Abstract
The purpose of this review is to describe recent clinical and epidemiological studies examining the adverse effects of urban air pollution on the central nervous system (CNS). Air pollution and particulate matter (PM) are associated with neuroinflammation and reactive oxygen species (ROS). These processes affect multiple CNS pathways. The conceptual framework of this review focuses on adverse effects of air pollution with respect to neurocognition, white matter disease, stroke, and carotid artery disease. Both children and older individuals exposed to air pollution exhibit signs of cognitive dysfunction. However, evidence on middle-aged cohorts is lacking. White matter injury secondary to air pollution exposure is a putative mechanism for neurocognitive decline. Air pollution is associated with exacerbations of neurodegenerative conditions such as Alzheimer’s and Parkinson’s Diseases. Increases in stroke incidences and mortalities are seen in the setting of air pollution exposure and CNS pathology is robust. Large populations living in highly polluted environments are at risk. This review aims to outline current knowledge of air pollution exposure effects on neurological health.
Keywords: Air pollution, PM, Cognitive dysfunction, White matter disease, Stroke, Carotid artery disease
Introduction
The adverse effects of ambient air pollution on respiratory and cardiovascular health are firmly established. However, impact on the central nervous system (CNS) was first described only a decade ago.[1] A significant number of clinical and epidemiological studies indicate adverse associations between air pollution and neurological disease, but mechanistic pathways remain elusive.
Ambient air pollution is a mixture of gases and particulate matter released into the surrounding air by stationary (industrial and household etc.) and mobile (vehicles, trains, ships etc.) sources.[2] The gaseous mixture is primarily composed of Carbon Monoxide (CO), Ozone (O3), Nitrogen dioxide (NO2) and Sulfur dioxide (SO2).[2] These chemical constituents are all implicated in human pathophysiology. However, studies suggest particulate matter <250 nm (PM2.5) as a principal antagonist due to small aerodynamic diameter and ability to traverse the alveolar region of the respiratory system.[3] Of relevance to the present review, PM2.5 is also the component most consistently implicated in adverse neurological processes.[4]
Air pollution and particulate matter are persistent sources of neuroinflammation and reactive oxygen species (ROS); processes strongly related to the pathogenesis of CNS diseases.[4–6] Air pollution exposure is associated with exacerbated cognitive dysfunction and enhanced progression of neurodegenerative processes underlying Alzheimer’s (AD) and Parkinson’s diseases (PD). Further, studies demonstrate evidence of structural brain effects such as white matter injury. Exposure is also associated with adverse vascular effects. The relationship between stroke and air pollution has been established over the past decade. Growing evidence supports a role in facilitating the process of atherosclerosis, particularly carotid artery disease. Air pollution exposure strongly influences CNS development and disease. This review aims to examine clinical and epidemiological effects of air pollution and its association with CNS pathologies to better set the stage for further investigation.
Study identification
The database used in the preparation of this review was PubMed, accessing dates between 2004 and 2017. Search criteria were based off the four following primary sections: cognitive dysfunction, stroke, carotid artery disease and white matter damage (Table 1). A total of 482 articles were identified.
Table 1.
Search Criteria
| Section | Search Terms |
|---|---|
| Cognitive dysfunction |
|
| Stroke |
|
| Carotid Artery Disease |
|
| White Matter Damage |
|
Inclusion criteria:
Clinical and epidemiological studies including human subjects.
Studies including all known constituents of air pollution.
Studies examining cognitive dysfunction, stroke, carotid artery disease, white matter damage.
Exclusion criteria:
All animal studies.
Publications were only included if they met inclusion criteria. Initial screening included screening title and abstract of articles with further screening of article text in certain cases. 243 articles were included in the initial screen. 95 relevant articles were included in the writing of this review (Figure 1).
Figure 1.
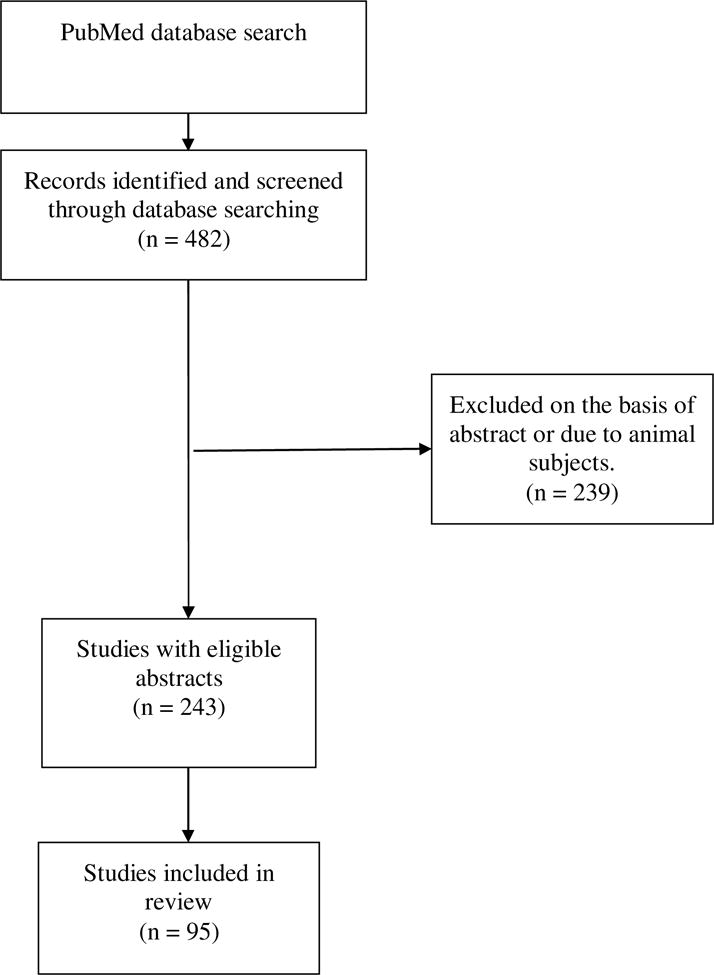
Search strategy.
Air pollution and Cognitive Dysfunction
An association between air pollution and CNS impairment was first reported in the year 2000 in a small cohort of men exposed to diesel exhaust.[1] Ever since, studies of the relationship between air pollution and cognitive function have been a point of focus. Residential proximity to a major roadway is a commonly accepted method for determining long-term air pollution exposure. Ranft et al. found that older individuals (ages 68–79), who lived near a major roadway for greater than 20 years, had an increased incidence of mild cognitive impairment. Authors also found a dose-response relationship between air pollution exposure and test performances.[7] A population based cohort study of 2.2 million individuals demonstrated an association between near-major-roadway residence and dementia incidence.[8] This finding was further supported by the U.S. Department of Veteran Affairs Normative Aging Study.[9] Major roadway proximity was associated with diminished verbal learning/memory, psychomotor speed, language, and executive functioning.[10] However, no associations are found for depressive symptoms.[11]
Particulate matter is an important element of near-roadway air pollution. Age and sex adjusted models suggest associations between particulate matter and cognitive dysfunction.[12, 13] A subset analysis of the Nurses’ Health Study Cognitive Cohort demonstrated significant cognitive decline in elderly women exposed to PM2.5.[14] A longitudinal study of a northern Sweden population conducted by Oudin et al. found an association between local traffic pollution and AD/vascular dementia.[15] Ailshire et al., still found an association between PM2.5 and cognitive dysfunction after adjusting for social and economic factors (Table 2).[16]
Table 2.
