Abstract
Purpose
High levels of BCL-2 family members in colorectal carcinoma cause resistance to treatment. Inhibition of NANOG or its paralog NANOGP8 reduces the proliferation, stemness, and tumorigenicity of colorectal carcinoma cells. Our hypothesis was that inhibition of NANOG/NANOGP8 enhances the cytotoxic effect of BH3 mimetics targeting BCL-2 family members in colorectal carcinoma cells through reducing expression of MCL-1, a prosurvival BCL-2 protein.
Experimental Design
Lentiviral vector (LV) shRNA to NANOG (shNG-1) or NANOGP8 (shNp8-1) transduced colorectal carcinoma cells that were also exposed to the BH3 mimetics ABT-737 or ABT-199 in vivo in colorectal carcinoma xenografts and in vitro where proliferation, protein and gene expression, and apoptosis were measured.
Results
Clone A and CX-1 were sensitive to ABT-737 and ABT-199 at IC50s of 2 to 9 μmol/L but LS174T was resistant with IC50s of 18 to 30 μmol/L. Resistance was associated with high MCL-1 expression in LS174T. LVshNG-1 or LVshNp8-1 decreased MCL-1 expression, increased apoptosis, and decreased replating efficiency in colorectal carcinoma cells treated with either ABT-737 or ABT-199 compared with the effects of either BH3 mimetic alone. Inhibition or overexpression of MCL-1 alone replicated the effects of LVshNG-1 or LVshNp8-1 in increasing or decreasing the apoptosis caused with the BH3 mimetic. The combination therapy inhibited the growth of LS174T xenografts in vivo compared with untreated controls or treatment with only LV shRNA or ABT-737.
Conclusions
Inhibition of NANOGP8 or NANOG enhances the cytotoxicity of BH3 mimetics that target BCL-2 family members. Gene therapy targeting the NANOGs may increase the efficacy of BH3 mimetics in colorectal carcinoma.
Introduction
Colorectal carcinoma is the second leading cause of cancer death in the United States without recent improvements in stage-specific death rates. Chemotherapy is used for the adjuvant therapy of stage II and stage III colorectal carcinoma because it causes programmed cell death or apoptosis (1). However, chemotherapy may not kill colorectal carcinoma that expresses high levels of prosurvival BCL2 proteins (2–4). This supports the development of new treatments to overcome the overexpression of these BCL-2 proteins (5, 6).
The BCL-2 family of proteins decides whether a cell continues to live or undergoes death through the intrinsic or mitochondrial apoptotic pathway. Multidomain BCL-2, BCL-xL.MCL-1, BCL-W, and BFL-1 are the prosurvival members of the BCL2 family, whereas BAX, BAK, and BOK are the proapoptotic members (7). Single domain BH3, only members of the family, include PUMA, NOXA, BIM, BID, BAD, and BIK that modulate the actions of the multidomain members (7). Various models explain how the BH3 only proteins affect the function of BCL-2 proteins regulating apoptosis (8, 9). This has led to the development of such BH3 mimetics as ABT-737 and ABT-199 that induce apoptosis in cancer cells. ABT-737 has high affinity to BCL-2, BCL-XL, and BCL-W (10), whereas ABT-199, a second generation BH3 mimetic, is a highly potent and specific inhibitor of BCL-2 (11). ABT-737 has shown good response in killing colorectal carcinoma cell lines as a single agent or in combination with chemotherapy(3, 12), whereas ABT-199 has shown strong activity against chronic lymphocytic leukemia, multiple myelomas, and estrogen receptor-positive breast cancers, either alone or in combination with other drugs. (13–15). However, neither molecule inhibits the other important prosurvival protein MCL-1. Thus, when MCL-1 is highly expressed in cancer cells, ABT-737 has shown activity only when used in combination with molecules which neutralize MCL-1 (3, 9, 16–19). At this point, there seem to be little data on the efficiency of ABT-199 in presence of MCL-1.
NANOG is a key embryonic transcription factor that maintains pluripotency (20, 21) and is located on chromosome 12. NANOGP8 is a retrogene located on chromosome 15 that is expressed in a wide variety of cancers (22–25). Our group showed that inhibition of NANOG and its retrogene NANOGP8 ablates stemness in human colorectal carcinoma as measured by reduced spherogenicity, side population size, proliferation in vitro, and tumorigenicity, and metastatic potential in NOD/SCID mice (26). NANOGP8 may replace NANOG in supporting characteristics of stemness such as proliferation (22) and spherogenicity (26). Moreover, it was recently reported that inhibiting NANOG expression decreases MCL-1 protein levels indirectly through a decrease in the phosphorylation of AKT (27).
We postulated that inhibition of NANOG or NANOGP8 may inhibit MCL-1 expression in colorectal carcinoma and enhance the cytotoxicity of ABT-737 or ABT-199. Our approach was to test this in vivo in mice, in vitro in the WST-1 survival assay as well as to measure the effect of the agents upon caspase-3 and -7 activity as a direct measure of the induction of apoptosis. NANOG and NANOGP8 are essentially identical proteins of 305 amino acids whose coding regions differ by only five nucleotides that create nonsynonymous changes in two amino acids. Our allele specific shRNAs target codon 759 of NANOG (shNG-1) or NANOGP8 (shNp8-1; ref. 26) decreased MCL-1 expression and enhanced the cytotoxicity of the BH3 mimetics in the three colorectal carcinoma cell lines Clone A, CX-1, and LS 174T.
Materials and Methods
ABT-737 and ABT-199 were purchased from Selleck Chemicals LLC. ABT-737 and ABT-199 and stocks in DMSO at 10 mmol/L/L were stored at −20°C. Lipofectamine 2000 for transfections was purchased from Invitrogen. Polybrene and protamine sulfate for Lentivirus transduction and propylene glycol and Tween-80 were purchased from Sigma-Aldrich Chemical Co. Precast NU-PAGE 4–12% Bis Tris gels, NU-PAGE MES SDS Running Buffer, and NU-PAGE transfer buffer were purchased from Invitrogen. Ninety-six–well white plates (ViewPlate-96 TC) for Caspase Glo assay were purchased from PerkinElmer life sciences. Caspase-3 inhibitor (Z-DEVD-FMK) was obtained from R&D systems. MCL-1 overexpression plasmid pTOPO-MCL1 (Plasmid No 21605) was purchased from Addgene.
Cell culture, cell transfection, lentivirus packaging, and cell transduction
Clone A is a subclone of the DLD-1 cell line. (26, 28) CX-1 is a highly metastatic variant of HT29 (28) and LS174T is a colorectal carcinoma cell line obtained from ATCC and used in our previous study (26). The cell lines were authenticated by the University of Arizona Genetics Core, Tuscon, AZ (Supplementary Table S2). All these cell lines were cultured in RPMI (Invitrogen) media supplemented with 10% FBS (Invitrogen) and 2 mmol/L L-glutamine (Invitrogen) at 37°C, 5% CO2 incubator. The Lentivirus particles containing the allele specific shRNAs for NANOG (shNG-1), NANOGP8 (shNp8-1), and negative control (shNEG) were produced by cotransfection of 293T cells with packaging and envelope plasmids using Lipofectamine 2000 (Invitrogen) as described (26). The transduction of the lentiviral particles at an multiplicity of infection of five to eight for all the experiments was done using polybrene or protamine sulfate as the transducing agent.
