Abstract
Study Design:
Narrative literature review.
Objective:
The numbers of low-energy cervical fractures seen in patients suffering from ankylosing spondylitis (also known as Bechterew disease) or diffuse idiopathic skeletal hyperostosis (also known as Forestier disease) have greatly increased over recent decades. These fractures tend to be particularly overlooked, leading to delayed diagnosis and secondary neurological deterioration. The aim of the present evaluation was to summarize current knowledge on cervical fractures in patients with ankylosing spinal disorders (ASDs).
Methods:
The literature was analyzed through an extensive PubMed search focusing on cervical fractures, especially with delayed diagnosis.
Results:
In ASDs, it was mainly the cervical spine that was found to be affected by fractures. Fifty percent of ASD patients had neurological deficits at admission, with a high probability of secondary deterioration due to an initially missed diagnosis. Multislice high-resolution imaging techniques should be the radiological standard of care if a vertebral fracture is suspected. Nevertheless, many of these spinal fractures are overlooked, leading to feared secondary deterioration of existing unstable fractures. Long posterior instrumentations were found to be the treatment of choice, followed by anterior and combined anterior-posterior instrumentations.
Conclusions:
Delayed diagnosis of cervical fractures in ASDs contributes to initially misinterpreted clinical symptoms, inadequate imaging techniques, and a lack of knowledge about this disease entity due to its peculiarities. Thorough assessment of the patients’ neurological morbidity at admission might reduce the occurrence of the associated fractures. The biomechanical behavior of ASD fractures is completely different from that of non-ASD fractures, so that the treatment strategy for these patients should be at least surgical, in combination with long dorsal instrumentations or combined anterior-posterior approaches.
Keywords: ankylosing spinal disorders, ankylosing spondylitis, diffuse idiopathic skeletal hyperostosis, cervical fractures
Introduction
Ankylosing spinal disorders (ASDs) lead to progressive ossification of the spinal column.1 These ossifications entail bridging bone formations (syndesmophytes) in the spinal segments involved, with a high susceptibility to trauma even after low-energy impacts.1–5 This is a result of long ankylosed lever arms combined with a reduced capability for deformation, resulting in unstable spinal fractures, especially in the lower cervical segments.6,7 The most common entities involved in ASDs are ankylosing spondylitis (AS; also known as Bechterew disease) and diffuse idiopathic skeletal hyperostosis (DISH; also known as Forestier disease). These 2 types share essential clinical features. The current prevalence of DISH is estimated at between 2.9% and 25%. The prevalence of DISH peaks in the 60- to 69-year-old age group and rises progressively with increasing age.8–10 Interestingly, DISH tends to be more common in men, although the etiology of the condition is still unknown.8–11 There may be a strong association with obesity, type 2 diabetes mellitus, and higher age, as described in the literature (Table 1).12,13 Despite the increasing number of DISH cases, as a result of its association with traits involved in the modern Western affluent lifestyle, the prevalence of AS is still stable at 0.% to –1.4% and it mainly affects males.1 In contrast to AS, DISH is regarded as a noninflammatory disorder in which the spinal longitudinal ligaments and entheses slowly develop ossification over time in the segments involved, ultimately ending in complete rigid ankylosis.14 The diagnosis of DISH is established when bridged ossification of the anterior longitudinal ligament is present over at least 4 consecutive segments on conventional radiography. It was first defined as “senile ankylosing hyperostosis of the spine” by Forestier and Rotes-Querol.15,16 A progressive chronic inflammatory component is assumed to be the cause of Bechterew disease. The clinical characteristics of the disease consist of progressive stiffness, combined with pain as a result of advanced inflammation of the spinal and sacroiliac joints, occurring approximately around the 25th year of life.17 Complex interactions between genetic (HLA-B27) and environmental factors are involved in the etiology of the disease, but it continues to be one of the most puzzling mysteries among the rheumatic disorders.18–21 Due to improvements in the medical treatment available for AS and DISH, associated with increased life expectancy, the incidence of complicated spinal fractures among these patients can be expected to rise dramatically during the coming decades.2,7 The cervical spine is the region that is most susceptible to these fractures.2–4,22 The reason for this may be the hypermobility of the cervical spine in combination with the weight of the skull, small vertebral bodies, and the position of the cervical facet joints.23,24 In addition, patients suffering from AS frequently present with concomitant osteoporosis, especially in the early stages of the disease.20,25–27 There is also often a delay in the diagnosis of cervical spine fractures as a result of initially mild symptoms and the use of standard fluoroscopic imaging.2,10,20,21,26,28,29 Finally, delayed diagnosis of cervical fractures may lead to severe secondary deterioration as a result of unstable spine fractures.30–33 The analysis of the literature presented here reports on cervical spine fractures in ASD, their diagnosis, neurological symptoms, and therapy, as well as complications and mortality.
Table 1.
Differences Between Ankylosing Spondylitis and Diffuse Idiopathic Hyperostosis in Relation to Prevalence, Age, Etiology, and Diagnosis.
| Ankylosing Spondylitis | Diffuse Idiopathic Hyperostosis | |
|---|---|---|
| Prevalence | 0.1% to 1.4%1 | Estimated at between 2.9% and 25%8–10 |
| Age | Onset in second and third decades of life1 | Peak between 60 and 69 years8 |
| Etiology | Inflammatory rheumatic disorder, genetic interaction (HLA-B27), environmental factors18–21 | Associations with obesity, type 2 diabetes mellitus, and advanced age, noninflammatory12,13 |
| Diagnosis | Inflammatory changes confirmed by imaging (magnetic resonance imaging, radiography) (typically sacroiliac joints, axial spine, ie, “bamboo spine,” enthesitis) and clinical symptoms (morning stiffness, back/buttock pain), elevated inflammatory parameters, acute anterior uveitis92–94 | Bridged ossification of the anterior longitudinal ligament over at least 4 consecutive segments on conventional radiography15,16 |
Methods
The authors performed a narrative literature review based on an extensive PubMed search. Three authors searched independently, using the following key words with the “advanced” searching option in PubMed without limit, based on the publication year: (ankylosing spondylitis (Title)) OR (ankylosing spinal disorders) OR (diffuse skeletal hyperostosis) OR (bechterew’s disease) OR (forestier’s disease) AND (cervical) AND (spine) AND (spinal fractures) AND (trauma) AND (spinal) AND (injury) AND (injuries). All studies published in English with full-text availability were considered for inclusion. A total of 241 articles were found (230 records identified through PubMed and 11 records manually added after screening of reference lists). The articles collected were screened initially for relevance by title and abstract (182 articles excluded). After all appropriate articles had been compiled, 59 articles were checked by the authors (Figure 1). Thirty articles were not appropriate for inclusion due to inappropriate language, lack of full-text availability, and missing information according to our inclusion criteria and were therefor rejected. A total of 29 articles were included in the narrative literature review presented (Table 2). The majority of the reviewed articles are evidence level “3” and “4” (case-control studies, retrospective comparative studies, case series). The information presented focuses on the following results in summarized form:
Figure 1.
