Abstract
Objective:
The aim of this study was to assess the importance of early diagnosis of potentially malignant lesions in the prevention of oral cancer.
Material and methods:
In order to achieve the set objectives, we selected our participant pool. Of the 340 patients who came to the initial examination at the Clinic for Oral Medicine and Periodontology, we selected 40 patients with potentially malignant oral lesions (PMOL) of both sexes and of different ages. After an extensive anamnesis and a clinical examination of all mucous membranes, we documented potentially malignant lesions, their localization, subjective and objective symptoms, duration of pathological lesion, and bad habits (smoking and alcohol). All lesions were colored with Toluidine blue, which indicates malignancy in 75% of cases. Patients who had a positive Toluidine blue staining test were sent to biopsy and pathohistological analysis.
Results:
The most common potentially malignant lesions are Lichen reticularis (25%), Lichen erosivus (20%), and Leukoplakia (15%). The most common localization of lesions is the buccal mucosa bilaterally (26%), buccal mucosa unilaterally (10%), and the lower lip (10%). The staining test with Toluidine blue was positive at 23% PMOLs. In patients with positive Toluidine staining findings, biopsy and pathohistological analysis were performed, which showed that 20% of all lesions are carcinoma (CIS, Baseocellular Carcinoma, Squamocellular Carcinoma), while 14% are mucosal epithelial dysplasia. Statistical analysis confirmed the significance of positive staining of Toluidine blue and Leukoplakia (Spearman’s coefficient = 0.427, p = 0.006, N = 40), and statistically significant positive association of Squamocellular Carcinoma and Toluidine blue staining (Spearman’s coefficient = 0.619, p = 0.000, N = 40).
Conclusion:
Most oral cancers are caused by potentially malignant lesions, which is why a very detailed clinical examination with the visualization of pathological lesions is very important. Toluidine blue test can be an auxiliary tool for clinical diagnosis but does not replace the pathohistological finding. Biopsy and pathohistological findings are the gold standard in the diagnosis of oral cancers, as confirmed in our research.
Keywords: oral cancer, potentially malignant lesions, Toluidine test, biopsy
1. INTRODUCTION
Oral cancer is a carcinoma that occurs in the oral cavity and belongs to the group of head and neck tumors. Malignant oral cavity tumors account for about 3-5% of all tumors. According to epidemiological data, oral cavity cancer is the sixth most frequent among all types of cancer, and one of the ten most common causes of death, with an incidence of 10 in 100,000 people.
The most common type is squamous cell carcinoma that makes up 90% of all malignant tumors (1, 2, 3). Oral cancer accounts for about 4% of all malignant tumors in men, and 2 % in women, of an average age of about 60, although an increase in incidence has been recorded recently in people of younger age (4). The main etiologic factors for the development of oral cavities cancers are smoking, alcohol consumption, sun exposure, liver cirrhosis, dietary deficiencies, viruses, chronic tooth injuries, etc (5, 6, 7). Oropharyngeal carcinoma belongs to the group of the most malignant tumors, given the fact that the survival rate is about 50%. Although the oral cavity is accessible for visual examination, oral cancers are generally diagnosed late. Lack of awareness in patients and the phase of negation and ignoring the symptoms are the reasons for not seeing a doctor right away, and is considered the “first loss of time”. The “second loss of time” occurs due to lack of awareness of medical and dental professionals and the lack of a timely diagnosis. The “third loss of time” is the period that passes from the diagnosis to the commencement of treatment (8). It is important to reduce the “first loss of time” by increasing awareness of the importance of self-examination, and to shorten the “second loss of time” through education of medical and dental staff.
Oral cancers mostly develop from potentially malignant lesions (precancerouses). Potentially malignant lesions (PML) are lesions of the oral mucosa which are at an increased risk for malignant transformation compared to healthy mucosa. At the congress of the World Health Organization in 2005, “potentially malignant diseases” was suggested as a term for malignant and precancerous conditions (9,10). The most common precancerous lesions are leukoplakia, erythroplakia, oral lichen planus, and actinic cheilitis. Leukoplakia is a white spot or plaque which cannot be clinically nor histologically characterized as any other lesion, and is not associated with any physical or chemical causal factor, aside from the use of tobacco (Figure 2). According to epidemiological data, general prevalence of leukoplakia ranges from 0.6% to 4.6%. It is most common in men of middle and older age. Cancer will develop from rom leukoplakia in 1-20% of cases. The main activators of cancerization are exogenous factors such as smoking, alcohol, human papilloma virus, or chewing betel (11). According to clinical studies, the most common site of malignant transformation of leukoplakia is the oral cavity floor (12).