Tumors
Animal experiments were performed under the protocol LEC-052 approved by the NCI Animal Care and Use Committee. Three million viable untreated LS174T cells or LS174T cells transduced with shNEG, shNG-1, or shNp8-1 were injected subcutaneously into eight groups of 5- to 6-week-old NOD/SCID male mice (Fig. 1). ABT-737 was dissolved in 30% propylene glycol, 5% Tween-80, 3.3% D5W (pH 1.0), and 1% DMSO, sonicated, and pH adjusted to pH 4-5. When tumors reached approximately 100 mm3, ABT-737 (100 mg/kg) was injected intraperitoneally daily for 5 days. Tumor volumes were calculated by the formula perpendicular length × width2. Mice were sacrificed when the control tumor volume reached 2,000 mm3 8 days later. Statistical analysis of the treated tumors relative to control was done using one-way ANOVA with Holm–Sidak multiple comparisons correction test in GraphPad Prism 6.
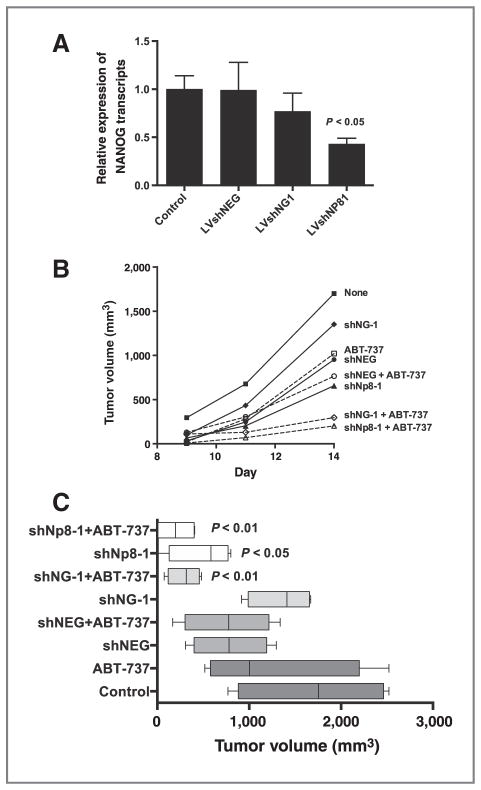
Figure 1.
Antitumor effects of LVNG1/LVNp81-ABT-737 combinations. Three million parental LS174T cells or LS174T cells transduced with LV shNEG, shNG-1, or shNp8-1 were injected subcutaneously into groups of 8 NOD/SCID male mice. At day 8, ABT-737 (100 mg/mL) was injected daily intraperitoneally for 5 days. A, three mice from each group were sacrificed on the 8th day before ABT-737 treatment, tumors collected, and qRT-PCR performed to determine the relative expression of total transcripts of the NANOGs. Mean ± SD of the expression of the NANOGs normalized by GAPDH. B, mean growth curves of each group of mice. C, box and whisker plots for each group of mice with mean and 5%–95% confidence intervals are presented by the error bars. The P values were determined by one-way ANOVA and compared with the control (untreated) group.
Assays
WST-1 (Roche) and Caspase-Glo were used according to the directions supplied by the manufacturers. For the clonogenic or regrowth assay, the three cell lines were seeded with 10,000 cells in a 48-well plate (Costar/Corning) in RPMI-1640 media with supplements. After 16 hours, cells were treated with lentiviral vector (LV) shNEG, LVshNG-1, and LVshNp8-1 or ABT-737 alone for 8 days or with one of the three shRNAs for 5 days followed by ABT-737 (2 μmol/L) for 3 more days. The supernatant was removed from the wells after 8 days and remaining adherent cells were trypsinized and an equal number of cells as described in the text were plated in 60 mmol/L dishes with complete RPMI media, in duplicates for each treatment. The cells were incubated for 14 days and fixed and stained with 0.05% Crystal violet in 10% neutral-buffered formalin (37% vol), methanol (1%), and 0.15 mol/L PBS (62% vol). The plates were washed with water and the colonies counted. For assessment of caspase function, caspase-3 inhibitor (Z-DEVD-FMK) was added 4 hours after adding LV and ABT-737 at 10 μmol/L and then the cultures were analyzed by WST-1 assay as explained above.
Western blot analysis
Colorectal carcinoma cells were washed with PBS and then solubilized with RIPA buffer containing both protease and phosphatase inhibitors. Pre-cast NU-PAGE 4% to 12% gels were used to separate cell lysates. Lysates transferred to Nitrocellulose membranes were probed with rabbit anti-MCL-1 (Cell Signaling Technology, Cat# 4572, Cat#sc819), BCL-2 (Cat#2876), BCL-XL (Cat#2762), NANOG(Cat#4903), AKT (Cat#9272), AKT-Ser473 (Cat#4060), BCL-W(Cat#2724), and BIM (Cat#2819), and β-actin (Cat#4967) to monitor changes in the level of these proteins. The primary antibodywas detected with goat anti-rabbit-HRP (Jackson Immunoresearch).
Statistical analysis
ANOVA was performed for statistical analysis of multiple comparisons using GraphPad Prism 6. Data in graphs are presented as mean ± SD except where indicated in the text. For the analyses, P < 0.05 was considered to be statistically significant. All experiments were repeated at least twice independently.
Results
Combination treatment of ABT-737 and LVshNG-1/LVshNp8-1 in mice bearing LS174T xenografts
To test the combination of ABT-737 with LVshNG1 and LVshNp81 in vivo, we injected NOD/SCID male mice with 3 × 106 LS174T cells transduced with LV shNG-1 or shNp8-1 or the control shNEG or left untreated. The ABT-737 treatment was started at day 8 when the tumors were approximately 100 mm3. The mice were sacrificed at day 17 when the tumors of the control groups of mice reached around 2,000 mm3. When tumors were analyzed at day 8 before the start of ABT-737 treatment, the levels of total NANOG transcripts in tumors initiated with LV shNG-1 or LV shNp8-1 were two-thirds or one-half, respectively, of the transcript levels in the control tumors (Fig. 1A). The volume of tumors of mice treated with the single agents of LV shNEG, LV shNG1, LV shNp8-1, or ABT-737 or the control combination of LV shNEG + ABT-737 was not significantly reduced compared with the size of the untreated controls (Fig. 1B and C). However, the mean volume of tumors in mice treated with combined LV shNG1 + BT-737 (P <; 0.01) or LV shNp81 + ABT-737 (P <; 0.01) was one-third that of the mean of the untreated controls (Fig. 1C). These results support the postulate that inhibition of NANOG/NANOGP8 enhances the efficacy of ABT-737 in colorectal carcinoma xenografts. Further studies were performed in vitro to elucidate mechanism.