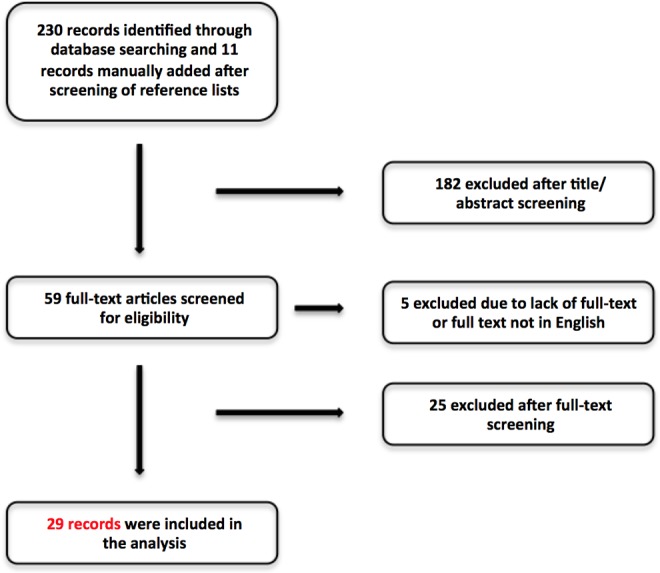
Flow chart for the literature search and study selection.
Table 2.
Important Studies Identified in the Literature Review Relative to the Numbers of Patients Treated, Treatment Option, Summarized Results, and Delayed Diagnosis of Ankylosing Spondylitis (AS) and Diffuse Idiopathic Skeletal Hyperostosis (DISH) (Oxford Centre for Evidence-Based Medicine; Available at http://www.cebm.net).
| First Author, Reference | Year | Study Location | Level of Evidence | Study Design | Disease Entity | Number Of Patients With Fractures | Treatment | Results |
|---|---|---|---|---|---|---|---|---|
| Lukasiewicz22 | 2016 | USA | 3 | Retrospective cohort study | AS | 498 patients with cervical spine fractures | Surgery and conservative treatment | Spinal cord injury in 21% of patients; 13% of patients had fractures in more than one region of the spine; 29% adverse events (urinary tract infections, intubation, pneumonia), 6.6% of patients died during their inpatient stay; high morbidity and mortality of fractures in the ankylosed spine |
| Ma68 | 2015 | China | 3 | Retrospective study | AS | 25 patients with cervical spine fractures | Anterior-only stabilization (6); posterior-only stabilization (9); combined posterior-anterior or anterior-posterior stabilization (10); median segments of fixation 4 | Surgical treatment advocated, highly unstable cervical spine fractures; looseness or migration of internal fixation was not observe; 14 patients with complications (one death) |
| Robinson78 | 2015 | Sweden | 3 | National registry cohort study | AS | 534 cervical spine fractures (in 990 patients with 1131 fractures) | 381 surgery; 153 conservative treatment | Clear beneficial effect on survival of AS spinal fractures if treated surgically (long posterior fixation of at least 3 levels above and below the fracture is recommended); spinal cord injury threatened the survival of patients |
| Xiang72 | 2015 | China | 3 | Retrospective study | AS | 11 patients with cervical spine fractures | Anterior-posterior stabilization of all fractures | No treatment-related injury to the spinal cord, nerve roots, or vessels; no wound infection; primary intention; fracture healing generally required 4-6 months without loosening, no pull-out or collapse of the bone graft, no loosening or breaking of the internal fixators, no pseudarthrosis, or other complications; combination of anterior-posterior approaches seems to be feasible |
| Schiefer51 | 2015 | USA | 3 | Retrospective review | DISH and AS | 36 (39%) cervical spine fractures (of 92 fractures in 81 patients with DISH (42%) or AS (58%) | Percutaneous instrumentation (21.7%), posterior instrumented fusion (51.1%) with or without decompression, circumferential decompression and fusion (4.4%), or anterior decompression and fusion (6.6%); remaining patients treated with primary external immobilization | Instrumentation over a median of 7 levels; approximately the half of initial conservative treated patients required surgery; neurologic deterioration after presentation in 7 patients (8.6%); 5 of these deteriorated after surgical treatment, 7.6% surgical risk; ASIA grade and patient age predictors of poor outcome at 1 year (P < .001); delayed diagnosis in 20% (19) of the patient cohort (median delay of 8 days) |
| Prieto-Alhambra6 | 2014 | Denmark | 3 | Case-control study | AS | 139 patients with fracture vs 271 controls (age- and gender-matched controls) | Not stated | Fivefold higher risk of spine fracture for AS patients, peak 2.5 years following diagnosis |
| Westerveld10 | 2014 | Netherlands | 3 | Retrospective cohort study | AS and DISH | 14 patients with AS, 40 patients with DISH; 111 patients in control group | Surgical treatment in 8 AS patients, 21 DISH patients, 39 control patients; total of 68 patients with surgery | Unstable fractures in AS and DISH; complication rate higher in ASD compared to controls; age and presence of DISH predictors of mortality after a spinal fracture |
| Gilard31 | 2014 | France | 4 | Retrospective cases series | AS | 7 patients with cervical spine fracture or luxation | All surgical | Mean of 13 days’ delay between trauma and admission; cervical spine fracture in AS with high instability; early surgical treatment due to the risk of secondary neurological deterioration; CT should be the gold standard for exploration of these patients |
| Mathews43 | 2013 | USA | 4 | Retrospective cases series | AS | 6 patients with cervical spine fractures (11 patients) | 1 patient posterior instrumentation; 1 patient combined anterior-posterior instrumentation (with discectomy); 1 patient laminectomy with posterior instrumentation; 3 patients conservative treatment | No deaths, more nonneurological complications in surgically treated patients (urinary tract infection, pneumonia, cardiac complications) |
| Hong 63 | 2013 | China | 3 | Retrospective study | AS | 8 patients with cervical spine fractures | 5 patients anterior instrumentation; 1 patient posterior instrumentation; 1 patient anterior–posterior instrumentation | High rate of neurological deficits; surgery should be performed as early as possible |
| Bransford42 | 2012 | USA | 3 | Retrospective study | DISH | 33 patients with cervical spine fractures | 16 patients anterior instrumentation, 12 patients posterior instrumentation, 5 patients anterior-posterior instrumentation | Average time to diagnosis 2 days; significant experience of neurological injuries of fractures through the disc space (lower ASIA scale), average number of instrumented vertebral bodies 3.6; 5 (15%) patients required reoperation: 2 wound infections (posterior), 1 anterior screw displacement, 1 anterior revision due to unsatisfied reduction, 1 construct failure in a 1-level corpectomy; significant association with lower preoperative neurological status and postoperative complications; mortality of 27% (9 patients; all with neurological deficits; 23 days postinjury) |
| Backhaus32 | 2011 | Germany | 3 | Retrospective study | AS | 51 patients with 51 cervical fractures | 31 patients anterior instrumentation, 8 patients posterior instrumentation, 12 patients anterior-posterior instrumentation | Early diagnosis of spine fractures with conventional radiographs and CT for adequate treatment; severe neurological complications after dislocation of the fracture; underdiagnosed or underestimated fractures in AS |
| Caron3 | 2010 | USA | 3 | Retrospective study | AS and DISH | 112 patients with a total of 67 cervical spine fractures (28 AS patients and 39 DISH patients with cervical spine fractures) | 75 patients treated surgically, 37 patients treated with bracing | Majority cervical spine fractures (67 patients; 55%); median time interval from admission to surgical intervention 2 days; most common surgical treatment posterior segmental fixation with at least 3 bilateral points of fixation above and below; higher likelihood of delay in diagnosis and to be treated surgically in AS patients; age and cardiac disease major predictors of mortality; 84% patients with at least 1 complication (pulmonary problem, urinary tract infection) |
| Sapkas5 | 2009 | Greece | 4 | Not stated | AS | 7 patients with cervical spine fractures | 4 patients posterior stabilization; 3 anterior-posterior stabilization | Spinal fusion in all cases; 100% fusion rate; no intraoperative complications; after surgery, improvement of all patients’ neurological status; loosening of posterior screws without loss of stability in 2 patients; Philadelphia-type cervical collar in all patients postoperatively for 3 to 6 months |
