Abstract
Introduction:
Intracranial dermoid cystic tumors account for <1% of all intracranial masses.
Case report:
A 52-year-old male, having headaches, nausea and is presented with a history of 2 episodes of new onset seizures. On presentation, the patient had a normal physical exam, including a complete neurological and cranial nerve exam.
Methods:
Precontrast MRI; TSE/T2Wsequence in axial/coronal planes; 3D – HI-resolution T1W sagittal; FLAIR/T2W axial; FLAIR/T2W, Flash/T2W oblique coronal plane, GRE/T2W axial. Post-contrast TSE/T1W sequence in axial, coronal and sagittal planes. Diffusion weighted and ADC mapping, postcontrast: TSE/T1W sequence in axial, coronal and sagittal planes.
Results:
Subsequent MRI of the brain revealed an oval and lobulated 47x34x30mm (TRxAPxCC) non-enhancing T1-hyperintense mass in right cavernous sinus, with compression of surrounding mesial temporal lobe and right anterolateral aspect of mesencephalon. Findings are consistent with ruptured dermoid cyst, given the evacuated sebum content at its lower half. Sebum particles in millimetric sizes are seen within right Sylvian fissure, anterior horns of lateral ventricles and to a lesser extent within left Sylvian fissure, right parietal sulci, cerebral aqueduct, and basal cisterns. No restricted diffusion is seen, eliminating the possibility of epidermoid. A shunt catheter is evident traversing between right lateral ventricle and right parietal bone; besides, slit-like right lateral ventricle is noted (likely secondary to over-draining shunt catheter).
Conclusion:
Intracranial dermoid cysts are benign rare slow-growing tumors that upon rupture, however, widespread presence of T1 hyperintense droplets and leptomeningeal enhancement can be noted–making MRI the best imaging modality for diagnosis of this rare entity.
Keywords: Intracranial dermoid cyst, ruptured, MRI, UCCK, Pristine, Kosova
1. INTRODUCTION
Intracranial dermoid cystic tumors account for <1% of all intracranial masses. Intracranial dermoid cysts are uncommon lesions with characteristic imaging appearances. They can be thought of as along the spectrum: from epidermoid cysts at one end (containing only desquamated squamous epithelium) and teratomas at the other (containing essentially any kind of tissue from all three embryonic tissue layers).
Dermoids are nonneoplastic, congenital ectodermal inclusion cysts that contain varying amounts of ectoderm derivatives to include apocrine, sweat, and sebaceous cysts as well as hair follicles, squamous epithelium, and possibly teeth. They are not to be confused with an epidermoid cyst, which contains only squamous epithelium. Teratomas, although similar in some respects, are a separate entity. Teratomas are true neoplasms that contain tissue from all three embryonic germ cell layers (1).
Dermoid cystic tumors arise from the inclusion of ectodermally committed cells at the time of neural tube closure during the third to fifth week of embryogenesis. These lesions are slow growing due to the active production of hair and oils from the internal dermal elements (2). The presentation of dermoid tumors is quite variable. Occasionally they are incidental findings discovered on brain computed tomography (CT) or magnetic resonance imaging (MRI) for otherwise unrelated clinical complaints, or they are discovered during imaging investigation of unexplained headaches, seizures, and rarely olfactory delusions (3, 4). When dermoid cystic tumors rupture and spread their contents into the ventricles and subarachnoid and/or subdural spaces, the most common clinical presentation is that of headache and seizures. Headache may be the consequence of compression of adjacent neural structures, chemical meningitis from cyst content irritation, or perhaps the effects of hydrocephalus if present.
Dermoid cystic tumor rupture usually occurs spontaneously; however, cases of rupture secondary to closed head trauma or iatrogenic surgical complications have been reported. Supratentorial dermoids often present in the second or third decades of life, while posterior fossa dermoids typically present in the first decade of life as a consequence of mass effect exerted on the fourth ventricle with resulting hydrocephalus (5). Posterior fossa cystic tumors may have visible occipital scalp dimples or sinus tracts. If present, these are usually discovered in infancy. A fistulous sinus tract may lead to recurrent bouts of bacterial meningitis.