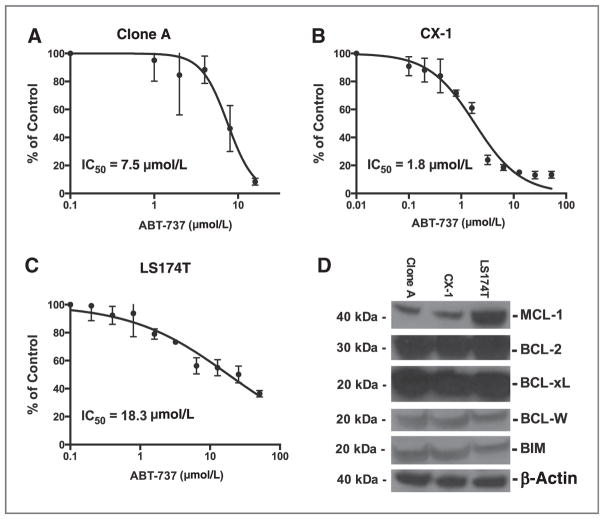
Colorectal cancer cell lines are variably sensitive to ABT-737
We began these studies by determining the IC50 of ABT-737 on three cell lines (Clone A, CX-1, and LS174T). IC50 values were 7.5 μmol/L for Clone A cells, 1.8 μmol/L for CX-1, and high 18.3 μmol/L for LS174T cells in a 48-hour viability treatment (Fig. 2A–C). The protein levels of the prosurvival proteins BCL-2 (BCL2), BCL-xL (BCL2L1), MCL-1 (MCL1), (BCL-W BCL2L2), and BIM (BCL2L11) were also analyzed (Fig. 2D). LS174T cells express nearly three times the amount of MCL-1 as Clone A and CX-1, but the other prosurvival Bcl-2 family proteins are expressed similarly by the three cell lines (Fig. 2D).
Figure 2.
Dose response of colorectal carcinoma cell lines to the BH3 mimetic ABT-737. A–C, Clone A, CX-1, or LS174T cells were treated with ABT-737 (0.2 –60 μmol/L) for 72 hours. Cell survival was determined using the WST-1 reagent. The viability of cells (% of control) is presented as % absorbance of treated cells at 450 nm/% absorbance of untreated cells at 450 nm expressed as a percentage of the untreated parental cells. IC50swere calculated with GraphPad Prism 6 using the nonlinear regression subprogram. D, immunoblot analysis for detection of MCL-1, BCL-2, BCl-xL, BCL-W, and BIM levels in Clone A, CX-1 and LS174T.
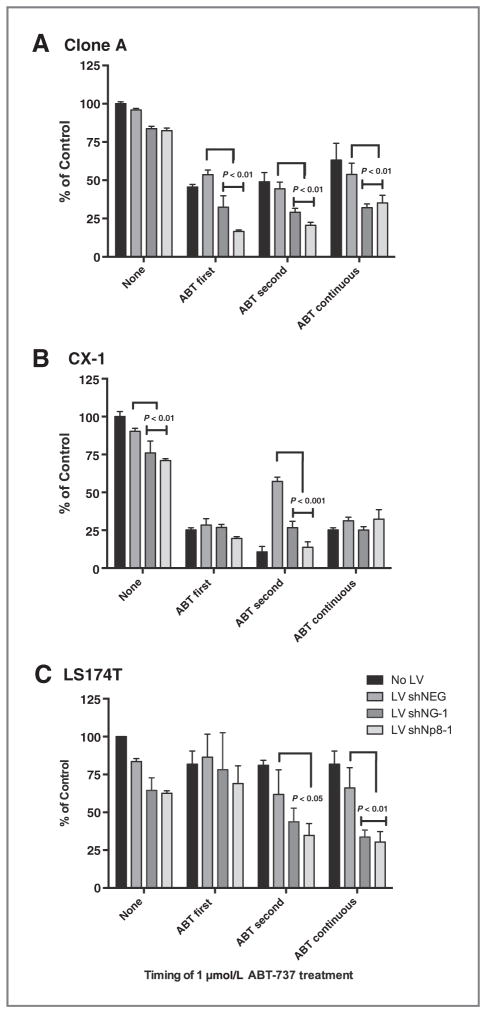
Enhanced killing via combinations of ABT-737 and LVshNG-1 and LVshNp8-1 in colorectal carcinoma cell lines
Prior studies have demonstrated that inhibition of NANOG decreases cell proliferation, causes cell-cycle arrest, induces apoptosis, and inhibits stemness in a variety of cancer cell lines (26, 29). Conditional knockout of NANOG in mice induces apoptotic cell death in murine migrating primordial germ cells (30). We tested the combination of ABT-737 with LV shRNAs in these colorectal carcinoma cell lines at a concentration of 1 μmol/L ABT-737. This concentration of ABT-737 by itself produced little or no cytotoxicity in Clone A, CX-1, and LS174T (Fig. 3). The combination experiment was done to test also the timing of ABT-737 and shRNA on the response of colorectal carcinoma cells to the combination where colorectal carcinoma cells were exposed ABT-737 (1 μmol/L) for at least 3 days with exposure to LV shRNA for at least 5 days (Fig. 3). In “ABT First” experiments, cells were treated first with ABT-737 (1 μmol/L) for 3 days followed by treatment with LV shRNAs (LV shNEG, LV shNG-1, and LV shNp8-1) for 5 days. In “ABT Second” studies, the three cell lines were treated with LV shRNAs for 5 days first followed by treatment with ABT-737 (1 μmol/L) for 3 days. “ABT Continuous” studies represent the cell lines treated with ABT-737 and LV shRNAs simultaneously for 8 days. All combination treatments lasted 8 days. Cell survival was determined by metabolism of WST-1 and results presented as the mean ±SD of the% of control values of the untreated colorectal carcinoma cells after 8 days: fewer cells are associated with a lower amount of WST-1 metabolized (Fig. 3). In Clone A, the combination treatment (LV shNp8-1 + ABT-737) decreased cell survival by as much as by 40% relative to the lentiviral treatment control (LV shNEG1 + ABT-737) in all the combination therapy groups (Fig. 3A), and LS174T cells had a similar decrease in survival relative to the lentiviral control shNEG but only when the cells were transduced with lentiviral shRNA first or concurrently with ABT-737 addition (Fig. 3C). Interestingly, the CX-1 cells were only inhibited when the lentiviral shRNA was transduced first (Fig. 3B). Because CX-1 is sensitive to ABT-737, the BH3 mimetic effect may mask the potential effect from inhibiting NANOG and/or NANOGP8. As a result, a dose–response experiment with ABT-737 was performed with CX-1 cells treated with LV shNp8-1. The combination enhances the growth inhibition of CX-1 cells by reducing the IC50 of 2.8 μmol/L for ABT-737 alone by more than 50% to 1.31 μmol/L for the combination (Supplementary Fig. S1, P < 0.0001). Also in each cell line, shNp8-1 transduction was more active than shNG-1 in inhibiting growth (Fig. 3A–C).
Figure 3.