| Vives86 | 2008 | USA | 4 | Case report | AS | 1 patient with a C7 fracture | Laminectomy without instrumented fusion followed by a cervicothoracic orthosis postoperatively | Progressive weakness over the course of 2-3 hours after admission; spinal cord injury at the C5 level; premedication of clopidogrel (Plavix); C5 and C6 lamina and spinous process fractures with a large epidural hematoma extending from the C3-C7 levels; hematoma evacuation through a laminectomy of C3-C7 without instrumented fusion; use of cervicothoracic orthosis postoperatively; excellent recovery after 18 months without malalignment; presence of syringomyelia on follow-up images |
| Einsiedel20 | 2006 | Germany | 3 | Retrospective study | AS | 37 patients with cervical spine fractures | Anterior-only instrumentation (10); single-session anterior-posterior instrumentation (11); 2-session anterior-posterior instrumentation (13); uninstrumented laminectomy (1); no radiologically detected fracture); posterior-only instrumentation (2) | Preoperative neurological deficits in 36 patients; 13 patients with delayed diagnosis and more severe neurological deficits and less postoperative improvement compared to prompt diagnosis; 5 patients with early implant failures (all required revision surgery, initially anterior-only instrumentation); 3 deaths due to respiratory distress syndrome (rigid thorax) or cerebral ischemia (rupture of the vertebral arteries); recommendation for anterior decompression and fusion with posterior instrumentation (1- or 2-stage) |
| Payer71 | 2006 | Switzerland | 4 | Case series | AS | 4 patients with cervical fractures | Combined anterior-posterior instrumentation | Combined anterior-posterior instrumentation of 1 patient after progressive deformity with initial treatment of a halo fixator; combined approach in 1 patient after early redislocation of an anterior monosegmental fixation; 2 patients operated on primarily using the combined approach; good postoperative alignment and stability and no dislocation or deformity during a mean observation period of 11 months with the use of the anterior-posterior approach |
| Zdichavsky4 | 2005 | Germany | 3 | Retrospective study | AS | 32 patients with 19 cervical spine fractures | Anterior-only instrumentation (9); posterior-only instrumentation (2); posterior-anterior instrumentation (6); conservative (2) | 8 of 17 patients with cervical spine fractures initially treated conservatively were operated on secondarily due to insufficient repositioning (1), instability/fracture dislocation (4), or neurological deterioration (2); banal traumas mostly associated with fractures at the C5/6 and C6/7 levels; anterior-posterior instrumentation better for mobilization and avoiding complications |
| Cornefjord75 | 2005 | Sweden | 3 | Retrospective chart review | AS | 19 patients with cervical fractures | Posterior instrumentation (15); anterior-posterior instrumentation (4) | 11 patients without neurological deficits preoperatively; 8 patients with neurological deficits preoperatively—improvement of 2 patients postoperatively during their hospital stay, others remained unchanged; no signs of disturbed healing, nonunions or loosening of implants using plain radiographs |
| Lange66 | 2005 | Germany | 4 | Case series | AS | 2 patients with cervical spine fractures | 1 patient posterior instrumentation; 1 patient anterior instrumentation; both patients secondary combined posterior-anterior instrumentation due to secondary fracture dislocation | Neurological deficit in 1 patient before the initial treatment, with complete recovery after the first treatment postoperatively (anterior-only); second patient without neurological deficit before the dorsal instrumentation—due to fracture dislocation, a second anterior instrumentation was carried out; after combined instrumentation, no dislocation and uneventful healing in both cases |
| El Masry76 | 2004 | UK | 4 | Case report | AS | 1 patient with C7 fracture | Anterior-posterior instrumentation (vertebrectomy) | No neurological deficit at admission; displaced fracture and running through the right lamina of C7 vertebra; initially hard collar; combined anterior-posterior instrumentation with vertebrectomy; mobilization (2 days after surgery) and Philadelphia collar (for 12 weeks) postoperatively; regular clinical and radiological follow-up; maintenance of anatomical reduction and solid fusion with no shift or breakage of the instrumentation 4-year postoperatively |
| Moreau73 | 2003 | UK | 4 | Case series | AS | 2 patients with cervical spine fractures (one patient with accompanying lumbar fracture) | Anterior-posterior instrumentation (1); anterior instrumentation (1) | 1 patient with sensory level of T4 and paraplegia of lower extremities (anterior instrumentation); second patient without motor weakness but accompanying lumbar fracture (anterior-posterior instrumentation) |
| Schröder91 | 2003 | Germany | 4 | Case series | AS | 3 patients with cervical fractures | Halo treatment | 2 pin-track infections and pin protrusion through the skull, with one case of intracerebral hemorrhage and craniotomy; local revision in the second patient |
| Einsiedel56 | 2001 | Germany | 4 | Retrospective case series | AS | 12 patients with cervical spine fractures | All surgical | 12 patients with cervical fractures, 11 with preoperative neurological deficits; all patients underwent surgery (posterior-anterior instrumentation, anterior stabilization, laminectomy); 5 patients improved after surgery; in 5 patients, the neurological deficits disappeared after surgery; 2 patients died (acute respiratory distress syndrome and cerebral ischemia); 1 patient with revision surgery due to implant dislocation |
| Taggard77 | 2000 | USA | 4 | Not stated | AS | 7 patients with cervical spine fractures | Posterior instrumentation | 7 patients suffering from AS with cervical fractures; 4 patients were neurologically intact; 3 had quadriparesis; 1 with quadriparesis; all patients treated with posterior stabilization; 4 patients within 2 weeks, 3 patients after failed conservative treatment; no patients with postoperative deterioration; no perioperative complications, 2 patients died of nonsurgical complications during the follow-up |
| Wu80 | 1998 | Taiwan | 4 | Case report | AS | 1 patient with a C6 fracture | Laminectomy followed by a halo vest fixation | 1 patient with a C6 fracture and a spinal epidural hematoma developed progressive weakness and numbness below C5; laminectomy and hematoma evacuation was performed; neurological function improved after surgery |
| Olerud41 | 1996 | Sweden | 4 | Not stated | AS | 19 patients with cervical fractures | 17 patients with anterior or posterior instrumentation, 2 patients with conservative treatment | 19 patients with cervical spine fractures, 17 treated surgically with posterior and anterior approaches, 2 patients received halo treatment |
| Detwiler90 | 1990 | USA | 3 | Retrospective study | AS | 11 patients cervical fractures | 8 posterior instrumentations with and without decompression | 11 patients with cervical spine fractures; all patients initially treated with traction (1 patient with Philadelphia collar); 3 patients died shortly after injury; 8 patients underwent posterior instrumentation; improvement of all neurological deficits in 2 patients; none of the patients deteriorated after surgical treatment |
| Broom81 | 1988 | USA | 4 | Case series | AS | 5 patients with cervical fractures (4 with delayed diagnosis) | Not stated | 5 patients with cervical spine fractures; all developed delayed neurological complications ranging from 2 to 35 days; the diagnosis of the cervical fracture was delayed in 4 patients |
Abbreviations: ASIA, American Spinal Injury Association; CT, computed tomography.