On MRI scans, dermoids will be hyperintense (bright) on T1-weighted imaging and heterogenous on T2-weighted imaging. If the internal fat content is relatively low, the lesion will reveal cerebrospinal fluid–like signal intensity. In such cases, fluid attenuation inversion recovery (FLAIR) is useful, in that the fat will appear hyperintense (bright) on a background of suppressed fluid signal (dark). On MRI, fat constituents create a so-called “chemical shift” artifact due to misregistration of the signal in the frequency-encoded direction. This can be particularly useful in diagnosing these lesions preoperatively. When a dermoid tumor ruptures, fat droplets - appearing hypodense on CT or T1 hyperintense on MRI - may be seen scattered and floating within the nondependent portions of the ventricular system and/or subarachnoid space. This is considered a classic imaging feature of these lesions. In the setting of complicating chemical meningitis, intense pial and ventricular ependymal enhancement may be detected after the administration of MRI gadolinium contrast (6-8).
2. CASE REPORT
A 52-year-old male, eight years ago, in 2008, complaints of severe headaches, vomiting thus visits the neurosurgeon, who recommends him for CT examination. After the examination, it is verified a dermatoid cyst, that causes compression in the ventricular system with development of the shunt. The patient does not refer of any problems till December 2016, where he refers of having headaches, nausea and is presented with a history of 2 episodes of new onset seizures. On presentation, the patient had a normal physical exam, including a complete neurological and cranial nerve exam.
We did MRI with protocol: precontrast MRI; TSE/T2W sequence in axial/coronal planes; 3D – Hi-resolution T1W sagittal; FLAIR/T2W axial; FLAIR/T2W and Flash/T2W oblique coronal plane, GRE/T2W axial plane for detection of heme products. Post-contrast TSE/T1W sequence in axial, coronal and sagittal planes. Diffusion weighted and ADC mapping MRI images for EPI sequence in axial plane.
3. RESULTS
Subsequent MRI Figures 1 (a, b, c, d, e, f, g, h) of the brain revealed an oval and lobulated 47x34x30mm (TRxAPxCC) non-enhancing T1-hyperintense mass in right cavernous sinus, with compression of surrounding mesial temporal lobe and right anterolateral aspect of mesencephalon. Findings are consistent with ruptured dermoid cyst, given the evacuated sebum content at its lower half. Sebum particles in millimetric sizes are seen within right Sylvian fissure, anterior horns of lateral ventricles and to a lesser extent within left Sylvian fissure, right parietal sulci, cerebral aqueduct, and basal cisterns. No restricted diffusion is seen, eliminating the possibility of epidermoid. A shunt catheter is evident traversing between right lateral ventricle and right parietal bone; besides, slit-like right lateral ventricle is noted (likely secondary to over-draining shunt catheter).
Figure 1.
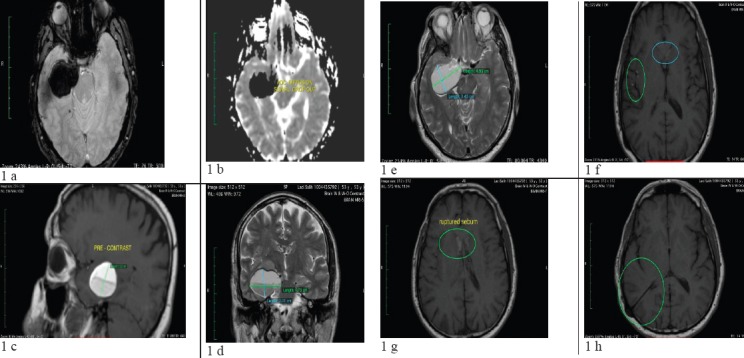
(a- h): Subsequent MRI of the brain revealed an oval and lobulated 47x34x30mm (TRxAPxCC) non-enhancing T1-hyperintense mass in right cavernous sinus, with compression of surrounding mesial temporal lobe and right anterolateral aspect of mesencephalon. Findings are consistent with ruptured dermoid cyst, given the evacuated sebum content at its lower half. Sebum particles in millimetric sizes are seen within right Sylvian fissure, anterior horns of lateral ventricles and to a lesser extent within left Sylvian fissure, right parietal sulci, cerebral aqueduct, and basal cisterns. No restricted diffusion is seen, eliminating the possibility of epidermoid. A shunt catheter is evident traversing between right lateral ventricle and right parietal bone; besides, slit-like right lateral ventricle is noted (likely secondary to over-draining shunt catheter)
4. DISCUSSION
Intracranial dermoid cysts are rare, comprising 0.04–0.7% of intracranial tumors. They are derived from ectopic epithelial cells that are part of the neural tube, which also explains their typical location close to the midline. Although they are benign, slow-growing tumors, they may cause focal neurologic signs through encroachment of neurovascular structures and, rarely, rupture (9). Dermoid cysts contain lipid material, and previous reports have discussed that they may have fatty tissue peripherally and fluid centrally. They can contain hair follicles, sebaceous and sweat glands, and the presence of these structures helps distinguish a dermoid from the more common epidermoid cysts (10). They are not true neoplasms, as they enlarge through accumulation of desquamation products and sebaceous secretions inside a cystic cavity rather than via cell division.