Air Pollution and Cognitive Dysfunction
| Author | Study | N | Age (years) | Air Pollutants | Summary |
|---|---|---|---|---|---|
| Kilburn et al., 2000 [1] | Effects of diesel exhaust on neurobehavioral and pulmonary functions | 16 | 42–60 | Diesel Exhaust | Significant association of diesel exhaust with decreased performance on neuropsychological tests |
| Ranft et al., 2009 [7] | Long-term exposure to traffic-related particulate matter impairs cognitive function in the elderly. | 399 | 68–79 | PM10 | Significant association of PM10 with mild cognitive impairment |
| Chen et al., 2017 [8] | Living near major roads and the incidence of dementia, Parkinson’s disease, and multiple sclerosis: a population-based cohort study | ~2.2 million | 55–85 | PM2.5, NO2, roadway proximity | Significant association of air pollution and roadway proximity with increased dementia incidence |
| Power et al., 2011 [9] | VA Normative Aging Study | 680 | 50–99 | Black Carbon | Significant association of black carbon with poor cognitive performance in older men |
| Wellenius et al., 2012 [10] | Residential proximity to nearest major roadway and cognitive function in community-dwelling seniors | 765 | ≥65 | Roadway proximity | Roadway proximity associated with decreased verbal learning/memory, psychomotor speed, language, and executive functioning |
| Wang et al., 2014 [11] | Ambient air pollution and depressive symptoms in older adults: results from the MOBILIZE Boston study | 732 | ≥65 | Roadway pollution | No association between ambient air pollution and depressive symptoms |
| Chen & Schwartz, 2009 [12] | Neurobehavioral effects of ambient air pollution on cognitive performance in US adults. | 1764 | 20–59 | PM2.5, O3 | Significant association of PM2.5 and O3 with poor results on neurobehavioral tests |
| Ailshire & Clarke, 2015 [13] | 2001/2002 Americans’ Changing Lives Study | 780 | ≥55 | PM2.5 | Significant association of PM2.5 and cognitive dysfunction |
| Weuve et al., 2012 [14] | Nurses’ Health Study Cognitive Cohort | 19,409 | 70–81 | PM10, PM2.5 | Significant association of PM10 and PM2.5 with cognitive decline in older women |
| Oudin et al., 2016 [15] | Betula Study | 1,806 | 55–85 | NOx | Significant association of NOx and AD/vascular dementia |
| Ailshire & Crimmins, 2014 [16] | Health and Retirement Study | 13,996 | 50–102 | PM2.5 | Significant association of PM2.5 with episodic memory impairment |
Air pollution is linked to the pathogenesis of neurodegenerative diseases such as PD and AD, which are associated with pronounced cognitive dysfunction. This was first observed by Ritz et al., who demonstrated a 9% increase in risk of developing PD among individuals living in Copenhagen when compared to rural residents.[17] Exposure time period is an important factor. Long-term exposure (>12 years) to PM is associated with an increased risk for AD in the elderly (>60 years old).[18] Increases in annual PM2.5 exposure are associated with time to first hospitalization for common neurodegenerative diseases (dementia, AD, and PD).[19] The associations between densely populated urban cities, poor socioeconomic environments, and high stress living conditions could potentially confound these relationships. Older adults with dementia demonstrate exacerbations with PM2.5 exposure and high stress living conditions.[20] Calderon-Garciduenas et al., suggest that carriers of the APOE4 allele, an independent risk factor for AD, are at higher risk of developing AD by living in a polluted environment.[21] Air pollution causes neuroinflammation and accumulation of AB42 and alpha-synuclein in the brain, providing a potential mechanism for neurodegeneration.[21, 22] Sex steroid hormones modulate multiple inflammatory pathways (APOE4, obesity, air pollution) involved in the pathogenesis of AD.[23] For example, the Estrogen Receptor-2 (ESR2) allele is implicated in gene-environment interactions.[24]
Ozone (O3) is strongly implicated in the pathophysiological influence of air pollution.[25] Substantial evidence supports respiratory health effects of O3,[26–28] but more recent studies show an association between O3 exposure and dementia. Many factors can affect the severity of cognitive dysfunction due to O3 exposure. Known influences include gender, body mass index (BMI), and presence of the APOE4 allele.[29] Epidemiological studies have examined the effects of O3 on cognition. Long term O3 exposure (14-years) is associated with increased risk for vascular dementia in the elderly.[18] Further, reduced exposure to O3 is associated with decreased hospital admissions.[30] A study in Taiwan demonstrated that high O3 concentration and particulate matter exposure were associated with a 211% and 138% increased risk of AD onset, respectively.[31] When considering populations susceptible to O3, those with dementia due to neurodegenerative diseases are at risk for further exacerbation. Of note, other components of air pollution, such as NO2 and CO are also associated with increased dementia risk.[32]
Discrete components of air pollution and their functional effects on cognition have been examined, albeit in a limited capacity. A single study demonstrated that PM is associated with lower verbal learning performance, NO2 is inversely associated with logical memory abilities, and O3 exposure is associated with lower executive functioning.[33]
Pediatric exposure to air pollution is of unique concern due to its adverse effect during critical years of central nervous system development. Young children in Mexico City exposed to PM and O3 concentrations above the current USA standards exhibit vascular and perivascular damage in the prefrontal white matter region. The Neurovascular units (NVU), comprised of tight junctions in endothelial cells, basement membrane, and perivascular glial sheets, were compromised in these children. NVU stability is important for maintaining brain health, whereas disruption is linked to neurodegenerative diseases including AD.[34] Children with lifetime air pollution exposures demonstrate significant increases in serum high affinity antibodies to tight junctions and neural proteins. Importantly, exposed urban children have CSF antibodies for myelin basic protein.[35] Cyclooxygenase-2 (COX2) and interleukin-1B (IL-1B) are also unregulated in the olfactory bulb and frontal cortex.[36] Further, the children exhibit astrocytic build up of B-amyloid peptide (AB42) in the frontal cortex.[36] Air pollution leads to olfactory bulb pathology in young healthy individuals, with greater vulnerability in carriers of the APOE4 allele. Collectively, these findings suggest strong proinflammatory and immune-upregulating capacities of air pollution; which may contribute to the pathogenesis of neurodegenerative disease.
Substantial evidence suggests that inflammatory mechanisms contribute to cognitive impairment secondary to air pollution exposure.[5, 37] Deregulation of fasting blood glucose may represent an additional risk factor. PM exposure is associated with higher fasting blood glucose (FBG; an independent risk factor for dementia) levels in non-diabetic individuals. Studies suggest that air pollution exposure upregulates ICAM-1 expression due to reduced epigenetic methylation secondary to high FBG.[38] This, in turn, may increase the ability for inflammatory mediators to penetrate the blood-brain barrier, leading to increased CNS inflammation.
Metabolic and structural brain alterations are observed in individuals exposed to air pollution. Children with prenatal and lifetime exposures to particulate matter demonstrate decreased hippocampal metabolite ratios; biomarker changes associated with mild cognitive impairment in mouse models of AD. This effect is exacerbated in APOE4 carriers.[39] Elevated levels of PM likely accelerate brain atrophy typically associated with aging.[40] Higher levels of PM exposure among community dwelling women >65 years of age are associated with significantly diminished white matter volumes on structural brain magnetic resonance imaging.[41]
Functional and structural CNS changes have been documented in both pediatric and elderly cohorts exposed to air pollution, however, little is known about mid-life exposures.
Air Pollution and White Matter Injury
Air pollution is associated with white matter injury, which can manifest as neurocognitive dysfunction. Voxel-based morphometry, a magnetic resonance imaging (MRI) technique that measures regional brain volumes and tissue concentration,[42] indicates that PM2.5 exposure is associated with smaller white matter volumes in the subcortical areas of the external capsule, extreme capsule, and calcarine cortex of older women. Interestingly, no clear associations were found between PM2.5 exposure and hippocampal volume, suggesting white matter damage as the primary insult.[43] Residence in a highly polluted environment is associated with white matter damage in children.[37, 44] A cohort of children living in Mexico City demonstrated subcortical and prefrontal white matter hyperintense lesions compared to aged matched controls.[37] These findings are further supported by experimental evidence in dogs.[37] Children carrying the APOE4 alleles demonstrated reductions in the right frontal white matter (Table 3).[45]
Table 3.
