Abstract
Background
One major consequence of economic development in South-East Asia has been a rapid expansion of rubber plantations, in which outbreaks of dengue and malaria have occurred. Here we explored the difference in risk of exposure to potential dengue, Japanese encephalitis (JE), and malaria vectors between rubber workers and those engaged in traditional forest activities in northern Laos PDR.
Methodology/Principal findings
Adult mosquitoes were collected for nine months in secondary forests, mature and immature rubber plantations, and villages. Human behavior data were collected using rapid participatory rural appraisals and surveys. Exposure risk was assessed by combining vector and human behavior and calculating the basic reproduction number (R0) in different typologies. Compared to those that stayed in the village, the risk of dengue vector exposure was higher for those that visited the secondary forests during the day (odds ratio (OR) 36.0), for those living and working in rubber plantations (OR 16.2) and for those that tapped rubber (OR 3.2). Exposure to JE vectors was also higher in the forest (OR 1.4) and, similar when working (OR 1.0) and living in the plantations (OR 0.8). Exposure to malaria vectors was greater in the forest (OR 1.3), similar when working in the plantations (OR 0.9) and lower when living in the plantations (OR 0.6). R0 for dengue was >2.8 for all habitats surveyed, except villages where R0≤0.06. The main malaria vector in all habitats was Anopheles maculatus s.l. in the rainy season and An. minimus s.l. in the dry season.
Conclusions/Significance
The highest risk of exposure to vector mosquitoes occurred when people visit natural forests. However, since rubber workers spend long periods in the rubber plantations, their risk of exposure is increased greatly compared to those who temporarily enter natural forests or remain in the village. This study highlights the necessity of broadening mosquito control to include rubber plantations.
Author summary
Rapid economic development in South-East Asia has resulted in a high demand for rubber, leading to the felling of natural forest and the expansion of rubber plantations. Hundred-thousands of people work in these man-made forests throughout the region, with some studies showing a higher risk of vector-borne diseases for rubber workers compared to typical village populations. In this study we assessed the risk of exposure to vector mosquitoes in relation to different typologies of human behavior. Whilst the highest risk of vector-borne diseases is in natural forest, those living and working in the rubber plantations are at higher risk of dengue and lower risk of malaria vector exposure than villagers that stay in the village. As dengue is endemic in our study area and malaria is not, rubber workers should be encouraged to live in the villages instead of plantations. Furthermore, vector-borne disease control in Lao PDR should broaden from its current focus on villages to include outdoor protection in both rubber plantations and forests, using larval control and personal protection methods.
Introduction
Today we have entered the Anthropocene epoch, in recognition of the major impact human beings have on the environment [1]. Many of the changes in land use and climate are also likely to increase the risk of vector-borne diseases [2–6]. One of the largest environmental changes in South-East Asia (SEA) has been the rapid expansion of rubber plantations. Natural rubber, obtained as latex from the rubber tree Hevea brasiliensis (Willd. ex A Juss.), provides 42% of the global rubber [7, 8]. In 2010 rubber plantations covered 9.2 million ha in SEA [9], supplying more than 90% of the global demand for natural rubber [10]. Stimulated by the high profitability of this crop, the area cultivated for mature rubber in Lao PDR increased rapidly from 900 ha in 2010 to 147,500 ha in 2015 [11]. This is likely to increase to 342,400 ha of mature rubber plantations in the next decade, employing over 100,000 people [11]. Although rubber cultivation is decreasing with the slowdown in the Chinese economy, an estimated four and a half to six million workers will be needed to tap the mature rubber trees in the region in the next decade [12]. Outbreaks of mosquito-borne diseases such as malaria, dengue, and chikungunya have been reported in rubber plantations [13–16]. It has been suggested that rubber workers in SEA are at increased risk of malaria, as plantation workers tap latex at night when malaria vectors are active [13]. With the high number of migrant workers in the rubber plantations, there is fear that these plantations may aid the spread and increase the incidence of mosquito-borne diseases in the region.
Surprisingly little work has been done to assess the importance of rubber plantations as a nidus for the transmission of mosquito-borne diseases in SEA. In this study we investigated the risk of exposure to dengue, Japanese encephalitis (JE), and malaria vectors in relation to different patterns of behavior or typologies commonly represented in this part of northern Lao PDR, in order to understand which behaviors put people most at risk from mosquito-borne diseases.
Methods
Study sites
The adult mosquito sampling and behavioral studies were conducted in Thinkeo (19°41’02.13”N 102°07’05.49”E), Silalek (19°37’02.80”N 102°03’05.70”E), and Houayhoy (19°33’03.22”N 101°59’42.42”E) in Xieng-Ngeun and Nane district, Luang Prabang province. In each study site four common habitats were selected: secondary forests, mature rubber plantations, immature rubber plantations, and villages. The secondary forests were young forests consisting of young small trees with a high density of undergrowth. The mature rubber plantations were those where >70% of the trees were tapped for latex and the immature rubber plantations consisted of rubber trees less than five years old which have not been tapped for latex. The rural villages were small linear settlements of about 150 to 200 bamboo and cement houses. The risk of mosquito-borne disease is highest during the rainy season from May to October. Dengue and JE cases are relatively common, but according to data from Xieng Ngeun and Nane district health centers, malaria has not been locally-transmitted in our study area, with one to five malaria cases imported into the districts every year.
Adult mosquito sampling
Routine entomological measurements were made monthly for nine months from July to November 2013 and in February, March, May and July 2014. A detailed description of the mosquito species collected in the different habitats during the adult mosquito sampling is described in [17]. A total of 78 human subjects gave written informed consent to participate and collect mosquitoes using the human-baited double bed net (HDN) trap [18]. This trap consists of a person on a bamboo bed (30 cm high x 230 cm long x 100 cm wide) covered by two untreated bed nets (small: 97 cm high x 200 cm long x 100 cm wide, mesh size 1.5 mm; large 100 cm high x 250 cm long x 150 cm wide, mesh size 1.5 mm). The internal net protects the occupant from mosquito bites, whilst the outer large net is raised off the ground and traps mosquitoes coming to feed. Mosquitoes were collected outdoors from between the nets at hourly intervals during the day and night. A total of 36 HDN traps were used i.e. three HDN traps in each of the four different habitats. Mosquitoes were morphologically identified to species or species complex using stereo-microscopes and mosquito identification keys of Thailand [19].
Human behavior studies
Daily and monthly activities of the rubber workers and villagers were described qualitatively in the three study sites in November 2013 using rapid participatory rural appraisals (PRA) [20]. All villagers and rubber workers from the study area were invited to participate in the discussions with a local translator present to facilitate the meeting. Participants were asked to complete timetables together, in which they recorded the intensity, from one to five, monthly and hourly according to their experience (one: very low, five: very high) for: rainfall, temperature, mosquito numbers, villagers feeling unwell and travel, including visits to secondary forest, latex tapping, collecting latex and rice production.
A further survey was carried out in June 2015, at the beginning of the rainy season, to collect information on the daily activities of the local population in the past 24 hours. The frequency of visits to the rubber plantations and the methods used to protect themselves from mosquito bites when outdoors was recorded. The study was conducted by a medical doctor fluent in the Lao language. For realistic representation of the different villages, 54 people per village were surveyed (power ω = 0.8, α = 0.05 and size effect of 0.5) [21]. Both studies were anonymous with no sensitive information collected.