Rupture of intracranial dermoid cysts is a rare phenomenon (5 out of 2707, or 0.18% of all new CNS tumors operated on during a 12-year period at a major tertiary care center) and typically spontaneous, although can occur secondary to closed head trauma (11). The pathophysiology behind spontaneous rupture is not clearly understood, and hypotheses have implicated glandular secretions caused by age-dependent hormones as well as head movements and brain pulsations (12). The dissemination of intracystic keratin and cholesterol breakdown products following rupture can cause a wide variety of symptoms ranging from headache to hallucinations (13). Clinical presentation can vary depending on the cyst location, and in one analysis of available case reports by El-Bayh et al. (14) headache was the most common symptom (32.6%), followed by seizures (26.5%), cerebral ischemia with sensory and/or motor hemi syndrome (16.3%), and aseptic meningitis (8.2%) (15). The case presented involved a spontaneously ruptured intracranial dermoid cyst causing new onset seizures due to presumed chemical meningitis and chemical irritation secondary to dissemination of fat droplets (16-19).
On CT scans, dermoid cysts can have mixed densities, and rarely enhance following contrast administration (20-23). The intracystic fat and disseminated fat droplets appears hypodense, whereas calcifications in the wall are hyperdense. Hydrocephalus and fat-fluid level may be present following rupture into the ventricular system. On MRI, dermoid cysts are hyperintense on T1-weighted sequences and variable on T2-weighted sequences, although the presence of cholesterol can often make them appear hypointense on T2 as well (23-26). Dermoid cysts can be differentiated from epidermoid cysts in that the former demonstrates fat signal on CT and MRI whereas the latter resembles CSF (27-29). Although Fluid Attenuated Inversion Recovery (FLAIR) sequences and Diffusion Weighted Imaging (DWI) have been used to distinguish the two entities, dermoid cysts can resemble epidermoids due to their bright signal on DWI (30, 31).
MRI is more sensitive than CT in the detection of dermoid cysts and due to the higher contrast resolution, the ease of multiplanar imaging and the lack of bone artifacts (32). Orakcoiglu et. al. (33) in particular emphasizes the importance of using an MRI protocol involving T2-WI, T1-WI, T1 fat saturated-WI, Magnetic Resonance Angiography (MRA) and DWI. Conventional MRI is not very helpful in distinguishing dermoids from other cystic masses such as arachnoid cysts. On DWI, however, the dermoids are hyperintense to brain parenchyma, but demonstrate an ADC that is similar to that of parenchyma and CSF. This is in contrast to arachnoid cysts, which show the opposite pattern (low DWI, but elevated ADC) (34, 35). Differentiating a dermoid cyst from craniopharyngiomas is relatively easier, as the latter enhances strongly on CT (36, 37). In addition, the craniopharyngioma cyst walls also display strong enhancement on T1-weighted MRI sequences (38, 39). Teratomas help distinguish themselves via their calcifications, which are hyperintense on CT (40, 41) and show up as shadowing echogenic foci on ultrasound (42-44).
Dermoid cysts are benign entities, and have a generally favorable prognosis. Surgery is only indicated in cases where dermoid cysts cause mass effect and serious neurological deficits. In cases where the cyst is intact, the goal is complete surgical removal of the primary tumor capsule and intracystic contents and dissection from adjacent neurovascular structures.
5. CONCLUSION
Intracranial dermoid cysts are benign rare slow-growing tumors that, when intact, are of mixed or predominantly low density on CT and hyperintense on MRI T1 with little to no contrast enhancement. The cysts are hyperintense on DWI and isointense to brain parenchyma on ADC, which helps distinguish them from other cystic masses. Upon rupture, however, widespread presence of T1 hyperintense droplets and leptomeningeal enhancement can be noted–making MRI the best imaging modality for diagnosis of this rare entity.
