study. Wound complications occurred in 140 patients (2.4%) and were significantly associated with other adverse outcomes, including higher rates of unplanned reoperation (P < .0001) and prolonged length of stay (P < .0001). Regardless of fusion length, wound complication rates were higher with a posterior approach (short = 2.7%; long = 3.7%) than an anterior one (short = 2.2%; long = 2.7). According to the multivariate analysis, posterior fusion (odds ratio [OR] = 1.8; P = .010), obese class II (OR = 1.7; P = .046), obese class III (OR = 2.8; P < .0001), preoperative blood transfusion (OR = 6.1; P = .021), American Society of Anesthesiologists class ≥3 (OR = 1.7; P = .009), and operative time >4 hours (OR = 1.8; P = .006) were statistically significant risk factors for wound complications.
Conclusion:
The 30-day incidence of wound complication in adult spinal deformity surgery is 2.4%. The risk factors for wound complication are multifactorial. This data should provide a step toward developing quality improvement measures aimed at reducing complications in high-risk adults.
Keywords: adult spinal deformity, American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP), wound complication, infection, spinal fusion
Introduction
Adult spinal deformity (ASD) is becoming increasingly prevalent as the percentage of elderly in the United States accelerates.1,2 With the advancement of surgical techniques to treat ASD, there has been a concurrent rise in the number of patients opting for spinal fusion.3,4 This subset of patients is generally felt to be at higher risk for overall complications. Despite efforts to improve patient safety, surgical site infection (SSI) remains a burdensome risk for many adults undergoing spinal fusion surgery. Rates of SSI following spine fusion surgery range from 1% to 20%, varying with the procedure, patient demographic, and instrumentation use.5–8 In the literature, wound infections have been associated with higher morbidity and mortality, increased risk for readmission, and greater health care costs.9–11 Given the increased demand for ASD surgery, identifying the underlying factors that influence complication risk in this population is a critical step toward providing higher quality care.
Prior studies have investigated the potential risk factors for clinical outcomes following spinal fusion. Among the most recent published works, high body mass index (BMI), insulin-dependent diabetes mellitus, poor nutritional status, higher American Society of Anesthesiologists (ASA) status, longer hospital stay, and extended operative time were commonly found to be predictors for postoperative complications of spinal fusion.12–15 These studies were largely retrospective analyses, which focused on individual complications, specific subsets of spinal fusion procedures, general populations, or included wound complications in larger pooled-analysis of overall morbidity. Furthermore, many of these studies were single-center6,12 or single-surgeon retrospective series resulting in limited generalization given their inherent selection bias.12,14 Some studies have used the National Surgical Quality Improvement Program (NSQIP) database to assess postoperative outcomes after various spine surgeries; however, the impact of adult comorbidities on wound complications following ASD surgery remains undefined.
To our knowledge, no study has used a large-scale, multi-institutional database to describe the risk profile for wound complications in ASD patients. In this study, the American College of Surgeons (ACS) NSQIP database was used to investigate the incidence and underlying factors, which predict wound complications within 30 days of ASD surgery.
Materials and Methods
Data Source
The ACS NSQIP database is a multicenter registry, which collects more than 150 variables on patients undergoing major surgical procedures. This database is maintained by on-site surgical clinical reviewers (SCRs) at participating institutions. In order to ensure data of the highest quality and reliability, NSQIP employs a series of rigorous training programs for the SCRs and conducts an ongoing internal auditing process. Per NSQIP, the variables collected include preoperative risk factors, intraoperative variables, and 30-day postoperative mortality and morbidity outcomes. This study was qualified as exempt by the Mount Sinai Hospital Institutional Review Board.
Data Collection
This patient population was extracted from NSQIP Participant Use Data Files from 2010 to 2014. This study retrospectively reviewed all adult patients (≥18 years) who underwent spinal fusion for deformity using the following Current Procedural Terminology (CPT) codes: 22800, 22802, 22804, 22808, 22810, 22812, 22818, and 22819. CPT codes 22843, 22844, 22846, and 22847 were also included to capture long, multi-level fusion constructs. Patients with CPT codes 22842 and 22845 were included if they had an International Classification of Diseases, Ninth Edition, diagnosis for spinal deformity (including 737.1, 737.2, 737.3, 737.4, 737.8, and 737.9). Cases with missing preoperative data; wound class of 2, 3, or 4; an open wound on their body; current sepsis; current pneumonia; prior surgeries within 30 days; cases requiring cardiopulmonary resuscitation prior to surgery; emergency cases; or any patient undergoing a nonelective procedure were excluded from the analysis. Additionally, patients with diagnoses relating to cervical spine, trauma or injury to spine, or neoplasm of spine were excluded in order to focus on elective spinal deformity cases.