Basic reproduction number
Mosquito survival was assessed in all habitats in Thinkeo during the rainy season in July and August 2015. Two HDN traps were deployed in each habitat from 17.00–6.00 h. All Anopheles species previously identified as putative malaria vectors [22–29] and Aedes albopictus (Skuse), previously identified as a putative dengue vector in Lao PDR [30, 31], were dissected to determine parity [32]. The basic reproduction number (R0) for dengue and malaria was calculated in each habitat during both the rainy season (May-September) and dry season (October-April). R0 is calculated based on the Ross-Macdonald model and is an estimate of the number of new infections derived from one infective case in a habitat before the patient dies or is cured [33–35]. Values greater than one suggest that the pathogen would persist in an area if introduced, and values less than one indicate that the pathogen would become extinct.
R0 for dengue was calculated for Ae. albopictus, the only dengue vector in our study area, based on the following formulae (1) [36], using parameters in Table 1.
Table 1. Description of the parameters used for the dengue basic reproductive number model.
| Description | Formula/calculation | |
|---|---|---|
| a | Frequency of the vector mosquito feeding on a person/day | a = C/x |
| C | Proportion of mosquitoes feeding on human blood instead of other animals | 0.99 [37] |
| x | Gonotrophic cycle length, measured by the interval between blood meals taken | Conservative estimate of 4.5 days [38] |
| r | Rate of human recovery (1/number of days) |
Four to five days [36, 39–41] So, 1/4.5 |
| ma | Number of mosquito bites per person/day | Average number of mosquitoes collected per person/day during the adult mosquito sampling study |
| μ | Mortality rate of female mosquitoes | 1- p |
| p | Daily survival probability of adult mosquitoes | A1/X |
| A | Average proportion of parous mosquitoes | Proportion parous from the mosquito survival data |
| n | Development days of virus in mosquito | Using graph [42] with Average Tdry in study area = 23.2 °C Average Train in study area = 23.3 °C |
| b | Proportion of female mosquitoes infective after taking infective blood meal | 0.4 [36, 43] |
| d | Transmission from human to mosquito | 0.4 [36, 43] |
| (1) |
The R0 for malaria was calculated for both Plasmodium falciparum and Plasmodium vivax malaria infections. We calculated the R0 for both parasites, since although 73% of all malaria infections in Lao PDR are due to P. falciparum [44], the last malaria outbreak recorded close to our study area was caused by P. vivax. The R0 was calculated for the primary malaria vectors Anopheles maculatus s.l., An. minimus s.l., and An. dirus s.l., using the following formula (2) [45, 46], with the description of parameters in Table 2.
Table 2. Description of the parameters used for the malaria basic reproductive number model.
| Description | Formula and calculation | |
|---|---|---|
| ma | Number of mosquito bites per person/day | Average number of mosquitoes collected per person/day during the adult mosquito sampling study |
| a | Frequency of the vector mosquito feeding on a person/day | a = C/x |
| C | Proportion of mosquitoes feeding on human blood instead of other animals | 1/3 proportion fed on human for An. maculatus s.l. and An. minimus s.l. [47] 2/3 proportion fed on human for An. dirus s.l. |
| x | Gonotrophic cycle length, measured by the interval between blood meals taken | 2.35 days for An. maculatus s.l. [47, 48] Two days for rainy season and three days for dry season for An. minimus s.l.[49] Three days for An. dirus s.l. [23, 50] |
| b | Proportion of female mosquitoes developing parasites after taking an infective blood meal | Dependent on genetic and non-genetic determinants [51, 52], conservative estimate of 0.5 for all [53] |
| p | Daily survival probability of adult mosquitoes | A1/X |
| A | Average proportion of parous mosquitoes | Proportion parous from the mosquito survival data |
| n | Development days of parasite in mosquito (sporogonic cycle) using Moshkovsky's method | For P. falciparum the thermal sum required to complete parasite development is 111°C above 16°C. For P. vivax the thermal sum required to complete parasite development is 105°C above 14.5°C [54] Average Tdry in study area = 23.2 °C Average Train in study area = 23.3 °C |
| r | Rate of human recovery (1/number of days) | 60 days, so 1/60 [55, 56] |
| (2) |
Analysis
The hourly mosquito sampling results were averaged for the nine months collection period to describe the daily activity of dengue, JE, and malaria vectors in the different habitats. The three PRA’s were summarized by taking the mean intensity of activities from the three appraisals. The study results were described as percentages. The exposure risk to the dengue vector Ae. albopictus, JE vector Culex vishnui s.l., and malaria vectors was assessed using several behavioral typologies. The daily activities of villagers and rubber workers were associated with vector mosquito exposure risk, using the entomological and human behavioral data. The basic reproductive numbers were calculated as described earlier and compared for the different habitats.
Ethics
This study was approved by the Lao ethics committee (approval number 017/NECHR issued 21-04-2013) and the School of Biological and Biomedical Sciences Ethics Committee, Durham University (issued 25-07-2013).
Results
Mosquito sampling
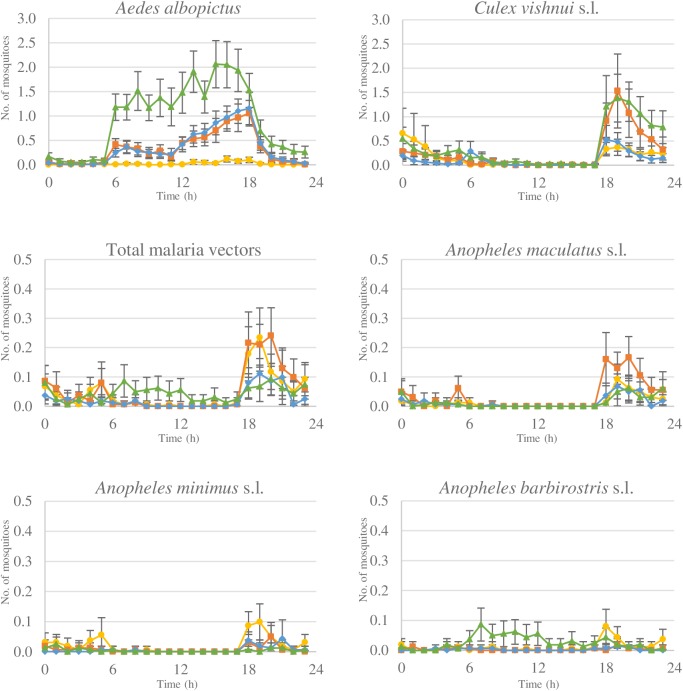
During the adult mosquito sampling 24,927 females were collected. Of these 8,585 were Aedes, with 6,302 Ae. albopictus. The greatest numbers of Ae. albopictus were collected in the secondary forests with similar numbers in rubber plantation habitats (Fig 1). Aedes albopictus were active throughout the day, from 06.00 to 18.00 h. A total of 5,022 Culex were collected, of which 3,562 were Cx. vishnui s.l. Culex vishnui s.l. showed peak activity in the evening from 18.00 h to 20.00 h for all habitats (Fig 1). A total of 1,341 Anopheles mosquito species were collected, of which 661 were putative malaria vectors, including An. maculatus s.l. (n = 294), An. barbirostris s.l. (n = 170), An. minimus s.l. (n = 151 samples), and An. dirus s.l. (n = 46). Malaria vectors were collected in low numbers throughout the day and night. In the secondary forests An. barbirostris s.l. was mostly collected during the day and An. maculatus s.l. during the evening (Fig 1). In all the other habitats malaria vectors were generally collected between 18.00 to 21.00 h. The An. dirus s.l. mosquito samples collected in the different habitats showed similar behavior. About 67% of total An. dirus s.l. were collected between 18.00 and 22.00 h (30/46), with the remaining samples collected between 01.00 and 05.00 h. All data has been deposited in the Dryad repository http://dx.doi.org/10.5061/dryad.8nf05 [57].
