Abstract
Introduction:
Modeling can be a useful tool to find out how the distributions of hospital length of stay (LOS) and the factors affecting the length of stay. The present study aims to determine factors affecting the length of stay and selecting suitable statistical models.
Material and Method:
this is a cross – sectional study of 565 patients who were treated in the intensive care unit of Imam Khomeini hospital in Ahwaz. Preliminary data were collected retrospectively through the medical records of all patients admitted on intensive care units of Ahwaz Imam Khomeini Hospital in 2015. Statistical analysis and multivariate regression models were done using of SPSS 21 and STATA 7 software.
Results:
Average length of stay in ICU was 8.16±0.75 days. The Mean and Median age of patients were 58.61±20 and 61 respectively, The Mean LOS for females (16.44±9.37 days) was more than the men (11.5±5.35 days) (p<0.01). The maximum and minimum lengths of stay belonged to patients with endocrine disorders (14.7±3.1 days) and patients with gastrointestinal disorders (5.53±1.1 days) respectively (p<0.01). The goodness of fit for Gamma model showed that this model was more suitable and powerful than Log-normal model to predict the factors affecting the patient’s length of stay in intensive care units of hospital.
Conclusion:
Gamma regression model was more robust to predict factors regarding the hospital length of stay. According to Gamma model the key factor in predicting the length of stay in ICU was the type of disease diagnosis. The result of statistical modeling can help managers and policy makers to estimate hospital resources and allocate them for different hospital services.
Keywords: length of stay, statistical modeling, ICU, teaching hospital
1. INTRODUCTION
Intensive care unit (ICU) is one of the critical parts of a hospital which can reduce the rate of mortality and side effects of hospitalization (1, 2). An increase in the length of stay and the hospital costs are the main problems of admitted patients in intensive care units (3). The LOS is the key indicators that use to plan for hospital resources in making plans for patients (4-6). Clinical, demographic, and managerial factors are impact on the hospital length of stay in ICU (7-14). Since the optimum use of resources plays an important role in enhancing the efficiency of hospitals, reducing the length of stay can led to increase hospital resources efficiency and effectiveness (15-16). To manage hospital beds and patients LOS in ICU we need to model hospital data (17).
Modeling is one of the basic tools used in explaining the medical and health phenomena. These tools determine the distribution of specific variables and their relations with other variables by means of regression statistic methods. Modeling the length of stay is a valuable way to know about the status of distribution of LOS (18). The effecting factors in the length of stay cannot be predicted by using common statistic methods like linear regression method since the useful variable because the distribution of LOS data is normal. Hospital length of stay data have a right skewness (19-20). LOS is a numerical discrete variable; therefore, numerical data distribution should be used to analyze them (17). To model the numerical discrete variable should be used the model which has been a suitable prediction power (18). Statistical models with different distribution can predict the length of stay, as well as the factors influencing it (21). Identifying a robust model with a high sensitivity to predict the factors affecting the length of stay can help hospital managers to control prolonged hospital length of stay. The present study aims to determine factors affecting the length of stay and theirs suitable statistical models.
2. MATERIAL AND METHODS
This is a cross-sectional study of 565 patients treated in the intensive care unit of Imam Khomeini hospital in Ahwaz. Preliminary data were collected retrospectively from medical records of all patients admitted to the intensive care unit from 1 January 2015 to 31 December 2015. To confirm the content validity of data form, we used the expert’s views about questions and variables. In this study According to Kolmogorov-Smirnov test, distribution of the dependent variable data was abnormal and had a right skewness. In this study six percent of the patients an intensive care units died on the first day (LOS=0), so zero data have not been included in modeling. First, data were analyzed by univariate tests. Including Mann- Whitney, kruskal - Wallis, and Spearman coefficient. Then we selected the significant variables to model by using multi-variate regression analysis and stepwise modeling method. In this study significant level was determined 0.01. In this study Log-normal model was used base on formular: In (y) = 0+1+, in which X variable data are made from even distribution (0, 1), ~N (0, 2), in which, σ2 = 0.5, 1.0, 1.5. 1=1 was used, 0 was estimated in this way:
E(y) =1:
E (ylx) =exp 0+1x+0.52)
Also Y variable skewness is as follows:
(Exp (2)+2)(Exp (2)-1)0.5
And also some data are produced by log- normal distribution with variances of 0.5, 1, 1.5 and 2. Also, GAMMA model was used based on following formula: Variable data from standard GAMMA with density function
In which scale parameter is b = exp (β0 + β1x). and are chosen in such a way that result will be and they are produced by parameters of 5,0,1,2,4. We used SPSS 21 and STATA 7 to analyze the data modeling.