The capability of MR to evaluate the associated vessel displacement, either by flow void or MR angiography, paired with better visualization of the lesions relative to the base of the skull owing to lack of bone interference and multiplanar imaging capability, make MR the preferred preoperative imaging method.
Footnotes
• Conflict of interest: none declared
REFERENCES
- 1.Rubin G, Scienza R, Pasqualin A, Rosta L, Da Pian R. Craniocerebral epidermoids and dermoids. A review of 44 cases. Acta Neurochir (Wien) 1989;97(1–2):1–16. doi: 10.1007/BF01577734. [DOI] [PubMed] [Google Scholar]
- 2.Osborn AG, Preece MT. Intracranial cysts: radiologic-pathologic correlation and imaging approach. Radiology. 2006;239(3):650–64. doi: 10.1148/radiol.2393050823. [DOI] [PubMed] [Google Scholar]
- 3.Kim KS, Weinberg PE. Dermoid tumor. Surg Neurol. 1981;15(5):375–6. doi: 10.1016/0090-3019(81)90175-0. [DOI] [PubMed] [Google Scholar]
- 4.Graham DV, Tampieri D, Villemure JG. Intramedullary dermoid tumor diagnosed with the assistance of magnetic resonance imaging. Neurosurgery. 1988;23(6):7657. doi: 10.1227/00006123-198812000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Cha JG, Paik SH, Park JS, Park SJ, Kim DH, Lee HK. Ruptured spinal dermoid cyst with disseminated intracranial fat droplets. Br J Radiol. 2006;79(938):167–9. doi: 10.1259/bjr/17232685. [DOI] [PubMed] [Google Scholar]
- 6.Smirniotopoulos JG, Chiechi MV. Teratomas, dermoids, and epidermoids of the head and neck. Radiographics. 1995;15(6):1437–55. doi: 10.1148/radiographics.15.6.8577967. [DOI] [PubMed] [Google Scholar]
- 7.Osborn AG, Preece MT. Intracranial cysts: radiologic-pathologic correlation and imaging approach. Radiology. 2006;239(3):650–64. doi: 10.1148/radiol.2393050823. [DOI] [PubMed] [Google Scholar]
- 8.Venkatesh SK, Phadke RV, Trivedi P, Bannerji D. Asymptomatic spontaneous rupture of suprasellar dermoid cyst: a case report. Neurol India. 2002;50(4):480–83. [PubMed] [Google Scholar]
- 9.Stendel R, Pietila TA, Lehmann K, Kurth R, Suess O, Brock M. Ruptured intracranial dermoid cysts. Surg Neurol. 2002;57(6):391–8. doi: 10.1016/s0090-3019(02)00723-1. [DOI] [PubMed] [Google Scholar]
- 10.Yasargil MG, Abernathey CD, Sarioglu AC. Microneurosurgical treatment of intracranial dermoid and epidermoid tumors. Neurosurgery. 1989;24(4):561–7. doi: 10.1227/00006123-198904000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Liu JK, Gottfried ON, Salzman KL, Schmidt RH, Couldwell WT. Ruptured intracranial dermoid cysts: clinical, radiographic, and surgical features. Neurosurgery. 2008;62(2):377–84. doi: 10.1227/01.neu.0000316004.88517.29. [DOI] [PubMed] [Google Scholar]
- 12.Phillips WE, Martinez CR, Cahill DW. Ruptured intracranial dermoid tumor secondary to closed head trauma. Computed tomography and magnetic resonance imaging. J Neuroimaging. 1994;4(3):169–170. doi: 10.1111/jon199443169. [DOI] [PubMed] [Google Scholar]
- 13.Lunardi P, Missori P. Supratentorial dermoid cysts. J Neurosurg. 1991;75(2):262–6. doi: 10.3171/jns.1991.75.2.0262. [DOI] [PubMed] [Google Scholar]
- 14.Karabulut N, Oguzkurt L. Tetraventricular hydrocephalus due to ruptured intracranial dermoid cyst. Eur Radiol. 2000;10(11):1810–1. doi: 10.1007/s003300000440. [DOI] [PubMed] [Google Scholar]
- 15.Cohen JE, Abdallah JA, Garrote M. Massive rupture of suprasellar dermoid cyst into ventricles. Case illustration. J Neurosurg. 1997;87(6):963. doi: 10.3171/jns.1997.87.6.0963. [DOI] [PubMed] [Google Scholar]