Independent Variables
Although the NSQIP database collects 150 variables, each patient case contains nearly 300 Health Insurance Portability and Accountability Act (HIPAA)–compliant data values, which include patient demographics, medical comorbidities, preoperative laboratory values, operative data, and postoperative outcomes. The additional variables relate to the computed elements of the originally collected data. Patient demographics include age, gender, race, and BMI. Other race included American Indian or Alaska Native, Asian, Native Hawaiian or Pacific Islander, or unknown. BMI was classified into separate classes: nonobese (BMI < 30), class I (30-34.9), class II (35-39.9), and class III (≥40). Other preoperative variables included diabetes (none, insulin dependent, non–insulin dependent), smoking status, dyspnea, functional status prior to surgery (independent, dependent), and ASA class.
Comorbidities included pulmonary (ventilator dependence during the 48 hours preceding surgery, chronic obstructive pulmonary disease), renal (acute renal failure, dialysis), cardiac (congestive heart failure within 30 days before admission, hypertension requiring medication) systems. Operative variables included health care setting (inpatient, outpatient), discharge destination (eg, home, rehab, skilled care facility), operative time, total relative value units (RVU). Using the list of CPT codes described in the work by Martin et al,16 this study categorized patients according to the type of surgical procedure performed. Additional procedure subanalyses of fusion length and approach were included as well.
Outcome Variables
The outcome variable of interest was wound complication within 30 days of surgery. The definition of wound complication included superficial SSI, deep SSI, wound dehiscence, or an organ space infection. Superficial SSI involves only skin or subcutaneous tissue, whereas deep SSI was an infection that involves deep soft tissues, such as fascial and muscle layers. Infections that involve both superficial and deep incisional sites were reported as deep incisional SSI. Wound dehiscence occurrences involved partial or complete disruptions of the fascia of a surgical wound. Organ space infection is related to organs or spaces other than the incision, which were opened or manipulated during an operation.17
To assess the impact of wound complications on other 30-day clinical outcomes, the rates of mortality, unplanned reoperations, blood transfusions, and total length of stay (LOS) >5 days were assessed for those with and without wound complication.
Statistical Analysis
To determine which candidate features were significantly associated with wound complication, both univariate and multivariate analyses were performed on variables related to patient demographics, comorbidities, preoperative laboratory tests, operative conditions, and other clinical parameters. Student t tests and χ2 tests were used for continuous and categorical variables, respectively. The Kendall Tau-b correlation coefficient was calculated to inspect any pattern between the incidences of wound complications versus operating years.
For the multivariate analysis, a stepwise logistic regression was fitted for the presence or absence of a wound complication. Any variable with a P value less than .2 from the univariate analysis was assessed in the multivariate analysis. Additionally, surgical procedure type was included in the model, as it has been previously described to be associated with SSI.18 Multivariate logistic regression requires a complete data set with no missing values. When preoperative laboratory data was included in the model, more than 60% of the cases were removed. For this reason, only a univariate analysis was performed on laboratory measures. The odds ratios (ORs) and 95% confidence intervals (CIs) were reported for the final multivariate model. The regression model was assessed using the C statistic, which is the area under the receiver operating characteristic curve. The quality of the model was assessed using the calibration of the Homer-Lemeshow test. A P value less than .05 was defined as significant. SAS software (Version 9.3; SAS Institute Inc, Cary, NC) was used for all statistical analyses.
Results
This study identified 5803 patients who underwent ASD surgery from 2010 to 2014. During this time, wound complication rates have trended downward (Kendall Tau-b correlation = −.013) from 3.33% to 2.38% (Figure 1). A total of 140 patients encountered at least one wound complication (2.4%), and nearly half of these cases were documented as superficial site infections (N = 62, 44.3%; Table 1).
Figure 1.
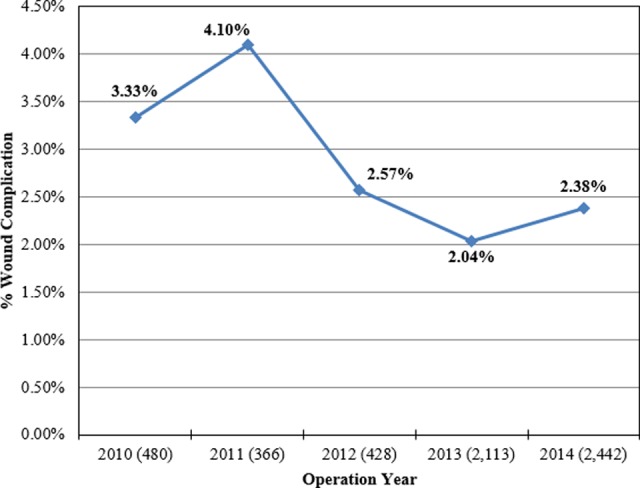
Adult deformity surgery: wound complication incidence versus year (Kendall Tau-b correlation = −.013).
Table 1.