3. RESULTS
Table 1 shows the demographic and clinical characteristics which influence the patients’ length of stay in intensive care unit. Average length of stay in ICU was 8.16±0.75 days. The Mean and Median age of patients were 58.61±20 and 61 respectively, The Mean LOS for females (16.44±9.37 days) was more than the men (11.5±5.35 days) (p<0.01). The maximum and minimum lengths of stay belonged to patients with endocrine disorders (14.7±3.1 days) and patients with gastrointestinal disorders (5.53±1.1 days) respectively (p<0.01). The lowest age group was 12 while the highest was 99.
Table 1.
Findings related to clinical and demographic variables affecting the length of stay in ICU
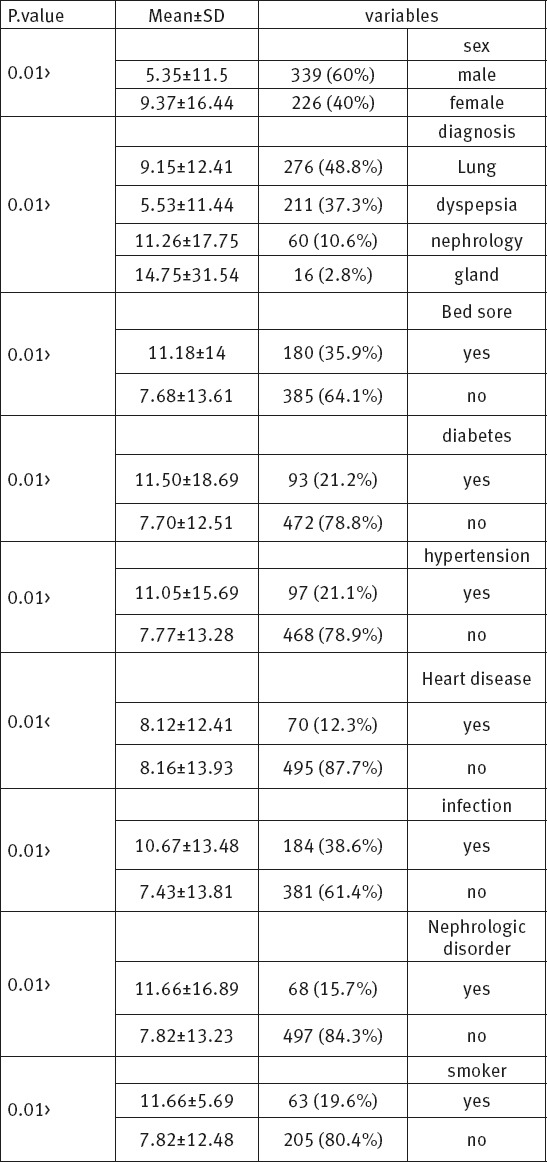
The intensive care unit included patients with pulmonary diseases (%48.8), dyspepsia (%37.3), nephrology disorder (%10.6) and endocrine disorders (%2.8). Patients with endocrine disorders (14.7±3.1 days) and those with dyspeptic diseases (5.53±1.1 days) had respectively the highest and lowest length of stay. The result shows that all patients had rehospitalization history. The result of the study showed that 48.3 percent of the patient ICU died. Diagram 1 shows the data distribution of the patients’ length of stay.
Diagram 1.
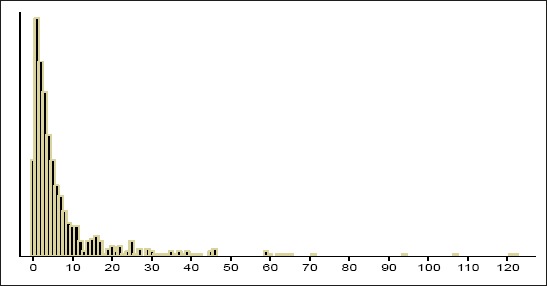
Data distribution of LOS
The distribution of the patients’ length of stay was from 0 to 122 days. Most patients (%16.6) stayed in intensive care unit 1 day and 6 percent of patients stayed zero (0) day. According to Table 2, comparison between log-normal regression model and Gamma model showed that in Gamma model type of diagnosis (β= -.5493982; CI= [-0.9413864,–0.15741]) variable was significant. Factors to predict length of stay in ICU in Log – normal model:
Table 2.