Figure 1.

Oral lichen erosivus
Figure 2.

Oral leukoplakia
Oral lichen planus is immune-mediated inflammatory mucocutaneous disease which occurs in adults, more frequently in females. It occurs in three basic forms (lichen ruber planus, erosivus, and bulosus), and it is classified by its appearance as either reticular, annular, nodular, atrophic, and sclerosus. Premalignant potential of this disease is from 0.4% to 3.3%, particularly for erosive lichen (13, 14) (Figure 1).
Actinic cheilitis is a potentially malignant lesion caused by exposure to sunlight. It affects males more often than females, and the most common localization is the lower lip. Off-white or red changes may be ulcerated. It is estimated that the rate of malignant alteration ranges from 1.4% to 36% (15).
From the above, we can conclude that there may be potentially malignant lesions in the oral mucosa that can turn malignant, and that early diagnosis of PML is of great importance in cancer prevention and early stage cancer detection. If cancer is detected in the initial stage, the potential for remission is 80%.
2. MATERIALS AND METHODS
The study included 340 patients who came for an initial examination at the Clinic for Oral Medicine and Periodontology during the period of 8 months. Out of these patients, there were 40 patients with potentially malignant lesions, of both sexes and of different ages. After extensive anamnesis and clinical examination, patients with potentially malignant lesions underwent vitroadhesion, sialometry, and innate test for Candida albicans. For better diagnostics of premalignant lesions, the Toluidine blue was used for color staining. All lesions were coated with 1% Toluidine blue, which is retained on tissue with increased mitotic activity (Figure 3). Patients who had a positive Toluidine test were sent to Maxilofacial Surgery Clinic of the CCUS to undergo biopsy and pathohistological analysis.
Figure 3.

Toluidine blue test
After a detailed clinical examination, all PMLs were coated with 1% Toluidine blue.
Toluidine will adhere to tissue with increased mitotic activity, such as cancer tissue. Toluidine test is not a substitute for pathohistological findings, despite indicating malignancy in more than 75% of cases, but the biopsy and pathohistological finding is a gold standard in diagnosing oral cancer.
3. RESULTS
Of the 340 patients who came to the clinic for the first time with a certain problem, there were 40 patients with premalignant or potentially malignant lesions. We treated these 40 patients, 23 of whom were female, while 17 were male. Regarding the bad habit of smoking, 14 patients (35%) were smokers and 26 patients (65%) were non-smokers. 77% of patients do not consume alcohol, while 23% consume alcohol, most commonly all types (beer, wine, and spirits).
The most common oral disease is Lichen reticularis (25%). Lichen erosivus was observed in 20% of patients, leukoplakia in 15%, focal hiperceratosis in 11%, ulcus chronicus in 8%, erosia mucosae in 7%, while actinic cheilitis, morsicatio buccarum, pemphigus, and hemangioma were each represented by 2%.
The most common localization of the change is the buccal mucosa bilaterally (26%). Pathological lesions were located on buccal mucosa unilaterally in 10% of patients, as well as on the lower lip (10%).
The staining test using Toluidine blue was performed for all patients with potentially malignant lesions. The test was positive in 23% of PMLs.
Patients with positive Toluidine blue staining findings underwent biopsy and pathohistological analysis.
Diagram 1-4 shows that 20% of all diagnoses are cancers (CIS, basal cell carcinoma, squamous cell carcinoma), and 14% are dysplasiae.
Diagram 1.
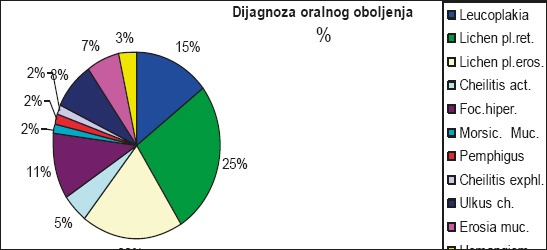
Percentage representation of oral diseases (potentially malignant diseases)
Diagram 2.