Incidence of Wound Complications (2010-2014), N = 5803.
| Type | n | % |
|---|---|---|
| Patients with ≥1 wound complication | 140 | 2.4% |
| Superficial site infection | 62 | 1.1% |
| Deep surgical site infection | 49 | 0.8% |
| Wound dehiscence | 28 | 0.5% |
| Organ space infection | 17 | 0.3% |
Univariate Analysis
In the univariate analysis, patients with higher race (P = .003), age (P = .021), BMI (P < .0001), diabetes (P = .034), ASA class ≥3 (P < .0001), ventilator dependence (P = .0003), hypertension (P = .019), preoperative transfusion (P = .002), preoperative albumin (P = .011), preoperative hematocrit (P = .001), discharge status (P < .0001), operative time >4 hours (P < .0001), total RVU (P < .0001), fusion approach (P < .0001), pelvic fixation (P = .0004), and osteotomy (P = .002) were significantly associated with higher risk of complication (Tables 2 and 3).
Table 2.
Preoperative Variables for Those With and Without Wound Complication.a
| Total (N = 5802, 100%) | No Wound Complication (n = 5663, 97.6%) | Wound Complication (n = 140, 2.4%) | P Value | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Sex | |||||||
| Female | 3423 | 59.0% | 3338 | 58.9% | 85 | 60.7% | .674 |
| Male | 2380 | 41.0% | 2325 | 41.1% | 55 | 39.3% | |
| Race | |||||||
| White | 4709 | 81.1% | 4598 | 81.2% | 111 | 79.3% | .003 |
| Black | 442 | 7.6% | 431 | 7.6% | 11 | 7.9% | |
| Hispanic | 219 | 3.8% | 215 | 3.8% | 4 | 2.9% | |
| Otherb | 433 | 7.5% | 419 | 7.4% | 14 | 10.0% | |
| Age (years) | |||||||
| <51 | 1254 | 21.6% | 1235 | 21.8% | 19 | 13.6% | .021 |
| 51-60 | 1508 | 26.0% | 1472 | 26.0% | 36 | 25.7% | |
| 61-70 | 1841 | 31.7% | 1787 | 31.6% | 54 | 38.6% | |
| 71-80 | 1017 | 17.5% | 995 | 17.6% | 22 | 15.7% | |
| >80 | 183 | 3.2% | 174 | 3.1% | 9 | 6.4% | |
| BMI class | |||||||
| Nonobese | 3373 | 58.1% | 3311 | 58.5% | 62 | 44.3% | <.0001 |
| Obese class I | 1383 | 23.8% | 1348 | 23.8% | 35 | 25.0% | |
| Obese class II | 657 | 11.3% | 636 | 11.2% | 21 | 15.0% | |
| Obese class III | 390 | 6.7% | 368 | 6.5% | 22 | 15.7% | |
| Diabetes | |||||||
| No diabetes | 4955 | 85.4% | 4844 | 85.5% | 111 | 79.3% | .034 |
| Insulin dependent | 272 | 4.7% | 266 | 4.7% | 6 | 4.3% | |
| Non–insulin dependent | 576 | 9.9% | 553 | 9.8% | 23 | 16.4% | |
| Current smoker within 1 year | |||||||
| Yes | 1208 | 20.8% | 1182 | 20.9% | 26 | 18.6% | .508 |
| No | 4595 | 79.2% | 4481 | 79.1% | 114 | 81.4% | |
| Dyspnea | |||||||
| Yes | 347 | 6.0% | 337 | 6.0% | 10 | 7.1% | .557 |
| No | 5456 | 94.0% | 5326 | 94.0% | 130 | 92.9% | |
| Functional status prior to surgery | |||||||
| Independent | 5538 | 95.4% | 5408 | 95.5% | 130 | 92.9% | .051 |
| Dependent | 265 | 4.6% | 255 | 4.5% | 10 | 7.1% | |
| ASA | |||||||
| 1 or 2 | 2718 | 46.8% | 2678 | 47.3% | 40 | 28.6% | <.0001 |
| 3 or 4 | 3085 | 53.2% | 2985 | 52.7% | 100 | 71.4% | |
| Comorbidities | |||||||
| Ventilator dependent | 10 | 0.2% | 8 | 0.1% | 2 | 1.4% | .0003 |
| History of COPD | 286 | 4.9% | 282 | 5.0% | 4 | 2.9% | .216 |
| History of CHF | 24 | 0.4% | 23 | 0.4% | 1 | 0.7% | .575 |
| Hypertension requiring medication | 3162 | 54.5% | 3072 | 54.2% | 90 | 64.3% | .019 |
| Acute renal failure | 7 | 0.1% | 7 | 0.1% | 0 | 0.0% | .677 |
| Dialysis | 20 | 0.3% | 17 | 0.3% | 3 | 2.1% | .0002 |
| Steroid use for chronic condition | 219 | 3.8% | 214 | 3.8% | 5 | 3.6% | .899 |
| >10% loss body weight in last 6 months | 11 | 0.2% | 10 | 0.2% | 1 | 0.7% | .149 |