Fig 1. The average number of female mosquitoes collected per person/hour in the four different habitats ( secondary forests, mature plantations, immature plantations, villages) for Aedes albopictus, Culex vishnui s.l., total malaria vectors, Anopheles maculatus s.l., Anopheles minimus s.l., and Anopheles barbirostris s.l. during 24 hrs.
All including 95% confidence interval.
Human behavioral studies
Between 15 to 19 villagers, 16 to 60 years old, participated in a single two hour long PRA at each of the three study sites. During the rainy season (May to November) considerable time was spent cultivating rice, the staple food. Secondary forests were also visited during the rains, most frequently during daylight hours (05.00 h to 17.00 h; S1 Table), to collect food, wood, and other commodities. Occasionally the forests were visited at night to hunt small animals, like rodents and muntjacs. Rubber tapping also occurred in the rainy season with the trees tapped at night, between 02.00 h and 07.00 h, when latex flow is highest. Generally latex is collected from the latex collection cups in the morning from 07.00 h to 10.00 h. From 17.00 to 07.00 h usually most villagers were in the village to cook, clean, and sleep. Young children (< 14 years), villagers who did not have to work and elderly villagers (> 60 years) stayed in the village throughout the day. From December to February, when there was no farming, some villagers travelled to other parts of Lao PDR and abroad to find work (S2 Table).
A total of 162 participants were surveyed to identify their movement in the last 24 hrs, of which 8.6% (14/162) were rubber workers. Usually villagers 14 to 55 years old leave the village during the day from 07.00 h to 17.00 h; with 40% (65/162) working on the farm, 10% (17/162) going to high school, 5% (8/162) working in rubber plantations, 3% (5/162) going to the forest and 3% (4/162) visiting Luang Prabang, the provincial capital. The remaining 39% (63/162) stayed in the village. More than 91% (147/162) of villagers and rubber workers stayed in the village at night the day before the study was conducted. They generally slept from 20.00 h to 05.00 h. The remaining 6% (10/16) slept in the farms and 3% (5/162) worked in the rubber plantations. One person spent the whole night in the secondary forest. About 77% (114/148) of the non-rubber workers visited the rubber plantations at least once every month (range in age from one to 96 years) to help with maintenance of the plantation area (cutting undergrowth and clearing fallen trees), to collect fire wood, and to collect food such as mushrooms, insects, and edible plants. More than 90% (148/162) of participants had insecticide-treated bed nets in their houses. Furthermore, a total of 34% (55/162) of respondents used methods to protect themselves against mosquitoes when outdoors, with 60% (33/55) using mosquito coils and 35% (19/55) using the repellent N,N-Diethyl-meta-toluamide (DEET). About 7% (4/55) of participants said they wore long sleeves to protect against mosquito bites and 2% (1/55) mentioned the use of lemongrass.
Human behavioral typologies
We identified four distinct behavioral typologies: (1) villagers that visit the forest during the day, (2) villagers that work in the rubber plantations, (3) migrant workers that live and work in the rubber plantations, and (4) villagers that stay in the village.
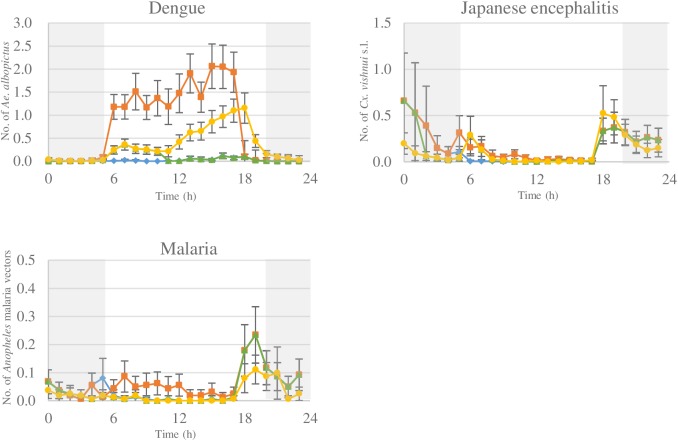
Villagers that visit the forest during the day
In this typology, villagers visit the forest during the day from 05.00 h to 17.00 h and sleep in the village at night. Exposure to Ae. albopictus is highest in the secondary forests during the day from 06.00 h to 17.00 h (Fig 1). Therefore, risk of exposure to Ae. albopictus is 36 times greater when villagers visit the forest during the day (Fig 2, Table 3). Culex vishnui s.l. exposure is also greater when visiting the forest during the day, although highest exposure still occurs in the villages after returning from the forest (Fig 2, Table 3). Exposure to malaria vectors is 1.3 times higher in the forest (Table 3). Risk of exposure to dengue, JE, and malaria vectors is higher for villagers that visited the secondary forests than those that stayed in the village.
Fig 2. The average hourly exposure to female Aedes albopictus (dengue vector), Culex vishnui s.l. (Japanese encephalitis vector), and Anopheles malaria vectors for the different typologies, ( villagers that visit the forest during the day from 5.00 to 17.00 h, villagers that work in the rubber plantations, migrant workers that live and work in the rubber plantations, villager that stays in the village) with the possible use of bed nets indicated from 20.00 h to 5.00 h with .
All including 95% confidence interval.
Table 3. The daily risk of exposure to vectors for people in different human behavior typologies.
|
Dengue vector exposure risk |
Japanese encephalitis vector exposure risk |
Malaria vector exposure risk |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Exposure per 24 hrs | Ae. albopictus exposure (95% CI) | OR (95% CI) | P | Cx. vishnui s.l. exposure (95% CI) | OR (95% CI) | P | Malaria vectors exposure (95% CI) | OR (95% CI) | P |
| Villagers that visit the forest during the day | 16.8 (14.1–19.4) | 36.0 (24.6–52.6) | <0.001* | 4.5 (2.9–6.2) | 1.4 (1.2–1.7) | <0.001* | 1.4 (1.1–1.8) | 1.3 (1.2–1.4) | <0.001* |
| Villagers that work in the rubber plantations | 1.6 (1.3–2.0) | 3.2 (2.3–4.5) | <0.001* | 3.6 (2.3–5.0) | 1.0 (0.9–1.0) | 0.357 | 1.0 (0.7–1.3) | 0.9 (0.8–1.0) | 0.062 |
| Migrant workers that live and work in the rubber plantations | 8.2 (7.0–9.5) | 16.2 (11.5–22.9) | <0.001* | 2.7 (1.8–3.7) | 0.8 (0.6–1.1) | 0.195 | 0.6 (0.4–0.8) | 0.6 (0.4–1.0) | 0.037* |
| Villagers that stay in the village | 0.5 (0.4–0.7) | 1 | 3.7 (2.1–5.4) | 1 | 1.1(0.8–1.4) | 1 | |||
Results are shown using generalized estimating equations with odds ratio (OR) and 95% confidence interval (CI).
