In low- and middle-income countries (LMIC), the rapidly growing end-stage renal disease (ESRD) burden overwhelms limited capacity for renal replacement therapy (RRT).(1) Nearly 1.5 million persons with ESRD living in LMIC are estimated to die annually because they cannot receive RRT.(2,3) While hemodialysis (HD) is the modality-of-choice for the vast majority of patients on dialysis, investment in peritoneal dialysis (PD) can potentially expand capacity for RRT for many emerging economies with nascent ESRD populations. As compared with HD, PD requires less technological support, electricity, and medical staff; thus it can be scaled up more efficiently as the need for RRT grows. Further, PD can better reach patients living in remote, rural regions.(4)
Using a survey administered to nephrologists, and to patients on PD and HD in Dhaka, we explored barriers to wider use of PD in Bangladesh. In particular we probed four barriers commonly conceived to be unique to LMIC, i.e., costs, staff training, patients’ living situation, and concern for peritonitis.
Methods
We developed two surveys, one for practitioners in Dhaka and one for patients on dialysis. After obtaining Institutional Review Board approval from National Institute of Kidney Disease and Urology (NIKDU), we surveyed nephrologists and patients from 6 hospitals in Dhaka, using convenience sampling but ensuring a 50-50 mix of public-private funding. We validated both questionnaires by administering to a sub-sample (10 participants), with open-ended questions about available options and clarity of questions; we used their feedback to refine the questionnaire before reaching out to the larger group of practitioners. We used t-test or Chi-square to compare differences in patients on PD and HD, and in providers with patients both on PD and HD versus those with patients on HD only. We present results of responses to questions with fewer than 10% missingness.
Results
Nephrologists
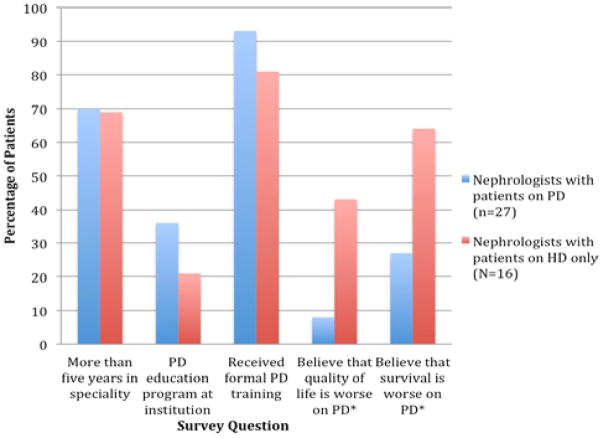
A total of 43 nephrologists responded to the survey. Of these, 27 nephrologists (63%) provided care for patients on PD; 16 (37%) only provided care for patients on HD. Nearly 70% of nephrologists had been practicing for more than five years. While >80% reported receiving formal training in PD, an institutional PD education program was uncommon and when present, associated with a higher frequency of nephrologists managing patients on PD (Figure 1).
Figure 1. Nephrologist training in and beliefs about PD.
Nephrologists with patients on PD (blue bar) are more likely to have been exposed to a PD education program or have received formal training in PD as compared to nephrologists with patients on HD only (red bar). Additionally, nephrologists with patients on PD are also less likely to believe that PD is associated with worse quality of life or survival than those with no patients on PD. Abbreviations: PD-peritoneal dialysis; HD-hemodialysis; * indicates p value <0.0
Patients
A total of 157 patients responded to the survey. Of these, 41 patients (26%) were on PD and 116 patients (74%) were on HD. Both groups had similar overall health status (as represented by the number of hospitalizations in the past year) and level of education attainment, but counter-intuitively patients on PD were more likely to have disabilities that would affect ability to care for themselves (Table 1). Living conditions of patients receiving PD were more capable of supporting home-based care (Table 2). Notably, 98% of patients on PD versus 68% of patients on HD were expected to fully pay for dialysis care.
Table 1.