| Bleeding disorders | 70 | 1.2% | 67 | 1.2% | 3 | 2.1% | .304 |
| Preoperative transfusion of ≥1 unit of whole/packed RBCs in 72 hours prior to surgery | 13 | 0.2% | 11 | 0.2% | 2 | 1.4% | .002 |
| Preoperative laboratory values, mean (SD) | |||||||
| Albumin | 4.1 (0.5) | 4.1 (0.5) | 3.9 (0.5) | .011 | |||
| Hematocrit | 40.1 (4.5) | 40.1 (4.5) | 38.5 (5.2) | .001 | |||
| Platelet | 246.7 (71.6) | 246.7 (71.5) | 248.5 (78.1) | .778 | |||
| INR | 1.0 (0.2) | 1.0 (0.2) | 1.0 (0.4) | .118 | |||
| PTT | 29.3 (4.7) | 29.3 (4.6) | 29.2 (8.1) | .857 | |||
| PT | 12.0 (2.3) | 11.9 (2.3) | 12.5 (1.7) | .243 | |||
| Operative variables | |||||||
| Health care setting | |||||||
| Inpatient | 5592 | 96.4% | 5453 | 96.3% | 139 | 99.3% | .062 |
| Outpatient | 211 | 3.6% | 210 | 3.7% | 1 | 0.7% | |
| Discharge destination | |||||||
| Home | 3453 | 59.5% | 3,394 | 59.9% | 59 | 42.1% | <.0001 |
| Rehab | 522 | 9.0% | 506 | 8.9% | 16 | 11.4% | |
| Skilled care, not home | 548 | 9.4% | 522 | 9.2% | 26 | 18.6% | |
| Otherc | 32 | 0.6% | 32 | 0.6% | 0 | 0.0% | |
| Missing | 1248 | ||||||
| Operative time >4 hours | 2,779 | 47.9% | 2,680 | 47.3% | 99 | 70.7% | <.0001 |
| Total RVU, mean (SD) | 73.4 (28.8) | 73.1 (28.6) | 84.7 (32.8) | <.0001 | |||
Abbreviations: BMI, body mass index; ASA, American Society of Anesthesiologists; COPD, chronic obstructive pulmonary disease; CHF, congestive heart failure; RBC, red blood cell; INR, international normalized ratio; PTT, partial thromboplastin time; PT, prothrombin time; RVU, relative value unit.
aBoldface indicates statistically significant P = .05.
bRace Other = American Indian or Alaskan Native, Asian, Native Hawaiian or Pacific Islander, or unknown.
cOther Discharge Status = separate acute care, unknown, unskilled facility not home, death.
Table 3.
Procedure Subanalysis for Wound Complications.a
| Total (N = 5803, 100%) | No Wound Complication (n = 5663, 97.6%) | Wound Complication (n = 140, 2.5%) | |||||
|---|---|---|---|---|---|---|---|
| Procedure Subanalysis | n | % | n | % | n | % | P |
| Length of fusion | |||||||
| Short | 3657 | 63.0% | 3569 | 63.0% | 88 | 62.9% | .968 |
| Long | 2146 | 37.0% | 2094 | 37.0% | 52 | 37.1% | |
| Short fusion approach | |||||||
| Anterior | 583 | 10.0% | 570 | 10.1% | 13 | 9.3% | .559 |
| Posterior | 1664 | 28.7% | 1619 | 28.6% | 45 | 32.1% | |
| Combined | 99 | 1.7% | 95 | 1.7% | 4 | 2.9% | |
| Long fusion approach | |||||||
| Anterior | 1715 | 29.6% | 1700 | 30.0% | 15 | 10.7% | <.0001 |
| Posterior | 1626 | 28.0% | 1566 | 27.7% | 60 | 42.9% | |
| Combined | 116 | 2.0% | 113 | 2.0% | 3 | 2.1% | |
| Bone graftb | |||||||
| Yes | 4049 | 69.8% | 3958 | 69.9% | 91 | 65.0% | .213 |
| No | 1754 | 30.2% | 1705 | 30.1% | 49 | 35.0% | |
| Pelvic fixation | |||||||
| Yes | 482 | 8.3% | 459 | 8.1% | 23 | 16.4% | .0004 |
| No | 5321 | 91.7% | 5204 | 91.9% | 117 | 83.6% | |
| Osteotomy | |||||||
| Yes | 837 | 14.4% | 804 | 14.2% | 33 | 23.6% | .002 |
| No | 4966 | 85.6% | 4859 | 85.8% | 107 | 76.4% | |
| Intervertebral device insertion | |||||||
| Yes | 2410 | 41.5% | 2361 | 41.7% | 49 | 35.0% | .113 |
| No | 3393 | 58.5% | 3302 | 58.3% | 91 | 65.0% | |
aBoldface indicates P = .05.
bBone graft refers to either autograft (Current Procedural Terminology [CPT] 20936, 20937, 20938), allograft (20930, 20931), or bone marrow aspirate (38220); pelvic fixation (22848); osteotomy (22206, 22207, 22208, 22210, 22212, 22214, 22216, 22220, 22222, 22224, 22226); intervertebral device insertion (22851).