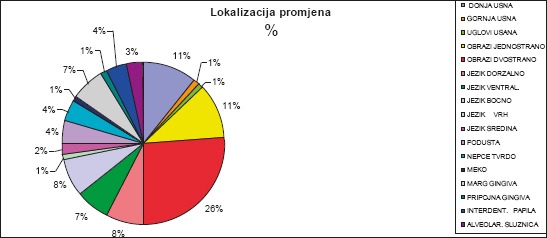
Localization of pathological changes in %
Diagram 3.
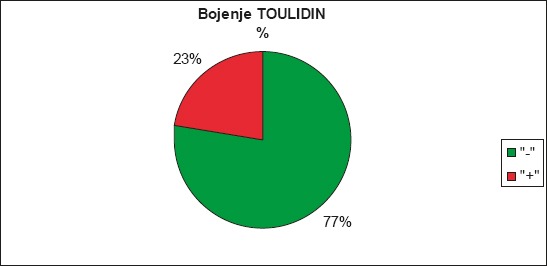
Staining PMLs with Toluidine blue in%
Diagram 4.
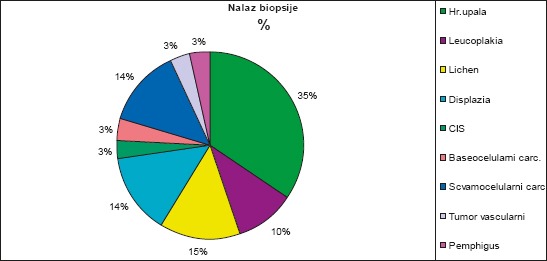
Proportional representation of biopsy diagnosis
Diagram 5.

Most common localization of mucosal changes in cancer patients
The most common localization of malignant changes or carcinomas are the floor of the oral cavity, lower lip, buccal mucosa unilaterally, and ventral side of the tongue, with 17% each.
We investigated the correlation between certain parameters by using Spearman’s correlation. We obtained a significant correlation between Leukoplakia and staining with Toluidine blue. Staining with Toluidine blue is more frequently positive in Leukoplakia patients (Spearman’s coefficient = 0.427, p = 0.006, N = 40). Statistically, there is a significant positive correlation between squamous cell carcinoma and staining with Toluidine blue (Spearman’s coefficient = 0.619, p = 0.000, N = 40).
4. DISCUSSION
Oropharyaringeal carcinomas are usually preceded by potentially malignant lesions, but are generally diagnosed quite late. It is estimated that approximately 50% of patients with oral cavity cancer have local or remote metastases at the time of diagnosis, so it is very important to diagnose potential malignant lesions (16, 17).
According to recent studies and confirmed by our study, the incidence of potentially malignant diseases is on the rise.
The average age of our sample was 69 years and the majority were female, which is in accordance with the findings by Sankari, S.L. et al, whose average sample age was 70 years (18).
The most common location where pathological changes occurred were the oral cavity floor, buccal mucosa and the lower lip, while Bokor-Bratie et al found that lesions are more common in the oral mucosa and alveolar ridge. Many authors suggest that smoking and drinking alcohol are the main etiologic factors of emergence of PML, but we did not find a statistically significant correlation for smoking habit, but we saw a statistically significant correlation between cancer and alcohol consumption. Maia, H.C. et al examined the incidence of potentially malignant lesions in a sample of 340 patients, of whom 106 had potentially malignant lesions (31.2%) and 61 (17.9%) underwent a biopsy. The most common malignant alterations were erythroplakia, leukoplakia, and ulcus chronicus (19), while the most common PML in the Onofre, M.A. study is leukoplakia, followed by lichen and actinic cheilitis. The prevalence of epithelial dysplasia and carcinoma was 17.8%, more often in leukoplakia, which is consistent with our results.
Aghbari, S.M.H. investigated the malignant transformation of lichen and, despite a small percentage of malignant transformation, recommended clinical observation of the lesion and cessation of smoking due to an increased incidence in smokers (20). Habits such as smoking and alcohol are predisposing factors for PML and oral cancers. Our study did not statistically confirm the positive association between smoking and cancer, which is consistent with the results of Muthukrishnan, A. (21, 22). According to Nevill et al., tobacco is a potent carcinogen, as is alcohol. Our study confirmed the statistically significant correlation between alcohol consumption and cancer (Spearman’s coefficient = 0.320, p = 0.044, N = 40). Our biopsy research showed the presence of squamous cell carcinoma in 20% of potentially malignant lesions, which is consistent with a study by Renaud-Vilmer, C. et al which states that squamous cell carcinoma of the oral cavity has a high incidence frequency, and that it is observed at a rate of 10-80% in the existing PMLs (23).