*significantly different, P<0.05
Villagers that work in the rubber plantations
Rubber workers that live in the villages and work in the rubber plantations at night from 02.00 h to 10.00 h are exposed to both village and rubber plantation mosquitoes. Highest Ae. albopictus exposure occurs when working in the plantation, with peak exposure from 06.00 to 10.00 h (Fig 2). Working in the plantations thus increases dengue vector exposure risk more than three times compared to staying in the village (Table 3). Risk of Cx. vishnui s.l. exposure is highest when rubber workers are resting in the village with presence in rubber plantations not increasing risk (Fig 2, Table 3). Similarly, malaria vector exposure risk does not increase when rubber plantations are visited at night (Fig 2, Table 3). Compared to remaining in the village, working in the plantations increases the risk of dengue vector exposure, but not for JE or malaria.
Migrant workers that live and work in the rubber plantations
Migrant workers that live and work in the rubber plantations are only exposed to mosquitoes present in the mature rubber plantations. Here the risk of dengue vector exposure is 16 fold higher than staying in the village (Fig 2, Table 3). However, rubber workers living in the plantations are exposed to similar number of Cx. vishnui s.l. mosquitoes and slightly fewer malaria vectors than those remaining in the villages (Fig 2, Table 3). Living and working in the rubber plantations increases risk of dengue vector exposure and decreases risk of malaria vector exposure, compared to villagers staying in the village, while JE vector exposure remains the same.
Villagers that stay in village
These individuals are only exposed to mosquitoes present in the village, with peak biting at dusk from 18.00 to 19.00 h (Fig 2). Exposure to mosquitoes is generally low with three Cx. vishnui s.l., one malaria vector, and 0.5 Ae. albopictus mosquitoes captured each day (Fig 2, Table 3). When a bed net is used during the night from 20.00 to 5.00 h, exposure to JE vectors can decrease to less than one mosquito exposure every 24 hrs and halve malaria vector exposure (Fig 2). Generally villagers that stay in the village are at low risk of exposure to JE and malaria vectors, with very low risk of exposure to dengue vectors.
Basic reproduction number for mosquito-borne diseases
Mosquito survival
During 42 nights of collection, a total of 1,048 Ae. albopictus mosquitoes and 82 Anopheles malaria vectors (An. aitkenii group, An. dirus s.l., An. barbirostris s.l., An. epiroticus (Linton & Harbach), An. hodgkini (Reid), An. maculatus s.l., An. minimus s.l., An. tesselatus (Theobald) and An. umbrosus s.l.) were dissected. Twenty six Ae. albopictus and seven Anopheles malaria vectors could not be dissected successfully for identification of parity. In general the parity rate was high with long-lived vectors present in all habitats (S3 Table). For An. maculatus s.l., 34 samples were collected in the four different habitats of which 31 were parous (91.2%). For An. minimus s.l., 18 samples were collected of which 17 were parous (94.4%) and for An. dirus s.l., 14 samples were collected, of which eight were parous (57.1%).
Basic reproduction number for dengue
The R0 for the dengue vector Ae. albopictus was calculated using the average number of Ae. albopictus bites per person per day (ma) in the different habitats (S4 Table). The R0 was considerably higher than one for all natural and man-made forest habitats during both the rainy season and dry season, and considerably lower than one for the villages (Table 4). The R0 was highest in the secondary forests and second highest in the mature rubber plantations. Of the three forest habitats, the R0 was lowest in the immature rubber plantations.
Table 4. The basic reproductive number (R0) for dengue vector Ae. albopictus in the secondary forest, mature rubber plantation, immature rubber plantation, and village habitats during the rainy season and dry season.
| Secondary forest | Mature rubber plantation | Immature rubber plantation | Village | |
|---|---|---|---|---|
| Rainy season | 42.0 | 18.8 | 9.5 | 0.06 |
| Dry season | 10.6 | 2.8 | 1.5 | 0.01 |
Basic reproductive number for malaria
The R0 for malaria was calculated using the average number of bites per person per day (ma) for the different malaria vectors in each of the different habitats (S4 Table). Parity data of An. maculatus s.l., An. minimus s.l., and An. dirus s.l. were used separately. All habitats exhibited high malaria R0 during both the rainy season and dry season, with similar outcomes for P. falciparum and P. vivax (Table 5). Both An. maculatus s.l. and An. minimus s.l. are important malaria vectors in the study sites, whilst An. dirus s.l. is not.
Table 5. The basic reproductive number for P. falciparum and P. vivax malaria parasites calculated for the different vectors in the different habitats during the rainy season and dry season.
| Malaria parasite | Malaria vector | Secondary forest | Mature rubber plantation | Immature rubber plantation | Village | |
|---|---|---|---|---|---|---|
| Rainy season | P. falciparum | An. maculatus s.l. | 28.6 | 16.6 | 64.0 | 28.6 |
| An. minimus s.l. | 8.3 | 2.8 | 6.9 | 42.8 | ||
| An. dirus s.l. | 0.2 | 0.1 | 0.5 | 0 | ||
| P. vivax | An. maculatus s.l. | 31.2 | 18.1 | 69.8 | 31.2 | |
| An. minimus s.l. | 8.8 | 2.9 | 7.4 | 45.7 | ||
| A. dirus s.l. | 0.3 | 0.2 | 0.7 | 0 | ||
| Dry season | P. falciparum | An. maculatus s.l. | 13.1 | 22.1 | 39.2 | 11.4 |
| An. minimus s.l. | 18.1 | 36.1 | 41.6 | 84.9 | ||
| An. dirus s.l. | 0.03 | 0.2 | 0.5 | 0.02 | ||
| P. vivax | An. maculatus s.l. | 14.9 | 25.2 | 44.8 | 13.1 | |
| An. minimus s.l. | 19.3 | 38.5 | 44.3 | 90.6 | ||
| A. dirus s.l. | 0.05 | 0.3 | 1.0 | 0.05 |
Discussion
We assessed how human behavior changes the risk of exposure to mosquito-borne diseases in rural parts of northern Lao PDR. This study shows that the greatest risk is associated with visiting secondary forest during the day; increasing the risk of dengue, JE, and malaria. Working in the rubber plantations also increases the risk of dengue, which is exacerbated when workers both live and work in the plantations. However, staying in the rubber plantations did not increase risk of exposure to JE vectors and decreased risk of exposure to malaria vectors. Our estimates of R0 show that the risk of dengue outbreaks in secondary forests, mature rubber plantations, and immature rubber plantations is extremely high, largely because of the high survival of the vector, Ae. albopictus. The villages are relative sanctuaries with values of R0 considerably less than 1, indicating that the transmission of dengue would not be maintained. The R0 estimates also showed that the risk of malaria outbreaks in all investigated habitats is very high, with the most important malaria vector in the rainy season being An. maculatus s.l. and in the dry season, An. minimus s.l.