ABT-737 and LV shRNA combination therapy increases inhibition of colorectal carcinoma growth. Five thousand colorectal carcinoma cells were cultured in monolayer culture in individual wells of a 96-well microtiter plate in complete medium and LV shRNA or ABT-737 or both added as indicated for a total of 8 days. Cells were treated with either LV shRNA for 5 days or 1 μmol/L ABT-737 for 3 days or with both from the beginning of the culture. The “None” cells did not receive any ABT-737, whereas the “ABT First,” “ABT Second,” or “ABT Continuous” represent cells exposed to ABT-737 First and then LV, or “ABT Second” with cells exposed to LV shRNA first for 5 days and then ABT-737 for 3 days or “ABT Continuous” where both agents were added at the beginning of the 8 day culture. Results are presented as means with SD. P values are the significance of the indicated LV shNG-1 and/or shNp8-1 compared with the LV shNEG in the same treatment group determined by two-way ANOVA. Where there is a horizontal cupped bracket spanning across shNG-1 and shNp8-1, the P value of each compared with the corresponding shNEG control is the indicated value.
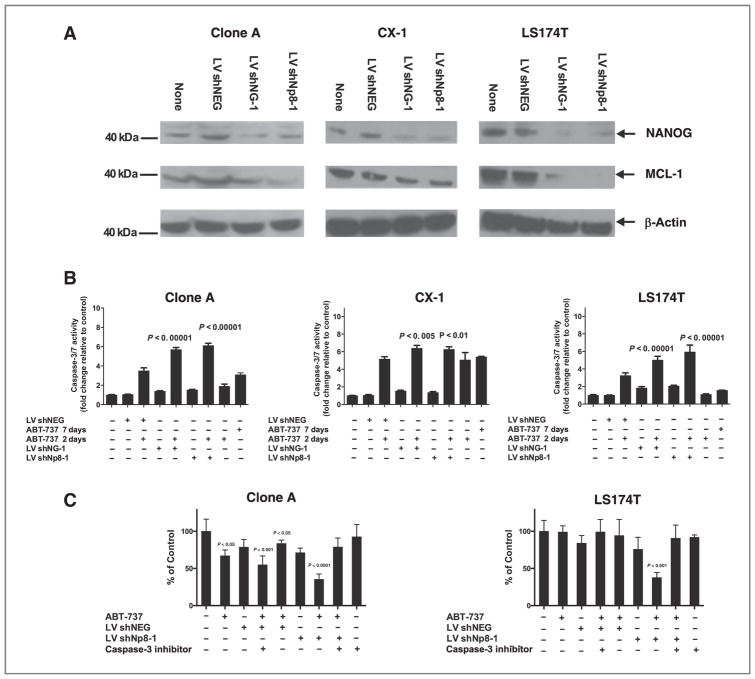
Killing of cells is associated with loss of MCL-1 and increase in caspase-3/7 activity
Inhibition of NANOG in cancer cell lines has been associated with loss of AKT phosphorylation and a decrease in MCL-1 levels (27). To elucidate whether enhanced killing associated with combination of LV shRNA against NANOG or NANOGP8 and ABT-737 is associated with loss of AKT phosphorylation and decrease in MCL-1 levels due to inhibition of NANOG, we treated the three colorectal carcinoma cell lines with the LV-delivered shRNA. The inhibition of either NANOG or NANOGP8 in Clone A cells resulted in a decrease in the levels of NANOG, phosphorylation of AKT at Ser-473, and in MCL-1 (Supplementary Fig. S2). Inhibition of NANOG and NANOGP8 gene expression by shRNA did not decrease relative MCL-1 transcript levels (Supplementary Fig. S2A and S2B) but did decrease MCL-1 protein expression by at least 50% in all three colorectal carcinoma cell lines, whereas treatment with the control LVshNEG did not (Fig. 4A). Caspase-3/7 activity was induced in Clone A, CX-1, and LS174T cell lines when colorectal carcinoma cells were cultured with 1 μmol/L ABT-737 after first being pretreated with LV shRNAs (Fig. 4B). Transduction with LV shNEG, LV shNG-1, or LV shNp8-1 alone did not increase caspase-3/7 activity (Fig. 4B), whereas ABT-737 alone increased caspase-3/7 activity significantly in CX-1 cells and to a lesser extent in Clone A treated for 7 days (Fig. 4B). The combination of LV shNEG and ABT-737 increased caspase-3/7 activity moderately 2- to 4-fold in the three cell lines (Fig. 4B). However, in all three cell lines, the combination treatment with LV shNG-1 or LV shNp8-1 increased caspase-3/7 activity by 5.5- to 7.5-fold compared with untreated cells and more than that caused by LV shNEG and ABT-737 (Fig. 4B). Inhibition of colorectal carcinoma growth induced by the combination therapy of shRNA and ABT-737 is associated with apoptosis as reflected by the activity of the executioner caspases. The inhibition of cell survival by combination therapy is caused by caspase-dependent cell death because addition of a caspase-3 inhibitor peptide blocked the cytotoxic effect of LV shNp8-1 and ABT-737 (Fig. 4C).
Figure 4.
LV shRNA to Nanog or NanogP8 inhibits MCL-1 and increases caspase-3/7 activity. A, Clone A, CX-1, or LS174T cells were treated with the indicated LV shRNA for 5 days in monolayer culture or left untreated. Lysates were blotted and probed for NANOG and MCL-1 protein expression. B, the three cell lines were treated with LV shRNA alone for 7 days or LVshRNA for 5 days followed by ABT-737 (1 μmol/L) for 2 days in triplicate in complete medium. Caspase-3/7 activity was determined in the wells using the Promega caspase-3/7–Glo kit according to the manufacturer’s protocol. The results are mean ± SD of the activity normalized to the untreated control cells within each experiment. P values are the significance of the indicated caspase-3/7 fold increase in LV shNG-1 + ABT-737(1 μmol/L) and shNp8-1 + ABT-737 (1 μmol/L) compared with the LV shNEG + ABT-737(1 μmol/L) for each cell line determined by one-way ANOVA with the Holm-Sidak multiple comparisons test. C, Clone A or LS174T cells were cultured in complete medium for 16 hours and then treated with LV shNEG or shNp8-1, ABT-737 (2 μmol/L), or the combination. Four hours later, 10 μmol/L caspase-3 inhibitor (Z-DEVD-FMK) was added. Cell viability was determined 5 days later. Results are presented as the mean ± SD normalized to the untreated control cells. P values are determined by one-way ANOVA with means compared with the untreated cells with the Holm–Sidak multiple comparisons test.