- 16.Yoshimoto K, Nishio S, Suzuki S, Fukui M, Hasuo K. Movable oil in the brain: intracranial ruptured dermoid tumors. Case illustration. J Neurosurg. 1997;86(4):734. doi: 10.3171/jns.1997.86.4.0734. [DOI] [PubMed] [Google Scholar]
- 17.Ernemann U, Rieger J, Tatagiba M, Weller M. An MRI view of a ruptured dermoid cyst. Neurology. 2006;66(2):270. doi: 10.1212/01.wnl.0000195282.47210.42. [DOI] [PubMed] [Google Scholar]
- 18.Detweiler MB, David E, Arif S. Ruptured intracranial dermoid cyst presenting with neuropsychiatric symptoms: a case report. South Med J. 2009;102(1):98–100. doi: 10.1097/SMJ.0b013e318188b290. [DOI] [PubMed] [Google Scholar]
- 19.El-Bahy K, Kotb A, Galal A, El-Hakim A. Ruptured intracranial dermoid cysts. Acta Neurochir (Wien) 2006;148(4):457–62. doi: 10.1007/s00701-005-0722-0. [DOI] [PubMed] [Google Scholar]
- 20.Stephenson TF, Spitzer RM. MR and CT appearance of ruptured intracranial dermoid tumors. Comput Radiol. 1987;11(5-6):249–51. doi: 10.1016/0730-4862(87)90007-2. [DOI] [PubMed] [Google Scholar]
- 21.Hamer J. Diagnosis by computerized tomography of intradural dermoid with spontaneous rupture of the cyst. Acta Neurochir (Wien) 1980;51(3-4):219–26. doi: 10.1007/BF01406748. [DOI] [PubMed] [Google Scholar]
- 22.Jamjoom AB, Cummins BH. The diagnosis of ruptured intracranial dermoid cysts. Br J Neurosurg. 1989;3(5):609–12. doi: 10.3109/02688698909002854. [DOI] [PubMed] [Google Scholar]
- 23.Davidson HD, Ouchi T, Steiner RE. NMR imaging of congenital intracranial germinal layer neoplasms. Neuroradiology. 1985;27(4):301–3. doi: 10.1007/BF00339561. [DOI] [PubMed] [Google Scholar]
- 24.Osborn AG, Preece MT. Intracranial cysts: radiologic- pathologic correlation and imaging approach. Radiology. 2006;239(3):650–64. doi: 10.1148/radiol.2393050823. [DOI] [PubMed] [Google Scholar]
- 25.Chen S, Ikawa F, Kurisu K, Arita K, Takaba J, Kanou Y. Quantitative MR evaluation of intracranial epidermoid tumors by fast fluid-attenuated inversion recovery imaging and echo-planar diffusion-weighted imaging. AJNR Am J Neuroradiol. 2001;22(6):1089–96. [PMC free article] [PubMed] [Google Scholar]
- 26.Dutt SN, Mirza S, Chavda SV, Irving RM. Radiologic differentiation of intracranial epidermoids from arachnoid cysts. Otol Neurotol. 2002;23(1):84–92. doi: 10.1097/00129492-200201000-00019. [DOI] [PubMed] [Google Scholar]
- 27.Smith AS, Benson JE, Blaser SI, Mizushima A, Tarr RW, Bellon EM. Diagnosis of ruptured intracranial dermoid cyst: value MR over CT. AJNR Am J Neuroradiol. 1991;12(1):175–180. [PMC free article] [PubMed] [Google Scholar]
- 28.Orakcioglu B, Halatsch ME, Fortunati M, Unterberg A, Yonekawa Y. Intracranial dermoid cysts: variations of radiological and clinical features. Acta Neurochir (Wien) 2008;150(12):1227–34. doi: 10.1007/s00701-008-0152-x. [DOI] [PubMed] [Google Scholar]
- 29.Schaefer PW, Grant PE, Gonzalez RG. Diffusion-weighted MR imaging of the brain. Radiology. 2000 Nov;217(2):331–45. doi: 10.1148/radiology.217.2.r00nv24331. [DOI] [PubMed] [Google Scholar]
- 30.Tsuruda JS, Chew WM, Moseley ME, Norman D. Diffusion-weighted MR imaging of the brain: value of differentiating between extraaxial cysts and epidermoid tumors. AJNR. American journal of neuroradiology. 11(5):925–31. [PMC free article] [PubMed] [Google Scholar]