Dengue is a sylvatic disease that has been spread from the forest to rural and urban areas by the highly adaptable vector Ae. albopictus, that has readily colonized a variety of different rural habitats [58, 59]. In this study, we found a substantial risk of Ae. albopictus exposure and consequently risk of dengue infection in the natural forests and rubber plantations, compared with the villages. According to the behavioral analysis, both the natural and man-made forests are regularly visited by villagers. It therefore seems likely that the forest and plantation habitats are where dengue transmission occurs. As dengue is endemic in our study area and malaria is not, rubber workers should be encouraged to live in the villages instead of plantations. This is especially important for migrant rubber plantation workers, as presence in the village increases knowledge on diseases and lowers the threshold to get treatment. Worryingly, dengue vector control in the country is presently focused in the villages where the risk of transmission is low. There is therefore a clear need to broaden the control efforts to protect people when entering the surrounding forest and rubber plantations. In future studies, the presence of dengue infections in Ae. albopictus needs to be molecularly confirmed.
Villagers that visit the secondary forests during the day are exposed to a higher number of JE vectors than when staying in the village. Japanese encephalitis infection risk is dependent on the presence of water birds, the reservoir hosts, and pigs, the amplifying host. Although there are pigs in the forests, there are considerably more water birds and pigs within and close to the villages, increasing the risk of JE infections in the villages. It is therefore important to take the local dynamics of the disease pathogens into account.
Rubber workers that live in the villages are exposed to similar numbers of malaria vectors as the villagers staying at home, with the risk of malaria exposure dropping when workers both live and work in the rubber plantations. This is contrary to earlier suggestions from Thailand that rubber tapping activity increases exposure to malaria vectors [13]. Working in the rubber plantations at night from 02.00 to 10.00 h is not a risky behavior for malaria vector exposure in this study area, due to the early evening host seeking behavior of the malaria vectors An. maculatus s.l. and An. minimus s.l. However, the high R0 of malaria identified for all habitats does imply that if a malaria-infected person moves into the rubber plantations, the potential for a large number of new infections would arise, transmitted by An. maculatus s.l. and An. minimus s.l. We identified two ways in which malaria transmission could occur in the study area. Firstly, we found that local villagers often migrate to find temporary work in other areas of SEA. These migrant workers could be infected by malaria parasites in other regions and carry the parasites back to their own village. Secondly, many of the rubber plantations workers that live in the plantations are migrant workers that only live in the plantations during the rainy season. These migrant workers could introduce malaria parasites from other areas in SEA to the rubber plantation areas. In this study we have shown that the rubber plantations are visited regularly by the local population, indicating that the pathogens established in the rubber plantations could easily spread to the villages. Although malaria is currently not endemic in the study area, if malaria parasites are introduced, all necessary factors are present for an outbreak, and the establishment of malaria. Monitoring the malaria disease presence is thus essential in both the local population and migrant workers. Future entomological studies in the area should focus on the dissection of putative malaria vectors for the identification of sporozoites and oocysts, and focus on the molecular identification of malaria parasites, including the possible presence of Plasmodium knowlesi.
Mathematical models simplify the complexity of natural systems. The R0 calculations in this paper are no exception. Our models do not consider the dynamics of the larval stages of the mosquitoes, spatial heterogeneity, interrupted feeding of Ae. albopictus, the vertical and sexual transmission of dengue viruses, nor the immune status of the population. The high basic reproduction numbers found in this study reflects the extraordinarily high mosquito survival rates calculated in this study, often exceeding 90%.
Including human behavioral patterns is important for appropriate recommendations on disease control [60]. There is a lack of suitable methods to measure human behavior, especially on an individual scale, with limits to the predictability of human mobility [61–63]. There are a number of techniques commonly used to capture human movement, such as GPS tracking systems [64, 65], cellular phones [66] and photo voice [67]. In this study we used a combination of PRA’s and surveys to collect human behavior data, which is novel for vector-borne disease studies. The PRA’s and surveys do not result in detailed quantitative information. Both methods are sensitive to memory decay, social desirability, and other biases. Yet the two methods combined allowed us to describe broad patterns of human behavior and relate risk of vector-borne infections to villagers and rubber workers behavior.
Identifying risky behaviors should help explain the heterogeneous pattern of vector-borne diseases, and result in more targeted disease control [61, 68–72]. Currently mosquito control in Lao PDR focusses on the distribution of long-lasting insecticidal nets (LLINs), indoor residual spraying (IRS) and larval source management (LSM) in the villages. The current control strategies are insufficient to control vector-borne diseases, with dengue and malaria outbreaks still occurring regularly. This study has highlighted the importance of secondary forest and rubber plantations in the mosquito-control strategies, specifically for the control of dengue. As in our study area, dengue is an important endemic disease and malaria is not, rubber workers could be encouraged to live in the villages, where dengue vector exposure is lower. Mosquito-control in rubber plantations should focus on the rubber worker houses inside the plantations and on outdoor control. For control in rubber plantation houses, similar methods can be used as in the villages; such as using LLINs, spatial repellents, and screening of houses [12]. For outdoor control, both personal protection and LSM is necessary. Personal protection methods should include motivating rubber workers to wear long-sleeved clothing and closed shoes when in the plantation. Additionally, insecticide-treated clothing, insecticide emanators, and portable insecticide coils could be used for personal protection [12]. However, these personal protection methods need to be further investigated to identify if vector-borne disease cases can be prevented. Rubber plantations provide a plethora of potential breeding sites including latex-collection cups [73–75]. Larval control in rubber plantations can therefore be achieved by draining the latex collection cups by turning them upside down. In forested areas, mosquito control is more challenging than the rubber plantation areas. Particularly larval control is difficult to implement in the natural forests due to the vastness and diversity of breeding sites, and the high biodiversity of other insects present. Emphasis should therefore be on personal protection methods, which are similar to the rubber workers. Additionally, insecticide treated hammocks could be used when staying in the forests overnight [76–78].
Conclusion
This study demonstrates that entering secondary forest or rubber plantations represents a higher risk of dengue vector exposure than staying in the villages, where current vector control is focused. As rubber workers spend a substantial amount of time in the plantations, this increases their risk of dengue vector exposure compared to villagers who irregularly visit the natural forests or remain in the village. Rubber workers could be encouraged to live in the villages instead of the rubber plantations. Additionally, JE and malaria vector risk increases when visiting the forests during the day, but does not increase when working and living in the rubber plantations. This study highlights the importance of understanding human behavior in order to identify risky behaviors. Specifically, it demonstrates the necessity of broadening current vector control activities to include rubber plantations.
Supporting information
Summary of data obtained from the rapid participatory rural appraisals on the daily intensity of mosquito and human activity in different habitats.
(DOCX)
Summary of data obtained from the rapid participatory rural appraisals on the monthly intensity of environmental variables, mosquito activity, and human activity.
(DOCX)
The parity rate of the dengue vector Ae. albopictus and of the putative malaria vectors in the secondary forests, mature rubber plantations, immature rubber plantations, and villages.
(DOCX)
The average number of mosquito bites per person per day (ma) for the important vector species Ae. albopictus, An. maculatus s.l., An. minimus s.l., and An. dirus s.l. in the secondary forest, mature rubber plantation, immature rubber plantation and village habitats during the rainy season and dry season.
(DOCX)
Acknowledgments
We are grateful to the residents of Thin Keo, Silalek, and Houayhoy village for their hospitality and cooperation. We thank the district heads of Nane and Xieng Ngeun and the provincial head of Luang Prabang for their assistance. We could not have done this study without the support of our driver Hongnakhon Xayasing, nor with the helpful input from Sok Dara and Min Sophoan from Agronomes et Vétérinaires Sans Frontières (AVSF). We are appreciative for the input from Yves Froehlich and Julia Ledien from Institut Pasteur de Cambodge. Finally, we thank the staff of Institut Pasteur Laos for their commitment in helping establish and providing support throughout the study.
