Abstract
Introduction:
Today, the structure of comprehensive health care emphasizes self-care more than therapy. Medication therapy is a strong instrument for therapy received through the health setting, especially in medication area. Error in medication administration has produced different problems and they cost billions of dollars every year. Regarding mobile phone extensions, we developed a local medication reminder mobile application called “Seeb” as a suitable solution for decreasing medication errors for Iranians.
Methods:
We conducted a mixed methods study in three Phases: 1) Comparative study of existing mobile applications; 2) developed its object-oriented model; 3) Developed the initial version of “Seeb” that was approved for production.
Results:
This application was designed for the appropriate medication administration including time and dosages through: recording patient and medication data; scheduling patients’ medication; and reporting medication administration on progress.
Conclusion:
“Seeb” has been designed in compliance with Iranian health information technologists and pharmacists requirements. It is expected to reduce medication error and improve patient adherence to medical prescriptions.
Keywords: Medication Reminder, Mobile Application, Medication Errors
1. INTRODUCTION
Discharged patients from hospitals need more medication order compliance (1); creating the essential conditions for reviewing the patient medication administration orders after discharge decreases the hospitalization and mortality, and increases patient quality of life (2). One of the factors that are known as the medical errors is lack of patient adherence to physician orders (3). Five percent of hospitals’ admissions are because of medication errors that patients themselves commit. The most common patients’ errors are their incorrect interpretation of physician orders and the ambiguities in relation to the medication administration (4). The safety improvement of the medication therapy is more important in outpatient care because prescribed medications have different types and variations. (5, 6). Medical orders non-adherence is the most important problem of the health system. Medications’ non-adherence causes almost between 33 and 69 percent of the hospitalization and 23 percent of the nursing home services in the U.S. It costs 100 billion dollars for the health system. Apart from the kind of disease, medications interactions, and the quality of patient non-adherence schedules measures, the medication non-adherence mean in chronic diseases is about 50 percent (6, 7).
Medication orders non-adherence in intentional and accidental cases includes: forgetting to take the medication because of amnesia or dizziness (8), the incorrect dose administration, medication complexity because of the poly pharmacy (9, 10), lack of enough information for the correct administration of the medication (11), incorrect timing, the incorrect use of the instruments of the medication administration such as inhalation medications, lack of enough self-confidence for managing the disease, lack of enough awareness from the disease condition, the complications resulting from re-consumption of the medication prescription which shouldn’t have been used again, and the less relationship between the patient and health services provider (12, 13).
Medication non-adherence has some consequences such as: the decrease in the effectiveness of the patient treatment, lack of the disease control, weak clinical outcomes like the development of preventable diseases, medication side effects, the reduction in quality of life, disability, and even death, creating the poor economic outcomes, and the growing use of health resources (13). Therefore Information technology solutions can help patients to manage the medication administration (14) and to reduce medication errors (15).
Figure 1.
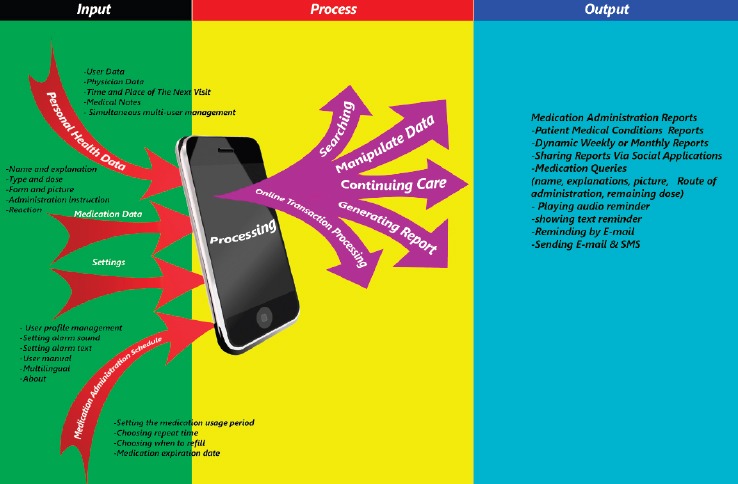
Model of the medication reminder mobile application called “Seeb”
World Health Organization (WHO)encourages the utilization of new technologies in providing health care in societies with not enough resources (16). Today, regarding availability of powerful computer resources and mobile devices, mobile health systems field has been developed with following benefits: availability of necessary hardware and applications, easy use, time saving for users, and great economic benefits (17, 18). In developing countries, smart phones have remarkable effects on health outcomes. Smart phones make opportunities for decreasing costs and increasing achievement to the services to improve the efficiency and the effectiveness of health care processes (19).