Air Pollution and White Matter Injury
| Author | Study | N | Air Pollutants | Summary |
|---|---|---|---|---|
| Casanova et al., 2016 [43] | A Voxel-Based Morphometry Study Reveals Local Brain Structural Alterations Associated with Ambient Fine Particles in Older Women | 1365 | PM2.5 | Significant association of PM2.5 exposure with smaller white matter volumes in the subcortical areas of the external capsule, extreme capsule, and calcarine cortex of older women |
| Calderon-Garciduenas et al., 2008 [37] | Air pollution, cognitive deficits and brain abnormalities: A pilot study with children and dogs | 73 | O3, PM10, SO2, NO2, CO, Pb | Significant association of highly polluted environment with white matter damage in children, namely the presence of subcortical and prefrontal white matter hyperintense lesions compared to aged matched controls |
| Calderon-Garciduenas et al., 2015 [45] | Decreases in Short Term Memory, IQ, and Altered Brain Metabolic Ratios in Urban Apolipoprotein 4 Children Exposed to Air Pollution | 50 | PM2.5, O3 | Children carrying the APOE e4 alleles demonstrated reductions in the right frontal white matter |
Air Pollution and Stroke
The impact of air pollution on ischemic/hemorrhagic stroke is under-recognized, yet substantial. The Global Burden of Disease Study 2013 found 29.2% of the global stroke burden was attributable to air pollution.[46] Satellite reconstruction of PM2.5 concentrations across China reveals changes in spatial distribution over time. Strikingly, the 3.25% annual growth rate in stroke mortality is attributable to increased stroke incidences in areas of highest outdoor exposure to PM2.5.[47] A recent study suggests that PM2.5 increases stroke mortality rate, number of hospital admission days, and related healthcare costs.[48]
Meta Analyses of Air Pollution and Stroke
To date, several meta-analyses examining the association between air pollution and stroke incidence have been conducted. A recent meta-analysis of 20 epidemiological studies examined the association between stroke incidence/mortality and long-term exposure to PM. Exposure to PM10 (which included results from PM2.5) resulted in pooled hazard ratios of 1.061 (95% CI, 1.018–1.105) and 1.080 (0.992–1.177) for stroke events and stroke mortality, respectively. A high degree of heterogeneity was found when results were stratified by continent. A positive correlation between long term PM10 exposure and stroke events was evident in Europe and North America, however results were more ambiguous in Asia.[49] A meta-analysis of 94 studies found stroke hospital admissions to be associated with high concentrations of CO, SO2 and NO2. Hospital admissions with subsequent mortality due to stroke were primarily associated with increases in PM2.5 and PM10, with weaker, but still significant, effects with O3.[50] Additional inconsistencies and non-significant associations are documented for analyses examining hospital admissions of certain stroke sub-types.[51] While greater caution should be exercised when interpreting these conclusions, they may prove informative for future studies. A 2014 meta-analysis including 34 studies examined the transient effects of air pollution. Findings suggest increased risk for hospitalization and subsequent stroke mortality following a transient increase in the following constituents: PM2.5, PM10, SO2, CO and NO2. Further, this study found a stronger association with ischemic versus hemorrhagic stroke.[52] The European Study of Cohorts for Air Pollution Effects (ESCAPE) project reported that small increases (5 um/m3) in PM2.5 were associated with 19% increased risk in stroke. Robust findings were manifest in those greater than 60 years of age and among never-smokers (Table 4).[53]
Table 4.
Meta Analyses of Air Pollution and Stroke
| Author | Study | Number of studies | Air Pollutants | Summary |
|---|---|---|---|---|
| Scheers et al., 2015 [49] | Long-Term Exposure to Particulate Matter Air Pollution Is a Risk Factor for Stroke: Meta-Analytical Evidence | 20 studies | PM2.5, PM10 | Increase in stroke events and stroke mortality. Continental geographic variability shown |
| Shah et al., 2015 [50] | Short term exposure to air pollution and stroke: systematic review and meta-analysis | 94 studies | PM2.5, PM10, SO2, CO and NO2 | Increases in hospital admissions and mortality due to stroke |
| Wang et al., 2014 [51] | Short-term changes in ambient particulate matter and risk of stroke: a systematic review and meta-analysis | 45 studies | PM2.5, PM10 | Increases in total cerebrovascular disease mortality |
| Yang et al., 2014 [52] | An evidence-based appraisal of global association between air pollution and risk of stroke | 34 studies | PM2.5, PM10, SO2, CO and NO2 | Transient increases in air pollution increase risk of stroke hospitalization and mortality |
Air Pollution and Stroke Admissions
Levels of air pollution directly correlate with the number of ischemic stroke admissions to the emergency department.[54] Positive associations exist for both ischemic and hemorrhagic stroke. Studies examining the effect of air pollution on cerebrovascular hospital admissions likely underestimate the strength of associations due to study design.[55] As evidenced throughout this section, many of these relationships are more pronounced within specific demographic subgroups.
Ambient temperature may influence air pollution and associated hospital admissions for stroke. PM2.5 is associated with increased hemorrhagic stroke admissions on both warm (>23 C) and cold (< 23 C) days.[56] Further, PM2.5 increases the relative risk of hospital admissions caused by ischemic stroke by 11% on warm days (>23 C) and by 4% on cold days (<23 C) in Taiwan.[57] Warm temperature (>13.5 C) was associated with increased hospital admissions for ischemic and hemorrhagic stroke during short-term exposure to PM2.5, PM2.5–10 and PM10 individually.[58] Increased NO2 exposure is positively associated with stroke admissions during the cold season in Wuhan, China, where air pollution concentrations are 50% greater in the winter.[59]
Specific constituents of PM2.5 (nitrate, sulfate, organic carbon and elemental carbon) are individually associated with emergency room visits for hemorrhagic stroke.[60] Increases in same day 03 exposures are associated with a 1.9% higher total stroke hospitalization risk.[61] Men are more sensitive to the adverse effects of O3,[61] and risk of hemorrhagic stroke hospitalization is higher among African American individuals than European Americans.[62] There is also a positive correlation between stroke admissions and NO2 levels,[63] with long-term exposure increasing the risk of subsequent 30-day mortality.[64] Same day exposure to PM, SO2, and O3 are all associated with an increased risk of hospitalization due to stroke (Table 5).[65]
Table 5.
Air Pollution and Stroke Admissions
| Author | Study | N | Air Pollutants | Summary |
|---|---|---|---|---|
| Alimohammadi et al., 2016 [54] | The Effects of Air Pollution on Ischemic Stroke Admission Rate | 379 | PM10, PM2.5, NO2, O3 and SO2 | Air pollution levels correlate with ischemic stroke admission |
| Chiu et al., 2014 [56] | Relationship between hemorrhagic stroke hospitalization and exposure to fine particulate air pollution in Taipei, Taiwan | 2.64 million | PM2.5 | Air temperature influences air pollution and hospital admissions for stroke |
| Xiang et al., 2013 [59] | Estimation of short-term effects of air pollution on stroke hospital admissions in Wuhan, China | 10,663 hospital admissions | NO2 | NO2 levels during the cold season is associated with increase stroke admissions |
| Chen et al., 2014 [60] | Increasing emergency room visits for stroke by elevated levels of fine particulate constituents | 3,362 | nitrate, sulfate, organic carbon and elemental carbon | Each individual constituent associated with hemorrhagic stroke |
| Xu et al., 2013 [61] | Association between ozone exposure and onset of stroke in Allegheny County, Pennsylvania, USA, 1994–2000 | 26,210 | O3 | Same day O3 exposure associated with increase total stroke hospitalization risk |
| Montresor-Lopez et al., 2016 [62] | Short-term exposure to ambient ozone and stroke hospital admission: A case-crossover analysis | 35,413 | O3 | O3 associated with increased stroke hospitalization for African Americans compared to European Americans |
The effects of CO exposure on acute stroke remain unclear and potentially paradoxical. At low concentrations, CO may be neuroprotective, a phenomenon reinforced by experimental and clinical studies.[66] Consistent with these findings, Tian et al., recently reported a negative association between short-term CO exposure and emergency stroke hospitalizations.[67] By contrast, a recent meta-analysis demonstrated increased hospital admissions secondary to CO exposure.[50] Further study is warranted.
Air Pollution and Stroke Mortality
Exposures to PM10, SO2 and NO2 increase the risk of stroke mortality.[68] In 2013, 1.37 million premature mortalities were associated with PM2.5 in China, with 688 thousand of these mortalities attributed to stroke.[69] Air pollution is associated with stroke mortality, however specific subtypes of PM2.5 that are attributable to this burden have yet to be ascertained.