Relation between LOS and demographic and clinical variables by using log-normal and Gamma regression. 1. Fast blood sugar, 2. Blood Sodium, 3. Refrence Category 4. Bayesian information criterion 5. Akaike information criterion, *P<0.05, **P<0.01
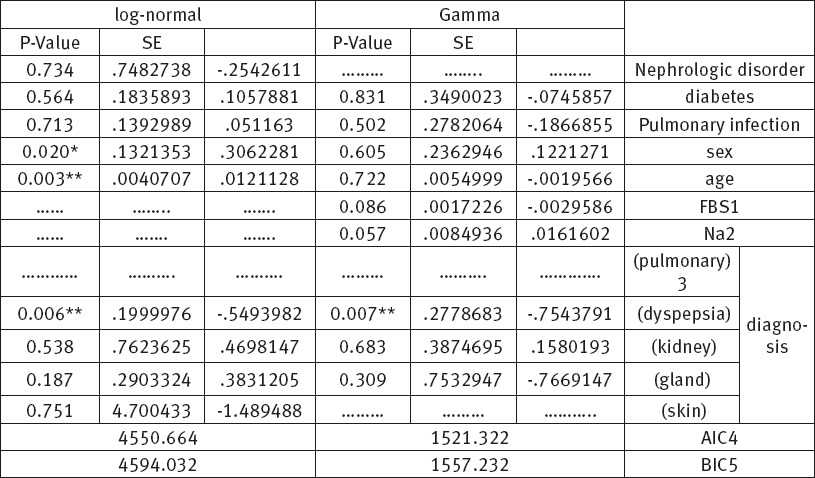
a) Age (β=0.0200913; CI= [0.0121126, 0.0041343]),
b) Sex (β=0.5652086; CI= [0.3062281, 0.472476]), and
c) Type of diagnosis ((β= -.7543791; CI= [-1.298991,–0.2097672])) were significant factors affecting the length of stay.
Gamma model showed that patient with dyspepsia had a significant shorter length of stay than other patients. According to AIC and BIC test, Gamma model was better than Log-normal model to predict factor affecting the LOS in ICU patients.
4. DISCUSSION
The present study aims to determine factors affecting the length of stay and selecting suitable statistical models. LOS data are right skewness to model skew data; we use Gamma and Log-normal regression to model skewed data (21). In this study, affecting factors LOS were assessed, the result of univariate regression analysis showed that increase of age of patients led to increase in LOS. Some study also showed that increase of patient age led to increase in LOS (22-28).
Most patients hospitalized in intensive care unit were elderly people, so managers and policy makers are recommended to make suitable plans and programs which can better provide necessary services for aging people.
The result of study showed that 35.9% of patient had a bedsore and the patient with Bedsore had longer LOS than other patients. Also some study showed that Bedsore led to increase LOS in ICU (22-24).
So due to the meaningful relation between bedsore and LOS by making suitable plans to control and prevent bedsore we can shorten the patients’ length of stay and speed up their recovery. Considering the following points can help prevent and lessen bed sore in patients: Planning and implementing protocol in order to idenfity the patients in danger before admission to ICU. Paying special attention by unrses and hospital staff to elderly patients, women, patients with long periods of stay, those refered from other hospitals or centers, patients with physical disorders and patients with low consciousness, diabetes, fever, infection, hypertention and respiratory diseases.
Forming and activating a committee or community attended by nurses, doctors, units officials and high ranking hospital managers in order to hold regular meetings in which the bottom cause and the solution of this problem (bed sore) are discussed and units with more problems are identified.
Identifying patients in danger of bedsore before admission along with a particular attention to the factors creating it can be effective in preventing this problem. It seems that designing and using special forms for examining the risk of bedsore before admission is necessary. Other studies show that bed sore has a meaningful relation with an increase in length of stay in ICU (22-24). According to the result, 38.6% of patients had hospital infections. Univariate analysis showed that patient with hospital infection had significantly longer LOS than other patients. Some study showed that hospital infection led to increase LOS in ICU (25-27).
So because of the high rate of hospital infections and the significance of controlling them to reduce medical loss and the length of stay in ICU it is necessary to identify the factors which cause these hospital infections in order to take efficient steps that consequently lead to a decrease in LOS.