The technology of the smart phones is being developed quickly in the health system. There are 10 billion users of the smart phones and personal digital assistants (PDA) in the world. 90 percent of the people in the world and 80 percent of the villagers have cellphones (20, 21). Due to availability and ease of use, number of clinical decision support systems is increasing (22). The technology of smart phones has a lot of potentials for improving the results of the medication adherence in the health system. This technology increases patients’ awareness, improves therapy results, encourages the change of the patients’ behavior, and improves the health care provider participation in limited resource constraints (23).
The application of smart phones is a new approach for improving medication adherence and patient training. This function will be done by developing and distributing specialty mobile applications which users can easily download and use. Therefore, the localized medication reminder mobile application called “Seeb” was developed in compliance with experts’ opinions (including health information technologists and pharmacists) as a clinical decision support system to help outpatients for making correct decisions about the timing and dosage of their medication and preventing errors in medication administration, side/adverse effects and billions of dollars cost every year.
2. MATERIAL AND METHODS
This is a mixed method study that is going to be conducted in three phases from 2014 to 2016 as followings:
Phase 1: Comparative study of some existing mobile applications and providing a comparative model for Iran: In the first step of this phase, we searched for medication reminder mobile applications and their related articles to identify features of the applications. In this step, we analyzed content of eleven mobile applications (Drug reminder; On time-RX: On time Android pill reminder; Med minder Software; Medisafe; My pill box; I pharmacy; Dose cast; Med helper in English language and 3 in Persian: Yadavare darooei (“medication reminders” in Persian); Daroonama (“medication demonstrator” in Persian) Daroohat yadet nareh(“Do not forget your medications”) because of the easy installation and availability. We extracted all their features and attributes and recorded on the “data extracted form” and classified them as application functions and elements of each function in input, process, and output.
In the second step, the extracted features, which were common in 50 percent of the applications, were selected for comparative model of “Seeb”. In order to assess the validity of the comparative features and attributes, a research-made questionnaire was developed on the basis of the selected entities (with 88 questions). The reliability (Cronbach’s Alpha=0.964) and content validity of the questionnaire was confirmed. Then, the questionnaire was distributed through two rounds of Delphi technique. It was filled by 50 experts of health information technology and pharmacology professionals and the results were analyzed.
In the third step of this phase, the comparative modal of “Seeb” was prepared with study participants.
Phase 2: Developing its object-oriented model: The conceptual modal of Seeb application was designed through drawing unified modeling language (UML) diagrams, which include five kinds of diagrams as followings: Class diagram, Package diagram, Use-case diagram, and Sequence diagram.
Phase 3: Providing Seeb application: In this Phase, using Android Studio software, we developed the initial version of physical model for medication reminder mobile application according to the findings of comparative and conceptual model. The developed application can be installed on Android operating system version 4-6.
2. RESULTS
By content analysis on 11 different models, 88 features were extracted in three parts of input, processing, and output. Some of them had commonly been used in different mobile applications, but there were some features that had been used unique in some models and received special data from the user. After completing the questionnaire during two rounds of Delphi technique, the agreement was done on the required features of the prototype design of the medication reminder mobile application that include submitting user information, setting reminder of the medication administration, and the insert of the medication picture to show while warning, reporting the patient medication and setting alarms.
How to perform tasks in the software apples are as follows:
Input: Inputs are directly entered by a user; including demographic, medication and medical data. The base of “Seeb” inputs has been provided according to studied applications inputs.
Process (The application functions): patient data processed through the formulas.
Output: Includes the results of data analysis and reports.
3. DISCUSSION
Patients Knowledge of the proper medication administration is not enough; so it is necessary to adopt appropriate methods for rational medication administration by different walks of life. According to the results of Iranian medication reminder applications’ content analysis, there are few applications that are available by application markets in Persian. Some features of these apps include:
Reminding the patient’s medication to one of his/her friends or nurses.