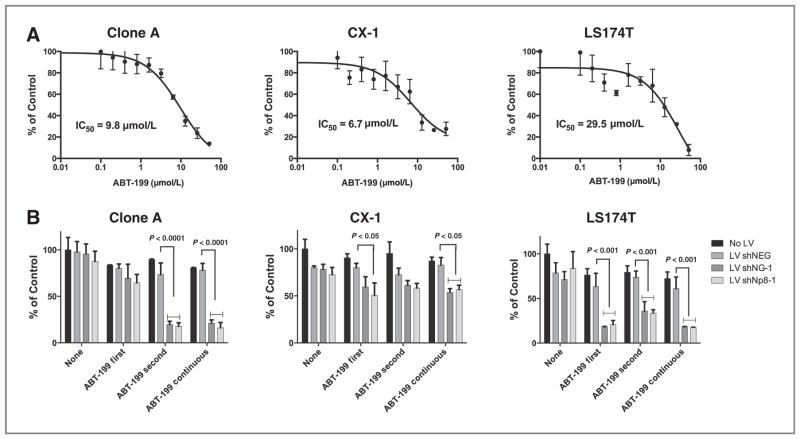
ABT-199 and its activity in colorectal carcinoma cell lines
The IC50s for Clone A, CX-1, and LS174T treated with ABT-199 are 9.8 μmol/L, 6.7 μmol/L, and 29.5 μmol/L, respectively (Fig. 5A). Clone A showed similar sensitivity to ABT-737 and ABT-199 (Supplementary Table S1). In contrast, CX-1 and LS174T were more sensitive to ABT-737 than ABT-199 (Supplementary Table S1). These patterns of differing sensitivity have also been observed in other cancer cell lines (14). To test the activity of ABT-199 in combination with LV shNG-1 or shNp8-1 in these three colorectal carcinoma cell lines, the combination treatment was done in a similar manner as explained for ABT-737 above (Fig. 5B). The concentration of ABT-199 used for this experiment was 2 μmol/L. In Clone A and LS174T cells, the combination treatment (LV shNp8-1 + ABT-199) resulted in the inhibition of cell growth by as much as 60% relative to LV control (LV shNEG + ABT-199; Fig. 5B). CX-1 survival was inhibited by 30% when treated with the combination (LV shNp8-1 + ABT-199) relative to control (LV shNEG + ABT-199). Inhibition of BCL-2 alone by a low concentration of ABT-199 enhances the inhibition of Clone A and LS 174T cells treated with LV shNG-1 or LV shNP8-1, especially if the ABT-199 is given after or continuously with the LV shRNA (Fig. 5B).
Figure 5.
Activity of ABT-199 in colorectal carcinoma cells alone or in combination with shRNA against Nanog and NanogP8. A, Clone A, CX-1, and LS174T cells were treated with ABT-199 for 72 hours and viability determined with IC50calculated for each cell line as described in Fig. 2. B, five thousand colorectal carcinoma cells were cultured in complete medium and LV or ABT-199 or both added as indicated for a total of 8 days. The scheme of the experiment was the same as described for Fig. 3. Results are mean ± SD normalized to the untreated colorectal carcinoma cells. P values are the significance of the indicated LV shNG-1 and/or shNp8-1 compared with the LV shNEG in the same treatment group as determined by two-way ANOVA with the Holm–Sidak multiple comparisons test.
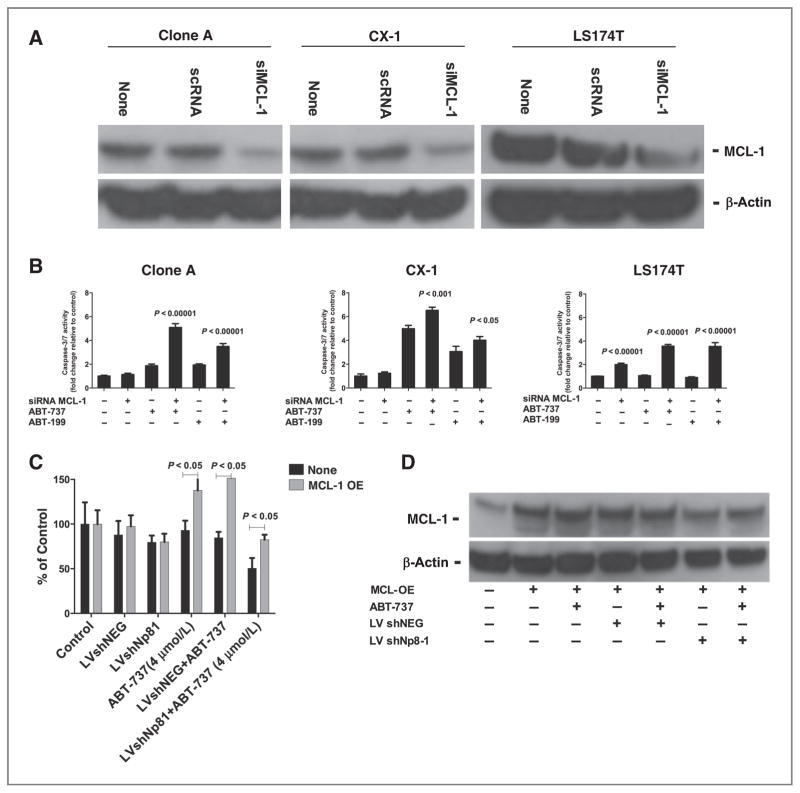
Inhibition of MCL-1 by siRNA increases caspase-3/7 activity in colorectal carcinoma cell lines when used in combination with ABT-737/ABT-199
We tested whether the effect of inhibiting NANOG/NANOGP8 on augmenting the cytotoxicity of the BH3 mimetics depended on the reduction of MCL-1 protein expression by directly modulating the expression of MCL-1 and assessing sensitivity to the BH3 mimetics. Colorectal carcinoma cells were transfected with siRNA MCL-1 (100 nmol/L) alone or in combination with ABT-737/ABT-199 treatment. Transfection of the three colorectal carcinoma cell lines decreased MCL-1 by 3- to 6-fold (Fig. 6A). Transfection of LS174T cells with only siRNA to MCL-1 increased 2-fold the caspase-3/7 activity, whereas such transfection did not increase caspase-3/7 activity in Clone A or CX-1 (Fig. 6B). Treatment with ABT-737 induced caspase-3/7 activity similar to what occurred earlier with inhibition of NANOG/NANOGP8 (Fig. 6B). ABT-199 alone induced caspase-3/7 activity that was similar to ABT-737 in Clone A and LS174T cells (Fig. 5B). In CX-1 cells, ABT-737 induced more Caspase 3/7 activity than ABT-199 alone (Fig. 6). The combination of siRNA to MCL-1 with either BH3 peptide further increased caspase-3/7 activity in each cell line (Fig. 6B). In contrast, overexpression of MCL-1 in LS174T cells rescued the growth of LS174T treated with the combination of LVshNp8-1 + ABT-737 (Fig. 6C) while increasing the level of MCL-1 protein in all cells transfected with the MCL-1 (Fig. 6D). Thus, direct modulation of MCL-1 expression mimics the effects of inhibition of NANOG/NANOGP8 on BH3 mimetics on caspase activity and survival.
Figure 6.
Inhibition of Mcl-1 expression is similar to the effect of LV shNG-1 or shNp8-1 on caspase-3/7 activity when combined with BH3 mimetics. A, Clone A, CX-1, or LS174T cells were transfected with siRNA to Mcl-1 (siMCL-1, 100 nmol/L) or scrambled RNA (scRNA, 100 nmol/L) and lysed and immunoblotted for MCL-1 and β-actin after 72 hours. B, the three cell lines were transfected with siRNA Mcl-1 (100 nmol/L) and 3 days later ABT-737 (2 μmol/L) or ABT-199 (2 μmol/L) was added as indicated. Caspase-3/7 activity was measured at a total of 5 days by Promegaspase 3/7 –Glo kit according to the manufacturer’s protocol. The results are presented as mean ± SD of the activity normalized to the untreated control cells within each experiment. P values were determined by one-way ANOVA with Holm–Sidak multiple comparisons correction test. C, five thousand LS174T cells were seeded in individual wells of a 96-well plate in triplicate and next day treated with LVshNEG and LVshNP81. After 3 days, p-TOPO-MCL-1 was transfected using Lipofectamine. After 48 hours, 4 μmol/L ABT-737 was added and cell viability was measured 3 days later by WST-1 metabolism. The viability of cells is represented as mean ± SD of the% absorbance of cells at 450 nmol/L compared with the controls. P values were calculated by one-way ANOVA. D, lysates of the combinations of ABT-737 and LV shRNAs on the MCL-1 and β-actin protein expression in LS174T cells treated as in C were probed and demonstrate that MCL-1 is overexpressed in all of the p-TOPO MCL-1–transfected cells.