Particle size and chemical constituents of PM may contribute to mortality associated with both ischemic and hemorrhagic strokes.[70] Among the chemical components of PM2.5, Lin et. al demonstrated that exposures to organic carbon, elemental carbon, sulfate, nitrate, and ammonium are significantly associated with stroke mortality.[70] Long-term exposure to PM2.5 was associated with an increased hazard of death up to 5 years after stroke, with trends favoring the ischemic subtype.[71] Residential proximity to a major roadway, a marker for air pollution, is associated with an increase in mortality rate among stroke survivors. The strongest association exists among individuals living within 100 meters from a major roadway.[72] A national multi-city time series study found that a 10 ug/m3 increase in 2-day averaged PM2.5 exposure is associated with a 1.76% increase in stroke incidence as well as an 1.18% increase in all cause mortality. A subset analysis found smoking and alcohol consumption were associated with greater PM2.5 effects.[73] PM<10, SO2 and NO2 exposures are significantly associated with total stroke, ischemic stroke, and hemorrhagic stroke mortalities. Further, individuals with co-morbid cardiac disease have an increased risk of ischemic stroke mortality when exposed to increased NO2 levels (Table 6).[74]
Table 6.
Air Pollution and Stroke Mortality
| Author | Study | N | Air Pollutants | Summary |
|---|---|---|---|---|
| Chen et al., 2013 [68] | Acute effect of ambient air pollution on stroke mortality in the China air pollution and health effects study | ~45 million | PM10, SO2 and NO2 | PM10, SO2 and NO2 increase the risk of stroke mortality |
| Liu et al., 2016 [69] | Estimating adult mortality attributable to PM2.5 exposure in China with assimilated PM2.5 concentrations based on a ground monitoring network | * | PM2.5 | Increases in premature mortalities and stroke |
| Lin et al., 2016 [70] | Differentiating the effects of characteristics of PM pollution on mortality from ischemic and hemorrhagic strokes | 5.5 million | organic carbon, elemental carbon, sulfate, nitrate, and ammonium | Increase in stroke mortality |
| Desikan et al., 2016 [71] | Effect of Exhaust- and Nonexhaust-Related Components of Particulate Matter on Long-Term Survival After Stroke | 357,308 | PM2.5 | increase mortality risk up to 5 years post stroke |
| Wilker et al., 2013 [72] | Residential proximity to high-traffic roadways and post stroke mortality | 1,683 | Roadway proximity | Highway proximity increases mortality rate among stroke survivors |
| Dai et al., 2014 [73] | Associations of fine particulate matter species with mortality in the United States: a multicity time-series analysis | 4,473,519 | PM2.5 | Increased risk of stroke and all-cause mortality |
| Qian et al., 2013 | Epidemiological evidence on association between ambient air pollution and stroke mortality | 13.8 million | PM10, SO2 and NO2 | Transient increases in air pollution associated with total, ischemic and hemorrhagic strokes |
Air pollution and cardiovascular risk factors for stroke
It is proposed that cardiovascular risk factors/mechanisms may play a critical role in the increases in stroke incidences evident on highly polluted days in urban cities. Elevations in daily maximum heart rate, heart block frequency, and atrial fibrillation are associated with O3, NO2 and PM.[75] Premature atrial contractions are also associated with long-term PM2.5 exposure.[76] Short-term exposure (7 days) to PM10 and SO2 is associated with cardioembolic stroke.[77] Qin et al. report that obese (BMI ≥ 30 kg/m2) and overweight individuals (BMI 25–29 kg/m2) may experience enhanced effects of air pollution and increased stroke risk.[78]
Public Policy and Health effects of Air Pollution on Stroke
The Environmental Protection Agency (EPA) sets policy and federal law to protect the American public from the health effects of air pollution. However, levels of air pollution generally found safe by the EPA are associated with increases in the risk of ischemic stroke within hours of exposure.[79] Epidemiological studies concerning the health effects of air pollution have principally focused on large population cities, with studies of rural populations lacking. Communities that meet the EPA’s safe PM2.5 standard still experience increases in overall mortality. Selection and information bias may contribute to gross underestimates of exposure levels.[80] In an effort to minimize the adverse health effects of air pollution, some states have passed smoke-free air laws. An 18.1% reduction in hospitalization due to stroke was seen in Florida due to such legislature.[81] Overall, smoke-free air laws are effective policy tools to reduce the incidence of stroke.
The Confounding effect of Asian Dust
Dust blown from the deserts of China and Mongolia comprise a natural phenomenon known as “Asian Dust.” PM10 is thought to be the primary constituent in Asian dust storms.[82] Storms are associated with increased risk of stroke hospital admissions that persists for two days following dust storms.[83] Asian studies must adjust their analysis for the confounding effect of Asian dust. Accounting for this adjustment, hemorrhagic and ischemic stroke mortality in Japan between the years of 2005 and 2010 were still increased due to same-day spikes in suspended particulate matter.[84]
Effects of Noise and Air Pollution on Stroke
Urban noise pollution potentially confounds the association between air pollution and stroke, however results are still ambiguous. A 2015 study by Hoffmann et al., demonstrated that long-term exposure to PM is associated with an increased risk of stroke, regardless of the subject’s exposure to noise.[85] However, another study that adjusted for these variables found road traffic noise is associated with ischemic stroke, while air pollution is not. Further investigations are needed.[86]
Air Pollution and Carotid Artery Disease
Carotid artery disease is a significant risk factor for stroke and cognitive impairment. In a 2010 report, Kunzli et al. demonstrated that residential proximity to a major roadway is associated with increased carotid intima-media thickness (CIMT).[87] Results from screening over 300,000 residents of New York, New Jersey and Connecticut demonstrated that PM2.5 is an independent risk factor for carotid artery stiffness. When controlled for multiple cardiovascular risk factors, a 10 ug/mg3 increase in PM2.5 was associated with a two-fold increase in carotid artery stiffness.[88] African Americans living near a major roadway show a 6.67% increase in CIMT.[89] A meta-analysis, including 18,590 subjects in 8 studies, found considerable heterogeneity in the amount of CIMT thickness after PM2.5 exposure. However, results suggested a positive correlation with mean values within the range associated with adverse cardiovascular events.[90] Short-term elevations in black carbon exposure, even up to 8 hours prior to clinical assessment, are associated with carotid artery stiffness.[91] The European Study of Cohorts for Air Pollution Effects (ESCAPE) study found positive, but non-significant, associations between PM2.5 (as well as residence proximity to a major roadway) and increased CIMT.[92] A single 5-year prospective cohort study of 509 individuals did not find an association between long term exposure to air pollution and carotid artery atherosclerosis. However, the authors attribute these results to low ambient air pollution in the region of study and small study sample.[93] Air pollution is also linked to intracranial vascular disease. Among seniors, PM2.5 increases resting cerebrovascular resistance and decreases cerebral blood flow velocity.[94]
Prenatal PM2.5 and O3 exposure are associated with carotid artery stiffness[95] and increased CIMT[96], respectively. Further, children living near major roadways exhibit increases in carotid artery stiffness.[97] The Multi-Ethnic Study of Atherosclerosis and Air Pollution reports long-term exposure to PM2.5 is associated with increasing rates of CIMT progression. The authors also report that reductions in ambient air pollution lead to slowed progression of carotid intima-media thickening.[98] Additional risk factors that may contribute to the effects of air pollution related to carotid-intima thickening include age, gender, and ethnicity. Elderly men[99] and those of Chinese ancestry[100] may exhibit greater CIMT when exposed to PM2.5 (Table 7).
Table 7.