Data Availability
All data files are available from the DRYAD database: http://dx.doi.org/10.5061/dryad.8nf05.
Funding Statement
This work was supported by The Agence Française de Développement; Grant number CZZ 1809 AA; http://www.afd.fr/lang/en/home. This project falls under the project ECOMORE; http://ecomore.org. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Whitmee S, Haines A, Beyrer C, Boltz F, Capon AG, de Souza Dias BF, et al. Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation-Lancet Commission on planetary health. Lancet. 2015;386: 1973–2028. doi: 10.1016/S0140-6736(15)60901-1 [DOI] [PubMed] [Google Scholar]
- 2.Foley JA, DeFries R, Asner GP, Barford C, Bonan G, Carpenter SR, et al. Global consequences of land use. Science. 2005;309: 570–574. doi: 10.1126/science.1111772 [DOI] [PubMed] [Google Scholar]
- 3.Patz JA, Olson SH, Uejio CK, Gibbs HK. Disease emergence from global climate and land use change. Med Clin North Am. 2008;92: 1473–1491. doi: 10.1016/j.mcna.2008.07.007 [DOI] [PubMed] [Google Scholar]
- 4.Norris D. Mosquito-borne diseases as a consequence of land use change. EcoHealth. 2004;1: 19–24. doi: 10.1007/s10393-004-0008-7 [Google Scholar]
- 5.Parham PE, Waldock J, Christophides GK, Hemming D, Agusto F, Evans KJ, et al. Climate, environmental and socio-economic change: weighing up the balance in vector-borne disease transmission. Phil Trans R Soc B. 2015;370: 1665 doi: 10.1098/rstb.2013.0551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Millenium Ecosystem Assessment. Chapter 14: Human health: ecosystem regulation of infectious diseases. Washington: MEA, 2005.
- 7.Sustainable Mekong Research Network. Discussion paper: rubber investment and market linkages in Lao PDR: approaches of sustainability. Vientiane: Sumernet, 2009. [Google Scholar]
- 8.International Rubber Study Group. Rubber industry report. Singapore: IRSG, 2012. [Google Scholar]
- 9.Food and Agriculture Organization. Global forest resources assessment 2010. Rome: FAO, 2010. [Google Scholar]
- 10.International Rubber Study Group. Statistical summary of world rubber situation. Statistical Rubber Bulletin 2014;April—June
- 11.National Agriculture and Forestry Research Institute. Review of rubber plantations. Vientiane: Ministry of Agriculture and Forestry, NAFRI, 2016. [Google Scholar]
- 12.Tangena J-AA, Thammavong P, Wilson AL, Brey PT, Lindsay SW. Risk and control of mosquito-borne diseases in Southeast Asian rubber plantations. Trends Parasitol. 2016;32: 402–415. doi: 10.1016/j.pt.2016.01.009 [DOI] [PubMed] [Google Scholar]
- 13.Bhumiratana A, Sorosjinda-Nunthawarasilp P, Kaewwaen W, Maneekan P, Pimnon S. Malaria-associated rubber plantations in Thailand. Travel Med Infect Dis. 2013;11: 37–50. doi: 10.1016/j.tmaid.2012.11.002 [DOI] [PubMed] [Google Scholar]
- 14.Wangroongsarb P, Sudathip P, Satimai W. Characteristics and malaria prevalence of migrant populations in malaria-endemic areas along the Thai-Cambodian border. Southeast Asian J Trop Med Public Health. 2012;43: 261–269. [PubMed] [Google Scholar]
- 15.Palaniyandi M. The environmental aspects of dengue and chikungunya outbreaks in India: GIS for epidemic control. Int J Mosq Res. 2014;1: 35–40. [Google Scholar]
- 16.Kumar NP, Suresh A, Vanamail P, Sabesan S, Krishnamoorthy KG, Mathew J, et al. Chikungunya virus outbreak in Kerala, India, 2007: a seroprevalence study. Mem Inst Oswaldo Cruz. 2011;106: 912–916. [DOI] [PubMed] [Google Scholar]
- 17.Tangena J-AA, Thammavong P, Malaithong N, Inthavong T, Ouanesamon P, Brey PT, et al. Diversity of Mosquitoes (Diptera: Culicidae) Attracted to Human Subjects in Rubber Plantations, Secondary Forests, and Villages in Luang Prabang Province, Northern Lao PDR. J Med Entomol 2017. doi: 10.1093/jme/tjx071 [DOI] [PubMed] [Google Scholar]
- 18.Tangena J-AA, Thammavong P, Hiscox A, Lindsay SW, Brey PT. The human-baited double net trap: an alternative to human landing catches for collecting outdoor biting mosquitoes in Lao PDR. PLoS One. 2015;10: e0138735 doi: 10.1371/journal.pone.0138735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rattanarithikul R, Harbach RE, Harrison BA, Panthusiri P, Coleman RE, Richardson JH. Illustrated keys to the mosquitoes of Thailand II-VI. Southeast Asian J Trop Med Public Health. 2005–2010;36, 37 and 41. [PubMed] [Google Scholar]
- 20.Annett H, Rifkin SB. Guidelines for rapid participatory appraisals to assess community health needs: a focus on health improvements for low-income urban and rural areas. Geneva: WHO, 1995. [Google Scholar]
- 21.Statstodo. Sample size calculation: Statstodo; 2013 [28-03-2013 and 12-06-2014]. Available from: https://www.statstodo.com/index.php.
