Abstract
Background and aims
There is inconsistent evidence that alcohol-specific coping is a mechanism of change in cognitive-behavioral therapy (CBT) for alcohol use disorder (AUD). Our primary aim was to test whether baseline dependence severity moderates the mediational effect of CBT on drinking outcomes via coping.
Design
Secondary data analysis of Project MATCH (1), a multi-site alcohol treatment trial in which participants, recruited in outpatient and aftercare arms, were randomized to three treatments: CBT, motivational enhancement therapy (MET) and twelve-step facilitation (TSF).
Setting
Nine research sites in the United States.
Participants
1063 adults with AUD.
Measurements
The primary outcomes were percent days abstinent and percent heavy drinking days at the one-year follow-up. Coping was assessed with the Processes of Change Questionnaire (2). Dependence severity was measured with the Alcohol Dependence Scale (3).
Findings
Among the full available sample (across treatment arms), there were no significant moderated mediation effects. Double moderated mediation analyses indicated that several moderated mediation effects were moderated by treatment arm (all p < .05). In the outpatient arm, there were several significant moderated mediation effects (all p < .05), but no significant moderated mediation effects in the aftercare arm. For outpatient clients with high baseline dependence severity, end-of-treatment coping mediated the positive treatment effects of CBT, as compared with both MET and TSF, on one-year drinking outcomes (all p < .05). Coping did not mediate treatment effects of CBT among those with low or moderate dependence severity.
Conclusions
In the Project MATCH outpatient sample, whether or not coping mediated the effects of cognitive-behavioral therapy (CBT) for alcohol use disorder was conditional on dependence severity. End-of-treatment coping mediated the positive treatment effects of CBT on one-year drinking outcomes among outpatient clients when dependence severity was high, but not when dependence severity was low or moderate.
Keywords: Coping, Alcohol Use Disorder, Alcohol Treatment, Cognitive-Behavioral Therapy, Moderated Mediation, Mechanisms of Behavior Change
Introduction
There are several evidence-based psychosocial treatments for alcohol use disorder (AUD), including cognitive-behavioral therapy (CBT; 3), motivational enhancement therapy (MET;4), and twelve-step facilitation (TSF; 5). However, research has not demonstrated that one psychosocial treatment for AUD is superior to others, and existing AUD treatments are still only modestly effective (1,7). Researchers have emphasized the need to shift focus to understanding mechanisms of behavior change (MOBC) within treatments in order to enhance the overall effectiveness of psychosocial treatment for AUD (8). Developing a greater understanding of MOBC in alcohol treatment is ultimately aimed at optimizing treatment outcomes through the refinement and personalization of treatment delivery.
Preliminary research on MOBC in psychosocial treatments for AUD has yielded promising findings, but overall the findings are mixed (8). For example, even though CBT for AUD is theorized to work by enhancing alcohol-specific coping skills, there is inconsistent evidence regarding this MOBC (9–12). One possibility is that these inconsistent findings are the result of mediational analyses that have been insufficiently precise. To our knowledge, no studies have used moderated mediation to study coping as a MOBC for AUD. Moderated mediation can be used to test whether the mediating role of coping depends on other factors (13). That is, whether coping skills mediate outcomes following CBT treatments may be contingent on client or contextual factors (14).
The importance of utilizing coping skills to change one’s alcohol use may depend on degree of alcohol dependence severity. Alcohol dependence is characterized by several interrelated symptoms, such as salience of alcohol-related stimuli, drinking to relieve negative affective states and withdrawal symptoms, strong desire or craving to drink, and frequent return to drinking following periods of abstinence (15,16). It is plausible that higher dependence severity may warrant greater need to utilize alcohol-specific coping skills in order to change one’s alcohol use and to prevent relapse. Alcohol-specific coping skills are directly aimed at challenges related to AUD and include skills such as avoiding alcohol-related cues, reappraising the consequences of drinking, seeking social support in high-risk situations, and engaging in alternative behavioral activities (17). Individuals with higher dependence severity may be more likely to use these alcohol-specific coping skills during and after treatment, because using them may become particularly important in enabling these individuals to adequately manage elevated symptoms of alcohol dependence. Furthermore, it is possible that CBT clinicians modify the degree to which they focus on and reinforce client use of coping skills depending on the degree of the client’s dependence severity. CBT is unique in its systematic and central focus on teaching coping skills. Thus, for individuals with higher dependence severity, the focus on coping skills in CBT may be particularly helpful in enabling these individuals to acquire and implement an adequate repertoire of coping skills. Relative to MET, TSF provides a greater emphasis on coping skills and past research has shown TSF may mobilize coping skills to a similar degree as CBT (18). Accordingly, TSF may also be particularly helpful in enhancing coping among those with higher dependence severity.
For the current study, we conducted secondary analyses of Project MATCH (1), an AUD treatment trial that compared the efficacy of CBT, MET, and TSF among adults seeking outpatient AUD treatment (outpatient treatment arm) and adults who completed inpatient or intensive outpatient treatment and were referred to AUD outpatient-based aftercare treatment (aftercare treatment arm). Prior analyses of the Project MATCH data (19) found no significant differences among the three MATCH treatments in end-of-treatment treatment coping, as measured by the Processes of Change Questionnaire (PCQ; 2). Hence, the aims of the current study were: 1) in the full available sample (across treatment arms), to test whether the indirect (i.e., mediational) effects of treatment on drinking outcomes via coping (i.e., treatment condition → end-of-treatment coping → drinking outcome) was moderated by baseline dependence severity, and 2) to test whether treatment arm moderates the moderated mediation effects (i.e., a double moderated mediation effect) in aim 1 to determine if the moderated mediation models should be tested in each treatment arm separately. Overall, our main hypothesis was that coping would mediate the treatment effects of CBT among individuals when dependence severity was high.