Cervical spine fractures in ASD
Delayed diagnosis of cervical fractures in ASD
Surgical therapy of cervical spine fractures
Complications
Mortality
Cervical Spine Fractures in ASD
The characteristic feature in both AS and DISH is progressive ankylosing of the spinal segments involved. Inevitably, an ankylosed spine reacts differently to spinal trauma than a healthy one. The prevalence figures for vertebral fractures and osteoporosis in patients with AS are reported in the literature to be approximately 10% to 30% and 20% to 60%, respectively.34–39 The cervical spine in particular is prone to fractures, and more than 50% of AS and DISH patients present with fractures of the cervical spine.2,22 In addition to the frequently reduced bone mineral density in these patients, there is controversy over whether AS is also associated with increased bony formations due to ankylosing joints and syndesmophytes in the more advanced stages of the disease.35 Osteoporosis appears to be associated with AS activity, but spinal fractures appear to be more related to the duration and severity of AS rather than bone mineral density.36 In contrast to AS, there is still a lack of information on coexisting osteoporosis in patients with DISH. Nevertheless, some investigators have reported a possible relationship between DISH and a greater risk of vertebral fractures.14 Patients with both AS and DISH are considered to be highly susceptible to cervical spine fractures resulting from low-energy impacts.2–5,22 These fractures tend to be unstable and may lead to secondary deterioration after initially mild symptoms, often as a result of displacement.2,33,40,41 An initial presentation with mild symptoms may mask severe cervical fractures, leading to delayed diagnosis. The mechanism of injury commonly involves a fall from standing or sitting positions, with hyperextension of the cervical spine, but injury can also occur merely after rotating the head.3–5,42,43 According to Caron et al, cervical fractures in ASDs can be classified into disc injuries (type I), body injuries (type II), anterior body or posterior disc injuries (type III), and anterior disc or posterior body injuries (type IV).3 The typical transverse fractures of the spine are known as “carrot stick fractures.”44 Due to the functional deprivation of the intervertebral disc (IVD) in patients suffering from AS, the IVD represents the weakest point in the spine in these patients, which may be the reason for the typical fracture location through the IVD.45 In contrast to AS, DISH fractures are prone to occur through the vertebral body.45,46 Calcifications, especially at the level of the IVD, combined with stress shielding due to load transfer through the calcified/ossified anterior ligaments, prevent fractures through the IVD by weakening the vertebral body and strengthening the IVD.45,46 In healthy individuals, increased forces lead to elastic distortion of the cervical spine until rupture of ligaments or fractures of the vertebrae occur. These compensatory mechanisms of elastic distortion in ASD patients fail much earlier due to a significantly decreased range of motion (ROM) as a result of ankylosed spinal segments. The lower cervical spine, especially levels C5-7, is highly susceptible to these low-energy fractures.3,20,42,47 The age range during which fractures develop is approximately 60 to 70 years, with a significantly higher age at onset for DISH, as stated in the review by Westerveld et al.2,3,20
Delayed Diagnosis of Cervical Fractures in ASD (Table 3)
Table 3.
Recent Literature on Ankylosing Spinal Disorders (ASDs) in Relation to Delayed Diagnosis, Second Neurological Presentation With Associated Postoperative Recovery, and Overall Mortality Rate.
| First Author, Reference | Type of Article | Delayed Diagnosis (Patients) | ASD | Second Neurological Presentation | Postoperative Recovery After Delayed Diagnosis | Overall Mortality |
|---|---|---|---|---|---|---|
| Einsiedel20 | Retrospective analysis; 2-center | 13 (35%) | AS | Severe deficits | Improvement less pronounced | ≈ 8% |
| Caron3 | Retrospective analysis | 21 (19%) | AS + DISH | Neurological deterioration in 17 patients (81%) | — | ≈23% (≈40% for delayed diagnosis) |
| Backhaus32 | Retrospective analysis | 18 (15%) (+13% diagnosed stable fracture with second dislocation) | AS | Secondary dislocation with neurological decline | — | ≈23% |
| Yeoh53 | Retrospective analysis | 2 (20%) | AS + DISH | Neurological deficits | No improvement | — |
| Westerveld2 | Literature review | 36 (9%) | AS + DISH | — | — | 18% (AS) and 20% (DISH) |
| Sapkas5 | Prospective analysis | ≈12 (60%) | AS | — | — | 0% |
| Anwar95 | Retrospective analysis | 15 (47%) | AS | Development of spinal cord injury (ASIA grade A + D) few days after injury | — | — |
Abbreviations: AS, ankylosing spondylitis; DISH, diffuse idiopathic skeletal hyperostosis; ASIA, American Spinal Injury Association.
The annual numbers of cervical spine fractures occurring due to AS have increased dramatically over the past 20 years.7 Improved diagnosis and greater awareness of spinal fractures, combined with increased levels of activity particularly in older patients as a result of modern medical therapy, provide a reasonable explanation for these increasing numbers.48 Despite the increase, the numbers of missed fractures are decreasing due to better visualization and the preference for computed tomography (CT) and magnetic resonance imaging (MRI) instead of conventional methods.49 In most of these cases, mild injury patterns result in a delayed diagnosis.2,3,20,33,50–52 Several studies have reported a delay in diagnosis among patients with AS and DISH, ranging from approximately 10% to 50% of the patients presenting.2,3,51,53 One possible explanation for the delayed diagnosis of cervical fractures might be the fact that minor trauma with only moderate pain is combined with insufficient radiodiagnostic examinations, in which osteoporosis and fractures in the cervicothoracic junction may be overlooked.54 In addition, the physiological anatomy of the spine is sometimes substantially altered in patients with ASD, so that even with advanced imaging techniques it can still be challenging to identify the fractured levels.55
Delayed diagnosis often leads to secondary deterioration, with an associated decline in neurological function.2,3,40,51 The initial lack of symptoms in patients with AS has been described as the “fatal pause” before neurologic deterioration occurs.56 The delay in diagnosis of cervical fractures in AS contributes to initial misinterpretation of the clinical symptoms by physicians (52%), as well as by patients (48%), and this was described as the “doctor’s and patient’s delay” in the review by Westerveld et al.2 In contrast to AS, patients with DISH did not misinterpret their symptoms, so that delayed diagnoses were only caused by doctors’ delays, as stated by Westerveld et al.2
The use of standard imaging alone is also insufficient, and advanced imaging techniques should be used if there is a strong suspicion of fracture.2,57,58 Due to the thin fracture lines, high-resolution multislice CT imaging is preferable as one of the most reliable tools for identifying the fractured levels.54,59–61 Since the risk of concomitant spinal cord injury in patients with AS is 10 times higher than in the healthy population, additional MRI scans are strongly recommended and should be available for all patients.5,22,43,62,63 Concomitant epidural hematomas, with bleeding from ruptured epidural veins or cancellous bone due to displacement of unstable fractures, can be adequately visualized or excluded using an MRI scan.64–66