In other studies the meaningful effect of hospital infections on the length of stay in ICU was clearly demonstrated (25-27). In this study, risk factors including (diabetic, hypertension, and smoking) significantly impact on length of stay in ICU. Also some study showed that clinical and demographic variables significantly impact on LOS in ICU and hospital (22-28). Therefore hospital managers and clinicians can use the managerial and clinical methods to manage LOS patients with infection and Bedsores.
In order to decrease length of stay in ICU patients we used Gamma and Log-normal model. According to Log-normal model age, sex, and type of diagnosis were significant factors to predict length of stay in ICU.
According to Gamma model, Type of diagnosis variable was significant to predict length of stay in ICU. In this study BIC and AIC test showed that Gamma model was more robust than Log- normal model to predict affecting factors length of study. The study by Saki et al showed Gamma model has a better efficiency, sensitivity and prediction ability to predict affecting factors (19).
5. CONCLUSION
The results of this study showed that in comparison to other statistic models Gamma model had stronger ability in predicting the length of study. Choosing a suitable statistic model will enhance managers and policy makers’ ability to organize hospital resources in an optimum way, furthermore comprehensive and exact information about the average length of stay can be useful for managers better physical, financial and strategic hospital planning.
Acknowledgments
This study is part of M.Sc. thesis for Laleh Gharacheh. This work was financially supported by grant: U-95083 from the Vice-Chancellor for Research Affairs of Ahvaz Jundishapur University of Medical Sciences. The authors would like to thank all participants in this research.
Footnotes
• Conflict of interest: none declared.
REFERENCES
- 1.Marzban S, Maleki M, Nasiri Pour A, Jahangiri K. Assessment of patient safety management system in ICU. JQUMS. 2013;17(5):45–55. [Google Scholar]
- 2.Golaghaie F, Sarmadian H, Rafiie R, Nejat N. A study on waiting time and length of stay of attendants to emergency department of Vali-e-Asr Hospital, Arak-Iran. Journal of Arak University of Medical Sciences. 2008;11(2):74–83. [Google Scholar]
- 3.Besharati R, Sadeghian A, Mamori G, Lashkardoost H, Gholami S. Sources of bacteria causing nosocomial infections At NICU of Ghaem Hospital in Mashhad, Iran. Journal of North Khorasan University of Medical Sciences. 2013;5(1):25–9. [Google Scholar]
- 4.Pourreza A, Salavati S, Sadeghi darvishi S, Salehi Nasab M, Tabesh H, Mamivand F, et al. Factors influencing the length of stay in infectious ward of Razi hospital in Ahvaz: Iran. Health Inf Manage. 2015;11(6):779–88. [Google Scholar]
- 5.Ravangard R, Arab M, Zeraati H, Rashidian A, Akbarisari Niroomand N, Mansoori S. A Study of Patient Length of Stay in Tehran University of Medical Sciences Obstetrics and Gynecology Specialty Hospital and its Associated Clinical and Nonclinical Factors. Hakim Health Sys Res. 2010;13(2):129–36. [Google Scholar]
- 6.Ravangard R, Arab M, Rashidian A, Akbarisari A, Zare A, Salesi M, et al. Hospitalized patients’ length of stay and its associated factors in Tehran University of Medical Sciences Women’s Hospital using the survival analysis method. sjsph. 2010;8(3):25–35. [Google Scholar]
- 7.Arab M, Zarei A, Rahimi A, Rezaiean F, Akbari F. Analysis of Factors Affecting Length of stay in Public Hospitals in Lorestan Province, Iran. Hakim Health Sys Res. 2010;12(4):27–32. [Google Scholar]
- 8.Rezaei Hachesoo P, Ahmadi M, Alizadeh S, Sadoughi F. Use of data mining techniques to determine and predict length of stay of cardiac patients. Health Inform Res. 2013;19(2):121–9. doi: 10.4258/hir.2013.19.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang J, Harvey C, Andrew C. Factors associated with length of stay and the risk of readmission in an acute psychiatric inpatient facility: a retrospective study. Aust N Z J Psychiatry. 2011;45(7):578–85. doi: 10.3109/00048674.2011.585452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Soyiri IN, Reidpath DD, Sarran C. Asthma length of stay in hospitals in London 2001–2006: demographic, diagnostic and temporal factors. PloS One. 2011;6(11):1–5. doi: 10.1371/journal.pone.0027184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martin S, Smith P. Explaining variations in inpatient length of stay in the National Health Service. J Health Econ. 1996;15(3):279–304. doi: 10.1016/0167-6296(96)00003-3. [DOI] [PubMed] [Google Scholar]