Availability of User Guide, including guidance symbols and shapes.
Reminder remains in the phone’s memory, even If the device is switched on and off.
Inserting medications’ pictures and showing a simple report of the number of taken and canceled promises.
Recording the patient’s personal health data to report along with his/her taken medications, demographic, medical and pharmaceutical data.
These studied applications have the simultaneous multi-users ability. Therefore, entering each user data can be caused to differentiate him/her from others.
Employing of the mentioned features in “Seeb” creates a database from the patient and his/her conditions. After the software asks the user questions and measures, it records the medical information and finally shows a report of the patient conditions (blood pressure, diabetes, and weight trend).
In “Seeb”, to record the complete medication information, administration methods, and the medication schedule, we created the function of the medication data and its scheduling record and the users must enter the requested data. The following features were extracted from studied applications and were considered in “Seeb”: medication name and descriptions; type and the amount of the medication; Insertion of the medication picture; record of medication administration instruction; record of the user reaction to the medication warning (medication administration or non-administration); medication administration schedule (The time of the first and last medication administration, the repeat hours of administration, medication refill reminder, and medication expiration date). This function decreases medication errors such as the medication administration in the unsuitable time and dose, or wrong medication administration (24).
Fulfillment of outpatients’ prescribed medication is an important part of the self-care process, because it is related to patient safety and it can cause serious problems for patients’ health as well as threatening their safety. At the time of taking the medication, the following principles can greatly reduce medication errors: Identifying right patient, Identifying and selecting the right prescribed medication, correct time of administration, correct dose, and right taking way. Therefore, complete reporting of administered and non-administered medication is essential. Regarding all mentioned features such as the user reaction to the medication consumption reminder, “Seeb” creates a complete report of administered and non-administered medication number that can help both providers and patients to increase medication adherence, in line with saghaeiannejad-Isfahani, Yazdanshenas and Anglada-Martinez (25-27).
Personal space should be conducive to achieving privacy, independence, security and identity. Security and privacy in “Seeb” improves users’ information security and privacy. According to Kalakoti and Rodriguez-Feliz, this function leads to lack of other people access to the patient medical information (28-29). Some components of this function are as the followings: Application security with user name and password; Backup application data; and Ability to select backup storage and clear the application data. We believe that user control over own health care data and the impossibility of entering his/her privacy can leads to a decrease in feelings of fear and insecurity as well as increasing patient confidence and satisfaction.
In the studied application, reporting medical conditions and medications administration analysis divided into two parts: “weekly or monthly report of the medication administration” and “weekly or monthly report of vital signs measures”. “Seeb”, reports analysis of blood pressure, diabetes, and weight, as well as administered or non-administered prescribed medications. This function improves health service quality by following Treatment and decreasing the medication errors by sharing reports to the physician or health care providers (30-31).
4. CONCLUSION
Nowadays, using smart phones and mobile applications are increased dramatically, so developing mobile applications in health services (especially self-care) can create the desired effect in the community. Although there are various medication reminder mobile applications, a native mobile application is essential that is developed on the basis of the specialists’ ideas in this field. In addition to remind the medication administration time and dose, “Seeb” reports the analysis of the patient medication administration, as well as displaying suitable picture of the medication and its administration method when reminded of medication use. Existence of these functions in the medication reminder mobile application prevents medication errors by patients and increases medication adherence.
Undoubtedly, “Seeb” can play an important role in patient health improvement with the suitable reminder of the medication administration by user friendly interfaces, data processing, correct calculation of formulas and appropriate responds, the display of the medication pictures and descriptions. Therefore, we suggest that health care providers increase patients’ awareness and introduce them medication reminder mobile applications to promote these applications utilization and to improve medication adherence as well as decreasing medication errors.
•Acknowledgements:
This article was part of a research project (Master thesis) supported by Isfahan University of Medical Sciences (Grant No.: 395219). We extend our sincere thanks to the experts of health information technology and pharmacology professionals in Isfahan University of Medical Sciences.