In conclusion, suspected fractures justify the use of high-resolution imaging techniques for the entire spine, to evaluate concomitant injuries in other spinal regions and to avoid overlooking fractures with initially mild symptoms.22,55,67
Surgical Therapy for Cervical Spine Fractures
Ankylosed cervical spine segments result in long lever arms, with a 5-fold higher risk of clinical spine fractures in comparison to the normal population with spine fractures, as reported by Prieto-Alhambra et al.6 Particularly in patients with AS, this excessive increased risk peaks in the first 2.5 years after the onset of the disease. The combination of long lever arms with the comorbidity of osteoporosis indicates the problems faced in the surgical treatment of these patients using anterior, posterior, or combined procedures.26,68–71
Following the introduction of the anterior cervical approach by Smith and Robinson in the 1960s, the conventional discectomy was expanded into an anterior cervical corpectomy, including one or more cervical levels, in order to decompress the neural structures and accomplish fusion, or at least reconstruct the cervical spine using special cage systems. High rates of implant-related failures were observed with the use of anterior-only instrumentations. This can be explained by the accompanying fractures of the dorsal spine elements, which are characteristically transverse and often remain undetected, as mentioned above.20 Anterior-only instrumentation may then cause implant failures, so that circumferential instrumentation would be preferable.69,71–73 Due to the accompanying comorbidities in the patients affected (especially cardiovascular and pulmonary problems), a circumferential approach might lead to a high level of perioperative risk among the patients affected. If a circumferential approach is not feasible, a posterior-only approach should be considered.5,74
Most of the research groups identified in the literature search used a dorsal approach to treat patients with cervical fractures, but without accurate descriptions of the rationale behind this treatment strategy.2,10,41,51,75 However, several groups also used an anterior or combined anterior-posterior approach with satisfactory results, either planned after the index procedure or after implant failure.41,63,68,69,71–73,76
In conclusion, most of the patients described in the literature have been treated with multilevel posterior segmental fixation, using bilateral fixation points above and below the affected cervical levels.2,3,5,32,68,74,77 Surgical stabilization may also improve the survival among patients with spinal fractures related to AS.74,78 In patients with anterior cervical decompression, especially in corpectomy approaches, additional dorsal instrumentation is advocated in order to reduce implant-related complications.20 As reported in the literature, good neurological recovery is observed in many surgically treated patients.56,74,77–80
Complications
The complication rates for AS and DISH reported in the literature range from approximately 30% to 50%, with a trend toward increased complications due to DISH.2 One of the most feared complications is secondary deterioration due to an initially overlooked and delayed diagnosis of cervical fractures.2,3,20,33,40,43,81 The mortality rate among patients with surgically treated spine fractures in AS and DISH is reported in the literature to be approximately 18%. The higher mortality rate among trauma patients suffering from DISH, especially during the course of follow-up and regardless of the treatment option, may be explained by the etiology of the disease, associated with disorders of the metabolism, obesity, and advanced age.82–85
Finally, concomitant epidural hematomas, lacerations of the aorta (lower spine), and ruptures of the trachea in patients with AS have also been reported.64,65,80,86,87 In contrast to AS, cervical spine complications among DISH patients consist of myelopathy with spinal canal stenosis, dysphagia, and difficult endotracheal intubation when anesthesia is being administered.2,88,89
In general, the overall complication rate appears to be greater among conservatively treated patients.2 Most patients selected for conservative management have been treated with a cervical collar (DISH) or cervical traction devices (AS).3,90,91 The high proportion of brace therapy among DISH patients may possibly reflect the high incidence of thoracic fractures in this disease entity.2 In general, based on the published data, the overall morbidity and mortality appear to be greater among patients treated conservatively than among their surgical counterparts.2,91
Pneumonia and respiratory insufficiency, postoperative deep venous thrombosis, and wound infections are frequent postoperative complications among ASD patients.2,3,77 Pulmonary infections and associated respiratory insufficiency in particular lead to fatal outcomes in both disease entities.2,3,22
Mortality
The mortality associated with spine fractures among surgically treated patients with ASD is approximately 7% to 25%, based on our analysis of the literature.2,3,10,22,51,68,77 Regression analyses show that age, the presence of DISH, neurologic deficits, cardiac diseases, the number of additional comorbid conditions, and also a low-energy mechanism of injury are predictive of increased mortality.2,3,10 In particular, lacerations of the aorta or trachea and pneumonia with or without respiratory failure appear to be the severe complications mostly associated with fatal outcomes.2 For both entities (AS and DISH), pulmonary complications appear to be the most common cause of death. The mortality rate among surgically treated patients is reported to be lower than among those receiving conservative treatment.2
Conclusions
Ankylosing spinal disorders lead to progressive ossification of the spinal column, due to bridging bone formations in the spinal segments involved. An increased incidence of cervical spine fractures, particularly due to low-energy trauma, is observed among patients suffering from AS and DISH. This high susceptibility to trauma even after low-energy impacts may lead to a delay in the diagnosis of these fractures, contributing to initially misinterpreted clinical symptoms and inadequate imaging investigations, partly due to the lack of knowledge of the peculiarities of the disease. Secondary deterioration due to initially unstable fractures with neurologic compromise, associated with low recovery rates, is a frequent problem with these diseases. Thorough assessment of the patients’ neurological morbidity and additional radiography, MRI, and CT at admission should reduce the prevalence of overlooked fractures. The overall complication rate appears to be higher among conservatively treated patients. Conservative treatment usually involves cervical collars (DISH) or cervical traction devices (AS). In patients who receive surgical therapy after cervical spine fractures, a multisegmental posterior approach is preferable, followed by anterior instrumentation or circumferential approaches.
Key Points
There is an increased incidence of cervical spine fractures (after low-energy impacts) in patients suffering from AS and DISH.
There is a high risk of delayed diagnosis, with secondary deterioration due to unstable fractures.
Patients suffering from AS and DISH are at high risk of neurologic compromise, associated with low recovery rates.
If a fracture is only suspected, multislice high-resolution imaging techniques are advocated.