In the Goodson, M.L. research, of 1,248 potentially malignant lesions biopsy confirmed 58 carcinomas, 25 dysplasiae, and 33 non-dysplastic lesions. The authors emphasized the importance of clinical examination and monitoring of potentially malignant lesions (24). Toluidine blue is used to improve PML diagnosis and early cancer detection. Rahman, F. et al stained PMLs with 1% Toluidine blue in 86 patients, followed by cytological analysis. The results showed that the test with 1% Toluidine blue is highly sensitive, specific, and accurate in the detection of premalignant lesions and carcinoma (85%), which is consistent with our results which confirmed the statistically significant positive correlation of squamous cell carcinoma and staining with Toluidine blue (Spearman’s coefficient = 0.619, p = 0.000, N = 40). Other authors such as Sridharan, G. and Chainani-Wu also showed that Toluidine blue is a successful diagnostic tool that can be used in high-risk patients with PML, and is an auxiliary means for early detection of cancer (25,26).
5. CONCLUSION
Most oral cancers are caused by potentially malignant lesions, which is why a detailed clinical examination with visualization of pathological lesions is very important. The Toluidine blue test can be auxiliary in clinical diagnosis but does not replace the pathohistological analysis. Biopsy and pathohistological analysis are the gold standard in the diagnosis of oral cancer, as confirmed in our research. The importance of dental practitioners lies in diagnosing potentially malignant lesions and early detection of oral cancer, and great attention needs to be given to their long-term education in this area.
Footnotes
• Authors’ contributions: Conception and design: SH and MGV; Acquisition, analysis and interpretation of data: SH, MGV and EP; Drafting the article: SH and EP; Revising it critically for important intellectual content: SH and AD.
• Conflict of interest: none declared.
REFERENCES
- 1.Baykul T, Yilmaz HH, Aydin U, Aydin MA, Aksoy MC, Yildirim D. Early diagnosis of oral cancer. The Journal of International Medical Research. 2010;38(3):737–49. doi: 10.1177/147323001003800302. [DOI] [PubMed] [Google Scholar]
- 2.Silverman S. Oralcancer. USA: American Cancer Society; 2003. [Google Scholar]
- 3.Jemal A, Siegal R. Cancer statistics. CA Cancer J Clin. 2008;58(2):71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 4.Vlaho B. Stomatolog i rano otkrivanje oralnog karcinoma. Acta Med Croatica. 2015;69:45–48. [PubMed] [Google Scholar]
- 5.Neville BW, Day TA. Oral cancer and precancerous lesions. CA Cancer J Clin. 2002;52(4):195–215. doi: 10.3322/canjclin.52.4.195. [DOI] [PubMed] [Google Scholar]
- 6.Mortazavi H, Baharvand M, Mehdipour M. Oral potencially malignant disorders: an overview of more then 20 entities. J Dent Res Clin Dent Prospects. 2014;8(33):6–14. doi: 10.5681/joddd.2014.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arifhodžić F. Protokol za dijagnozu i terapiju oralne leukoplakije i eritroplakije. Posebno izdanje ANUBiH CLXV, OMN 47, str. :25–37. [Google Scholar]
- 8.Rogers SN, Vedpathak SV, Lowe D. Reasons for delayed presentation in oral and orophariyngealcancer: the patients perspective. Br J Oral Maxillofac Surg. 2011;49:349–53. doi: 10.1016/j.bjoms.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 9.van der Waal I. Potentially malignant disorders of the oral and oropharyngeal mucosa;terminology, classification and present concepts of management. Oral Oncol. 2009;45:317–323. doi: 10.1016/j.oraloncology.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 10.Thomas G, Hashibe M, Jacob BJ, Ramadas K, Mathew B, Sankaranarayanan R, Zhang ZF. Risk factors for multiple oral premalignant lesions. Int J Cancer. 2003;107:285–291. doi: 10.1002/ijc.11383. [DOI] [PubMed] [Google Scholar]