Air Pollution and Carotid Artery Disease
| Author | Study | N | Air Pollutants | Summary |
|---|---|---|---|---|
| Kunzli et al., 2010 [87] | Ambient air pollution and the progression of atherosclerosis in adults | 1483 | Road proximity and PM2.5 | Increase in CIMT |
| Newman et al., 2015 [88] | Particulate air pollution and carotid artery stenosis | 307,444 | PM2.5 | An independent risk factor for carotid artery stiffness |
| Wang et al., 2016 [89] | Residential Proximity to Traffic-Related Pollution and Atherosclerosis in 4 Vascular Beds Among African-American Adults: Results From the Jackson Heart Study | 4,800 | Road proximity | African Americans show increase in CIMT |
| Akintoye et al., 2016 [90] | Association between fine particulate matter exposure and subclinical atherosclerosis: A meta-analysis | 11,947 | PM2.5 | CIMT values within range of adverse cardiovascular events |
| Provost et al., 2016 [91] | Short-term fluctuations in personal black carbon exposure are associated with rapid changes in carotid arterial stiffening | 54 | Black carbon | Short term elevations associated with carotid artery stiffness |
| Perez et al., 2015 [92] | Air pollution and atherosclerosis: a cross-sectional analysis of four European cohort studies in the ESCAPE study | 9,183 | Road proximity and PM2.5 | Positive, but non-significant associations with increased CIMT |
| Gan et al., 2014 [93] | Long-term exposure to traffic-related air pollution and progression of carotid artery atherosclerosis: a prospective cohort study | 509 | black carbon, fine particles, nitrogen dioxide and nitric oxide | No association with carotid artery atherosclerosis |
| Breton et al., 2016 [95] | Prenatal Air Pollution Exposure and Early Cardiovascular Phenotypes in Young Adults | 768 | PM2.5 and O3 | Prenatal exposure, increases in carotid artery stiffness |
| Breton et al., 2012 [96] | Childhood air pollutant exposure and carotid artery intima-media thickness in young adults | 861 | PM2.5 and O3 | Prenatal exposure, increases in CIMT |
| Iannuzzi et al., 2010 [97] | Air pollution and carotid arterial stiffness in children | 52 | Road proximity | Increases in carotid artery stiffness |
| Adar et al., 2013 [98] | Fine particulate air pollution and the progression of carotid intima-medial thickness: a prospective cohort study from the multi-ethnic study of atherosclerosis and air pollution | 5,660 | PM2.5 | Reductions slowed CIMT progression |
| Wilker et al., 2013 [99] | Long-term exposure to black carbon and carotid intima-media thickness: the normative aging study | 380 | Black carbon | Increase in CIMT in elderly men |
Conclusion
Air pollution from urban environments affects the central nervous system in a multitude of ways. Exposures impact cognitive function, stroke risk, and carotid artery disease. Pediatric and elderly populations are highly vulnerable due to CNS development and aging processes. Compiling and contextualizing current evidence should provoke thought and future investigations focused on improving health outcomes.
Highlights.
Clinical and epidemiological studies have established adverse effects of air pollution on the central nervous system.
Air pollution is associated with cognitive dysfunction, Alzheimer’s Disease and Parkinson’s disease.
Air pollution is associated with structural brain effects and white matter injury.
Adverse outcomes in stroke and carotid artery disease are associated with air pollution.
This review examines the clinical effects of air pollution on neurological health.
Acknowledgments
Funding
This research was supported by National Institute of Health grant ES024936 to W.J.M.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kilburn KH. Effects of diesel exhaust on neurobehavioral and pulmonary functions. Archives of environmental health. 2000;55:11–7. doi: 10.1080/00039890009603379. [DOI] [PubMed] [Google Scholar]
- 2.Krzyzanowski M, Cohen A. Update of WHO air quality guidelines. Air Quality, Atmosphere & Health. 2008;1:7–13. [Google Scholar]
- 3.Harrison RM, Yin J. Particulate matter in the atmosphere: which particle properties are important for its effects on health? The Science of the total environment. 2000;249:85–101. doi: 10.1016/s0048-9697(99)00513-6. [DOI] [PubMed] [Google Scholar]
- 4.Block ML, Elder A, Auten RL, Bilbo SD, Chen H, Chen JC, et al. The outdoor air pollution and brain health workshop. Neurotoxicology. 2012;33:972–84. doi: 10.1016/j.neuro.2012.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Block ML, Calderon-Garciduenas L. Air pollution: mechanisms of neuroinflammation and CNS disease. Trends Neurosci. 2009;32:506–16. doi: 10.1016/j.tins.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Campbell A, Oldham M, Becaria A, Bondy SC, Meacher D, Sioutas C, et al. Particulate matter in polluted air may increase biomarkers of inflammation in mouse brain. Neurotoxicology. 2005;26:133–40. doi: 10.1016/j.neuro.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 7.Ranft U, Schikowski T, Sugiri D, Krutmann J, Kramer U. Long-term exposure to traffic-related particulate matter impairs cognitive function in the elderly. Environmental research. 2009;109:1004–11. doi: 10.1016/j.envres.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Chen H, Kwong JC, Copes R, Tu K, Villeneuve PJ, van Donkelaar A, et al. Living near major roads and the incidence of dementia, Parkinson’s disease, and multiple sclerosis: a population-based cohort study. The Lancet. doi: 10.1016/S0140-6736(16)32399-6. [DOI] [PubMed] [Google Scholar]
- 9.Power MC, Weisskopf MG, Alexeeff SE, Coull BA, Spiro A, 3rd, Schwartz J. Traffic-related air pollution and cognitive function in a cohort of older men. Environmental health perspectives. 2011;119:682–7. doi: 10.1289/ehp.1002767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wellenius GA, Boyle LD, Coull BA, Milberg WP, Gryparis A, Schwartz J, et al. Residential proximity to nearest major roadway and cognitive function in community-dwelling seniors: results from the MOBILIZE Boston Study. J Am Geriatr Soc. 2012;60:2075–80. doi: 10.1111/j.1532-5415.2012.04195.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang Y, Eliot MN, Koutrakis P, Gryparis A, Schwartz JD, Coull BA, et al. Ambient air pollution and depressive symptoms in older adults: results from the MOBILIZE Boston study. 2014 doi: 10.1289/ehp.1205909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen JC, Schwartz J. Neurobehavioral effects of ambient air pollution on cognitive performance in US adults. Neurotoxicology. 2009;30:231–9. doi: 10.1016/j.neuro.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 13.Ailshire JA, Clarke P. Fine particulate matter air pollution and cognitive function among US older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2015;70:322–8. doi: 10.1093/geronb/gbu064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weuve J, Puett RC, Schwartz J, Yanosky JD, Laden F, Grodstein F. Exposure to particulate air pollution and cognitive decline in older women. Archives of internal medicine. 2012;172:219–27. doi: 10.1001/archinternmed.2011.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oudin A, Forsberg B, Adolfsson AN, Lind N, Modig L, Nordin M, et al. Traffic-Related Air Pollution and Dementia Incidence in Northern Sweden: A Longitudinal Study. Environmental health perspectives. 2016;124:306–12. doi: 10.1289/ehp.1408322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ailshire JA, Crimmins EM. Fine particulate matter air pollution and cognitive function among older US adults. American journal of epidemiology. 2014:kwu155. doi: 10.1093/aje/kwu155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ritz B, Lee PC, Hansen J, Lassen CF, Ketzel M, Sorensen M, et al. Traffic-Related Air Pollution and Parkinson’s Disease in Denmark: A Case-Control Study. Environmental health perspectives. 2016;124:351–6. doi: 10.1289/ehp.1409313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu YC, Lin YC, Yu HL, Chen JH, Chen TF, Sun Y, et al. Association between air pollutants and dementia risk in the elderly. Alzheimers Dement (Amst) 2015;1:220–8. doi: 10.1016/j.dadm.2014.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kioumourtzoglou MA, Schwartz JD, Weisskopf MG, Melly SJ, Wang Y, Dominici F, et al. Long-term PM2.5 Exposure and Neurological Hospital Admissions in the Northeastern United States. Environmental health perspectives. 2016;124:23–9. doi: 10.1289/ehp.1408973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ailshire J, Karraker A, Clarke P. Neighborhood social stressors, fine particulate matter air pollution, and cognitive function among older U.S. adults. Social science & medicine (1982) 2017;172:56–63. doi: 10.1016/j.socscimed.2016.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Calderon-Garciduenas L, Solt AC, Henriquez-Roldan C, Torres-Jardon R, Nuse B, Herritt L, et al. Long-term air pollution exposure is associated with neuroinflammation, an altered innate immune response, disruption of the blood-brain barrier, ultrafine particulate deposition, and accumulation of amyloid beta-42 and alpha-synuclein in children and young adults. Toxicol Pathol. 2008;36:289–310. doi: 10.1177/0192623307313011. [DOI] [PubMed] [Google Scholar]