Method
Design
We conducted secondary analyses of data from Project MATCH (1), a multisite study evaluating three psychosocial treatments for AUD: cognitive-behavioral therapy (CBT; 3), motivational enhancement therapy (MET; 4), and twelve-step facilitation (TSF; 5). The study was conducted across nine research sites in the United States. Participants randomized to CBT and TSF received 12 treatment sessions and participants randomized to MET received 4 treatment sessions. In all conditions, the treatment was delivered over 12 weeks. In Project MATCH, there were two treatment arms: an aftercare arm, which included participants who had completed inpatient or intensive outpatient treatment and were referred to aftercare, and an outpatient arm, which included participants who were actively drinking prior to starting the study. For further details on the design of Project MATCH, see Project MATCH Research Group (20).
Prior secondary analyses of the Project MATCH data have been conducted with the full sample data (across treatment arms) and in each arm separately. In line with prior studies, we first tested moderated mediation models in the full available sample (across treatment arms). However, we suspected that there may be differences in the moderated mediation effects by treatment arm because clients in the aftercare arm had already completed inpatient or intensive outpatient treatment, which likely involved some coping skills training, whereas clients in the outpatient arm may not have been exposed to coping skills training prior to study entry. Hence, we also tested whether the moderated mediation effects were moderated by study arm in order to determine whether additional models should be conducted in each arm separately.
Participants
The full MATCH sample included 1726 participants. For the current study, we included participants who had available data on coping at both the end-of-treatment and an assessment that occurred during the first treatment session. A total of 1587 participants (92% of the full sample) had available data on coping at end-of-treatment. A total of 1154 participants (66.8% of the full sample) had available data on coping at the first treatment session. The available sample with data on coping at both the first treatment session and end-of-treatment was 1063 participants (61.6% of full sample). Table 1 presents the demographics of the full available sample, as well as the demographics by treatment group within each treatment arm.
Table 1.
Descriptive Statistics for Study Variables, N (%) or Mean (Standard Deviation)
| Aftercare Sample (n =567) | Outpatient Sample (n =496) | Full Available Sample (n =1063) | |||||
|---|---|---|---|---|---|---|---|
| MET (n= 195) | TSF (n=176) | CBT (n=196) | MET (n =158) | TSF (n=173) | CBT (n=165) | ||
| One-Year PDD | 22.38 (34.42) | 19.08 (32.80) | 18.82 (31.50) | 27.15 (35.45) | 27.63 (36.20) | 28.83 (34.96) | 23.70 (34.31) |
| One-Year PHD | 16.55 (30.36) | 15.46 (30.72) | 13.01 (26.34) | 18.19 (26.69) | 20.37 (31.82) | 18.96 (29.98) | 16.93 (34.31) |
| End-of-Treatment Coping | 127.15 (25.93) | 126.63 (25.54) | 129.61 (24.14) | 118.46 (21.63) | 118.59 (27.18) | 120.09 (25.22) | 123.65 (25.39) |
| First Treatment Session Coping | 27.15 (6.68) | 27.04 (7.05) | 28.29 (7.15) | 23.00 (6.68) | 22.57 (6.03) | 22.72 (5.91) | 25.29 (7.03) |
| Baseline Alcohol Dependence Severity | 18.02 (7.71) | 19.36 (8.29) | 18.79 (8.41) | 14.54 (6.99) | 14.74 (7.91) | 14.91 (7.39) | 16.83 (8.06) |
| Baseline PDD | 79.63 (25.14) | 77.69 (25.37) | 76.63 (27.70) | 69.45 (26.48) | 70.00 (29.94) | 72.88 (25.65) | 74.62 (26.97) |
| Baseline PHD | 76.76 (26.29) | 74.04 (28.18) | 71.28 (30.73) | 62.88 (27.36) | 62.44 (30.94) | 65.42 (28.66) | 69.14 (29.22) |
| Female | 32 (16.4%) | 29 (16.5%) | 45 (23%) | 33 (20.9%) | 47 (27.2) | 43 (26.1%) | 229 (21.5%) |
| Age | 42.33 (11.36) | 41.98 (10.58) | 42.93 (12.07) | 40.42 (10.99) | 41.37 (11.17) | 40.75 (10.54) | 41.70 (11.17) |
| Married | 64 (32.8%) | 50 (28.4%) | 63 (32.%) | 60 (38%) | 73 (42.2%) | 64 (38.8%) | 374 (35.2%) |
| Non-White | 37 (19.0%) | 35 (19.9%) | 40 (20.4%) | 21 (13.3%) | 21 (12.1%) | 32 (19.4%) | 186 (17.5%) |
| Baseline Readiness to Change | 11.14 (1.49) | 11.17 (1.67) | 11.18 (1.38) | 10.59 (1.55) | 10.36 (1.59) | 10.67 (1.63) | 10.87 (1.58) |
| Baseline Self-Efficacy | 3.23 (1.02) | 3.13 (1.05) | 3.27 (0.97) | 3.00 (0.82) | 2.95 (0.86) | 2.90 (0.81) | 3.09 (0.94) |
Note. PDD = Percent Drinking Days; PHD = Percent Heavy Drinking Days; MET = Motivational enhancement therapy; TSF =Twelve-step facilitation therapy; CBT = Cognitive-behavioral therapy. End-of-treatment coping was measured with the 40-item Processes of Change Questionnaire, whereas first treatment session coping was measured with a subset of 8 items from this questionnaire. Baseline readiness to change scores ranged from −2 to 14.