The incidence of wound complications was not associated with mortality (P = .343), but significantly associated with higher rates of intra-/postoperative blood transfusions (48.6%; P < .0001), LOS >5 days (55.7%; P < .0001), and unplanned reoperations (55.6%; P < .0001; Table 4).
Table 4.
Other Postoperative Complications Associated With Wound Complications.a
| Total (N = 5803, 100%) | No Wound Complication (n = 5663, 97.6%) | Wound Complication (n = 140, 2.5%) | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | P | |
| Transfusion (intra-/postoperative within 30 days) | 1568 | 27.0% | 1500 | 26.5% | 68 | 48.6% | <.0001 |
| Mortality | 29 | 0.5% | 27 | 0.5% | 2 | 1.4% | .115 |
| Length of stay >5 days | 1667 | 28.7% | 1589 | 28.1% | 78 | 55.7% | <.0001 |
| Unplanned reoperation (2011-2014), N = 5339 | 331 | 6.2% | 147 | 2.8% | 69 | 55.6% | <.0001 |
aBoldface indicates P = .05.
Multivariable Analysis
The multivariate analysis showed that a posterior surgical approach (OR = 1.8; CI = 1.2-2.9; P = .010), obese class II (OR = 1.7; CI = 1.0-2.8; P = .046), obese class III (OR = 2.8; CI = 1.7-4.7; P < .0001), preoperative blood transfusion (OR = 6.1; CI = 1.3-28.7; P = .021), ASA ≥ 3 (OR = 1.7; CI = 1.1-2.4; P = .009), and operative time >4 hours (OR = 1.8; CI = 1.2-2.7; P = .006) were statistically significant risk factors of postoperative wound complication (Table 5). The model had a C statistic of .722 and a Hosmer-Lemeshow P value equal to .143.
Table 5.
Independent Risk Factors for 30-Day Wound Complications Following ASD Surgery.a
| Effect | OR | 95% CI | P |
|---|---|---|---|
| Total RVU | 1.01 | 1.00-1.01 | .017 |
| Approach (reference = Anterior) | |||
| Combined | 1.7 | 0.7-4.2 | .233 |
| Posterior | 1.8 | 1.2-2.9 | .010 |
| Obesity class (reference = Nonobese) | |||
| Obese I | 1.4 | 0.9-2.2 | .094 |
| Obese II | 1.7 | 1.0-2.8 | .046 |
| Obese III | 2.8 | 1.7-4.7 | <.0001 |
| Blood transfusion (preoperative) | 6.1 | 1.3-28.7 | .021 |
| ASA ≥3 | 1.7 | 1.1-2.4 | .009 |
| Operative time >4 | 1.8 | 1.2-2.7 | .006 |
Abbreviations: ASD, adult spinal deformity; OR, odds ratio; CI, confidence interval; RVU, relative value unit; ASA, American Society of Anesthesiologists.
aBoldface indicates P = .05.
Discussion
The overall rate of wound complications for adults undergoing elective ASD surgery was 2.4%, with the majority having either an isolated superficial SSI (N = 62, 1.1%) or an SSI extending deep into the fascia (N = 48, 1.0%). This value was consistent with recently published studies that assess similar infection rates in adults.13,14,19–21 Additionally, this study found that wound complications were significantly associated with poor clinical outcomes, including prolonged LOS, higher rates of unplanned reoperation, and intra-/postoperative blood transfusion within 30 days of surgery. These findings emphasize the importance of studying wound complications in this defined population.
Higher ASA class as a risk factor early wound complication after spinal fusion has previously been demonstrated in prior works.13,19 Using the Veterans Affairs’ NSQIP database, 1997 to 2006, Veeravagu et al13 assessed 24 774 patients who underwent a spinal decompression and fusion and found that patients with ASA class 3 were 1.45 and ASA classes 4 to 5 were 1.66 times more likely to develop a wound infection after spinal surgery. In a more recent study, Tang et al19 assessed 236 patients who had undergone spinal fusion for degenerative lumbar scoliosis and came to a similar conclusion that there was a strong association between ASA class >2 and postoperative complications. This data suggests that preoperative ASA class ≥3 should be carefully considered for patients undergoing ASD surgery.
Many studies have documented surgical time as a risk factor for wound complications.13,19,22 According to this analysis, there was an 80% increase in the odds for postoperative wound complication in patients who experienced an operative time >4 hours. In general, procedural time is reflective of case complexity and has even been found to be directly related to the absolute number of bacteria found in a wound.23 Future interventions to reduce infection rates will require careful preoperative planning and effective implementation to minimize operative time, and thus exposure to bacteria.
This study demonstrates that a higher obesity class is associated with an increased likelihood of wound complication following ASD surgery. This finding is consistent with several other works.24–27 It is likely that BMI serves as a proxy measure for the thickness of subcutaneous fat and the skin-to-lamina distance, which are 2 known risk factors for SSIs.28 The increased adipose tissue may require a longer surgical time due to the need for deeper dissection. Prolonged surgical time in combination with thick adipose tissue, which is already poorly vascularized in comparison to muscular tissue, may increase the risk for the development of dead space and subsequent infection.
