Abstract
Male reproductive issues are frequently overlooked in patients of chronic myeloid leukemia (CML) on imatinib therapy. Current article describes a young man with CML on imatinib mesylate since 13 years who presented to us with painful left sided breast swelling. Mammography and fine needle aspiration cytology confirmed the diagnosis of gynaecomastia and hormone profile revealed low testosterone levels. Gynaecomastia was attributed to imatinib related hypogonadism. Gynaecomastia improved after hormone replacement therapy. Need for long term monitoring of reproductive hormones in patients of CML on imatinib therapy is emphasized in this report.
Keywords: Imatinib, Hypogonadism, Fine needle aspiration, Chronic myeloid leukemia
Male reproductive issues are frequently overlooked in patients of chronic myeloid leukemia (CML) on imatinib therapy. A 45-year-old man presented to our haematology clinic with a 2-month history of painful left breast swelling. He was a known case of Philadelphia positive CML (chronic phase) since 13 years and was on regular imatinib (400 mg once daily) since then. Patient achieved a complete haematological and cytogenetic remission at 3 and 12 months respectively. General examination revealed facial hyperpigmentation that occurred after initiation of imatinib therapy. A tender lump (3 × 3 cm) with ill defined margins was palpable below the left areola (Fig. 1). Examination of abdomen and gonads was unremarkable. His blood investigations were: hemoglobin- 130 g/l, white cell count- 10.4 × 109/l, differential counts- 58% polymorphs, 33% lymphocytes, 4% eosinophils, 4% monocytes and 1% basophils and platelets- 193 × 109/l. Liver and renal function tests were normal. Bcr-abl (by international scale) was undetectable in the peripheral blood by reverse transcriptase polymerase chain reaction. Results of the hormone profile are summarized in Table 1. Sonography of the left breast revealed decreased echogenicity of fibro-glandular stroma with dilated ducts in the retroareolar region. Mammography and fine needle aspiration (FNA) from the lump were consistent with gynaecomastia (Fig. 2). Patient was counseled about gynaecomastia being a possible adverse effect of imatinib therapy. Gynaecomastia improved after 2 months of testosterone replacement therapy. Inhibition of c-kit and platelet derived growth factor receptor in testis by imatinib is responsible for the reproductive adverse effects of Imatinib (due to suppression of testosterone production and leydig cell growth) [1, 2]. In a prospective study comparing reproductive hormone levels before and during Imatinib therapy in patients of CML (n = 38), 18% patients developed gynaecomastia after 5–13 months of therapy. Authors found low total testosterone, low free testosterone, high progesterone and a high 17-OH-progesterone in 92, 73, 49 and 42% patients respectively. Patients with gynaecomastia had a significantly more reduction in free testosterone concentration than those without it. Development of gynaecomastia is dose dependent, being more frequent at higher imatinib doses (600–800 versus 400 mg) [3]. Testosterone deficiency was responsible for gynaecomastia in our case as evidenced by its improvement following hormone replacement. Diurnal variation in pituitary hormone levels could explain normal LH and FSH levels in this case. Development of gynaecomastia after 13 years of imatinib therapy is unusual and emphasizes a need for long-term and comprehensive assessment of reproductive hormones in patients of CML on imatinib therapy. Need for FNA from suspicious breast lumps in patients of CML is also highlighted to rule out granulocytic sarcoma.
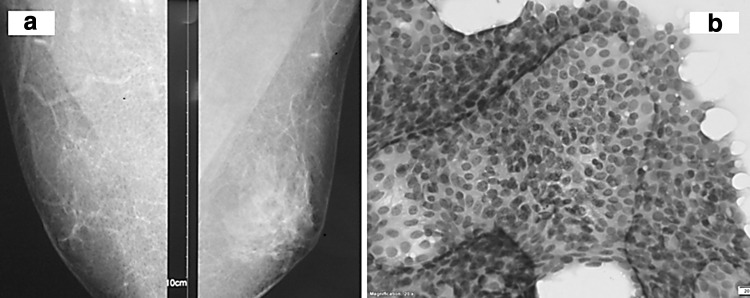
Fig. 1.