- 22.Vythilingam I, Sidavong B, Chan ST, Phonemixay T, Phetsouvanh R, Phompida S. Heavy natural oocyst infections in Anopheles dirus (Diptera: Culicidae) from Attapeu province, Lao PDR. Int J Trop Insect Sci 2001;25: 59–61. [Google Scholar]
- 23.Vythilingam I, Phetsouvanh R, Keokenchanh K, Yengmala V, Vanisaveth V, Phompida S, et al. The prevalence of Anopheles (Diptera: Culicidae) mosquitoes in Sekong Province, Lao PDR in relation to malaria transmission. Trop Med Int Health. 2003;8: 525–535. [DOI] [PubMed] [Google Scholar]
- 24.Vythilingam I, Sidavong B, Chan ST, Phonemixay T, Vanisaveth V, Sisoulad P, et al. Epidemiology of malaria in Attapeu Province, Lao PDR in relation to entomological parameters. Trans R Soc Trop Med Hyg. 2005;99: 833–839. doi: 10.1016/j.trstmh.2005.06.012 [DOI] [PubMed] [Google Scholar]
- 25.Toma T, Miyagi I, Okazawa T, Kobayashi J, Saita S, Tuzuki A, et al. Entomological surveys of malaria in Khammouane Province, Lao PDR, in 1999 and 2000. Southeast Asian J Trop Med Public Health. 2002;33: 532–546. [PubMed] [Google Scholar]
- 26.Do Manh C, Beebe N, Thi Van VN, Le Quang T, Lein C, Van Nguyen D, et al. Vectors and malaria transmission in deforested, rural communities in north-central Vietnam. Malar J. 2010;9: 259 doi: 10.1186/1475-2875-9-259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cui L, Yan G, Sattabongkot J, Cao Y, Chen B, Chen X, et al. Malaria in the Greater Mekong Subregion: heterogeneity and complexity. Acta trop. 2012;121: 227–239. doi: 10.1016/j.actatropica.2011.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kobayashi J, Somboon P, Keomanila H, Inthavongsa S, Nambanya S, Inthakone S, et al. Malaria prevalence and a brief entomological survey in a village surrounded by rice fields in Khammouan province, Lao PDR. Trop Med Int Health. 2000;5: 17–21. doi: 10.1046/j.1365-3156.2000.00516.x [DOI] [PubMed] [Google Scholar]
- 29.Kobayashi J, Nambanya S, Miyagi I, Vanachone B, Manivong K, Koubouchan T, et al. Collection of anopheline mosquitos in three villages endemic for malaria in Khammouane, Lao PDR. Southeast Asian J Trop Med Public Health. 1997;28: 20–21. [PubMed] [Google Scholar]
- 30.Tsuda Y, Kobayashi J, Nambanya S, Miyagi I, Toma T, Phompida S, et al. An ecological survey of dengue vector mosquitos in central Lao PDR. Southeast Asian J Trop Med Publ Health. 2002;33: 63–67. [PubMed] [Google Scholar]
- 31.Hiscox A, Winter CH, Vongphrachanh P, Sisouk T, Somoulay V, Phompida S, et al. Serological investigations of Flavivirus prevalence in Khammouane province, Lao People's Democratic Republic, 2007–2008. Am J Trop Med Hyg 2010;83: 1166–1169. doi: 10.4269/ajtmh.2010.09-0480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Detinova TS. Determination of the physiological age of female Anopheles from the changes of the tracheal system of the ovaries. Med Parazitol (Mosk). 1945;14: 45–49. [PubMed] [Google Scholar]
- 33.Ross R. The mathematics of malaria. BMJ. 1911;1: 1023. [Google Scholar]
- 34.Macdonald G. Analaysis of the sporozoite rate. Trop Dis Bull. 1952;49: 569–585. [PubMed] [Google Scholar]
- 35.Reiner RC, Perkins TA, Barker CM, Niu T, Chaves LF, Ellis AM, et al. A systematic review of mathematical models of mosquito-borne pathogen transmission: 1970–2010. J R Soc Interface. 2013;10: 20120921 doi: 10.1098/rsif.2012.0921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Coelho FC, Codeço CT, Struchiner CJ. Complete treatment of uncertainties in a model for dengue R0 estimation. Cad Saúde Pública. 2008;24: 853–861. [DOI] [PubMed] [Google Scholar]
- 37.Ponlawat A, Harrington LC. Blood feeding patterns of Aedes aegypti and Aedes albopictus in Thailand. J Med Entomol. 2005;42: 844–849. [DOI] [PubMed] [Google Scholar]
- 38.Delatte H, Gimonneau G, Triboire A, Fontenille D. Influence of temperature on immature development, survival, longevity, fecundity, and gonotrophic cycles of Aedes albopictus, vector of chikungunya and dengue in the Indian Ocean. J Med Entomol. 2009;46: 33–41. Epub 2009/02/10. [DOI] [PubMed] [Google Scholar]
- 39.Dubot-Pérès A, Vongphrachanh P, Denny J, Phetsouvanh R, Linthavong S, Sengkeopraseuth B, et al. An epidemic of Dengue-1 in a remote village in rural Laos. PLoS Negl Trop Dis. 2013;7: e2360 doi: 10.1371/journal.pntd.0002360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guha-Sapir D, Schimmer B. Dengue fever: new paradigms for a changing epidemiology. Emerg Themes Epidemiol. 2005;2: 1 doi: 10.1186/1742-7622-2-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.World Health Organization. Dengue and severe dengue fact sheet: World Health Organization; 2016. [updated July 201627-02-2016]. Available from: http://www.who.int/mediacentre/factsheets/fs117/en/. [Google Scholar]
- 42.Focks DA, Daniels E, Haile DG, Keesling JE. A simulation-model of the epidemiology of urban dengue fever—literature analysis, model development, preliminary validation, and samples of simulation results. Am J Trop Med Hyg. 1995;53: 489–506. [DOI] [PubMed] [Google Scholar]
- 43.Luz PM, Codeço CT, Massad E, Struchiner CJ. Uncertainties regarding dengue modeling in Rio de Janeiro, Brazil. Mem Inst Oswaldo Cruz. 2003;98: 871–878. [PubMed] [Google Scholar]
- 44.World Health Organization. World malaria report 2015. Geneva: WHO, 2015. [Google Scholar]
- 45.Aaron J, May R. The population dynamics of malaria In: Anderson R, editor. Population dynamics of infectious diseases. London: Chapman & Hall; 1982. pp. 139–179. [Google Scholar]
- 46.Lindsay SW, Thomas CJ. Global warming and risk of vivax malaria in Great Britain. GCHH. 2001;2: 80–84. doi: 10.1023/A:1011995115713 [Google Scholar]
- 47.Loong KP, Chiang GL, Eng KL, Chan ST, Yap HH. Survival and feeding behaviour of Malaysian strain of Anopheles maculatus Theobald (Diptera: Culicidae) and their role in malaria transmission. Trop Biomed. 1990;7: 71–76. [Google Scholar]
- 48.Chiang GL, Loong KP, Chan ST, Eng KL, Yap HH. Capture-recapture studies with Anopheles maculatus Theobald (Diptera: Culicidae) the vector of malaria in peninsular Malaysia. Southeast Asian J Trop Med Public Health. 1991;22: 643–647. [PubMed] [Google Scholar]
- 49.Ratanatham S, Upatham ES, Prasittisuk C, Rojanasunan W, Theerasilp N, Tremongkol A, et al. Bionomics of Anopheles minimus and its role in malaria transmission in Thailand. Southeast Asian J Trop Med Public Health. 1988;19: 283–289. [PubMed] [Google Scholar]
- 50.Chow CY. Bionomics of malaria vectors in the Western Pacific Region. Southeast Asian J Trop Med Publ Health. 1970. [Google Scholar]
- 51.Lefèvre T, Vantaux A, Dabiré KR, Mouline K, Cohuet A. Non-genetic determinants of mosquito competence for malaria parasites. PLoS Pathog. 2013;9: e1003365 doi: 10.1371/journal.ppat.1003365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Eling W, Hooghof J, Sauerwein RW, van Gemert GJ. Tropical temperatures can inhibit development of the human malaria parasite Plasmodium falciparum in the mosquito. Proc Neth Entomol Soc Meet. 2001;12: 151–156. [Google Scholar]
- 53.Hoshen M, Morse A. A weather-driven model of malaria transmission. Malar J. 2004;3: 32 doi: 10.1186/1475-2875-3-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Detinova TS. Age grouping methods in Diptera of medical importance. Geneva: WHO, 1962. [PubMed] [Google Scholar]