Characteristics of patients on PD versus HD.
| Patient characteristics | Percentage of patients on PD (n=41) | Percentage of patients on HD (N=116) |
|---|---|---|
| Never educated or less than primary school education | 20 | 23 |
| No caregiver support | 10 | 16 |
| Significant visual impairment | 34 | 4* |
| Impaired dexterity | 28 | 9 |
| Requires assistance with dressing self | 28 | 9* |
| More than one hospitalization in the past year | 44 | 43 |
Patients on PD and HD had similar rates of education attainment and hospitalizations in the past year. Patients on PD were more likely to have disabilities that would affect ability to care for themselves but had higher presence of caregiver support.
Indicates p value < 0.05
Table 2.
Living conditions of patients receiving dialysis care.
| Living conditions | Patients on PD (%) N=41 | Patients on HD (%) N=116 |
|---|---|---|
| Home | ||
| Standalone brick house | 34* | 24 |
| Flat or apartment | 59 | 49 |
| Semi-permanent material | 7 | 27 |
| Electricity | 100 | 98 |
| Single, unshared room | 7 | 19 |
| Water supply | ||
| Family-only tank | 93* | 70 |
| Shared tap | 3 | 26 |
| Shared well | 5 | 5 |
Patients receiving PD more robust living conditions as compared to those of patients receiving HD. They were also more likely to have a private, family-owned, water supply.
Indicates p value < 0.05
Nephrologists’ perceived barriers to PD expansion
Nephrologists caring for patients on PD and those only caring for patients HD were asked which barriers to PD expansion in Bangladesh they consider to be most significant, and both groups reported the same top five barriers (Table 3). The cost of PD supplies was identified as the number one barrier by a wide margin.
Table 3.
Rank list of Nephrologist-identified barriers to PD expansion in Bangladesh.
| 1. Cost of supplies |
| 2. Lack of trained nurses |
| 3. Poor patient hygiene |
| 4. Lack of trained doctors |
| 5. Lack of caregiver support |
There were no substantial differences between responses from nephrologists who have patients on PD and nephrologists who do not
The cost of PD supplies was cited as the number one barrier to PD expansion by both nephrologists with patients on PD and nephrologists with patients only on HD.
DISCUSSION
Extreme poverty complicates the ability of LMIC to address the ESRD crisis. In Bangladesh, all of the centers than offer RRT are located in large cities, completely inaccessible to patients living in rural and geographically remote areas. Even for urban residents, access to ESRD care is limited. There are many potential advantages to greater uptake of PD in this setting including better access to care for patients in remote areas and the convenience of home-based care.(5) As our survey confirms cost of supplies is the main the concern. Importing dialysate fluid is expensive; the government charges 5% as an advanced income tax and 4% advanced trade value added tax.(6) Lowering the import tax on dialysate and other PD materials would substantially lower cost of PD treatment. Thailand, Malaysia, and Nepal charge little to no import tax.(7) Reduced import taxes also incentivize greater competition amongst manufacturers.
Another strategy is to implement a national PD-first program in which patients are prescribed PD by default and receive HD only if they do not qualify for PD. Such a program has been successfully implemented in Thailand and Hong Kong; in fact, Hong Kong now has the highest rate of PD utilization in the world.(7) Countries that have adopted a PD-first strategy for ESRD management report improved patient satisfaction and survival.(8)
We also identified lack of well-trained personnel as a reason for lower uptake of PD. Only 120 nephrologists practice in Bangladesh, and a majority of these physicians are located in Dhaka.(9) However, training programs have been increasing capacity to meet the growing need; as of 2013, there were 28 nephrologists in training.(9) Nurses are the cornerstones of PD therapy but their scarcity is stark in Bangladesh, where only 15,000 are actively working.(10)
Interestingly, we found that while patients on PD in Bangladesh have better living conditions than those on HD, they also tend to require more assistance with care. This means that a supportive family structure is enabling home dialysis, and could potentially be an as-yet underutilized advantage in a low-resource setting (in comparison with HICs where lack of caregiver support is often cited as a reason for avoiding PD). Finally concern for peritonitis and patient personal hygiene was also consistently cited as a reason for underuse of PD. However findings from the Brazilian Peritoneal Dialysis (Braz-PD) Study report peritonitis rates in a low-resource setting that were in line with rates reported from HICs.(11,12) Further the Braz-PD study found that lower education level, but not family income, predicted higher risk for peritonitis. Thus culturally-appropriate patient training may mitigate these risks. Education can also benefit providers, since we found that an ongoing institutional education program about PD was associated with higher provider reliance on PD.