Clonogenic regrowth assay
The ability of lentiviral shRNA combined with ABT-737 to induce a long lasting inhibition of growth in the three colorectal carcinoma cell lines was determined by a colony-forming assay (ref. 31; Supplementary Fig. S3). Colorectal carcinoma cells were treated with ABT-737, LV shRNA, or the combination for 8 days and surviving adherent cells were collected and replated in fresh complete medium. In each experiment, 500 viable cells were plated for each condition and then after 14 days stained and colonies counted. The combination of LV shNp8-1 and ABT-737 significantly decreased regrowth colony efficiency compared with the combination of ABT-737 and LVshNEG1 by 50% and 80% (Supplementary Fig. S3). The combination of ABT-737 and LV shNG-1 had a lesser effect. These data suggest that even those cells that survive to the end of original incubation period have a residual persistent growth inhibition from the combination therapy.
Discussion
The inhibition of MCL-1 achieved through inhibition of NANOGP8 or NANOG increases the growth inhibitory effects of the BH3 mimetics ABT-737 and ABT-199. ABT-737 has potent activity against leukemia and lymphoma cancer cell lines as a single agent and is also effective against multiple myeloma, glioma, and small cell lung cancers (SCLC; ref. 32). In colorectal carcinoma cell lines, ABT-737 has shown poor efficacy as a single agent but the growth inhibition increases when ABT-737 is used in combination with other therapies (3, 5, 6, 12). In this study, the colorectal carcinoma cell lines exhibited low to moderate sensitivity when treated with ABT-737 or ABT-199 as single agents with CX-1 being the most sensitive cell line (Supplementary Table S1). LS174T cell line exhibited the greatest resistance (IC50 > 12 μmol/L; Supplementary Table S1) toward both ABT-737 and ABT-199 associated with the higher expression of MCL-1. Our study demonstrates that the treatment of three colorectal carcinoma cell lines with the combination of LVshNG-1 or LVshNp8-1 and BH3 mimetics enhances the growth inhibitory effect in these cell lines. Earlier studies have also demonstrated that when SCLC cell lines are treated with a combination of ABT-737 and agents which decrease MCL-1 levels, ABT-737-resistant SCLC cell lines demonstrate enhanced killing compared with ABT-737-sensitive SCLC cell lines which show only moderate increase in cell killing when treated with the combination. (16).
Furthermore, we also show that the inhibition of NANOG/NANOGP8 alone decreases the levels of MCL-1 protein. Our finding extends the study of Noh and colleagues (27) who demonstrated that NANOG promotes a stem-like and immune-resistant phenotype in multiple types of cancer cell lines, including the HCT-116 colorectal carcinoma cell line. They elucidated that NANOG acts through TCL1A-mediated AKT regulation of MCL-1 with knockdown of NANOG decreasing the levels of pAKT and MCL-1. Although Boyer and colleagues (33) demonstrated that NANOG binds to the MCL-1 promoter, we have confirmed that inhibition of NANOG or NANOGP8 does not change the levels of MCL-1 transcripts (Supplementary Fig. S2A and S2B). However, inhibition of the NANOGs decreases pAKT (Supplementary Fig. S2C) and MCL-1 expression (Fig. 4A). These results suggest that regulation of MCL-1 is a posttranslational event. Moreover, when we treated the three colorectal carcinoma cell lines with the combination of LV shNG-1 or LV shNp8-1 and ABT-737, it increased the caspase-3/7 activity. Caspase-3 inhibition blocked the enhanced growth inhibitory effect of the combination (Fig. 4C). We also demonstrate that the combination of siRNA MCL-1 and ABT-737/ABT-199 increased the caspase-3/7 activity in these colorectal carcinoma cell lines, whereas overexpression of MCL-1 neutralized the growth inhibitory effect of the shRNA-ABT combination (Fig. 6C). These findings further strengthen the findingthat enhancedcaspase-3/7 orgrowth inhibitory effect by combination of LVshNG-1/shNp8-1 and ABT-737/ABT-199 is the consequence of decrease in the levels of MCL-1. Thus, the combination of inhibition of NANOG/NANOGP8 and the BH3 mimetic combination increased caspase-dependent apoptosis.
ABT-199 combined with LVshNG-1 and/or LVshNp8-1 treatment was approximately 20% more active than the combination with ABT-737 in Clone A and LS174T. Recent studies (11, 14, 15) also support this finding that ABT-199 is more potent than ABT-737 when used alone or in combination with other drugs. Furthermore, the combination of LV shRNA to NANOG or NANOGP8 with ABT-199 reveals that the two agents administered together at the start of the experiment are more potent than when the treatments are administered sequentially (Fig. 5). These findings suggest that the combination of inhibition of the NANOGs could be administered on the same day in the clinic rather than on separate days. This would simplify preclinical testing of this combination. The proof of the principle was validated in vivo with the demonstration that transduction of a colorectal carcinoma xenograft with either LVshNG-1 or shNp8-1 enhanced systemic therapy with a BH3 mimetic (Fig. 1).
The clonogenic regrowth experiment performed in this study demonstrates that treating the colorectal carcinoma cell lines with ABT-737 alone (in Clone A and LS174T cells) or the combination of LVshNG-1 or LVshNp8-1 and ABT-737 (in all 3 cell lines) decreased the ability of the treated cells to regrow when replated in complete culture media. This experiment indicates that the colorectal carcinoma cells treated with these agents have reduced capacity to form colonies (clonogenicity) in normal media. Clonogenicity is associated with the stem cell nature of colorectal carcinoma (34), and the decrease in clonogenicity has been used as an indicator of a decrease in stem cell nature or self-renewal potential of different cancers (35–37). Inhibition of NANOG or NANOGP8 decreases the proliferation and self-renewal capacity of colorectal carcinoma and other cancers (26, 29, 38). Inhibition of antiapoptotic BCL-2 family members by other BH3 inhibitors, ABT-263 and sabutoclax, selectively killed stem cells in leukemias (39, 40). Taken together these findings suggest that the combination of shRNA against NANOG or NANOG P8 and BH3 mimetics may target cancer stem cells and decrease the self-renewal capacity of these colorectal carcinoma cell lines.
In summary, inhibition of NANOG and NANOGP8 by gene therapy combined with a BH3 mimetic may provide a rationale for new therapy regimen for colorectal cancers and target the stem cell properties of colorectal cancer cells, which may be essential in treatment and prevention of relapse of this resistant cancer.
Supplementary Material
Translational Relevance.