- 22.Calderon-Garciduenas L, Reed W, Maronpot RR, Henriquez-Roldan C, Delgado-Chavez R, Calderon-Garciduenas A, et al. Brain inflammation and Alzheimer’s-like pathology in individuals exposed to severe air pollution. Toxicol Pathol. 2004;32:650–8. doi: 10.1080/01926230490520232. [DOI] [PubMed] [Google Scholar]
- 23.Uchoa MF, Moser VA, Pike CJ. Interactions between inflammation, sex steroids, and Alzheimer’s disease risk factors. Front Neuroendocrinol. 2016;43:60–82. doi: 10.1016/j.yfrne.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fehsel K, Schikowski T, Janner M, Huls A, Voussoughi M, Schulte T, et al. Estrogen receptor beta polymorphisms and cognitive performance in women: associations and modifications by genetic and environmental influences. J Neural Transm (Vienna) 2016;123:1369–79. doi: 10.1007/s00702-016-1620-8. [DOI] [PubMed] [Google Scholar]
- 25.Huang YC. Outdoor air pollution: a global perspective. Journal of occupational and environmental medicine. 2014;56(Suppl 10):S3–7. doi: 10.1097/JOM.0000000000000240. [DOI] [PubMed] [Google Scholar]
- 26.Bell ML, McDermott A, Zeger SL, Samet JM, Dominici F. Ozone and short-term mortality in 95 US urban communities, 1987–2000. Jama. 2004;292:2372–8. doi: 10.1001/jama.292.19.2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Levy JI, Chemerynski SM, Sarnat JA. Ozone exposure and mortality: an empiric bayes metaregression analysis. Epidemiology (Cambridge, Mass) 2005;16:458–68. doi: 10.1097/01.ede.0000165820.08301.b3. [DOI] [PubMed] [Google Scholar]
- 28.Chan CC, Wu TH. Effects of ambient ozone exposure on mail carriers’ peak expiratory flow rates. Environmental health perspectives. 2005;113:735–8. doi: 10.1289/ehp.7636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Calderon-Garciduenas L, Jewells V, Galaz-Montoya C, van Zundert B, Perez-Calatayud A, Ascencio-Ferrel E, et al. Interactive and additive influences of Gender, BMI and Apolipoprotein 4 on cognition in children chronically exposed to high concentrations of PM2.5 and ozone. APOE 4 females are at highest risk in Mexico City. Environmental research. 2016;150:411–22. doi: 10.1016/j.envres.2016.06.026. [DOI] [PubMed] [Google Scholar]
- 30.Linares C, Culqui D, Carmona R, Ortiz C, Diaz J. Short-term association between environmental factors and hospital admissions due to dementia in Madrid. Environmental research. 2017;152:214–20. doi: 10.1016/j.envres.2016.10.020. [DOI] [PubMed] [Google Scholar]
- 31.Jung CR, Lin YT, Hwang BF. Ozone, particulate matter, and newly diagnosed Alzheimer’s disease: a population-based cohort study in Taiwan. Journal of Alzheimer’s disease : JAD. 2015;44:573–84. doi: 10.3233/JAD-140855. [DOI] [PubMed] [Google Scholar]
- 32.Chang KH, Chang MY, Muo CH, Wu TN, Chen CY, Kao CH. Increased risk of dementia in patients exposed to nitrogen dioxide and carbon monoxide: a population-based retrospective cohort study. PloS one. 2014;9:e103078. doi: 10.1371/journal.pone.0103078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gatto NM, Henderson VW, Hodis HN, St John JA, Lurmann F, Chen JC, et al. Components of air pollution and cognitive function in middle-aged and older adults in Los Angeles. Neurotoxicology. 2014;40:1–7. doi: 10.1016/j.neuro.2013.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Calderon-Garciduenas L, Reynoso-Robles R, Vargas-Martinez J, Gomez-Maqueo-Chew A, Perez-Guille B, Mukherjee PS, et al. Prefrontal white matter pathology in air pollution exposed Mexico City young urbanites and their potential impact on neurovascular unit dysfunction and the development of Alzheimer’s disease. Environmental research. 2016;146:404–17. doi: 10.1016/j.envres.2015.12.031. [DOI] [PubMed] [Google Scholar]
- 35.Calderon-Garciduenas L, Vojdani A, Blaurock-Busch E, Busch Y, Friedle A, Franco-Lira M, et al. Air pollution and children: neural and tight junction antibodies and combustion metals, the role of barrier breakdown and brain immunity in neurodegeneration. Journal of Alzheimer’s disease : JAD. 2015;43:1039–58. doi: 10.3233/JAD-141365. [DOI] [PubMed] [Google Scholar]
- 36.Calderon-Garciduenas L, Franco-Lira M, Torres-Jardon R, Henriquez-Roldan C, Barragan-Mejia G, Valencia-Salazar G, et al. Pediatric respiratory and systemic effects of chronic air pollution exposure: nose, lung, heart, and brain pathology. Toxicol Pathol. 2007;35:154–62. doi: 10.1080/01926230601059985. [DOI] [PubMed] [Google Scholar]
- 37.Calderon-Garciduenas L, Mora-Tiscareno A, Ontiveros E, Gomez-Garza G, Barragan-Mejia G, Broadway J, et al. Air pollution, cognitive deficits and brain abnormalities: a pilot study with children and dogs. Brain and cognition. 2008;68:117–27. doi: 10.1016/j.bandc.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 38.Peng C, Bind MC, Colicino E, Kloog I, Byun HM, Cantone L, et al. Particulate Air Pollution and Fasting Blood Glucose in Nondiabetic Individuals: Associations and Epigenetic Mediation in the Normative Aging Study, 2000–2011. Environmental health perspectives. 2016;124:1715–21. doi: 10.1289/EHP183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Calderon-Garciduenas L, Mora-Tiscareno A, Melo-Sanchez G, Rodriguez-Diaz J, Torres-Jardon R, Styner M, et al. A Critical Proton MR Spectroscopy Marker of Alzheimer’s Disease Early Neurodegenerative Change: Low Hippocampal NAA/Cr Ratio Impacts APOE varepsilon4 Mexico City Children and Their Parents. Journal of Alzheimer’s disease : JAD. 2015;48:1065–75. doi: 10.3233/JAD-150415. [DOI] [PubMed] [Google Scholar]
- 40.Wilker EH, Preis SR, Beiser AS, Wolf PA, Au R, Kloog I, et al. Long-term exposure to fine particulate matter, residential proximity to major roads and measures of brain structure. Stroke. 2015;46:1161–6. doi: 10.1161/STROKEAHA.114.008348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen JC, Wang X, Wellenius GA, Serre ML, Driscoll I, Casanova R, et al. Ambient air pollution and neurotoxicity on brain structure: Evidence from women’s health initiative memory study. Annals of neurology. 2015;78:466–76. doi: 10.1002/ana.24460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Good CD, Johnsrude IS, Ashburner J, Henson RN, Friston KJ, Frackowiak RS. A voxel-based morphometric study of ageing in 465 normal adult human brains. NeuroImage. 2001;14:21–36. doi: 10.1006/nimg.2001.0786. [DOI] [PubMed] [Google Scholar]
- 43.Casanova R, Wang X, Reyes J, Akita Y, Serre ML, Vizuete W, et al. A Voxel-Based Morphometry Study Reveals Local Brain Structural Alterations Associated with Ambient Fine Particles in Older Women. Frontiers in human neuroscience. 2016;10:495. doi: 10.3389/fnhum.2016.00495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Calderon-Garciduenas L, Engle R, Mora-Tiscareno A, Styner M, Gomez-Garza G, Zhu H, et al. Exposure to severe urban air pollution influences cognitive outcomes, brain volume and systemic inflammation in clinically healthy children. Brain and cognition. 2011;77:345–55. doi: 10.1016/j.bandc.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 45.Calderon-Garciduenas L, Mora-Tiscareno A, Franco-Lira M, Zhu H, Lu Z, Solorio E, et al. Decreases in Short Term Memory, IQ, and Altered Brain Metabolic Ratios in Urban Apolipoprotein epsilon4 Children Exposed to Air Pollution. Journal of Alzheimer’s disease : JAD. 2015;45:757–70. doi: 10.3233/JAD-142685. [DOI] [PubMed] [Google Scholar]