Patients with a preoperative blood transfusion were predisposed to a 6.1-fold increase in the odds for wound infection. It is known that hematological disorders can be associated with significant complications after spinal surgery.29,30 Other related studies report that anemia by low preoperative hematocrit counts and perioperative blood transfusions significantly increase the incidence of SSIs.13,31–34 In a case report, Bolan et al demonstrated the utility of controlling bleeding through a multidisciplinary approach in a patient with significant congenital coagulopathy.29 This analysis suggested that improved preoperative hematological examinations should be taken to prevent additional morbidity seen in patients with hematological disorders. Future management plans for these patients might include a more thorough laboratory evaluation and the input from multiple stakeholders with varied but complimentary experiences, such as surgeons, hematologists, anesthesiologists, as well as from the patient.
Few studies exist comparing the rate of wound complications for anterior versus posterior spinal fusion, and many of these studies offer conflicting views. In a prior study, Pradhan et al reviewed 122 patients who underwent single-level lumbar spine fusion and found that there was no statistical significance between surgical approaches to fusion.35 In another study, Memtsoudis et al examined 261 356 patients from the National Inpatient Sample database who underwent thoracolumbar spinal fusion, and they found that anterior and anterior-posterior fusions were significantly associated with higher rates of complications than posterior fusions.22 The current analysis demonstrated that posterior arthrodesis was associated with a 1.8-fold increased risk for postoperative wound complications (P = .010). The advantages of an anterior approach are the increased surface area available for fusion, avoidance of damage to the posterior supporting muscles and ligaments, and direct restoration of intervertebral disc space.35–37 It may be that formation of a dead space due to muscle dissection following posterior spinal fusion predisposes patients to infection more so than anterior fusion.
The overall incidence of wound complications was lower than the reported 3.5% observed in a similarly structured NSQIP study on pediatric patients.16 Since increasing age has been previously reported as a predictor for postoperative complications,38 a higher rate of wound infection was expected. However, it is important to consider that the incidence varied from 2.0% to 4.1% within the NSQIP database for adults, and the pediatric article reported data from a single year. This range can be attributed to the relatively low number of cases being reported prior to 2013, with fewer than 500 cases of ASD in earlier years. Additionally, the incidence has been trending downward, which may be another reason the rates were lower. Although not entirely clear, this trend may be the result of recent changes in the use of antibiotics (eg, intrawound vancomycin powder) and stricter adherence to Surgical Care Improvement Project guidelines to treat infection.39,40
There are several limitations to this study. An important limitation to consider is that academic medical centers are overrepresented in the NSQIP database.41,42 These hospitals are motivated to improve the quality of surgical care and thus the hospitals participating in this database are not a random sample from the United States. Another limitation of this study is that the observation period for morbidity is limited to 30 days after surgery. Therefore, this study’s estimations likely underrepresent the actual profile for complications in this population. Finally, most patients in the NSQIP database have a high percentage of missing preoperative laboratory data. These additional variables, such as albumin and hematocrit measurements, could not be included in this analysis without significantly reducing the power of this study.
Despite these limitations, this is one of the largest studies examining risk factors for postoperative wound complication after spinal deformity surgery in adults. The risks for postoperative complications after surgery for ASD are multifactorial. Using multivariate logistic regression analysis, this study identified both preoperative and intraoperative risk factors for postoperative wound complication. Such information might improve surgical planning strategies to reduce postoperative complications in adults.