Colorectal carcinoma is the second leading cause of cancer death in the United States with recurrence occurring in 30% to 50% of stage II and stage III colorectal carcinoma patients after surgery and adjuvant therapy that is resistant to chemotherapy. Inhibition of the stem cell transcription factor NANOG or its retrogene NANOGP8 decreases stemness and proliferation in colorectal carcinoma. Because high levels of BCL2 family proteins are expressed in colorectal carcinoma, we hypothesized that inhibition of NANOG/NANOGP8 will decrease the levels of prosurvival protein MCL-1 to enhance cytotoxicity of BH3 mimetics that target BCL2 proteins. Combining shRNA against NANOG/NANOGP8 with BH3 mimetics decreased MCL-1, increased caspase-dependent apoptosis of colorectal carcinoma in vitro, and inhibited colorectal carcinoma xenograft growth in vivo more than treatment with BH3 mimetics alone. Inhibition of NANOG/NANOGP8 may reduce the addiction of colorectal carcinoma to MCL-1 and enhance the effect of BH3 mimetics.
Acknowledgments
The authors thank Dr. Snorri Thorgeirsson for helpful comments about improving the manuscript, the valuable advice and support of Drs. Elizabeth Conner and Valentina Factor as well as the outstanding support of the Geneva Foundation, Tacoma, WA, the support provided by the Center for Cancer Research of the NCI for Project ZIA BC 011199, and by the Department of Defense for Grant Number W81XWH-11-1-0327.
Footnotes
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Disclaimer
The opinions expressed in this article are those of the authors and do not necessarily represent those of the National Cancer Institute, the NIH, the Department of Health and Human Services, or the Department of the Army.
Authors’ Contributions
Conception and design: A.R. Mattoo, J. Zhang, J.M. Jessup
Development of methodology: J. Zhang, L.A. Espinoza
Acquisition of data (provided animals, acquired and managed patients, provided facilities, etc.): A.R. Mattoo, L.A. Espinoza, J.M. Jessup
Analysis and interpretation of data (e.g., statistical analysis, biostatistics, computational analysis): A.R. Mattoo, J. Zhang, L.A. Espinoza, J.M. Jessup
Writing, review, and/or revision of the manuscript: A.R. Mattoo, J.M. Jessup
Study supervision: J.M. Jessup
References
- 1.Kaufmann SH, Earnshaw WC. Induction of apoptosis by cancer chemotherapy. Exp Cell Res. 2000;256:42–9. doi: 10.1006/excr.2000.4838. [DOI] [PubMed] [Google Scholar]
- 2.Hayward RL, Macpherson JS, Cummings J, Monia BP, Smyth JF, Jodrell DI. Antisense Bcl-xl down-regulation switches the response to topoisomerase I inhibition from senescence to apoptosis in colorectal cancer cells, enhancing global cytotoxicity. Clin Cancer Res. 2003;9:2856–65. [PubMed] [Google Scholar]
- 3.Okumura K, Huang S, Sinicrope FA. Induction of Noxa sensitizes human colorectal cancer cells expressing Mcl-1 to the small-molecule Bcl-2/Bcl-xL inhibitor, ABT-737. Clin Cancer Res. 2008;14:8132–42. doi: 10.1158/1078-0432.CCR-08-1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Violette S, Poulain L, Dussaulx E, Pepin D, Faussat AM, Chambaz J, et al. Resistance of colon cancer cells to long-term 5-fluorouracil exposure is correlated to the relative level of Bcl-2 and Bcl-X(L) in addition to Bax and p53 status. Int J Cancer. 2002;98:498–504. doi: 10.1002/ijc.10146. [DOI] [PubMed] [Google Scholar]
- 5.Schulze-Bergkamen H, Ehrenberg R, Hickmann L, Vick B, Urbanik T, Schimanski CC, et al. Bcl-x(L) and Myeloid cell leukaemia-1 contribute to apoptosis resistance of colorectal cancer cells. World J Gastro. 2008;14:3829–40. doi: 10.3748/wjg.14.3829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peddaboina C, Jupiter D, Fletcher S, Yap JL, Rai A, Tobin RP, et al. The downregulation of Mcl-1 via USP9X inhibition sensitizes solid tumors to Bcl-xl inhibition. BMC Cancer. 2012;12:541. doi: 10.1186/1471-2407-12-541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Youle RJ, Strasser A. The BCL-2 protein family: opposing activities that mediate cell death. Nat Rev Mol Cell Biol. 2008;9:47–59. doi: 10.1038/nrm2308. [DOI] [PubMed] [Google Scholar]
- 8.Chen L, Willis SN, Wei A, Smith BJ, Fletcher JI, Hinds MG, et al. Differential targeting of prosurvival Bcl-2 proteins by their BH3-only ligands allows complementary apoptotic function. Mol Cell. 2005;17:393–403. doi: 10.1016/j.molcel.2004.12.030. [DOI] [PubMed] [Google Scholar]
- 9.Certo M, Del Gaizo Moore V, Nishino M, Wei G, Korsmeyer S, Arm-strong SA, et al. Mitochondria primed by death signals determine cellular addiction to antiapoptotic BCL-2 family members. Cancer Cell. 2006;9:351–65. doi: 10.1016/j.ccr.2006.03.027. [DOI] [PubMed] [Google Scholar]
- 10.Tahir SK, Yang X, Anderson MG, Morgan-Lappe SE, Sarthy AV, Chen J, et al. Influence of Bcl-2 family members on the cellular response of small-cell lung cancer cell lines to ABT-737. Cancer Res. 2007;67:1176–83. doi: 10.1158/0008-5472.CAN-06-2203. [DOI] [PubMed] [Google Scholar]
- 11.Souers AJ, Leverson JD, Boghaert ER, Ackler SL, Catron ND, Chen J, et al. ABT-199, a potent and selective BCL-2 inhibitor, achieves antitumor activity while sparing platelets. Nature Med. 2013;19:202–8. doi: 10.1038/nm.3048. [DOI] [PubMed] [Google Scholar]
- 12.Raats DA, de Bruijn MT, Steller EJ, Emmink BL, Borel-Rinkes IH, Kranenburg O. Synergistic killing of colorectal cancer cells by oxali-platin and ABT-737. Cell Oncol (Dordr) 2011;34:307–13. doi: 10.1007/s13402-011-0026-8. [DOI] [PubMed] [Google Scholar]
- 13.Davids MS, Letai A, Brown JR. Overcoming stroma-mediated treatment resistance in chronic lymphocytic leukemia through BCL-2 inhibition. Leuk Lymp. 2013;54:1823–5. doi: 10.3109/10428194.2013.796051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Touzeau C, Dousset C, Le Gouill S, Sampath D, Leverson JD, Souers AJ, et al. The Bcl-2 specific BH3 mimetic ABT-199: a promising targeted therapy for t(11;14) multiple myeloma. Leukemia. 2014;28:210–2. doi: 10.1038/leu.2013.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vaillant F, Merino D, Lee L, Breslin K, Pal B, Ritchie ME, et al. Targeting BCL-2 with the BH3 mimetic ABT-199 in estrogen receptor-positive breast cancer. Cancer Cell. 2013;24:120–9. doi: 10.1016/j.ccr.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Mattoo AR, FitzGerald DJ. Combination treatments with ABT-263 and an immunotoxin produce synergistic killing of ABT-263-resistant small cell lung cancer cell lines. Int J Cancer. 2013;132:978–87. doi: 10.1002/ijc.27732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xu H, Krystal GW. Actinomycin D decreases Mcl-1 expression and acts synergistically with ABT-737 against small cell lung cancer cell lines. Clin Cancer Res. 2010;16:4392–400. doi: 10.1158/1078-0432.CCR-10-0640. [DOI] [PubMed] [Google Scholar]