- 46.Feigin VL, Roth GA, Naghavi M, Parmar P, Krishnamurthi R, Chugh S, et al. Global burden of stroke and risk factors in 188 countries, during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet Neurology. 2016;15:913–24. doi: 10.1016/S1474-4422(16)30073-4. [DOI] [PubMed] [Google Scholar]
- 47.Liu M, Huang Y, Ma Z, Jin Z, Liu X, Wang H, et al. Spatial and temporal trends in the mortality burden of air pollution in China: 2004–2012. Environment international. 2017;98:75–81. doi: 10.1016/j.envint.2016.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ginsberg GM, Kaliner E, Grotto I. Mortality, hospital days and expenditures attributable to ambient air pollution from particulate matter in Israel. Israel journal of health policy research. 2016;5:51. doi: 10.1186/s13584-016-0110-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Scheers H, Jacobs L, Casas L, Nemery B, Nawrot TS. Long-Term Exposure to Particulate Matter Air Pollution Is a Risk Factor for Stroke: Meta-Analytical Evidence. Stroke. 2015;46:3058–66. doi: 10.1161/STROKEAHA.115.009913. [DOI] [PubMed] [Google Scholar]
- 50.Shah AS, Lee KK, McAllister DA, Hunter A, Nair H, Whiteley W, et al. Short term exposure to air pollution and stroke: systematic review and meta-analysis. BMJ (Clinical research ed) 2015;350:h1295. doi: 10.1136/bmj.h1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang Y, Eliot MN, Wellenius GA. Short-term changes in ambient particulate matter and risk of stroke: a systematic review and meta-analysis. Journal of the American Heart Association. 2014;3 doi: 10.1161/JAHA.114.000983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yang WS, Wang X, Deng Q, Fan WY, Wang WY. An evidence-based appraisal of global association between air pollution and risk of stroke. International journal of cardiology. 2014;175:307–13. doi: 10.1016/j.ijcard.2014.05.044. [DOI] [PubMed] [Google Scholar]
- 53.Stafoggia M, Cesaroni G, Peters A, Andersen ZJ, Badaloni C, Beelen R, et al. Long-term exposure to ambient air pollution and incidence of cerebrovascular events: results from 11 European cohorts within the ESCAPE project. Environmental health perspectives. 2014;122:919–25. doi: 10.1289/ehp.1307301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alimohammadi H, Fakhri S, Derakhshanfar H, Hosseini-Zijoud SM, Safari S, Hatamabadi HR. The Effects of Air Pollution on Ischemic Stroke Admission Rate. Chonnam medical journal. 2016;52:53–8. doi: 10.4068/cmj.2016.52.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lokken RP, Wellenius GA, Coull BA, Burger MR, Schlaug G, Suh HH, et al. Air pollution and risk of stroke: underestimation of effect due to misclassification of time of event onset. Epidemiology (Cambridge, Mass) 2009;20:137. doi: 10.1097/ede.0b013e31818ef34a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chiu HF, Chang CC, Yang CY. Relationship between hemorrhagic stroke hospitalization and exposure to fine particulate air pollution in Taipei, Taiwan. Journal of toxicology and environmental health Part A. 2014;77:1154–63. doi: 10.1080/15287394.2014.926801. [DOI] [PubMed] [Google Scholar]
- 57.Chiu HF, Yang CY. Short-term effects of fine particulate air pollution on ischemic stroke occurrence: a case-crossover study. Journal of toxicology and environmental health Part A. 2013;76:1188–97. doi: 10.1080/15287394.2013.842463. [DOI] [PubMed] [Google Scholar]
- 58.Huang F, Luo Y, Guo Y, Tao L, Xu Q, Wang C, et al. Particulate Matter and Hospital Admissions for Stroke in Beijing, China: Modification Effects by Ambient Temperature. Journal of the American Heart Association. 2016;5 doi: 10.1161/JAHA.116.003437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Xiang H, Mertz KJ, Arena VC, Brink LL, Xu X, Bi Y, et al. Estimation of short-term effects of air pollution on stroke hospital admissions in Wuhan, China. PloS one. 2013;8:e61168. doi: 10.1371/journal.pone.0061168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chen SY, Lin YL, Chang WT, Lee CT, Chan CC. Increasing emergency room visits for stroke by elevated levels of fine particulate constituents. The Science of the total environment. 2014;473–474:446–50. doi: 10.1016/j.scitotenv.2013.12.035. [DOI] [PubMed] [Google Scholar]
- 61.Xu X, Sun Y, Ha S, Talbott EO, Lissaker CT. Association between ozone exposure and onset of stroke in Allegheny County, Pennsylvania, USA, 1994–2000. Neuroepidemiology. 2013;41:2–6. doi: 10.1159/000345138. [DOI] [PubMed] [Google Scholar]
- 62.Montresor-Lopez JA, Yanosky JD, Mittleman MA, Sapkota A, He X, Hibbert JD, et al. Short-term exposure to ambient ozone and stroke hospital admission: A case-crossover analysis. Journal of exposure science & environmental epidemiology. 2016;26:162–6. doi: 10.1038/jes.2015.48. [DOI] [PubMed] [Google Scholar]
- 63.Santurtun A, Ruiz PB, Lopez-Delgado L, Sanchez-Lorenzo A, Riancho J, Zarrabeitia MT. Stroke: Temporal Trends and Association with Atmospheric Variables and Air Pollutants in Northern Spain. Cardiovascular toxicology. 2016 doi: 10.1007/s12012-016-9395-6. [DOI] [PubMed] [Google Scholar]
- 64.Andersen ZJ, Kristiansen LC, Andersen KK, Olsen TS, Hvidberg M, Jensen SS, et al. Stroke and long-term exposure to outdoor air pollution from nitrogen dioxide: a cohort study. Stroke. 2012;43:320–5. doi: 10.1161/STROKEAHA.111.629246. [DOI] [PubMed] [Google Scholar]
- 65.Nascimento LF, Francisco JB, Patto MB, Antunes AM. Environmental pollutants and stroke-related hospital admissions. Cadernos de saude publica. 2012;28:1319–24. doi: 10.1590/s0102-311x2012000700010. [DOI] [PubMed] [Google Scholar]
- 66.Motterlini R, Otterbein LE. The therapeutic potential of carbon monoxide. Nature reviews Drug discovery. 2010;9:728–43. doi: 10.1038/nrd3228. [DOI] [PubMed] [Google Scholar]
- 67.Tian L, Qiu H, Pun VC, Ho KF, Chan CS, Yu IT. Carbon monoxide and stroke: A time series study of ambient air pollution and emergency hospitalizations. International journal of cardiology. 2015;201:4–9. doi: 10.1016/j.ijcard.2015.07.099. [DOI] [PubMed] [Google Scholar]
- 68.Chen R, Zhang Y, Yang C, Zhao Z, Xu X, Kan H. Acute effect of ambient air pollution on stroke mortality in the China air pollution and health effects study. Stroke. 2013;44:954–60. doi: 10.1161/STROKEAHA.111.673442. [DOI] [PubMed] [Google Scholar]
- 69.Liu J, Han Y, Tang X, Zhu J, Zhu T. Estimating adult mortality attributable to PM2.5 exposure in China with assimilated PM2.5 concentrations based on a ground monitoring network. The Science of the total environment. 2016;568:1253–62. doi: 10.1016/j.scitotenv.2016.05.165. [DOI] [PubMed] [Google Scholar]
- 70.Lin H, Tao J, Du Y, Liu T, Qian Z, Tian L, et al. Differentiating the effects of characteristics of PM pollution on mortality from ischemic and hemorrhagic strokes. International journal of hygiene and environmental health. 2016;219:204–11. doi: 10.1016/j.ijheh.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 71.Desikan A, Crichton S, Hoang U, Barratt B, Beevers SD, Kelly FJ, et al. Effect of Exhaust-and Nonexhaust-Related Components of Particulate Matter on Long-Term Survival After Stroke. Stroke. 2016;47:2916–22. doi: 10.1161/STROKEAHA.116.014242. [DOI] [PubMed] [Google Scholar]
- 72.Wilker EH, Mostofsky E, Lue SH, Gold D, Schwartz J, Wellenius GA, et al. Residential proximity to high-traffic roadways and poststroke mortality. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association. 2013;22:e366–72. doi: 10.1016/j.jstrokecerebrovasdis.2013.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dai L, Zanobetti A, Koutrakis P, Schwartz JD. Associations of fine particulate matter species with mortality in the United States: a multicity time-series analysis. Environmental health perspectives. 2014;122:837–42. doi: 10.1289/ehp.1307568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Qian Y, Zhu M, Cai B, Yang Q, Kan H, Song G, et al. Epidemiological evidence on association between ambient air pollution and stroke mortality. Journal of epidemiology and community health. 2013;67:635–40. doi: 10.1136/jech-2012-201096. [DOI] [PubMed] [Google Scholar]