In summary, while expansion of the PD program has the potential to tremendously increase access to RRT in Bangladesh, uptake has slow and sparse. Our study underscores that barriers to greater uptake of PD differ from those faced in HICs, with the high cost of supplies and shortages of trained personnel being the most prominent factors, and patient disability or lack of caregiver support not posing major challenges. We also find that creating institutional PD programs may empower nephrologists’ use of PD. Thoughtful and concerted governmental and clinical action could therefore enable wider use of PD in Bangladesh.
Acknowledgments
Dipal Savla’s work is supported by the Arnhold Institute for Global Health Research Fellowship Dr. Anand’s work was supported by NIDDK 5K23DK101826.
References
- 1.Wetmore JB, Collins AJ. Global challenges posed by the growth of end-stage renal disease. Ren Replace Ther [Internet] Renal Replacement Therapy. 2016 Dec 23;2(1):15. Available from: http://www.rrtjournal.com/content/2/1/15. [Google Scholar]
- 2.Anand S, Bitton A, Gaziano T. The Gap between Estimated Incidence of End-Stage Renal Disease and Use of Therapy. PLoS One. 2013;8(8) doi: 10.1371/journal.pone.0072860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rashid HU. Management of End Stage Renal Disease-Bangladesh Perspective. Open Urol Nephrol J. 2014;7(1) [Google Scholar]
- 4.Jain AK, Blake P, Cordy P, Garg AX. Global trends in rates of peritoneal dialysis. J Am Soc Nephrol Am Soc Nephrol. 2012;23(3):533–44. doi: 10.1681/ASN.2011060607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abraham G, Khanna P, Mathew M, Pushpkala P, Mehrotra A, Sairam A, et al. How to make peritoneal dialysis affordable in developing countries. Contrib Nephrol. 2009;163:243–9. doi: 10.1159/000223805. [DOI] [PubMed] [Google Scholar]
- 6.Bangladesh Customs National Tariff Fiscal Year: 2016–2017. 2017. [Google Scholar]
- 7.Karopadi AN, Mason G, Rettore E, Ronco C. Nephrol Dial Transplant [Internet] 10. Vol. 28. England: 2013. Oct, Cost of peritoneal dialysis and haemodialysis across the world; pp. 2553–69. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23737482. [DOI] [PubMed] [Google Scholar]
- 8.Li PK, Chow KM. Peritoneal dialysis–first policy made successful: perspectives and actions. Am J Kidney Dis Elsevier. 2013;62(5):993–1005. doi: 10.1053/j.ajkd.2013.03.038. [DOI] [PubMed] [Google Scholar]
- 9.Abraham G, Varughese S, Thandavan T, Iyengar A, Fernando E, Naqvi SAJ, et al. Clin Kidney J. Oxford University Press; 2015. Chronic kidney disease hotspots in developing countries in South Asia; p. sfv109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parfitt B, Nahar NS. Int Nurs Rev [Internet] 2. Vol. 63. England: 2016. Jun, Nursing education in Bangladesh: a social business model; pp. 285–91. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26830518. [DOI] [PubMed] [Google Scholar]
- 11.Bunke CM, Brier ME, Golper TA. Kidney Int [Internet] 2. Vol. 52. Elsevier Masson SAS; 1997. Aug, Outcomes of single organism peritonitis in peritoneal dialysis: gram negatives versus gram positives in the Network 9 Peritonitis Study; pp. 524–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9264012. [DOI] [PubMed] [Google Scholar]
- 12.Martin LC, Caramori JCT, Fernandes N, Divino-Filho JC, Pecoits-Filho R, Barretti P. Geographic and educational factors and risk of the first peritonitis episode in brazilian peritoneal dialysis study (BRAZPD) patients. Clin J Am Soc Nephrol. 2011;6(8):1944–51. doi: 10.2215/CJN.11431210. [DOI] [PMC free article] [PubMed] [Google Scholar]