Abstract
A 32-years-old male developed exfoliating skin lesions in bilateral axillae and groins on D-42 post matched sibling allogeneic transplant. These lesions masqueraded betadine burns with a positive history of betadine application in the affected regions. He gradually developed lesions involving other parts of the body with Glucksberg grade-IV acute GVHD (skin-stage: IV/gut-stage: III). He succumbed to his illness. We present this case to highlight the rare initial presentation of skin GVHD involving localized body regions with sparing of rest of the body and mimicking betadine burns.
Keywords: Skin GVHD, Betadine rash, Cutaneous
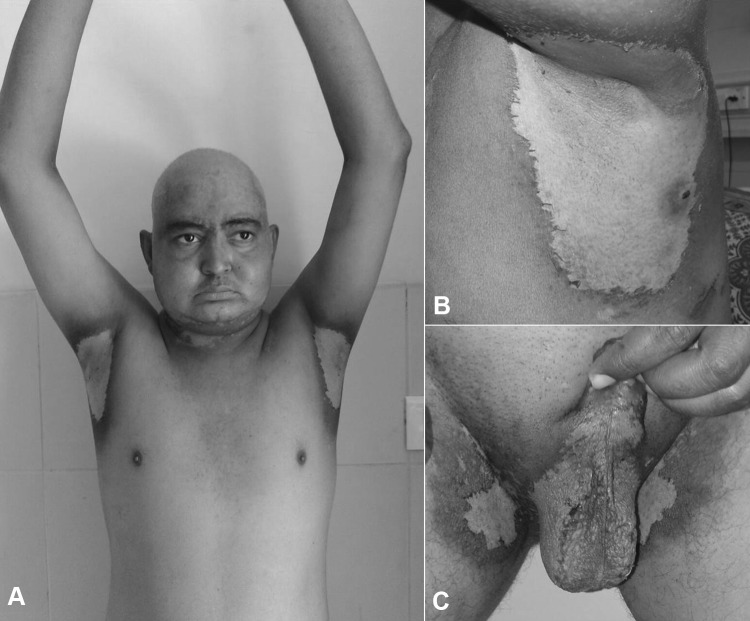
A 32-years-old male with chronic myeloid leukemia blast crisis in molecular remission underwent matched-sibling allogeneic hematopoietic stem cell transplantation (HSCT). He was on cyclosporine-methotrexate for graft versus host disease (GVHD) prophylaxis. He was discharged in an asymptomatic state on D24 post-HSCT. He presented on D42 post-HSCT with depigmented, exfoliated areas in bilateral axillary and inguinal areas including the scrotum (Fig. 1). As part of the post-transplant precautions, the individual was prescribed betadine applications to both axillae/groins and sitz bath with betadine twice daily. He was on GVHD prophylaxis (cyclosporine 150 mg BD with basal CsA levels of 200–300), antibiotic prophylaxis (Co-trimoxazole 2BD twice a week, Fluconazole 200 mg OD and Acyclovir 400 mg BD) and vitamin supplements at the time of development of these symptoms, but he was on these medications for last 6 weeks. Based on the history of betadine application in the affected areas, a possibility of betadine burns or Steven Johnson syndrome was considered. Despite withholding betadine soaks and the suspected implicative drugs, these lesions progressed to the cubital region, perianal region before generalized involvement (40% body surface area) in 2 days (Fig. 2). These skin lesions had nikolksy sign positive, erythroderma, bullae, and extensive epidermal necrosis. Punch biopsy done at presentation was suggestive of GVHD (Fig. 3). He gradually also developed hematuria, breathlessness on exertion with bloody diarrhea. He eventually developed Glucksberg grade-IV acute GVHD (skin-stage: IV/gut-stage: III). He was unsuccessfully treated with high dose steroids, mycophenolate mofetil, and monoclonal antibodies. He succumbed to complications of immunosuppression with thrombotic microangiopathy, septic shock, and ARDS.
Fig. 1.
Clinical photograph on D42 post-HSCT showing well demarcated exfoliated depigmented lesions in the bilateral axilla sparing chest and extremities (a). Lesions have a clear hyperpigmented margin seen in left axilla on a magnified view (b). Similar lesions also noted involving bilateral inguinal regions and scrotum sparing lower extremities or buttocks on D42 (c)
Fig. 2.