- 55.Boyd MF. Malariology; a comprehensive survey of all aspects of this group of disease from a global standpoint. Philadelphia: Saunders; 1949. [Google Scholar]
- 56.Bekessy A, Molineaux L, Storey J. Estimation of incidence and recovery rates of Plasmodium falciparum parasitaemia from longitudinal data. Bull World Health Organ. 1976;54: 685–693. [PMC free article] [PubMed] [Google Scholar]
- 57.Tangena JA, Thammavong P, Lindsay SW, Brey PT. Data from: Risk of Exposure to Potential Vector Mosquitoes for Rural Workers in Northern Lao PDR. Dryad Digital Repository http://dx.doi.org/10.5061/dryad.8nf05; 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vasilakis N, Cardosa J, Hanley KA, Holmes EC, Weaver SC. Fever from the forest: prospects for the continued emergence of sylvatic dengue virus and its impact on public health. Nat Rev Microbiol. 2011;9: 532–541. doi: 10.1038/nrmicro2595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hawley WA. The biology of Aedes albopictus. J Am Mosq Control Assoc. 1988;4: 2–39. [PubMed] [Google Scholar]
- 60.Lyttleton C. Deviance and resistance: malaria elimination in the Greater Mekong subregion. Soc Sci Med. 2016;150: 144–152. http://dx.doi.org/10.1016/j.socscimed.2015.12.033. doi: 10.1016/j.socscimed.2015.12.033 [DOI] [PubMed] [Google Scholar]
- 61.Stoddard S, Morrison A, Vazquez-Prokopec G, Paz Soldan V, Kochel T, Kitron U. The role of human movement in the transmission of vector-borne pathogens. PLoS Negl Trop Dis. 2009;3: e481 doi: 10.1371/journal.pntd.0000481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Song C, Qu Z, Blumm N, Barabási A-L. Limits of predictability in human mobility. Science. 2010;327: 1018–1021. doi: 10.1126/science.1177170 [DOI] [PubMed] [Google Scholar]
- 63.Gonzalez MC, Hidalgo CA, Barabasi A-L. Understanding individual human mobility patterns. Nature. 2008;453: 779–782. doi: 10.1038/nature06958 [DOI] [PubMed] [Google Scholar]
- 64.Vazquez-Prokopec GM, Stoddard ST, Paz-Soldan V, Morrison AC, Elder JP, Kochel TJ, et al. Usefulness of commercially available GPS data-loggers for tracking human movement and exposure to dengue virus. Int J Health Geogr. 2009;8: 1–11. doi: 10.1186/1476-072X-8-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Paz-Soldan VA, Stoddard ST, Vazquez-Prokopec G, Morrison AC, Elder JP, Kitron U, et al. Assessing and maximizing the acceptability of global positioning system device use for studying the role of human movement in dengue virus transmission in Iquitos, Peru. Am J Trop Med Hyg. 2010;82: 723–730. doi: 10.4269/ajtmh.2010.09-0496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Williams NE, Thomas TA, Dunbar M, Eagle N, Dobra A. Measures of human mobility using mobile phone records enhanced with GIS data. PLoS ONE. 2015;10: e0133630 doi: 10.1371/journal.pone.0133630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hergenrather KC, Rhodes SD, Cowan CA, Bardhoshi G, Pula S. Photovoice as community-based participatory research: a qualitative review. Am J Health Behav. 2009;33: 686–698. doi: 10.5993/AJHB.33.6.6 [DOI] [PubMed] [Google Scholar]
- 68.Woolhouse MEJ, Dye C, Etard JF, Smith T, Charlwood JD, Garnett GP, et al. Heterogeneities in the transmission of infectious agents: Implications for the design of control programs. Proceedings of the National Academy of Sciences of the United States of America. 1997;94: 338–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gryseels C, Durnez L, Gerrets R, Uk S, Suon S, Set S, et al. Re-imagining malaria: heterogeneity of human and mosquito behaviour in relation to residual malaria transmission in Cambodia. Malar J. 2015;14: 165 doi: 10.1186/s12936-015-0689-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gubler DJ. Human behaviour and cultural context in disease control. TropMedIntHealth. 1997;2: A1–A2. [PubMed] [Google Scholar]
- 71.Killeen G. Characterizing, controlling and eliminating residual malaria transmission. Malar J. 2014;13: 330 doi: 10.1186/1475-2875-13-330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wangroongsarb P, Satimai W, Khamsiriwatchara A, Thwing J, Eliades J, Kaewkungwal J, et al. Respondent-driven sampling on the Thailand-Cambodia border. II. Knowledge, perception, practice and treatment-seeking behaviour of migrants in malaria endemic zones. Malar J. 2011;10: 117 doi: 10.1186/1475-2875-10-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sumodan PK, Vargas RM, Pothikasikorn J, Sumanrote A, Lefait-Robin R, Dujardin J-P. Rubber plantations as a mosquito box amplification in South and Southeast Asia In: Morand S, editor. Socio-ecological dimensions of infectious diseases in Southeast Asia. Singapore: Springer Science Business Media; 2015. pp. 160–165. [Google Scholar]
- 74.Thammapalo S, Wonghiranrat W, Moonmek S, Sriplong W. Biting time of Aedes albopictus in the rubber plantations and the orchards, the southern-most of Thailand. J Vector Borne Dis. 2009;6: 2. [Google Scholar]
- 75.Paily KP, Chandhiran K, Vanamail P, Kumar NP, Jambulingam P. Efficacy of a mermithid nematode Romanomermis iyengari (Welch) (Nematoda: Mermithidae) in controlling tree hole-breeding mosquito Aedes albopictus (Skuse) (Diptera: Culicidae) in a rubber plantation area of Kerala, India. Parasitol Res. 2013;112: 1299–1304. doi: 10.1007/s00436-012-3265-3 [DOI] [PubMed] [Google Scholar]
- 76.Magris M, Rubio-Palis Y, Alexander N, Ruiz B, Galván N, Frias D, et al. Community-randomized trial of lambdacyhalothrin-treated hammock nets for malaria control in Yanomami communities in the Amazon region of Venezuela. Trop Med Int Health. 2007;12: 392–403. doi: 10.1111/j.1365-3156.2006.01801.x [DOI] [PubMed] [Google Scholar]
- 77.Sochantha T, Van Bortel W, Savonnaroth S, Marcotty T, Speybroeck N, Coosemans M. Personal protection by long-lasting insecticidal hammocks against the bites of forest malaria vectors. Trop Med Int Health. 2010;15: 336–341. doi: 10.1111/j.1365-3156.2009.02457.x [DOI] [PubMed] [Google Scholar]
- 78.Thang N, Erhart A, Speybroeck N, Xa N, Thanh N, Van KP. Long-lasting insecticidal hammocks for controlling forest malaria: a community-based trial in a rural area of central Vietnam. PLoS One. 2009;4: e7369 doi: 10.1371/journal.pone.0007369 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Summary of data obtained from the rapid participatory rural appraisals on the daily intensity of mosquito and human activity in different habitats.
(DOCX)
Summary of data obtained from the rapid participatory rural appraisals on the monthly intensity of environmental variables, mosquito activity, and human activity.
(DOCX)
The parity rate of the dengue vector Ae. albopictus and of the putative malaria vectors in the secondary forests, mature rubber plantations, immature rubber plantations, and villages.
(DOCX)
The average number of mosquito bites per person per day (ma) for the important vector species Ae. albopictus, An. maculatus s.l., An. minimus s.l., and An. dirus s.l. in the secondary forest, mature rubber plantation, immature rubber plantation and village habitats during the rainy season and dry season.
(DOCX)
Data Availability Statement
All data files are available from the DRYAD database: http://dx.doi.org/10.5061/dryad.8nf05.