- 75.Cakmak S, Kauri L, Shutt R, Liu L, Green MS, Mulholland M, et al. The association between ambient air quality and cardiac rate and rhythm in ambulatory subjects. Environment international. 2014;73:365–71. doi: 10.1016/j.envint.2014.08.015. [DOI] [PubMed] [Google Scholar]
- 76.O’Neal WT, Soliman EZ, Efird JT, Judd SE, Howard VJ, Howard G, et al. Fine particulate air pollution and premature atrial contractions: The REasons for Geographic And Racial Differences in Stroke study. Journal of exposure science & environmental epidemiology. 2016 doi: 10.1038/jes.2016.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chung JW, Bang OY, Ahn K, Park SS, Park TH, Kim JG, et al. Air Pollution Is Associated With Ischemic Stroke via Cardiogenic Embolism. Stroke. 2017;48:17–23. doi: 10.1161/STROKEAHA.116.015428. [DOI] [PubMed] [Google Scholar]
- 78.Qin XD, Qian Z, Vaughn MG, Trevathan E, Emo B, Paul G, et al. Gender-specific differences of interaction between obesity and air pollution on stroke and cardiovascular diseases in Chinese adults from a high pollution range area: A large population based cross sectional study. The Science of the total environment. 2015;529:243–8. doi: 10.1016/j.scitotenv.2015.05.041. [DOI] [PubMed] [Google Scholar]
- 79.Wellenius GA, Burger MR, Coull BA, Schwartz J, Suh HH, Koutrakis P, et al. Ambient air pollution and the risk of acute ischemic stroke. Archives of internal medicine. 2012;172:229–34. doi: 10.1001/archinternmed.2011.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lee M, Koutrakis P, Coull B, Kloog I, Schwartz J. Acute effect of fine particulate matter on mortality in three Southeastern states from 2007–2011. Journal of exposure science & environmental epidemiology. 2016;26:173–9. doi: 10.1038/jes.2015.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Loomis BR, Juster HR. Association of indoor smoke-free air laws with hospital admissions for acute myocardial infarction and stroke in three states. Journal of environmental and public health. 2012;2012:589018. doi: 10.1155/2012/589018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cheng MT, Lin YC, Chio CP, Wang CF, Kuo CY. Characteristics of aerosols collected in central Taiwan during an Asian dust event in spring 2000. Chemosphere. 2005;61:1439–50. doi: 10.1016/j.chemosphere.2005.04.120. [DOI] [PubMed] [Google Scholar]
- 83.Kang JH, Liu TC, Keller J, Lin HC. Asian dust storm events are associated with an acute increase in stroke hospitalisation. Journal of epidemiology and community health. 2013;67:125–31. doi: 10.1136/jech-2011-200794. [DOI] [PubMed] [Google Scholar]
- 84.Yorifuji T, Kashima S. Associations of particulate matter with stroke mortality: a multicity study in Japan. Journal of occupational and environmental medicine. 2013;55:768–71. doi: 10.1097/JOM.0b013e3182973092. [DOI] [PubMed] [Google Scholar]
- 85.Hoffmann B, Weinmayr G, Hennig F, Fuks K, Moebus S, Weimar C, et al. Air quality, stroke, and coronary events: results of the Heinz Nixdorf Recall Study from the Ruhr Region. Deutsches Arzteblatt international. 2015;112:195–201. doi: 10.3238/arztebl.2015.0195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sorensen M, Luhdorf P, Ketzel M, Andersen ZJ, Tjonneland A, Overvad K, et al. Combined effects of road traffic noise and ambient air pollution in relation to risk for stroke? Environmental research. 2014;133:49–55. doi: 10.1016/j.envres.2014.05.011. [DOI] [PubMed] [Google Scholar]
- 87.Kunzli N, Jerrett M, Garcia-Esteban R, Basagana X, Beckermann B, Gilliland F, et al. Ambient air pollution and the progression of atherosclerosis in adults. PloS one. 2010;5:e9096. doi: 10.1371/journal.pone.0009096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Newman JD, Thurston GD, Cromar K, Guo Y, Rockman CB, Fisher EA, et al. Particulate air pollution and carotid artery stenosis. Journal of the American College of Cardiology. 2015;65:1150–1. doi: 10.1016/j.jacc.2014.12.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wang Y, Wellenius GA, Hickson DA, Gjelsvik A, Eaton CB, Wyatt SB. Residential Proximity to Traffic-Related Pollution and Atherosclerosis in 4 Vascular Beds Among African-American Adults: Results From the Jackson Heart Study. American journal of epidemiology. 2016;184:732–43. doi: 10.1093/aje/kww080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Akintoye E, Shi L, Obaitan I, Olusunmade M, Wang Y, Newman JD, et al. Association between fine particulate matter exposure and subclinical atherosclerosis: A meta-analysis. European journal of preventive cardiology. 2016;23:602–12. doi: 10.1177/2047487315588758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Provost EB, Louwies T, Cox B, Op’t Roodt J, Solmi F, Dons E, et al. Short-term fluctuations in personal black carbon exposure are associated with rapid changes in carotid arterial stiffening. Environment international. 2016;88:228–34. doi: 10.1016/j.envint.2015.12.023. [DOI] [PubMed] [Google Scholar]
- 92.Perez L, Wolf K, Hennig F, Penell J, Basagana X, Foraster M, et al. Air pollution and atherosclerosis: a cross-sectional analysis of four European cohort studies in the ESCAPE study. Environmental health perspectives. 2015;123:597–605. doi: 10.1289/ehp.1307711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gan WQ, Allen RW, Brauer M, Davies HW, Mancini GB, Lear SA. Long-term exposure to traffic-related air pollution and progression of carotid artery atherosclerosis: a prospective cohort study. BMJ open. 2014;4:e004743. doi: 10.1136/bmjopen-2013-004743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wellenius GA, Boyle LD, Wilker EH, Sorond FA, Coull BA, Koutrakis P, et al. Ambient fine particulate matter alters cerebral hemodynamics in the elderly. Stroke. 2013;44:1532–6. doi: 10.1161/STROKEAHA.111.000395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Breton CV, Mack WJ, Yao J, Berhane K, Amadeus M, Lurmann F, et al. Prenatal Air Pollution Exposure and Early Cardiovascular Phenotypes in Young Adults. PloS one. 2016;11:e0150825. doi: 10.1371/journal.pone.0150825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Breton CV, Wang X, Mack WJ, Berhane K, Lopez M, Islam TS, et al. Childhood air pollutant exposure and carotid artery intima-media thickness in young adults. Circulation. 2012;126:1614–20. doi: 10.1161/CIRCULATIONAHA.112.096164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Iannuzzi A, Verga MC, Renis M, Schiavo A, Salvatore V, Santoriello C, et al. Air pollution and carotid arterial stiffness in children. Cardiology in the young. 2010;20:186–90. doi: 10.1017/S1047951109992010. [DOI] [PubMed] [Google Scholar]
- 98.Adar SD, Sheppard L, Vedal S, Polak JF, Sampson PD, Diez Roux AV, et al. Fine particulate air pollution and the progression of carotid intima-medial thickness: a prospective cohort study from the multi-ethnic study of atherosclerosis and air pollution. PLoS medicine. 2013;10:e1001430. doi: 10.1371/journal.pmed.1001430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Wilker EH, Mittleman MA, Coull BA, Gryparis A, Bots ML, Schwartz J, et al. Long-term exposure to black carbon and carotid intima-media thickness: the normative aging study. Environmental health perspectives. 2013;121:1061–7. doi: 10.1289/ehp.1104845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Jones MR, Diez-Roux AV, O’Neill MS, Guallar E, Sharrett AR, Post W, et al. Ambient air pollution and racial/ethnic differences in carotid intima-media thickness in the Multi-Ethnic Study of Atherosclerosis (MESA) Journal of epidemiology and community health. 2015;69:1191–8. doi: 10.1136/jech-2015-205588. [DOI] [PMC free article] [PubMed] [Google Scholar]