Posterior instrumentation or circumferential approaches are recommended, due to high failure rates with anterior-only fixations.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Braun J, Sieper J. Ankylosing spondylitis. Lancet. 2007;369:1379–1390. [DOI] [PubMed] [Google Scholar]
- 2. Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J. 2009;18:145–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Caron T, Bransford R, Nguyen Q, Agel J, Chapman J, Bellabarba C. Spine fractures in patients with ankylosing spinal disorders. Spine (Phila Pa 1976). 2010;35:E458–E264. [DOI] [PubMed] [Google Scholar]
- 4. Zdichavsky M, Blauth M, Knop C, Lange U, Krettek C, Bastian L. Ankylosing spondylitis. Therapy and complications of 34 spine fractures [in German]. Chirurg. 2005;76:967–975. [DOI] [PubMed] [Google Scholar]
- 5. Sapkas G, Kateros K, Papadakis SA, et al. Surgical outcome after spinal fractures in patients with ankylosing spondylitis. BMC Musculoskelet Disord. 2009;10:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Prieto-Alhambra D, Muñoz-Ortego J, De Vries F, et al. Ankylosing spondylitis confers substantially increased risk of clinical spine fractures: a nationwide case-control study. Osteoporos Int. 2015;26:85–91. [DOI] [PubMed] [Google Scholar]
- 7. Robinson Y, Sandén B, Olerud C. Increased occurrence of spinal fractures related to ankylosing spondylitis: a prospective 22-year cohort study in 17,764 patients from a national registry in Sweden. Patient Saf Surg. 2013;7(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kim SK, Choi BR, Kim C, et al. The prevalence of diffuse idiopathic skeletal hyperostosis in Korea. J Rheumatol. 2004;31:2032–2035. [PubMed] [Google Scholar]
- 9. Weinfeld RM, Olson PN, Maki DD, Griffiths HJ. The prevalence of diffuse idiopathic skeletal hyperostosis (DISH) in two large American Midwest metropolitan hospital populations. Skeletal Radiol. 1997;26:222–225. [DOI] [PubMed] [Google Scholar]
- 10. Westerveld LA, van Bemmel JC, Dhert WJ, Oner FC, Verlaan JJ. Clinical outcome after traumatic spinal fractures in patients with ankylosing spinal disorders compared with control patients. Spine J. 2014;14:729–740. [DOI] [PubMed] [Google Scholar]
- 11. Westerveld LA, van Ufford HM, Verlaan JJ, Oner FC. The prevalence of diffuse idiopathic skeletal hyperostosis in an outpatient population in the Netherlands. J Rheumatol. 2008;35:1635–1638. [PubMed] [Google Scholar]
- 12. Denko CW, Malemud CJ. Body mass index and blood glucose: correlations with serum insulin, growth hormone, and insulin-like growth factor-1 levels in patients with diffuse idiopathic skeletal hyperostosis (DISH). Rheumatol Int. 2006;26:292–297. [DOI] [PubMed] [Google Scholar]
- 13. Kiss C, Szilágyi M, Paksy A, Poór G. Risk factors for diffuse idiopathic skeletal hyperostosis: a case-control study. Rheumatology (Oxford). 2002;41:27–30. [DOI] [PubMed] [Google Scholar]
- 14. Belanger TA, Rowe DE. Diffuse idiopathic skeletal hyperostosis: musculoskeletal manifestations. J Am Acad Orthop Surg. 2001;9:258–267. [DOI] [PubMed] [Google Scholar]
- 15. Resnick D, Shaul SR, Robins JM. Diffuse idiopathic skeletal hyperostosis (DISH): Forestier’s disease with extraspinal manifestations. Radiology. 1975;115:513–524. [DOI] [PubMed] [Google Scholar]
- 16. Forestier J, Rotes-Querol J. Senile ankylosing hyperostosis of the spine. Ann Rheum Dis. 1950;9:321–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Feldtkeller E, Khan MA, van der Heijde D, van der Linden S, Braun J. Age at disease onset and diagnosis delay in HLA-B27 negative vs. positive patients with ankylosing spondylitis. Rheumatol Int. 2003;23:61–66. [DOI] [PubMed] [Google Scholar]
- 18. Kim TH, Uhm WS, Inman RD. Pathogenesis of ankylosing spondylitis and reactive arthritis. Curr Opin Rheumatol. 2005;17:400–405. [DOI] [PubMed] [Google Scholar]
- 19. Pham T. Pathophysiology of ankylosing spondylitis: what’s new? Joint Bone Spine. 2008;75:656–660. [DOI] [PubMed] [Google Scholar]
- 20. Einsiedel T, Schmelz A, Arand M, et al. Injuries of the cervical spine in patients with ankylosing spondylitis: experience at two trauma centers. J Neurosurg Spine. 2006;5:33–45. [DOI] [PubMed] [Google Scholar]
- 21. Yilmaz N, Pence S, Kepekçi Y, Geyikli I, Ozaslan J. Association of immune function with bone mineral density and biochemical markers of bone turnover in patients with ankylosing spondylitis. Int J Clin Pract. 2003;57:681–685. [PubMed] [Google Scholar]
- 22. Lukasiewicz AM, Bohl DD, Varthi AG, et al. Spinal fracture in patients with ankylosing spondylitis: cohort definition, distribution of injuries, and hospital outcomes. Spine (Phila Pa 1976). 2016;41:191–196. [DOI] [PubMed] [Google Scholar]
- 23. Winkelstein BA, Myers BS. The biomechanics of cervical spine injury and implications for injury prevention. Med Sci Sports Exerc. 1997;29(7 suppl):S246–S255. [DOI] [PubMed] [Google Scholar]
- 24. Secin FP, Poggi EJ, Luzuriaga F, Laffaye HA. Disabling injuries of the cervical spine in Argentine rugby over the last 20 years. Br J Sports Med. 1999;33:33–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bessant R, Keat A. How should clinicians manage osteoporosis in ankylosing spondylitis? J Rheumatol. 2002;29:1511–1519. [PubMed] [Google Scholar]
- 26. Donnelly S, Doyle DV, Denton A, Rolfe I, McCloskey EV, Spector TD. Bone mineral density and vertebral compression fracture rates in ankylosing spondylitis. Ann Rheum Dis. 1994;53:117–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hanson JA, Mirza S. Predisposition for spinal fracture in ankylosing spondylitis. AJR Am J Roentgenol. 2000;174:150. [DOI] [PubMed] [Google Scholar]
- 28. Hendrix RW, Melany M, Miller F, Rogers LF. Fracture of the spine in patients with ankylosis due to diffuse skeletal hyperostosis: clinical and imaging findings. AJR Am J Roentgenol. 1994;162:899–904. [DOI] [PubMed] [Google Scholar]
- 29. El Maghraoui A, Bensabbah R, Bahiri R, Bezza A, Guedira N, Hajjaj-Hassouni N. Cervical spine involvement in ankylosing spondylitis. Clin Rheumatol. 2003;22:94–98. [DOI] [PubMed] [Google Scholar]
- 30. Colterjohn NR, Bednar DA. Identifiable risk factors for secondary neurologic deterioration in the cervical spine-injured patient. Spine (Phila Pa 1976). 1995;20:2293–2297. [DOI] [PubMed] [Google Scholar]
- 31. Gilard V, Curey S, Derrey S, Perez A, Proust F. Cervical spine fractures in patients with ankylosing spondylitis: importance of early management. Neurochirurgie. 2014;60:239–243. [DOI] [PubMed] [Google Scholar]
- 32. Backhaus M, Citak M, Kälicke T, et al. Spine fractures in patients with ankylosing spondylitis: an analysis of 129 fractures after surgical treatment. Orthopade. 2011;40:917–920, 922–924. [DOI] [PubMed] [Google Scholar]