- 12.Gohari M, Vahabi N, Moghadamifard Z. Semiparametric Cox regression for factors affecting hospitalization length. Daneshvar. 2012;19(99):23–30. [Google Scholar]
- 13.Etminani K, Naghibzadeh M, Pena JM, Democratic OP. A democratic way of aggregating Bayesian network parameters. Int J Approx Reason. 2013;54(5):602–14. [Google Scholar]
- 14.Etminani K, Naghibzadeh M, Razavi AR. Effective pruning strategies for branch and bound Bayesian networks structure learning from data. Scientica Iranica. 2013;20(13):682–94. [Google Scholar]
- 15.Nasiripour A, Riahi L, Gholamipour A. Presence of fulltime medicos in hospital and its effect on length of stay of Yazd hospital. Medical Military Organization of Islamic Republic of Iran Journal. 2010;28(2):169–75. [Google Scholar]
- 16.Soltani M H, Sahaf R, Mohammadi Shahbolaghi F, Ghaffari S, Khosravi A, Gohari MR. Elderly, Duration of Hospitalization and Hospital Cost in Milad Hospital in Iran. Salmand. 2012;6(1):58–65. [Google Scholar]
- 17.Golaghaie F, Sarmadian H, Rafiie R, Nejat N. A study on waiting time and length of stay of attendants to emergency department of Vali-e-Asr Hospital, Arak-Iran. Journal of Arak University of Medical Sciences. 2008;11(2):74–83. [Google Scholar]
- 18.Pourreza A, Salavati S, Sadeghi darvishi S, Salehi Nasab M, Tabesh H, Mamivand F, et al. Factors influencing the length of stay in infectious ward of Razi hospital in Ahvazs. 2014;11(6):779–88. [Google Scholar]
- 19.Basu A, Manning WG, Mullahy J. Comparing alternative models: log vs Cox proportional hazard? Health economics. 2004;13(8):749–65. doi: 10.1002/hec.852. [DOI] [PubMed] [Google Scholar]
- 20.Mihaylova B, Briggs A, O’Hagan A, Thompson SG. Review of statistical methods for analyzing healthcare resources and costs. Health economics. 2011;20(8):897–916. doi: 10.1002/hec.1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saki Malehi A, Pourmotahari F, Ahmadi Angali K. Statistical models for the analysis of skewed healthcare cost data: a simulation study. Health Economics Review. 2015;5(11):1–16. doi: 10.1186/s13561-015-0045-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nayak D, Srinivasan K, Jagdish S, Rattan R, Chatram VS. Bedsores: “top to bottom” and “bottom to top”. Indian J Surg. 2008;70(4):161–8. doi: 10.1007/s12262-008-0046-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Afkar A, Mahboubi M, Mehrabian F, Farmanbar R, Ghahramani F, Kazem Nezhad E, et al. Predictive factors of ICU bedsores using Braden scale. journal of Kermanshah University of Medical Sciences. 2012;8(4):220–5. [Google Scholar]
- 24.Beheshti Zavare Z, Arab M, Rashidian A, Golestan B. Factors affecting pressure ulcer in the ICU units of Tehran University of Medical Sciences teaching hospitals. SJSPH. 2010;8(3):81–92. [Google Scholar]
- 25.Shakib P, Lavakhamseh H, Mohammadi B. The prevalence of nosocomial infection in ICU, Besat Hospital, Sanandaj City, Iran. Zanko J Med Sci. 2014;15(45):36–41. [Google Scholar]
- 26.Ghiasvandian S. Nosocomial infection in the Intensive Care Unit. Hayat. 2002;8(1):27–34. [Google Scholar]
- 27.Dadmanesh M, Dormanesh B, Ghasemzadeh S, Ghorban Kh, Zahirian S. Evaluation of nosocomial urinary tract infection in the intensive care unit patients at Tehran 501 hospital during 2007. Journal of Army University. 2008;5(4):1407–10. [Google Scholar]
- 28.Rezaei Hachesoo P, Ahmadi M, Alizadeh S, Sadoughi F. Use of data mining techniques to determine and predict length of stay of cardiac patients. Health Inform Res. 2013;19(2):121–9. doi: 10.4258/hir.2013.19.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]