Footnotes
• Conflict of interest: none declared
REFERENCES
- 1.Grober-Gratz D, Waldmann UM, Metzinger U, Werkmeister P, Gulich M, Zeitler HP. Reasons of Changes in Drug Therapy after Hospital Discharge - A Qualitative Study of Perception by General Practitioners and Patients. Gesundheitswesen. 2014;76(10):643–8. doi: 10.1055/s-0033-1351239. [DOI] [PubMed] [Google Scholar]
- 2.Vasbinder EC, Goossens LMA, Rutten-van Molken M, de Winter BCM, van Dijk L, Vulto AG, et al. e-Monitoring of Asthma Therapy to Improve Compliance in children (e-MATIC): a randomised controlled trial 75. Eur Resp J. 2016;48(3):758–67. doi: 10.1183/13993003.01698-2015. [DOI] [PubMed] [Google Scholar]
- 3.Anderson JG, Jay SJ, Anderson M, Hunt TJ. Evaluating the capability of information technology to prevent adverse drug events: a computer simulation approach. Journal of the American Medical Informatics Association. 2002;9(5):479–90. doi: 10.1197/jamia.M1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mira JJ, Ortiz L, Lorenzo S, Royuela C, Vitaller J, Pérez-Jover V. Oversights, confusions and misinterpretations related to self-care and medication in diabetic and renal patients. Medical Principles and Practice. 2014;23(3):246–52. doi: 10.1159/000358225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Novo A, Masic I. Ensuring patient safety. Med Arh. 2007;61(4):262–3. [PubMed] [Google Scholar]
- 6.Stawarz K, Cox AL, Blandford A. Don’t forget your pill!: Designing effective medication reminder apps that support users’daily routines. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. 2014 ACM. [Google Scholar]
- 7.Dayer L, Heldenbrand S, Anderson P, Gubbins PO, Martin BC. Smartphone medication adherence apps: potential benefits to patients and providers. Journal of the American Pharmacists Association. 2013;53(2):172–81. doi: 10.1331/JAPhA.2013.12202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garfield S, Eliasson L, Clifford S, Willson A, Barber N. Developing the Diagnostic Adherence to Medication Scale (the DAMS) for use in clinical practice. BMC Health Serv Res. 2012;12(350):1472–6963. doi: 10.1186/1472-6963-12-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mira JJ, Navarro I, Botella F, Borras F, Nuno-Solinis R, Orozco D, et al. A Spanish pillbox app for elderly patients taking multiple medications: randomized controlled trial. J Med Internet Res. 2014;16:4. doi: 10.2196/jmir.3269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koper D, Kamenski G, Flamm M, Bohmdorfer B, Sonnichsen A. Frequency of medication errors in primary care patients with polypharmacy. Fam Pract. 2013;30(3):313–9. doi: 10.1093/fampra/cms070. [DOI] [PubMed] [Google Scholar]
- 11.Siu HY, Mangin D, Howard M, Price D, Chan D. Pilot Feasibility Stud. 2017;3(5):016–0118. doi: 10.1186/s40814-016-0118-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Porter G, Grills N. Medication misuse in India: a major public health issue in India. J Public Health. 2016;38(2):8. doi: 10.1093/pubmed/fdv072. [DOI] [PubMed] [Google Scholar]
- 13.Hall RL, Willgoss T, Humphrey LJ, Kongso JH. The effect of medical device dose-memory functions on patients’ adherence to treatment, confidence, and disease self-management. Patient Prefer Adherence. 2014;8:775–88. doi: 10.2147/PPA.S61248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gabriel M, Gagnon JP, Bryan CK. Improved patients compliance through use of a daily drug reminder chart. Am J Public Health. 1977;67(10):968–9. doi: 10.2105/ajph.67.10.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Isfahani SS, Raeisi AR, Ehteshami A, Janesari H, Feizi A, Mirzaeian R. The role of evaluation pharmacy information system in management of medication related complications. Acta Inform Med. 2013;21(1):26–9. doi: 10.5455/AIM.2012.21.26-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bigna JJ, Noubiap JJ, Kouanfack C, Plottel CS, Koulla-Shiro S. Effect of mobile phone reminders on follow-up medical care of children exposed to or infected with HIV in Cameroon (MORE CARE): a multicentre, single-blind, factorial, randomised controlled trial. Lancet Infect Dis. 2014;14(7):600–8. doi: 10.1016/S1473-3099(14)70741-8. [DOI] [PubMed] [Google Scholar]