- 31.Behari S, Banerji D, Mishra A, Sharma S, Chhabra DK, Jain VK. Intrinsic third ventricular craniopharyngiomas: report on six cases and a review of the literature. Surg Neurol. 2003;60(3):243–5. doi: 10.1016/s0090-3019(03)00132-0. [DOI] [PubMed] [Google Scholar]
- 32.Barajas MA, Ramirez-Guzman G, Rodriguez-Vazquez C, Toledo-Buenrostro V, Velasquez-Santana H, del Robles RV, et al. Multimodal management of craniopharyngiomas: neuroendoscopy, microsurgery, and radiosurgery. Journal of neurosurgery. 2002 Dec;97(5 Suppl):607–9. doi: 10.3171/jns.2002.97.supplement. [DOI] [PubMed] [Google Scholar]
- 33.Fujimoto Y, Matsushita H, Velasco O, Rosemberg S, Plese JP, Marino R. Jr Craniopharyngioma involving the infrasellar region: a case report and review of the literature. Pediatr Neurosurg. 2002;37(4):210–16. doi: 10.1159/000065396. [DOI] [PubMed] [Google Scholar]
- 34.Van Effenterre R, Boch AL. Craniopharyngioma in adults and children: a study of 122 surgical cases. J Neurosurg. 2002;97(1):3–11. doi: 10.3171/jns.2002.97.1.0003. [DOI] [PubMed] [Google Scholar]
- 35.Smirniotopoulos JG, Yue NC, Rushing EJ. Cerebellopontine angle masses: radiologic-pathologic correlation. Radiographics. 1993;13(5):1131–47. doi: 10.1148/radiographics.13.5.8210595. [DOI] [PubMed] [Google Scholar]
- 36.Liang L, Korogi Y, Sugahara T, Ikushima I, Shigematsu Y, Okuda T, et al. MRI of intracranial germ-cell tumours. Neuroradiology. 2002;44(5):382–8. doi: 10.1007/s00234-001-0752-0. [DOI] [PubMed] [Google Scholar]
- 37.Sandow BA, Dory CE, Aguiar MA, Abuhamad AZ. Best cases from the AFIP: congenital intracranial teratoma. 4. Vol. 24. Radiographics: a review publication of the Radiological Society of North America, Inc; pp. 1165–70. [DOI] [PubMed] [Google Scholar]
- 38.Larsson EM, Brandt L, Holtas S. Persisting intraventricular fat-fluid levels following surgery on a ruptured dermoid cyst of the posterior fossa. Acta Radiol. 1987;28(4):489–90. [PubMed] [Google Scholar]
- 39.Carvalho GA, Cervio A, Matthies C, Samii M. Subarachnoid fat dissemination after resection of a cerebellopontine angle dysontogenic cyst: case report and review of the literature. Neurosurgery. 2000;47(3):760–64. doi: 10.1097/00006123-200009000-00047. [DOI] [PubMed] [Google Scholar]
- 40.Kaido T, Okazaki a, Kurokawa S, Tsukamoto M. Pathogenesis of intraparenchymal epidermoid cyst in the brain: a case report and review of the literature. Surg Neurol. 2003;59(3):211–6. doi: 10.1016/s0090-3019(02)01042-x. [DOI] [PubMed] [Google Scholar]
- 41.Iaconetta G, Carvalho GA, Vorkapic P, Samii M. Intracerebral epidermoid tumor: a case report and review of the literature. Surg Neurol. 2001;55(4):218–22. doi: 10.1016/s0090-3019(01)00346-9. [DOI] [PubMed] [Google Scholar]
- 42.Caruso G, Germano A, Caffo M, Belvedere M, La Torre D, Tomasello F. Supratentorial dorsal cistern epidermoid cyst in childhood. Pediatr Neurosurg. 1998;29(4):203–7. doi: 10.1159/000028722. [DOI] [PubMed] [Google Scholar]
- 43.Kallmes DF, Provenzale JM, Cloft HJ, McClendon RE. Typical and atypical MR imaging features of intracranial epidermoid tumors. AJR Am J Roentgenol. 1997;169(3):883–7. doi: 10.2214/ajr.169.3.9275916. [DOI] [PubMed] [Google Scholar]
- 44.Jaing TH, Wang HS, Hung IJ, Tseng CK, Yang CP, Hung PC, et al. Intracranial germ cell tumors: a retrospective study of 44 children. Pediatr Neurol. 2002;26(5):369–73. doi: 10.1016/s0887-8994(01)00419-2. [DOI] [PubMed] [Google Scholar]