Footnotes
Authors’ Note: This study was qualified as exempt by the Mount Sinai Hospital Institutional Review Board. The article does not contain information about medical device(s)/drug(s).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Youssef JA, Orndorff DO, Patty CA, et al. Current status of adult spinal deformity. Global Spine J. 2013;3:51–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976). 2005;30:1082–1085. [DOI] [PubMed] [Google Scholar]
- 3. Cowan JA, Jr, Dimick JB, Wainess R, Upchurch GR, Jr, Chandler WF, La Marca F. Changes in the utilization of spinal fusion in the United States. Neurosurgery. 2006;59:15–20. [DOI] [PubMed] [Google Scholar]
- 4. Paulus MC, Kalantar SB, Radcliff K. Cost and value of spinal deformity surgery. Spine (Phila Pa 1976). 2014;39:388–393. [DOI] [PubMed] [Google Scholar]
- 5. Meng F, Cao J, Meng X. Risk factors for surgical site infection following pediatric spinal deformity surgery: a systematic review and meta-analysis. Childs Nerv Syst. 2015;31:521–527. [DOI] [PubMed] [Google Scholar]
- 6. Ramo BA, Roberts DW, Tuason D, et al. Surgical site infections after posterior spinal fusion for neuromuscular scoliosis: a thirty-year experience at a single institution. J Bone Joint Surg Am. 2014;96:2038–2048. [DOI] [PubMed] [Google Scholar]
- 7. Lonstein J, Winter R, Moe J, Gaines D. Wound infection with Harrington instrumentation and spine fusion for scoliosis. Clin Orthop Relat Res. 1973;(96):222–233. [PubMed] [Google Scholar]
- 8. Malamo-Lada H, Zarkotou O, Nikolaides N, Kanellopoulou M, Demetriades D. Wound infections following posterior spinal instrumentation for paralytic scoliosis. Clin Microbiol Infect. 1999;5:135–139. [DOI] [PubMed] [Google Scholar]
- 9. Lawson EH, Hall BL, Louie R, et al. Association between occurrence of a postoperative complication and readmission: implications for quality improvement and cost savings. Ann Surg. 2013;258:10–18. [DOI] [PubMed] [Google Scholar]
- 10. Calderone RR, Garland DE, Capen DA, Oster H. Cost of medical care for postoperative spinal infections. Orthop Clin North Am. 1996;27:171–182. [PubMed] [Google Scholar]
- 11. Schairer WW, Carrer A, Deviren V, et al. Hospital readmission after spine fusion for adult spinal deformity. Spine (Phila Pa 1976). 2013;38:1681–1689. [DOI] [PubMed] [Google Scholar]
- 12. Pull ter Gunne AF, van Laarhoven CJ, Cohen DB. Incidence of surgical site infection following adult spinal deformity surgery: an analysis of patient risk. Eur Spine J. 2010;19:982–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Veeravagu A, Patil CG, Lad SP, Boakye M. Risk factors for postoperative spinal wound infections after spinal decompression and fusion surgeries. Spine (Phila Pa 1976). 2009;34:1869–1872. [DOI] [PubMed] [Google Scholar]
- 14. Weinstein MA, McCabe JP, Cammisa FP., Jr Postoperative spinal wound infection: a review of 2,391 consecutive index procedures. J Spinal Disord. 2000;13:422–426. [DOI] [PubMed] [Google Scholar]
- 15. Schoenfeld AJ, Carey PA, Cleveland AW, 3rd, Bader JO, Bono CM. Patient factors, comorbidities, and surgical characteristics that increase mortality and complication risk after spinal arthrodesis: a prognostic study based on 5,887 patients. Spine J. 2013;13:1171–1179. [DOI] [PubMed] [Google Scholar]
- 16. Martin CT, Pugely AJ, Gao Y, Ilgenfritz RM, Weinstein SL. Incidence and risk factors for early wound complications after spinal arthrodesis in children: analysis of 30-day follow-up data from the ACS-NSQIP. Spine (Phila Pa 1976). 2014;39:1463–1470. [DOI] [PubMed] [Google Scholar]
- 17. American College of Surgeons. User guide for the 2012 ACS NSQIP Participant Use Data File. http://site.acsnsqip.org/wp-content/uploads/2013/10/ACSNSQIP.PUF_.UserGuide.2012.pdf. Accessed March 11, 2018.
- 18. Mackenzie WG, Matsumoto H, Williams BA, et al. Surgical site infection following spinal instrumentation for scoliosis: a multicenter analysis of rates, risk factors, and pathogens. J Bone Joint Surg Am. 2013;95:800–806. [DOI] [PubMed] [Google Scholar]
- 19. Tang H, Zhu J, Ji F, Wang S, Xie Y, Fei H. Risk factors for postoperative complication after spinal fusion and instrumentation in degenerative lumbar scoliosis patients. J Orthop Surg Res. 2014;9:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hodges SD, Humphreys SC, Eck JC, Covington LA, Kurzynske NG. Low postoperative infection rates with instrumented lumbar fusion. South Med J. 1998;91:1132–1136. [DOI] [PubMed] [Google Scholar]
- 21. Olsen MA, Nepple JJ, Riew KD, et al. Risk factors for surgical site infection following orthopaedic spinal operations. J Bone Joint Surg Am. 2008;90:62–69. [DOI] [PubMed] [Google Scholar]