Clinical photograph of the patient depicting unilateral (left) breast enlargement. There is no nipple discharge, ulceration or retraction
Table 1.
Table summarizing the complete hormone profile of the patient
| Parameter | Result (normal value) | Parameter | Result (normal value) |
|---|---|---|---|
| TSH | 0.730 µIU/ml (0.27–4.2) | Testosterone basal | 7.08 nmol/L (9.9–27.8) |
| T4 | 7.15 µg/dl (4.8–12.7) | E2-17 basal | 22.34 pg/ml (7.63–42.6) |
| T3 | 1.51 ng/ml (0.8–2) | LH | 4.56 m IU/ml (1.7–8.6) |
| Cortisol 8 AM | 367.7 nmol/L (171–536) | FSH | 3.61 m IU/ml (1.5–12.4) |
| Prolactin | 6.07 ng/ml (4.0–15.2) | 17 OH progesterone | 1.28 ng/ml (0.50–2.10) |
| Growth hormone | 2.3 ng/ml (<5) | DHEAS | 160 µg/dl (48–244) |
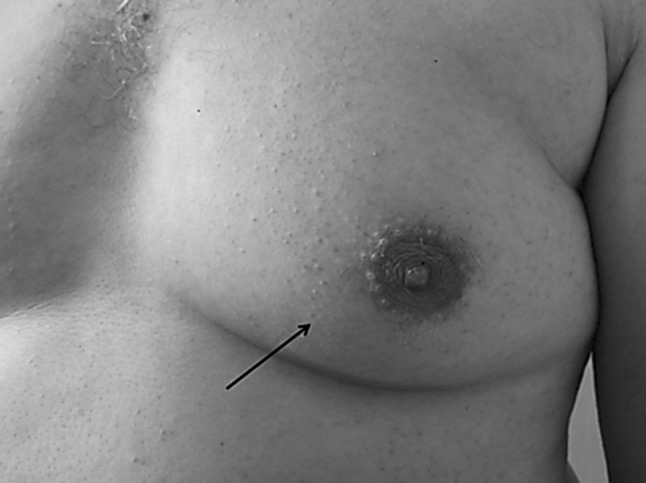
Fig. 2.
a Mammography showing a central dense tissue in retroareolar location radiating into the surrounding fibrofatty tissue without any evidence of calcification or architectural distortion (BIRADS 2). b Fine needle aspiration from the lump showing sheets of benign ductal cells with intermixed myoepithelial cells
Compliance with Ethical Standards
Conflict of interest
Nil.
Informed Consent
Obtained from the patient prior to publication of any material.
Ethical Clearance
The article follows the ethical guidelines as laid under Helsinki’s declaration 1976.
Contributor Information
Ankur Jain, Email: drankur589@yahoo.in.
Subhash Varma, Email: suvarma@hotmail.com.
Rashi Garg, Email: rashiigarg@yahoo.com.
Pankaj Malhotra, Email: hematpgi@gmail.com.
References
- 1.Griffin J. The biology of signal transduction inhibition: basic science to novel therapies. Semin Oncol. 2001;28:3–8. doi: 10.1016/S0093-7754(01)90097-1. [DOI] [PubMed] [Google Scholar]
- 2.Basciani S, Mariani S, Arizzi M, et al. Expression of platelet-derived growth factor-A (PDGF-A), PDGF-B, and PDGF receptor-alpha and -beta during human testicular development and disease. J Clin Endocrinol Metab. 2002;87:2310–2319. doi: 10.1210/jcem.87.5.8476. [DOI] [PubMed] [Google Scholar]
- 3.Gambacorti-Passerini C, Tornaghi L, Cavagnini F, et al. Gynaecomastia in men with chronic myeloid leukaemia after imatinib. Lancet. 2003;361:1954–1956. doi: 10.1016/S0140-6736(03)13554-4. [DOI] [PubMed] [Google Scholar]