Measures
Coping Skills
The Processes of Change Questionnaire (PCQ; 2) was used to assess coping at end-of-treatment. The PCQ is a 40-item self-report measure that assesses the frequency in which one uses 10 types of coping skills specific to changing one’s drinking: rewarding oneself, alternative activities, cognitive commitment to change, seeking social support, stimulus control, reading/thinking about information on drinking problems, drawing upon emotions in the change process, thinking about how drinking is hurting others, thinking about personal benefits of changing one’s drinking, and thinking about other individuals making similar changes. The Likert-type scale for each item ranges from 1 = Never to 5 = Repeatedly. Total scores from the PCQ at end-of-treatment were used in analyses. Total scores for the PCQ were examined in prior analyses of the PCQ data in Project MATCH (19). The internal reliability of the PCQ was excellent (Cronbach’s alpha = 0.95). In Project MATCH, the 40-item PCQ was not administered at baseline. Rather, an 8-item abbreviated version of the PCQ was included in the treatment session data collection. We used data from the 8-item PCQ at the first treatment session. The items from the 8-item abbreviated PCQ included: “Avoided situations that encourage drinking,” “Did something else to deal with tension/urges,” “Rewarded self for not drinking,” “Looked for information related to problem drinking,” “Had someone to listen when I wanted to talk about drinking,” “Made commitments to self not to drink,” “Got upset when I thought about drinking problem,” and “Avoided people/places that encourage drinking.” The internal reliability of the 8-item PCQ was adequate (Cronbach’s alpha = 0.79).
Alcohol Use
The Form-90 (21) was used to assess alcohol use at baseline and one-year post-treatment. The summary alcohol use variables were: percent drinking days (PDD) and percent heavy drinking days (PHD; with heavy defined as 5+/4+ standard drinks for men/women) during the 30 days prior to the baseline and one-year post-treatment assessment.
Moderator Variable
The Alcohol Dependence Scale (ADS; 21) was used to measure alcohol dependence severity. The ADS is a 25-item self-report measure of alcohol dependence severity that was originally created based on analyses of the Alcohol Use Inventory (3). A recent study showed that the ADS had good psychometric properties across three separate AUD samples (15). In the current study sample, the internal reliability of the ADS at baseline was adequate (Cronbach’s alpha = 0.86).
Covariates
A basic demographic questionnaire was used to measure gender, age, marital status, and race/ethnicity at baseline. The University of Rhode Island Change Assessment (URICA), a 24-item self-report measure using Likert-type responses (1 = Strongly Disagree, 5 = Strongly Agree), was used to assess baseline readiness to change (22). Total readiness scores were derived by summing the means of the contemplation, action, and maintenance subscales and then subtracting the mean of the precontemplation subscale(19). The internal reliability for the total readiness scores was adequate (Cronbach’s alpha = 0.79). The Alcohol Abstinence Self-Efficacy Scale (AASE; 24), a 20-item self-report measure with Likert-Type responses (1 = not at all confident, 5 = extremely confident) was used to assess baseline self-efficacy or confidence in abstaining from drinking in various situations. The internal reliability of the AASE was excellent (Cronbach’s alpha = 0.95).
Statistical Analyses
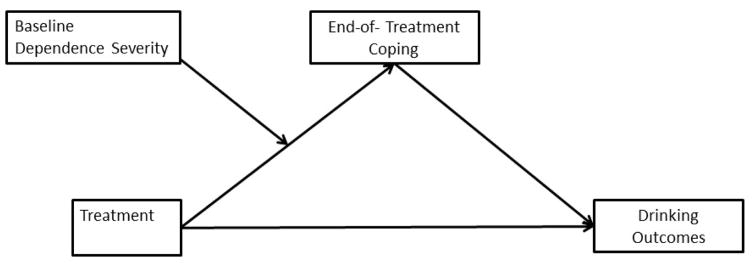
SPSS Version 22 was used to conduct descriptive analyses and missing data analyses, and Mplus Version 7.3 (24) was used to conduct all other analyses. For the mediation and moderated mediation models we used the product of coefficients approach (25). To test the statistical significance of the mediated effects and moderated mediated effects, we used the RMediation program (26), which provides 95% confidence intervals based on the product of coefficients approach (25,26). For all mediation and moderation models, we controlled for treatment site by using the sandwich estimator in Mplus (27). We conducted moderated mediation analyses to examine whether the mediational effect of coping in CBT was moderated by baseline alcohol dependence severity. The moderator variable used in moderated mediation models was a continuous variable derived from the total score on the ADS. Figure 1 shows the conceptual model for the hypothesized moderated mediation effect. The two primary outcomes were PDD and PHD at the one-year follow-up. We utilized dummy-coded treatment variables (e.g., CBT dummy variable: 1 = CBT, 0= other treatment; TSF dummy variable: 1 = TSF, 0 = other treatment; with MET as the reference group). We multiplied the treatment dummy-coded variables with ADS scores (mean–centered) to create interaction terms. For each moderated mediation model, we included the following: a) the dummy-coded treatment variables and the two interaction terms as predictors of end-of-treatment coping and the one-year outcome, b) the moderator variable (ADS scores) as a predictor of coping and one-year outcome, c) coping as a predictor of one-year outcome, and d) a set of covariates as predictors of coping and one-year outcome. For the moderated mediation models, the set of covariates included: baseline score for the drinking outcome variable, first treatment session coping, age, gender, marital status (married vs. not married), race (white vs. non-white), baseline readiness to change, and baseline self-efficacy. These covariates were chosen based on variables associated with coping and treatment outcome found in prior analyses of Project MATCH data (1,28) and based on missing data analyses described in the Results section.