Similar skin lesions in the cubital fossa developed on D44 post-HSCT with erythematous base (a) progressed to bullous lesions over the dorsal aspects of hands which have ruptured (b) and skin denudation over the buttocks by D46 (c)
Fig. 3.
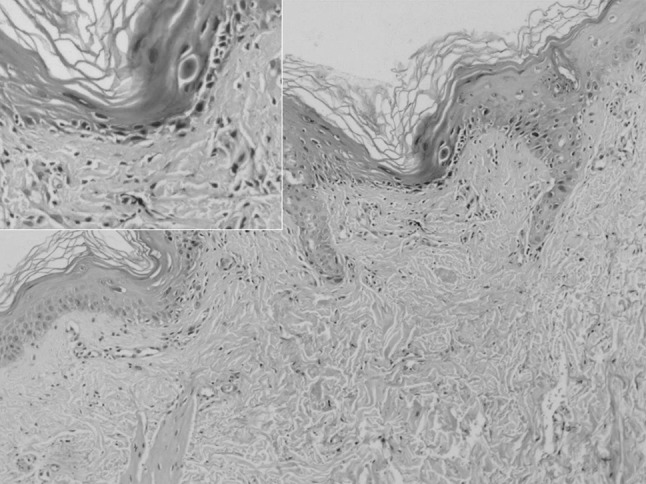
Microphotograph of punch biopsy from the axillary region on D42 depicting histology suggestive of skin GVHD with acanthocytosis, spongiosis and necrotic keratinocytes on Hematoxylin and Eosin staining (×40). Inset highlighting spongiosis and necrotic keratinocytes at higher magnification (×200)
Skin involvement is amongst the earliest manifestation of acute GVHD (<100 days post-HSCT) occurring within 2–4 weeks of HSCT. It usually begins as acral blanchable rash also involving ear, cheeks and back, which later coalesces to form confluent macules [1]. Acute skin GVHD can masquerade any skin disorder with common differentials being drug eruptions, viral exanthems, eruptions of lymphocyte recovery, acral erythema, toxic epidermal necrolysis, Baboon syndrome, zinc deficiency, engraftment syndrome, and radiation dermatitis [2]. In a post-transplant patient, skin GVHD is a potential possibility for any pattern of skin lesions. Cutaneous involvement in acute GVHD can be highly variable and is a harbinger to further systemic involvement of GVHD requiring close follow-up. Skin biopsy in patients with cutaneous involvement in a post-HSCT setting is an absolute necessity to differentiate skin GVHD from closely mimicking other skin disorders. Therapy primary includes high dose steroids and phototherapy in steroid resistant cases. Topical steroids/tacrolimus may help only in grade I skin GVHD [3]. We present this case to highlight the rare initial presentation of skin GVHD involving localized body regions (only bilateral axillae/inguinal regions with sparing of the rest of the body). Also, the morphology of skin lesions (localized exfoliating lesions) mimicking betadine burns is an extremely uncommon presentation for GVHD.
Compliance with Ethical Standards
Conflict of interest
Authors have no conflicts of interest to declare.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
The work is to be attributed at Department of Clinical Haematology and Internal Medicine, P.G.I.M.E.R, Chandigarh, U.T 160012, India.
References
- 1.Peñas PF, Zaman S (2010) Many faces of graft-versus-host disease. Australas J Dermatol 51(1):1–10; quiz 11. doi:10.1111/j.1440-0960.2009.00577.x. Review. PubMed PMID: 20148830 [DOI] [PubMed]
- 2.Mays SR, Kunishige JH, Truong E, Kontoyiannis DP, Hymes SR (2007) Approach to the morbilliform eruption in the hematopoietic transplant patient. Semin Cutan Med Surg 26(3):155–162. Review. PubMed PMID: 18070682 [DOI] [PubMed]
- 3.Abu-Dalle I, Reljic T, Nishihori T, Antar A, Bazarbachi A, Djulbegovic B, Kumar A, Kharfan-Dabaja MA (2014) Extracorporeal photopheresis in steroid-refractory acute or chronic graft-versus-host disease: results of a systematic review of prospective studies. Biol Blood Marrow Transplant. 20(11):1677–1686. PubMed PMID: 24867779 [DOI] [PubMed]