- 18.Brunelle JK, Ryan J, Yecies D, Opferman JT, Letai A. MCL-1-dependent leukemia cells are more sensitive to chemotherapy than BCL-2-dependent counterparts. J Cell Biol. 2009;187:429–42. doi: 10.1083/jcb.200904049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Letai A. Restoring cancer’s death sentence. Cancer cell. 2006;10:343–5. doi: 10.1016/j.ccr.2006.10.014. [DOI] [PubMed] [Google Scholar]
- 20.Chambers I, Colby D, Robertson M, Nichols J, Lee S, Tweedie S, et al. Functional expression cloning of Nanog, a pluripotency sustaining factor in embryonic stem cells. Cell. 2003;113:643–55. doi: 10.1016/s0092-8674(03)00392-1. [DOI] [PubMed] [Google Scholar]
- 21.Mitsui K, Tokuzawa Y, Itoh H, Segawa K, Murakami M, Takahashi K, et al. The homeoprotein Nanog is required for maintenance of plur-ipotency in mouse epiblast and ES cells. Cell. 2003;113:631–42. doi: 10.1016/s0092-8674(03)00393-3. [DOI] [PubMed] [Google Scholar]
- 22.Jeter CR, Badeaux M, Choy G, Chandra D, Patrawala L, Liu C, et al. Functional evidence that the self-renewal gene NANOG regulates human tumor development. Stem Cells. 2009;27:993–1005. doi: 10.1002/stem.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jeter CR, Liu B, Liu X, Chen X, Liu C, Calhoun-Davis T, et al. NANOG promotes cancer stem cell characteristics and prostate cancer resistance to androgen deprivation. Oncogene. 2011;30:3833–45. doi: 10.1038/onc.2011.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Palla AR, Piazzolla D, Abad M, Li H, Dominguez O, Schonthaler HB, et al. Reprogramming activity of NANOGP8, a NANOG family member widely expressed in cancer. Oncogene. 2014;33:2513–9. doi: 10.1038/onc.2013.196. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 25.Zbinden M, Duquet A, Lorente-Trigos A, Ngwabyt SN, Borges I, Ruiz i Altaba A. NANOG regulates glioma stem cells and is essential in vivo acting in a cross-functional network with GLI1 and p53. EMBO J. 2010;29:2659–74. doi: 10.1038/emboj.2010.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang J, Espinoza LA, Kinders RJ, Lawrence SM, Pfister TD, Zhou M, et al. NANOG modulates stemness in human colorectal cancer. Oncogene. 2013;32:4397–405. doi: 10.1038/onc.2012.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Noh KH, Kim BW, Song KH, Cho H, Lee YH, Kim JH, et al. Nanog signaling in cancer promotes stem-like phenotype and immune evasion. J Clin Invest. 2012;122:4077–93. doi: 10.1172/JCI64057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Samara RN, Laguinge LM, Jessup JM. Carcinoembryonic antigen inhibits anoikis in colorectal carcinoma cells by interfering with TRAIL-R2 (DR5) signaling. Cancer Res. 2007;67:4774–82. doi: 10.1158/0008-5472.CAN-06-4315. [DOI] [PubMed] [Google Scholar]
- 29.Cao J, Li L, Chen C, Lv C, Meng F, Zeng L, et al. RNA interference-mediated silencing of NANOG leads to reduced proliferation and self-renewal, cell cycle arrest and apoptosis in T-cell acute lymphoblastic leukemia cells via the p53 signaling pathway. Leukemia Res. 2013;37:1174–7. doi: 10.1016/j.leukres.2013.04.021. [DOI] [PubMed] [Google Scholar]
- 30.Yamaguchi S, Kurimoto K, Yabuta Y, Sasaki H, Nakatsuji N, Saitou M, et al. Conditional knockdown of Nanog induces apoptotic cell death in mouse migrating primordial germ cells. Development. 2009;136:4011–20. doi: 10.1242/dev.041160. [DOI] [PubMed] [Google Scholar]
- 31.Munshi A, Hobbs M, Meyn RE. Clonogenic cell survival assay. Methods Mol Med. 2005;110:21–8. doi: 10.1385/1-59259-869-2:021. [DOI] [PubMed] [Google Scholar]
- 32.Ni Chonghaile T, Letai A. Mimicking the BH3 domain to kill cancer cells. Oncogene. 2008;27:S149–57. doi: 10.1038/onc.2009.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boyer LA, Lee TI, Cole MF, Johnstone SE, Levine SS, Zucker JP, et al. Core transcriptional regulatory circuitry in human embryonic stem cells. Cell. 2005;122:941–56. doi: 10.1016/j.cell.2005.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yeung TM, Gandhi SC, Wilding JL, Muschel R, Bodmer WF. Cancer stem cells from colorectal cancer-derived cell lines. Proc Natl Acad Sci. 2010;107:3722–7. doi: 10.1073/pnas.0915135107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ma Y, Liang D, Liu J, Wen JG, Servoll E, Waaler G, et al. SHBG is an important factor in stemness induction of cells by DHT in vitro and associated with poor clinical features of prostate carcinomas. PloS ONE. 2013;8:e70558. doi: 10.1371/journal.pone.0070558. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 36.Zhang Z, Zhou Y, Qian H, Shao G, Lu X, Chen Q, et al. Stemness and inducing differentiation of small cell lung cancer NCI-H446 cells. Cell Death Dis. 2013;4:e633. doi: 10.1038/cddis.2013.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fedr R, Pernicova Z, Slabakova E, Strakova N, Bouchal J, Grepl M, et al. Automatic cell cloning assay for determining the clonogenic capacity of cancer and cancer stem-like cells. Cytometry A. 2013;83:472–82. doi: 10.1002/cyto.a.22273. [DOI] [PubMed] [Google Scholar]
- 38.Ibrahim EE, Babaei-Jadidi R, Saadeddin A, Spencer-Dene B, Hossaini S, Abuzinadah M, et al. Embryonic NANOG activity defines colorectal cancer stem cells and modulates through AP1- and TCF-dependent mechanisms. Stem Cells. 2012;30:2076–87. doi: 10.1002/stem.1182. [DOI] [PubMed] [Google Scholar]
- 39.Goff DJ, Recart AC, Sadarangani A, Chun HJ, Barrett CL, Krajewska M, et al. A Pan-BCL2 inhibitor renders bone-marrow-resident human leukemia stem cells sensitive to tyrosine kinase inhibition. Cell Stem Cell. 2013;12:316–28. doi: 10.1016/j.stem.2012.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lagadinou ED, Sach A, Callahan K, Rossi RM, Neering SJ, Minhajuddin M, et al. BCL-2 inhibition targets oxidative phosphorylation and selectively eradicates quiescent human leukemia stem cells. Cell Stem Cell. 2013;12:329–41. doi: 10.1016/j.stem.2012.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.