Figure 1.
Conceptual Model for the Moderated Mediation Effect.
Effect sizes for moderated mediated effects (i.e., conditional indirect effects) were computed as kappa-squared estimates (k2), with 0.01, 0.025, and 0.09 estimates considered small, medium, and large effects (29). In order to ascertain the specific nature of significant moderated mediation effects, we conducted two follow-up analyses. First, we tested the indirect effect of treatment on outcomes via coping among individuals at high (1 SD above mean) and low levels of ADS (1 SD below mean). Second, we conducted mediation analyses within each treatment group to examine the within-treatment group associations among baseline dependence severity, coping, and drinking outcomes.
The moderated mediation analyses were first conducted in the full sample. In order to determine whether moderated mediation analyses should be conducted in each treatment arm separately, we also tested the treatment condition x treatment arm x baseline dependence severity → coping → drinking outcome effects (i.e., double moderated mediation effects). We planned to conduct moderated mediation analyses in each treatment arm separately if these effects were statistically significant for each treatment comparison. Finally, parameters were estimated using maximum likelihood estimation and thus all available data were included in analyses (30).
Results
Missing Data Analyses
No study variables were significantly related to having missing data on coping at end-of-treatment. However, several study variables were related to having missing data on coping at the first treatment session. Treatment arm (χ2 (1) = 137.64, p < .001), gender (χ2 (1) = 12.93, p < .001), marital status (χ2 (1) = 4.30, p = .038), race/ethnicity (χ2 (1) = 10.07, p =.002), age (t (1583) = − 7.55, p < .001), baseline PDD (t (1584) = −4.71, p < .001), and baseline PHD (t (1584) = −5.66, p < .001). Compared to participants with data on coping at the first treatment session, participants with missing data on coping at the first treatment session were more likely to be in the outpatient arm, female, non-married, and non-white, and were older, had higher baseline PDD, and higher baseline PHD. Missing data on coping at the first treatment session was not significantly related to treatment assignment, baseline dependence severity, baseline readiness to change, and baseline self-efficacy. All study variables that were related to missing data on coping at the first treatment session were included as covariates in mediation and moderated mediation analyses.
Moderated Mediation Models
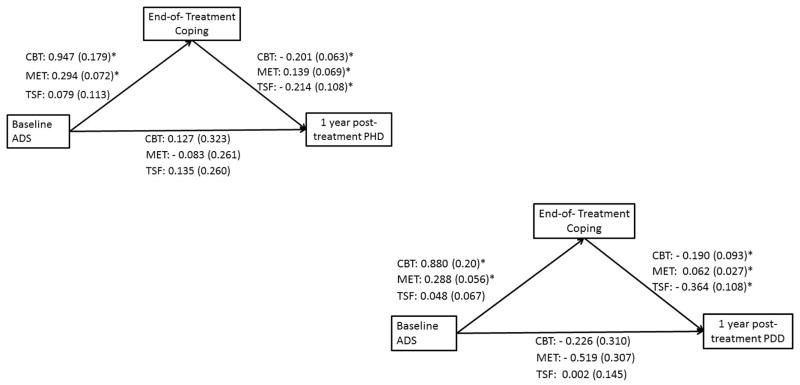
As seen in Table 2, there were no significant moderated mediation effects among the full available sample (across both treatment arms). As seen in Table 3, the treatment condition x baseline dependence severity x treatment arm → coping → drinking outcome effects (i.e., double moderated mediation effects) were significant for the CBT vs MET and the CBT vs. TSF comparisons, but not the TSF vs. MET comparison. Hence, we proceeded to conduct moderated mediation models by treatment arm with the CBT vs MET and CBT vs. TSF comparisons. Several significant moderated mediation effects were found in the outpatient sample (see Table 4). Among individuals in the outpatient sample only, the interaction of baseline dependence severity and the CBT vs. MET comparison had a significant indirect effect on one-year PDD (B (SE) = − 0.10 (0.060), p < 0.05, effect size k2 = 0.012) via end-of-treatment coping. As seen in Table 5, among those with high ADS (1 SD above mean) there was a significant negative indirect effect of CBT vs. MET on one-year PDD via end-of-treatment coping. However, this indirect effect was non-significant for those with low ADS (1 SD below mean) and moderate ADS (>1 SD below mean and < 1 SD above mean). Additional follow-up analyses aimed at probing the moderated mediated effect (see Figure 2) demonstrated the following: 1) among the CBT group only, baseline dependence severity was positively associated with coping, and coping was negatively associated with one-year PDD, and 2) among the MET group only, baseline dependence severity was positively associated with coping, but coping was positively associated with one-year PDD.
Table 2.
Summary of Results from Moderated Mediation Models among Full Available Sample (n=1063)
| Model for One-Year Post-Treatment Percent Drinking Days (PDD) | |
|---|---|
| CBT vs. MET x Baseline Dependence Severity → Coping → One-Year PDD | B (SE) = 0.01 (0.05) 95% CI [−0.11, 0.11] |
| CBT vs. TSF X Baseline Dependence Severity → Coping → One-Year PDD | B (SE) = − 0.06 (0.05) 95% CI [−0.17, 0.03] |
| TSF vs. MET X Baseline Dependence Severity → Coping → One-Year PDD | B (SE) = 0.06 (0.05) 95% CI [−0.02, 0.17] |
|
| |
| Model for One-Year Post-Treatment Percent Heavy Drinking Days (PHD) | |
| CBT vs. MET x Baseline Dependence Severity → Coping → One-Year PHD | B (SE) = 0.02 (0.04) 95% CI [−0.09, 0.08] |
| CBT vs. TSF X Baseline Dependence Severity → Coping → One-Year PHD | B (SE) = − 0.04 (0.04) 95% CI [−0.12, 0.02] |
| TSF vs. MET X Baseline Dependence Severity → Coping → One-Year PHD | B (SE) = 0.04 (0.04) 95% CI [−0.02, 0.12] |
Note.
p < 0.05;
B = unstandardized regression coefficient; SE = Standard Error); 95 % confidence intervals for moderated meditated effect computed using the distribution of the product of coefficients method. PDD = Percent Drinking Days; PHD = Percent Heavy Drinking Days. MET = Motivational enhancement therapy; TSF =Twelve-step facilitation therapy; CBT = Cognitive-behavioral therapy.