- 33. Finkelstein JA, Chapman JR, Mirza S. Occult vertebral fractures in ankylosing spondylitis. Spinal Cord. 1999;37:444–447. [DOI] [PubMed] [Google Scholar]
- 34. Jun JB, Joo KB, Her MY, et al. Femoral bone mineral density is associated with vertebral fractures in patients with ankylosing spondylitis: a cross-sectional study. J Rheumatol. 2006;33:1637–1641. [PubMed] [Google Scholar]
- 35. Davey-Ranasinghe N, Deodhar A. Osteoporosis and vertebral fractures in ankylosing spondylitis. Curr Opin Rheumatol. 2013;25:509–516. [DOI] [PubMed] [Google Scholar]
- 36. Ghozlani I, Ghazi M, Nouijai A, et al. Prevalence and risk factors of osteoporosis and vertebral fractures in patients with ankylosing spondylitis. Bone. 2009;44:772–776. [DOI] [PubMed] [Google Scholar]
- 37. Cooper C, Carbone L, Michet CJ, Atkinson EJ, O’Fallon WM, Melton LJ. Fracture risk in patients with ankylosing spondylitis: a population based study. J Rheumatol. 1994;21:1877–1882. [PubMed] [Google Scholar]
- 38. Klingberg E, Geijer M, Göthlin J, et al. Vertebral fractures in ankylosing spondylitis are associated with lower bone mineral density in both central and peripheral skeleton. J Rheumatol. 2012;39:1987–1995. [DOI] [PubMed] [Google Scholar]
- 39. van der Weijden MA, van der Horst-Bruinsma IE, van Denderen JC, Dijkmans BA, Heymans MW, Lems WF. High frequency of vertebral fractures in early spondylarthropathies. Osteoporos Int. 2012;23:1683–1690. [DOI] [PubMed] [Google Scholar]
- 40. Whang PG, Goldberg G, Lawrence JP, et al. The management of spinal injuries in patients with ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis: a comparison of treatment methods and clinical outcomes. J Spinal Disord Tech. 2009;22:77–85. [DOI] [PubMed] [Google Scholar]
- 41. Olerud C, Frost A, Bring J. Spinal fractures in patients with ankylosing spondylitis. Eur Spine J. 1996;5:51–55. [DOI] [PubMed] [Google Scholar]
- 42. Bransford RJ, Koller H, Caron T, Zenner J, Hitzl W, et al. Cervical spine trauma in diffuse idiopathic skeletal hyperostosis: injury characteristics and outcome with surgical treatment. Spine (Phila Pa 1976). 2012;37:1923–1932. [DOI] [PubMed] [Google Scholar]
- 43. Mathews M, Bolesta MJ. Treatment of spinal fractures in ankylosing spondylitis. Orthopedics. 2013;36:e1203–e1208. [DOI] [PubMed] [Google Scholar]
- 44. Huwart L, Amoretti N. CT- and fluoroscopy-guided percutaneous screw fixation of a “carrot-stick” spinal fracture in an elderly man with ankylosing spondylitis. Skeletal Radiol. 2013;42:1767–1773. [DOI] [PubMed] [Google Scholar]
- 45. Graham B, Van Peteghem PK. Fractures of the spine in ankylosing spondylitis. Diagnosis, treatment, and complications. Spine (Phila Pa 1976). 1989;14:803–807. [DOI] [PubMed] [Google Scholar]
- 46. Bobyn JD, Mortimer ES, Glassman AH, Engh CA, Miller JE, Brooks CE. Producing and avoiding stress shielding. Laboratory and clinical observations of noncemented total hip arthroplasty. Clin Orthop Relat Res. 1992;274:79–96. [PubMed] [Google Scholar]
- 47. An SB, Kim KN, Chin DK, Kim KS, Cho YE, Kuh SU. Surgical outcomes after traumatic vertebral fractures in patients with ankylosing spondylitis. J Korean Neurosurg Soc. 2014;56:108–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Carette S, Graham D, Little H, Rubenstein J, Rosen P. The natural disease course of ankylosing spondylitis. Arthritis Rheum. 1983;26:186–190. [DOI] [PubMed] [Google Scholar]
- 49. Heyde CE, Fakler JK, Hasenboehler E, et al. Pitfalls and complications in the treatment of cervical spine fractures in patients with ankylosing spondylitis. Patient Saf Surg. 2008;2:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Geusens P, Vosse D, van der Linden S. Osteoporosis and vertebral fractures in ankylosing spondylitis. Curr Opin Rheumatol. 2007;19:335–339. [DOI] [PubMed] [Google Scholar]
- 51. Schiefer TK, Milligan BD, Bracken CD, et al. In-hospital neurologic deterioration following fractures of the ankylosed spine: a single-institution experience. World Neurosurg. 2015;83:775–783. [DOI] [PubMed] [Google Scholar]
- 52. Metz-Stavenhagen P, Krebs S, Meier O. Cervical fractures in ankylosing spondylitis. Orthopade. 2001;30:925–931. [DOI] [PubMed] [Google Scholar]
- 53. Yeoh D, Moffatt T, Karmani S. Good outcomes of percutaneous fixation of spinal fractures in ankylosing spinal disorders. Injury. 2014;45:1534–1548. [DOI] [PubMed] [Google Scholar]
- 54. Tan E, Schweitzer ME, Vaccaro L, Spetell AC. Is computed tomography of nonvisualized C7-T1 cost-effective? J Spinal Disord. 1999;12:472–476. [PubMed] [Google Scholar]
- 55. Neugebauer R. Tissue-preserving ventral compression osteosynthesis of dens axis fractures using endoscopy and special instruments [in German]. Unfallchirurg. 1991;94:313–316. [PubMed] [Google Scholar]
- 56. Einsiedel T, Kleimann M, Nothofer W, Neugebauer R. Special considerations in therapy of injuries of the cervical spine in ankylosing spondylitis (Bechterew disease) [in German]. Unfallchirurg. 2001;104:1129–1133. [DOI] [PubMed] [Google Scholar]
- 57. Murray GC, Persellin RH. Cervical fracture complicating ankylosing spondylitis: a report of eight cases and review of the literature. Am J Med. 1981;70:1033–1041. [DOI] [PubMed] [Google Scholar]
- 58. Podolsky SM, Hoffman JR, Pietrafesa CA. Neurologic complications following immobilization of cervical spine fracture in a patient with ankylosing spondylitis. Ann Emerg Med. 1983;12:578–580. [DOI] [PubMed] [Google Scholar]
- 59. Harrop JS, Sharan A, Anderson G, et al. Failure of standard imaging to detect a cervical fracture in a patient with ankylosing spondylitis. Spine (Phila Pa 1976). 2005;30:E417–E419. [DOI] [PubMed] [Google Scholar]
- 60. Freemyer B, Knopp R, Piche J, Wales L, Williams J. Comparison of five-view and three-view cervical spine series in the evaluation of patients with cervical trauma. Ann Emerg Med. 1989;18:818–821. [DOI] [PubMed] [Google Scholar]
- 61. Mace SE. Emergency evaluation of cervical spine injuries: CT versus plain radiographs. Ann Emerg Med. 1985;14:973–975. [DOI] [PubMed] [Google Scholar]
- 62. Alaranta H, Luoto S, Konttinen YT. Traumatic spinal cord injury as a complication to ankylosing spondylitis. An extended report. Clin Exp Rheumatol. 2002;20:66–68. [PubMed] [Google Scholar]
- 63. Hong F, Ni JP. Retrospective study on the treatment of ankylosing spondylitis with cervical spine fracture: 8 cases report [in Chinese]. Zhongguo Gu Shang. 2013;26:508–511. [PubMed] [Google Scholar]