- 22. Memtsoudis SG, Vougioukas VI, Ma Y, Gaber-Baylis LK, Girardi FP. Perioperative morbidity and mortality after anterior, posterior, and anterior/posterior spine fusion surgery. Spine (Phila Pa 1976). 2011;36:1867–1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chaudhary SB, Vives MJ, Basra SK, Reiter MF. Postoperative spinal wound infections and postprocedural diskitis. J Spinal Cord Med. 2007;30:441–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Buerba RA, Fu MC, Gruskay JA, Long WD, 3rd, Grauer JN. Obese class III patients at significantly greater risk of multiple complications after lumbar surgery: an analysis of 10,387 patients in the ACS NSQIP database. Spine J. 2014;14:2008–2018. [DOI] [PubMed] [Google Scholar]
- 25. Soroceanu A, Burton DC, Diebo BG, et al. Impact of obesity on complications, infection, and patient-reported outcomes in adult spinal deformity surgery [published online July 31, 2015]. J Neurosurg Spine. doi:10.3171/2015.3.SPINE14743. [DOI] [PubMed] [Google Scholar]
- 26. Djurasovic M, Bratcher KR, Glassman SD, Dimar JR, Carreon LY. The effect of obesity on clinical outcomes after lumbar fusion. Spine (Phila Pa 1976). 2008;33:1789–1792. [DOI] [PubMed] [Google Scholar]
- 27. Koutsoumbelis S, Hughes AP, Girardi FP, et al. Risk factors for postoperative infection following posterior lumbar instrumented arthrodesis. J Bone Joint Surg Am. 2011;93:1627–1633. [DOI] [PubMed] [Google Scholar]
- 28. Mehta AI, Babu R, Karikari IO, et al. 2012 Young Investigator Award winner: The distribution of body mass as a significant risk factor for lumbar spinal fusion postoperative infections. Spine (Phila Pa 1976). 2012;37:1652–1656. [DOI] [PubMed] [Google Scholar]
- 29. Bolan CD, Rick ME, Polly DW., Jr Transfusion medicine management for reconstructive spinal repair in a patient with von Willebrand’s disease and a history of heavy surgical bleeding. Spine (Phila Pa 1976). 2001;26:E552–E556. [DOI] [PubMed] [Google Scholar]
- 30. Emori M, Takebayashi T, Imoto K, Ueno S, Mizuno S, Yamashita T. Spinal surgery in a patient with essential thrombocythemia resulting in leg paraplegia: a case report. Spine J. 2013;13:e7–e10. [DOI] [PubMed] [Google Scholar]
- 31. Dunne JR, Malone D, Tracy JK, Gannon C, Napolitano LM. Perioperative anemia: an independent risk factor for infection, mortality, and resource utilization in surgery. J Surg Res. 2002;102:237–244. [DOI] [PubMed] [Google Scholar]
- 32. Malone DL, Genuit T, Tracy JK, Gannon C, Napolitano LM. Surgical site infections: reanalysis of risk factors. J Surg Res. 2002;103:89–95. [DOI] [PubMed] [Google Scholar]
- 33. Calamy G, Mille C. The role of transfusions in post-operative cytomegalovirus infections (in non-immunosuppressed subjects). Rev Fr Transfus Immunohematol. 1984;27:355–364. [DOI] [PubMed] [Google Scholar]
- 34. Weber EW, Slappendel R, Prins MH, van der Schaaf DB, Durieux ME, Strumper D. Perioperative blood transfusions and delayed wound healing after hip replacement surgery: effects on duration of hospitalization. Anesth Analg. 2005;100:1416–1421. [DOI] [PubMed] [Google Scholar]
- 35. Pradhan BB, Nassar JA, Delamarter RB, Wang JC. Single-level lumbar spine fusion: a comparison of anterior and posterior approaches. J Spinal Disord Tech. 2002;15:355–361. [DOI] [PubMed] [Google Scholar]
- 36. Min JH, Jang JS, Lee SH. Comparison of anterior- and posterior-approach instrumented lumbar interbody fusion for spondylolisthesis. J Neurosurg Spine. 2007;7:21–26. [DOI] [PubMed] [Google Scholar]
- 37. Greenough CG, Taylor LJ, Fraser RD. Anterior lumbar fusion: results, assessment techniques and prognostic factors. Eur Spine J. 1994;3:225–230. [DOI] [PubMed] [Google Scholar]
- 38. Buerba RA, Giles E, Webb ML, Fu MC, Gvozdyev B, Grauer JN. Increased risk of complications after anterior cervical discectomy and fusion in the elderly: an analysis of 6253 patients in the American College of Surgeons National Surgical Quality Improvement Program database. Spine (Phila Pa 1976). 2014;39:2062–2069. [DOI] [PubMed] [Google Scholar]
- 39. Collins I, Wilson-MacDonald J, Chami G, et al. The diagnosis and management of infection following instrumented spinal fusion. Eur Spine J. 2008;17:445–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Munday GS, Deveaux P, Roberts H, Fry DE, Polk HC. Impact of implementation of the Surgical Care Improvement Project and future strategies for improving quality in surgery. Am J Surg. 2014;208:835–840. [DOI] [PubMed] [Google Scholar]
- 41. Schilling PL, Hallstrom BR, Birkmeyer JD, Carpenter JE. Prioritizing perioperative quality improvement in orthopaedic surgery. J Bone Joint Surg Am. 2010;92:1884–1889. [DOI] [PubMed] [Google Scholar]
- 42. Schoenfeld AJ, Ochoa LM, Bader JO, Belmont PJ., Jr Risk factors for immediate postoperative complications and mortality following spine surgery: a study of 3475 patients from the National Surgical Quality Improvement Program. J Bone Joint Surg Am. 2011;93:1577–1582. [DOI] [PubMed] [Google Scholar]