Table 3.
Summary of Results from Double Moderated Mediation Models
| Model for One-Year Post-Treatment Percent Drinking Days (PDD) | |
|---|---|
| CBT vs. MET x Baseline Dependence Severity X Treatment Arm → Coping → One-Year PDD | B (SE) = − 0.15 (0.08)* 95% CI [−0.33, −0.02] |
| CBT vs. TSF X Baseline Dependence Severity X Treatment Arm → Coping → One-Year PDD | B (SE) = − 0.17 (0.09)* 95% CI [−0.37, 0.02] |
| TSF vs. MET X Baseline Dependence Severity X Treatment Arm → Coping → One-Year PDD | B (SE) = − 0.09 (0.11) 95% CI [−0.35, 0.12] |
|
| |
| Model for One-Year Post-Treatment Percent Heavy Drinking Days (PHD) | |
| CBT vs. MET x Baseline Dependence Severity X Treatment Arm → Coping → One-Year PHD | B (SE) = − 0.09 (0.39)* 95% CI [−1.68, −0.15] |
| CBT vs. TSF X Baseline Dependence Severity X Treatment Arm → Coping → One-Year PHD | B (SE) = − 0.11 (0.06)* 95% CI [−0.26, −0.01] |
| TSF vs. MET X Baseline Dependence Severity X Treatment Arm → Coping → One-Year PHD | B (SE) = −0.06 (0.08) 95% CI [−0.26, 0.08] |
Note.
p < 0.05;
B = unstandardized regression coefficient; SE = Standard Error); 95 % confidence intervals for moderated meditated effect computed using the distribution of the product of coefficients method. PDD = Percent Drinking Days; PHD = Percent Heavy Drinking Days. MET = Motivational enhancement therapy; TSF =Twelve-step facilitation therapy. Treatment arm coded 0 = outpatient treatment arm, 1 =aftercare treatment arm.
Table 4.
Summary of Results from Moderated Mediation Models by Treatment Arm with CBT vs. MET and CBT vs. TSF comparisons
| Model for One-Year Post-Treatment Percent Drinking Days (PDD)
| ||
|---|---|---|
| Results for Outpatient Sample Only | Results for Aftercare Sample Only | |
|
| ||
| B (SE) | B (SE) | |
| Baseline Dependence Severity → Coping | 0.81 (0.20)* | 0.07 (0.24) |
| CBT vs. MET → Coping | 1.03 (0.99) | 1.14 (2.56) |
| CBT vs. TSF → Coping | 0.54 (2.40) | 0.57 (4.41) |
| CBT vs. MET X Baseline Dependence Severity → Coping (Moderation Effect) | 0.56 (0.27)* | − 0.38 (0.21) |
| CBT vs. TSF X Baseline Dependence Severity → Coping (Moderation Effect) | 0.55 (0.23)* | 0.09 (0.38) |
| Baseline Dependence Severity → One-Year PDD | − 0.33 (0.28) | − 0.05 (0.17) |
| Coping → One-Year PDD | − 0.18 (0.06) | − 0.27 (0.10) |
| CBT vs. MET → One-Year PDD | 0.57 (1.79) | − 2.36 (3.05) |
| CBT vs. TSF → One-Year PDD | − 0.34 (2.34) | 4.06 (3.87) |
| CBT vs. MET x Baseline Dependence Severity → One-Year PDD (Moderation Effect) | − 0.01 (0.67) | 0.11 (0.31) |
| CBT vs. TSF X Baseline Dependence Severity → One-Year PDD (Moderation Effect) | − 0.23 (0.25) | − 0.77 (0.23)* |
| CBT vs. MET x Baseline Dependence Severity → Coping → One-Year PDD (Moderated Mediation Effect) | − 0.10 (.06)* 95% CI [−0.24, − 0.003] |
0.10 (0.07) 95% CI [−0.01, 0.27] |
| CBT vs. TSF X Baseline Dependence Severity → Coping → One-Year PDD (Moderated Mediation Effect) | − 0.10 (0.055)* 95% CI [− 0.22, − 0.012] |
− 0.02 (0.11) 95% CI [−0.26, 0.20] |
|
| ||
|
Model for One-Year Post-Treatment Percent Heavy Drinking Days (PHD)
| ||
| Results for Outpatient Sample Only | Results for Aftercare Sample Only | |
|
| ||
| B (SE) | B (SE) | |
| Baseline Dependence Severity→ Coping | 0.85 (0.21)* | 0.06 (0.23) |
| CBT vs. MET → Coping | 0.99 (1.10) | 1.29 (2.45) |
| CBT vs. TSF → Coping | 0.59 (2.46) | 0.51 (4.45) |
| CBT vs. MET X Baseline Dependence Severity → Coping (Moderation Effect) | 0.58 (0.28)* | − 0.41 (0.21) |
| CBT vs. TSF X Baseline Dependence Severity → Coping (Moderation Effect) | 0.55 (0.24)* | 0.08 (0.38) |
| Baseline Dependence Severity → One-Year PHD | − 0.11 (0.29) | 0.10 (0.15) |
| Coping → One-Year PHD | − 0.11 (0.046)* | − 0.22 (0.08)* |
| CBT vs. MET → One-Year PHD | − 0.21 (1.52) | − 2.49 (2.99) |
| CBT vs. TSF → One-Year PHD | − 3.05 (1.38)* | 1.22 (2.54) |
| CBT vs. MET x Baseline Dependence Severity → One-Year PHD (Moderation Effect) | − 0.06 (0.64) | 0.04 (0.29) |
| CBT vs. TSF X Baseline Dependence Severity → One-Year PHD (Moderation Effect) | − 0.31 (0.45) | − 0.62 (0.24)* |
| CBT vs. MET x Baseline Dependence Severity → Coping → One-Year PHD (Moderated Mediation Effect) | − 0.06 (0.045) 95% CI [−0.17, 0.002] |
0.09 (0.06) 95% CI [−0.002, 0.226] |
| CBT vs. TSF X Baseline Dependence Severity → Coping → One-Year PHD (Moderated Mediation Effect) | − 0.061 (0.038)* 95% CI [−0.15, −0.002] |
− 0.02 (0.09) 95% CI [−0.21, 0.161] |
Note.