- 17.Masic I, Begic E. Mobile Clinical Decision Support Systems in Our Hands - Great Potential but also a Concern. Studies in health technology and informatics. 2016;226:63–6. [PubMed] [Google Scholar]
- 18.Masic I, Begic E, Begic N. Use and Knowledge on the Information Technologies in Medical Education - Bosnian and Herzegovinian Experience. Mater Sociomed. 2016;28(2):84–90. doi: 10.5455/msm.2016.28.84-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Klasnja P, Pratt W. Healthcare in the pocket: mapping the space of mobile-phone health interventions. J Biomed Inform. 2012;45(1):184–98. doi: 10.1016/j.jbi.2011.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turakhia MP, Kaiser DW. Transforming the care of atrial fibrillation with mobile health. J Interv Card Electrophysiol. 2016;47(1):45–50. doi: 10.1007/s10840-016-0136-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tamrat T, Kachnowski S. Special delivery: an analysis of mHealth in maternal and newborn health programs and their outcomes around the world. Matern Child Health J. 2012;16(5):1092–101. doi: 10.1007/s10995-011-0836-3. [DOI] [PubMed] [Google Scholar]
- 22.Begić E, Mandžuka M, Begić Z, Dobrača A, Hasanbegovic E. CMBEBIH 2017. Springer; 2017. Antihypertensive therapy dosage calculator; pp. 660–5. [Google Scholar]
- 23.Kliner M, Knight A, Mamvura C, Wright J, Walley J. Using no-cost mobile phone reminders to improve attendance for HIV test results: a pilot study in rural Swaziland. Infect Dis Poverty. 2013;2(1):2049–9957. doi: 10.1186/2049-9957-2-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siebert JN, Ehrler F, Combescure C, Lacroix L, Haddad K, Sanchez O, et al. A Mobile Device App to Reduce Time to Drug Delivery and Medication Errors During Simulated Pediatric Cardiopulmonary Resuscitation: A Randomized Controlled Trial. J Med Internet Res. 2017;19:2. doi: 10.2196/jmir.7005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saghaeiannejad-Isfahani S, Sharifi-Rad J, Raeisi A, Ehteshami A, Mirzaeian R. An evaluation of adherence to society of pharmacists’ standards care in pharmacy information systems in Iran. Indian J Pharmacol. 2015;47(2):190–4. doi: 10.4103/0253-7613.153428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yazdanshenas H, Bazargan M, Jones L, Seto T, Vawer M, Farooq S, et al. Improving Acceptability and Usability of Mobile Health Technologies to Increase Medication Adherence among Hypertensive Minority Older Adults. Gerontologist. 2016:56. [Google Scholar]
- 27.Anglada-Martinez H, Riu-Viladoms G, Martin-Conde M, Rovira-Illamola M, Sotoca-Momblona JM, Codina-Jane C. Does mHealth increase adherence to medication? Results of a systematic review. International Journal of Clinical Practice. 2015;69(1):9–32. doi: 10.1111/ijcp.12582. [DOI] [PubMed] [Google Scholar]
- 28.Kalakoti P, Sharma K, Harsh V, Haque FA, Veeranki SP. Use of mobile applications in neurosurgery: Are we compromising on patient confidentiality and privacy? Neurol India. 2015;63(4):641–U209. doi: 10.4103/0028-3886.162139. [DOI] [PubMed] [Google Scholar]
- 29.Rodriguez-Feliz JR, Roth MZ. The Mobile Technology Era: Potential Benefits and the Challenging Quest to Ensure Patient Privacy and Confidentiality. Plast Reconstr Surg. 2012;130(6):1395–7. doi: 10.1097/PRS.0b013e31826d9d81. [DOI] [PubMed] [Google Scholar]
- 30.Anderson K, Emmerton LM. Contribution of mobile health applications to self-management by consumers: review of published evidence. Aust Health Rev. 2016;40(5):591–7. doi: 10.1071/AH15162. [DOI] [PubMed] [Google Scholar]
- 31.Webb K, Bullock A, Dimond R, Stacey M. Can a mobile app improve the quality of patient care provided by trainee doctors? Analysis of trainees’ case reports. BMJ Open. 2016;6:9. doi: 10.1136/bmjopen-2016-013075. [DOI] [PMC free article] [PubMed] [Google Scholar]