- 64. Thumbikat P, Hariharan RP, Ravichandran G, McClelland MR, Mathew KM. Spinal cord injury in patients with ankylosing spondylitis: a 10-year review. Spine (Phila Pa 1976). 2007;32:2989–2995. [DOI] [PubMed] [Google Scholar]
- 65. Aoki Y, Yamagata M, Ikeda Y, et al. Failure of conservative treatment for thoracic spine fracture in ankylosing spondylitis: delayed neurological deficit due to spinal epidural hematoma. Mod Rheumatol. 2013;23:1008–1012. [DOI] [PubMed] [Google Scholar]
- 66. Lange U, Pape HC, Bastian L, Krettek C. Operative management of cervical spine injuries in patients with Bechterew’s disease [in German]. Unfallchirurg. 2005;108:63–68. [DOI] [PubMed] [Google Scholar]
- 67. Hägglund G, Johnsson R, Strömqvist B. Spinal fractures in Bechterew’s disease. Injuries most likely underdiagnosed [in German]. Lakartidningen. 1993;90:364–366. [PubMed] [Google Scholar]
- 68. Ma J, Wang C, Zhou X, Zhou S, Jia L. Surgical therapy of cervical spine fracture in patients with ankylosing spondylitis. Medicine (Baltimore). 2015;94:e1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Lange U, Kluge A, Strunk J, Teichmann J, Bachmann G. Ankylosing spondylitis and bone mineral density: what is the ideal tool for measurement? Rheumatol Int. 2005;26:115–120. [DOI] [PubMed] [Google Scholar]
- 70. Ulu MA, Batmaz İ, Dilek B, Çevik R. Prevalence of osteoporosis and vertebral fractures and related factors in patients with ankylosing spondylitis. Chin Med J (Engl). 2014;127:2740–2747. [PubMed] [Google Scholar]
- 71. Payer M. Surgical management of cervical fractures in ankylosing spondylitis using a combined posterior-anterior approach. J Clin Neurosci. 2006;13:73–77. [DOI] [PubMed] [Google Scholar]
- 72. Xiang LB, Yu HL, Liu J, Chen Y, Yang HF. One-stage surgery by a combined anterior-posterior approach to treat ankylosing spondylitis complicated by a multiple-level cervical vertebral chance fracture. Mod Rheumatol. 2015;25:282–285. [DOI] [PubMed] [Google Scholar]
- 73. Moreau AP, Willcox N, Brown MF. Immobilisation of spinal fractures in patients with ankylosing spondylitis. Two case reports. Injury. 2003;34:372–373. [DOI] [PubMed] [Google Scholar]
- 74. Robinson Y, Robinson AL, Olerud C. Complications and survival after long posterior instrumentation of cervical and cervicothoracic fractures related to ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis. Spine (Phila Pa 1976). 2015;40:E227–E233. [DOI] [PubMed] [Google Scholar]
- 75. Cornefjord M, Alemany M, Olerud C. Posterior fixation of subaxial cervical spine fractures in patients with ankylosing spondylitis. Eur Spine J. 2005;14:401–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. El Masry MA, Badawy WS, Chan D. Combined anterior and posterior stabilisation for treating an unstable cervical spine fracture in a patient with long standing ankylosing spondylitis. Injury. 2004;35:1064–1067. [DOI] [PubMed] [Google Scholar]
- 77. Taggard DA, Traynelis VC. Management of cervical spinal fractures in ankylosing spondylitis with posterior fixation. Spine (Phila Pa 1976). 2000;25:2035–2039. [DOI] [PubMed] [Google Scholar]
- 78. Robinson Y, Willander J, Olerud C. Surgical stabilization improves survival of spinal fractures related to ankylosing spondylitis. Spine (Phila Pa 1976). 2015;40:1697–1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Peh WC, Ho EK. Fracture of the odontoid peg in ankylosing spondylitis: case report. J Trauma. 1995;38:361–363. [DOI] [PubMed] [Google Scholar]
- 80. Wu CT, Lee ST. Spinal epidural hematoma and ankylosing spondylitis: case report and review of the literature. J Trauma. 1998;44:558–561. [DOI] [PubMed] [Google Scholar]
- 81. Broom MJ, Raycroft JF. Complications of fractures of the cervical spine in ankylosing spondylitis. Spine (Phila Pa 1976). 1988;13:763–766. [DOI] [PubMed] [Google Scholar]
- 82. Kao LS, Todd SR, Moore FA. The impact of diabetes on outcome in traumatically injured patients: an analysis of the national trauma data bank. Am J Surg. 2006;192:710–714. [DOI] [PubMed] [Google Scholar]
- 83. Irwin ZN, Arthur M, Mullins RJ, Hart RA. Variations in injury patterns, treatment, and outcome for spinal fracture and paralysis in adult versus geriatric patients. Spine (Phila Pa 1976). 2004;29:796–802. [DOI] [PubMed] [Google Scholar]
- 84. Byrnes MC, McDaniel MD, Moore MB, Helmer SD, Smith RS. The effect of obesity on outcomes among injured patients. J Trauma. 2005;58:232–237. [DOI] [PubMed] [Google Scholar]
- 85. Hollis S, Lecky F, Yates DW, Woodford M. The effect of pre-existing medical conditions and age on mortality after injury. J Trauma. 2006;61:1255–1260. [DOI] [PubMed] [Google Scholar]
- 86. Vives MJ, Harris C, Reiter MF, Drzala M. Use of stand-up magnetic resonance imaging for evaluation of a cervicothoracic injury in a patient with ankylosing spondylitis. Spine J. 2008;8:678–682. [DOI] [PubMed] [Google Scholar]
- 87. Fazl M, Bilbao JM, Hudson AR. Laceration of the aorta complicating spinal fracture in ankylosing spondylitis. Neurosurgery. 1981;8:732–734. [DOI] [PubMed] [Google Scholar]
- 88. Mader R. Clinical manifestations of diffuse idiopathic skeletal hyperostosis of the cervical spine. Semin Arthritis Rheum. 2002;32:130–135. [DOI] [PubMed] [Google Scholar]
- 89. Pascal-Moussellard H, Drossard G, Cursolles JC, Catonné Y, Smadja D. Myelopathy by lesions of the craniocervical junction in a patient with Forestier disease. Spine (Phila Pa 1976). 2006;31: E557–E560. [DOI] [PubMed] [Google Scholar]
- 90. Detwiler KN, Loftus CM, Godersky JC, Menezes AH. Management of cervical spine injuries in patients with ankylosing spondylitis. J Neurosurg. 1990;72:210–215. [DOI] [PubMed] [Google Scholar]
- 91. Schröder J, Liljenqvist U, Greiner C, Wassmann H. Complications of halo treatment for cervical spine injuries in patients with ankylosing spondylitis: report of three cases. Arch Orthop Trauma Surg. 2003;123:112–114. [DOI] [PubMed] [Google Scholar]
- 92. Bañares A, Hernández-García C, Fernández-Gutiérrez B, Jover JA. Eye involvement in the spondyloarthropathies. Rheum Dis Clin North Am. 1998;24:771–784. [DOI] [PubMed] [Google Scholar]
- 93. Shaikh SA. Ankylosing spondylitis: recent breakthroughs in diagnosis and treatment. J Can Chiropr Assoc. 2007;51:249–260. [PMC free article] [PubMed] [Google Scholar]
- 94. Ball J. Enthesopathy of rheumatoid and ankylosing spondylitis. Ann Rheum Dis. 1971;30:213–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Anwar F, Al-Khayer A, Joseph G, Fraser MH, Jigajinni MV, Allan DB. Delayed presentation and diagnosis of cervical spine injuries in long-standing ankylosing spondylitis. Eur Spine J. 2011;20:403–407. [DOI] [PMC free article] [PubMed] [Google Scholar]