p < 0.05;
B = unstandardized regression coefficient; SE = Standard Error); 95 % confidence intervals for moderated meditated effect computed using the distribution of the product of coefficients method. PDD = Percent Drinking Days; PHD = Percent Heavy Drinking Days. MET = Motivational enhancement therapy; TSF =Twelve-step facilitation therapy.
Table 5.
Indirect Effects of Treatment via Coping among Individuals with High, Moderate, and Low ADS Scores in the Outpatient Arm
| Model for One-Year Post-Treatment Percent Drinking Days (PDD)
| |||
|---|---|---|---|
| High ADS (1 SD above mean) | Moderate ADS (< 1 SD below mean and < 1 SD above mean) | Low ADS (1 SD below mean) | |
|
| |||
| B (SE) | B (SE) | B (SE) | |
| CBT vs. MET → Coping → One-Year PDD | −6.80 (2.6)* 95% CI [−12.50, −2.43] |
−0.25 (0.38) 95% CI [−1.10, 0.45] |
3.10 (2.55) 95% CI [−0.61, 9.17] |
| CBT vs. TSF → Coping → One-Year PDD | −2.54 (1.28)* 95% CI [−5.35, −0.34] |
−0.46 (0.52) 95% CI [−1.73, 0.32] |
3.90 (2.54) 95% CI [−0.30, 9.58] |
|
| |||
|
Model for One-Year Post-Treatment Percent Heavy Drinking Days (PHD)
| |||
| High ADS (1 SD above mean) | Moderate ADS (< 1 SD below mean and < 1 SD above mean) | Low ADS (1 SD below mean) | |
|
| |||
| B (SE) | B (SE) | B (SE) | |
| CBT vs. TSF → Coping → One-Year PHD | −2.17 (1.14)* 95% CI [−4.72, −0.26] |
−0.39 (0.27) 95% CI [−1.02, 0.01] |
0.40 (2.13) 95% CI [−3.84, 4.77] |
Note.
p < 0.05;
B = unstandardized regression coefficient; SE = Standard Error); 95 % confidence intervals for indirect effects computed using the distribution of the product of coefficients method. PDD = Percent Drinking Days; PHD = Percent Heavy Drinking Days. MET = Motivational enhancement therapy; TSF =Twelve-step facilitation therapy.
Figure 2.
Summary of Results from Mediation Models within Treatment Group in the Outpatient Arm. ADS = Alcohol Dependence Severity; PDD = Percent Drinking Days; PHD = Percent Heavy Drinking Days. * p < 0.05
Among individuals in the outpatient sample only, the interaction of baseline dependence severity and the CBT vs. TSF comparison had a significant indirect effect on one-year PDD (B (SE) = − 0.010 (0.055), p < 0.05, effect size k2 = 0.012) and on one-year PHD (B (SE) = − 0.06 (0.038), p < 0.05, effect size k2 = 0.010) via end-of-treatment coping. As seen in Table 5, among those with high ADS (1 SD above mean) there were significant negative indirect effects of CBT vs. TSF on one-year PDD and PHD via end-of-treatment coping. However, these indirect effects were non-significant for those with low ADS (1 SD below mean) and moderate ADS (>1 SD below mean and < 1 SD above mean). Additional follow-up analyses aimed at probing the moderated mediated effects (see Figure 2) demonstrated the following: 1) among those in the CBT group only, baseline dependence severity was positively associated with coping, and coping was negatively associated with one-year PHD and PDD, and 2) among those in the TSF group only, baseline dependence severity was not significantly associated with coping, and coping was negatively associated with one-year PHD and PDD.
Discussion
This study utilized moderated mediation analyses to investigate the use of alcohol-specific coping skills as a mechanism of change following three psychosocial treatments for alcohol use disorder in Project MATCH (1): cognitive-behavioral therapy (CBT), motivational enhancement therapy (MET), and twelve-step facilitation (TSF). We hypothesized that coping would mediate the positive treatment effects of CBT, as compared to MET and TSF, when dependence severity was high. As predicted, results demonstrated that coping mediated the positive treatment effect of CBT, as compared to both TSF and MET, on one-year post-treatment drinking outcomes when dependence severity was high, but not when dependence severity was low or moderate. The fact that significant moderated mediated effects were found for long-term drinking outcomes suggests that these effects may be substantive. However, it is also important to note that the effect sizes for these moderated mediated effects were in the small range. Hence, for individuals with high dependence severity who are presenting to outpatient treatment, CBT may exert its therapeutic effects by enhancing the use of alcohol-specific coping skills. These results are consistent with social-cognitive theory, which postulates that CBT reduces excessive drinking by addressing deficits in coping abilities (11).