- 11.Shiu MN, Chen TH, Chang Sh, Hahn LJ. Risk factors for leucoplacia and malignant transformation to oral carcinoma: a leukoplakia cohort in Taiwan. Br J Cancer. 2009;82(11):1871–4. doi: 10.1054/bjoc.2000.1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kilt TJ, Kim HS, Kim HJ, Nam W, Cha IH. Genetic Abnormalities in Oral Leukoplakia and Oral Cancer Progression. Asian Pac J Cancer Prev. 2016;17(6):3001–6. [PubMed] [Google Scholar]
- 13.Roopashree MR, Gondhalekar RV, Shashikanth MC, George J, Thippeswamy SH, Shukla A. Pathogenesis of oral lichen planus- a rewiew. J Oral Pathol Med. 2010;39:729–734. doi: 10.1111/j.1600-0714.2010.00946.x. [DOI] [PubMed] [Google Scholar]
- 14.Payeras P. Oral lichen planus. Otoralyngol Clin North Am. 2011;44:89–107. doi: 10.1016/j.otc.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 15.de Santana Sarmento DJ, da Costa Miguel MC, Querioz LM, Godoy GP, da Silveriera EJ. Actinic cheilitis: clinicopathologic profile and association with degree of dysplasia. Int J Dermatol. 2014;53:466–472. doi: 10.1111/ijd.12332. [DOI] [PubMed] [Google Scholar]
- 16.Neville BW, Day TA. Oral cancer and precancerous lesions. CA Cancer J Clin. 2002 Jul-Aug;52(4):195–215. doi: 10.3322/canjclin.52.4.195. [DOI] [PubMed] [Google Scholar]
- 17.Gurkan Yardimci, Zekayi Kutlubay, Burhan Engin, Yalcin Tuzun. Precancerous lesions of oral mucos. World J Clin Cases. 2014 Dec 16;2(12):866–872. doi: 10.12998/wjcc.v2.i12.866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sankari SL, Gayathri K, Balachander N, Malathi L. Cadida in potentially malignant oral disorders. J Pharm Bioall Sci. 2015;7(Suppl S1):162–4. doi: 10.4103/0975-7406.155886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maia HC, Pinto NA, Pereira Jdos S, de Medeiros AM, da Silveira EJ, Miguel MC. Potentially malignant oral lesions: clinicopathological correlations. Einstein (Sao Paulo) 2016 doi: 10.1590/S1679-45082016AO3578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aghbari SMH, Abushouk AI, Attia A, Elmaraezy A, Menshawy A, Ahmed MS, Elsaadany BA, Ahmed EM. Malignant transformation of oral lichen planus and oral lichenoid lesions: A meta-analysis of 20095 patient data. Oral Oncol. 2017 May;68:92–102. doi: 10.1016/j.oraloncology.2017.03.012. [DOI] [PubMed] [Google Scholar]
- 21.Muthukrishnan A, Bijai Kumar L. Actinic cheilosis: early intervention prevents malignant transformation. BMJ Case Rep. 2017 Mar 20;:2017. doi: 10.1136/bcr-2016-218654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Onofre MA, Sposto MR, Navarro CM, Motta ME, Turatti E, Almeida RT. Potentially malignant epithelial oral lesions: discrepancies between clinical and histological diagnosis. Oral Dis. 1997 Sep;3(3):148–52. doi: 10.1111/j.1601-0825.1997.tb00026.x. [DOI] [PubMed] [Google Scholar]
- 23.Reanaud-Vilmer C, Cavelier-Balloy B. Precancerous lesions of the buccal epitelium. Ann Dermatol Venerol. 2017 Feb;144(2):100–108. doi: 10.1016/j.annder.2016.07.017. [DOI] [PubMed] [Google Scholar]
- 24.Goodson ML, Sloan P, Robinson CM, Cocks K, Thomson PJ. Oral precursor lesions and malignant transformation—who, where, what, and when? Br J Oral Maxillofac Surg. 2015 Nov;53(9):831–5. doi: 10.1016/j.bjoms.2015.08.268. [DOI] [PubMed] [Google Scholar]
- 25.Rahman F, Tippu SR, Khandelwal S, Girish KL, Manjunath BC, Bhargava A. A Study to evaluate the efficacy of toluidine blue and cytology in detecting oral cancer and dysplastic lesions. Quintessence Int. 2012 Jan;43(1):51–9. [PubMed] [Google Scholar]
- 26.Chainani-Wu N, Madden E, Cox D, Sroussi H, Epstein J, Silverman S., Jr Toluidine blue aids in detection of dysplasia and carcinoma in suspicious oral lesions. Oral Dis. 2015 Oct;21(7):879–85. doi: 10.1111/odi.12358. [DOI] [PubMed] [Google Scholar]