The current study’s findings are also consistent with the notion that high dependence severity may warrant greater need to utilize alcohol-specific coping skills during the change process. Moreover, our findings suggest the systematic focus on coping skills in CBT is more effective than MET and TSF in facilitating the use of coping skills among individuals with high dependence severity. In the current study we examined total coping scores at end-of-treatment from the Processes of Change Questionnaire (PCQ), a measure that includes 10 different types of coping skills. Higher total scores on the PCQ at end-of-treatment may indicate an increased frequency of using particular skills and/or a broadening of one’s overall repertoire of skills. Of note, our recent investigation of patterns of coping in the Project MATCH and COMBINE study data suggests that broadening one’s repertoire of skills may be one key way in which individuals change their coping skills (28). It is possible that broadening one’s overall repertoire of skills may be particularly important for individuals with high dependence severity. For example, it may be the case that frequently using a broad range of skills may enable individuals with high dependence severity to adequately manage the range of challenges that can arise during the change process (e.g., negative affect, craving, lapses, etc.). Future work is needed to evaluate whether a broad repertoire is particularly helpful for individuals with high dependence severity and whether CBT is a particularly suitable treatment for broadening these individuals’ coping repertoires.
The finding that coping mediated the positive effects of CBT when dependence severity was high was not found in the aftercare sample. Descriptive analyses showed that clients in the aftercare sample had higher scores on coping at the first treatment session relative to clients in the outpatient sample. Thus, CBT may not exert its therapeutic effects by enhancing coping among aftercare clients because these clients may have been exposed to coping skills training during prior treatment and appear to be already using coping skills at the start of aftercare treatment.
The current study findings suggest that one potential reason for null findings regarding the mediating role of coping in CBT for AUD is that prior studies have not considered the moderating role of dependence severity. Our findings indicate that among individuals with low or moderate dependence severity CBT may work through mechanisms of change other than coping, such as the therapeutic alliance or perhaps self-efficacy. We also found that TSF did not mobilize coping to a greater degree than MET, despite the fact that TSF provides a greater emphasis on coping skills relative to MET. However, higher coping at the end-of-treatment was related to better drinking outcomes among those who received TSF in the outpatient sample, whereas higher coping at the end-of treatment was actually related to worse drinking among those who received MET in the outpatient sample. The positive relation between coping and drinking among those who received MET was unexpected. One possibility is that this effect was driven by MET participants with higher levels of dependence severity who increased their use of coping skills during treatment but were not able to sustain their use of coping skills in the long-term, which in turn led to poorer one-year drinking outcomes. However, it is also possible the positive relation between coping and drinking outcomes among MET participants is spurious. Overall, this finding should be interpreted with caution.
There are several limitations of this study that warrant mention. Initial pre-treatment coping was measured at the first treatment session rather than at baseline, and a substantial portion of the full sample was missing data on first treatment session coping. It is possible that the results from the available sample are biased, because there are variables related to missing data that we did not account for. The measure of coping at the first treatment session was also an abbreviated version of the Processes of Change Questionnaire (PCQ) and was not identical to the end-of-treatment measure of coping. Finally, the effect sizes for significant effects were relatively small, and a large number of statistical tests were conducted.
In conclusion, this study showed that for when dependence severity was high among clients in the outpatient sample, end-of-treatment coping mediated the positive treatment effects of CBT, as compared to both MET and TSF, on one-year post-treatment drinking outcomes. Thus, coping appears to be a plausible mechanism of change in CBT for AUD for clients who present to outpatient treatment with high dependence severity, but not for those with low dependence severity. Importantly, the notion that coping may function as a mechanism of change for some CBT clients and not others may explain why many prior studies, which have examined the mediating role across all clients, have failed to support coping as a mechanism of change in CBT (10,11). As noted by others (11), the mixed evidence in support of coping as a mechanisms of change in CBT for AUD might also be related to a lack of well-validated measures of coping. The current study findings and a recent study that examined patterns of alcohol-specific coping using the PCQ (28) suggest that the PCQ may be a useful measure for further research on coping as a mechanisms of change in alcohol treatment. Future studies testing hypotheses of moderated mediation are warranted to replicate the current findings and to investigate whether the mediating role of coping in CBT for AUD is contingent, at least in part, on individual difference factors.
Acknowledgments
This research was supported by grants funded by the National Institute on Alcohol Abuse and Alcoholism, including support for SAM and KW (R01 AA022328, Witkiewitz, PI), support for SAM (2K05 AA016928), and support for CR (T32 AA018108, McCrady, PI).
Footnotes
Conflicts of Interest Declaration: None
References
- 1.Project MATCH Research Group. Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997 Jan;58(1):7–29. [PubMed] [Google Scholar]
- 2.Prochaska JO, Velicer WF, DiClemente CC, Fava J. Measuring processes of change: applications to the cessation of smoking. J Consult Clin Psychol. 1988 Aug;56(4):520–8. doi: 10.1037//0022-006x.56.4.520. [DOI] [PubMed] [Google Scholar]
- 3.Skinner Ha, Allen Ba. Alcohol dependence syndrome: measurement and validation. J Abnorm Psychol. 1982;91(3):199–209. doi: 10.1037//0021-843x.91.3.199. [DOI] [PubMed] [Google Scholar]
- 4.Kadden RM, Carroll KM, Donovan DM, Cooney NL, Monti PM, Abrams DB, et al. Cognitive-Behavioral coping skills therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. Rockville, Maryland: NIAAA; 1992. [Google Scholar]
- 5.Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational enhancement therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. NIH publication. U.S. Dept. of Health and Human Services, Public Health Service, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism; 1999. p. xv.p. 121. [Google Scholar]
- 6.Nowinski J, Baker S, Carroll K. Twelve step facilitation therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. 1992;1 Project MATCH Monograph Series. [Google Scholar]
- 7.Miller WR, Wilbourne PL. Mesa Grande: A methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction. 2002;97:265–77. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- 8.Longabaugh R, Magill M. Recent advances in behavioral addiction treatments: focusing on mechanisms of change. Curr Psychiatry Rep. 2011 Oct;13(5):382–9. doi: 10.1007/s11920-011-0220-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kiluk BD, Nich C, Babuscio T, Carroll KM. Quality versus quantity: Acquisition of coping skills following computerized cognitive-behavioral therapy for substance use disorders. Addiction. 2010;105(12):2120–7. doi: 10.1111/j.1360-0443.2010.03076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Litt MD, Kadden RM, Cooney NL, Kabela E. Coping skills and treatment outcomes in cognitive-behavioral and interactional group therapy for alcoholism. J Consult Clin Psychol. 2003;71(1):118–28. doi: 10.1037//0022-006x.71.1.118. [DOI] [PubMed] [Google Scholar]
- 11.Morgenstern J, Longabaugh R. Cognitive-behavioral treatment for alcohol dependence: a review of evidence for its hypothesized mechanisms of action. Addiction. 2000;95(10):1475–90. doi: 10.1046/j.1360-0443.2000.951014753.x. [DOI] [PubMed] [Google Scholar]
- 12.Litt MD, Kadden RM, Kabela-cormier E. Individualized assessment and treatment program for alcohol dependence: results of an initial study to train coping Skills. 2010;104(11):1837–8. doi: 10.1111/j.1360-0443.2009.02693.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behav Res. 2007;42(1):185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- 14.Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: that was Zen, this is Tao. Am Psychol. 2004;59(4):224–35. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- 15.Witkiewitz K, Hallgren KA, O’Sickey AJ, Roos CR, Maisto SA. Reproducibility and differential item functioning of the alcohol dependence syndrome construct across four alcohol treatment studies: An integrative data analysis. Drug Alcohol Depend. 2016;158:86–93. doi: 10.1016/j.drugalcdep.2015.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Edwards G, Gross MM. Alcohol dependence: provisional description of a clinical syndrome. Br Med J. 1976;1(May):1058–61. doi: 10.1136/bmj.1.6017.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dolan SL, Rohsenow DJ, Martin RA, Monti PM. Urge-specific and lifestyle coping strategies of alcoholics: Relationships of specific strategies to treatment outcome. Drug Alcohol Depend. 2013;128(1–2):8–14. doi: 10.1016/j.drugalcdep.2012.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Finney JW, Noyes Ca, Coutts aI, Moos RH. Evaluating substance abuse treatment process models: I. Changes on proximal outcome variables during 12-step and cognitive-behavioral treatment. J Stud Alcohol. 1998;59(4):371–80. doi: 10.15288/jsa.1998.59.371. [DOI] [PubMed] [Google Scholar]
- 19.DiClemente CC, Carbonari JP, Zweben A, Morrell T, Lee R. Motivation Hypothesis Causal Chain Analysis. Proj MATCH Monogr Ser. 2001:8. (Project MATCH: Hypotheses, Results, and Causal Chain Analyses) [Google Scholar]
- 20.Group PMR. Project MATCH: Rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcohol Clin Exp Res. 1993;17(6):1130–45. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- 21.Miller WR. FORM 90: A structured assessment interview for drinking and related behaviors test manual. Vol. 5. NIAAA; 1996. [Google Scholar]
- 22.McConnaughy EA, Prochaska JO, Velicer WF. Stages of change in psychotherapy: Measurement and sample profiles. Psychother Theory, Res Pract. 1983;20(3):368–75. [Google Scholar]
- 23.DiClemente CC, Carbonari JP, Montgomery RP, Hughes SO. The alcohol abstinence self-efficacy scale. J Stud Alcohol. 1994;55(2):141–8. doi: 10.15288/jsa.1994.55.141. [DOI] [PubMed] [Google Scholar]
- 24.Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, California: Muthén & Muthén;; [Google Scholar]
- 25.MacKinnon D. Introduction to statistical mediation analysis. New York: Taylor & Francis Group; 2008. [Google Scholar]
- 26.Tofighi D, MacKinnon DP. RMediation: an R package for mediation analysis confidence intervals. Behav Res Methods. 2011 Sep;43(3):692–700. doi: 10.3758/s13428-011-0076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48(4):817–38. [Google Scholar]
- 28.Roos C, Witkiewitz K. Adding tools to the toolbox: The role of coping repertoire in alcohol treatment. J Consult Clin Psychol. 84:599–611. doi: 10.1037/ccp0000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Preacher KJ, Kelley K. Effect size measures for mediation models: quantitative strategies for communicating indirect effects. Psychol Methods. 2011;16(2):93–115. doi: 10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- 30.Hallgren KA, Witkiewitz K. Missing data in alcohol clinical trials: A comparison of methods. Alcohol Clin Exp Res. 2013;37(12):2152–60. doi: 10.1111/acer.12205. [DOI] [PMC free article] [PubMed] [Google Scholar]