Abstract
Introduction
Thymic carcinomas are rare epithelial malignancies with limited data to guide management.
Methods
In order to identify areas of agreement and variability in current clinical practice, a 16-question electronic survey was given to members of the International Thymic Malignancy Interest Group (ITMIG). Areas of controversy were discussed with the Thymic Carcinoma Working Group and consensus was achieved, as described.
Results
One hundred ITMIG members responded. There was general agreement regarding the role for multimodality therapy with definitive surgical resection in physically fit patients with advanced, but resectable disease. Areas of controversy included the need for histologic confirmation prior to surgery, the role of adjuvant therapy, the optimal first-line chemotherapy regimen, and the recommended treatment course for marginally resectable disease with invasion into the great vessels, pericardium, and lungs.
Conclusions
The results of the questionnaire provide a description of the management of thymic carcinoma by 100 ITMIG members with a specific interest or expertise in thymic malignancies. Although there was agreement in some areas, clinical practice appears to vary significantly. There is a great need for collaborative research to identify optimal evaluation and treatment strategies. Given the need for multimodality therapy in many cases, a multidisciplinary discussion of the management of patients with thymic carcinoma is critical.
Keywords: thymic carcinoma, clinical management, survey, multimodality therapy
Introduction
Thymic carcinomas are rare epithelial tumors of the thymus with limited data to guide management decisions1. Thymic carcinomas are the most aggressive thymic tumor subtype2. Surgery is considered the cornerstone of management and typically the first step in treatment3,4. Adjuvant therapies such as radiation therapy (RT) and chemotherapy are often used to decrease the risk of recurrence5-9. Given the rarity of thymic epithelial tumors and paucity of prospective clinical trials, variability exists in the management practices.
The International Thymic Malignancies Interest Group (ITMIG) was established to increase collaborative efforts focused on these tumors, and develop management guidelines to enhance uniformity in treatment of these tumors. The Thymic Carcinoma Working Group (TCWG) is composed of a multidisciplinary group of ITMIG clinicians who meet regularly to identify ways to standardize and advance the work-up and management of thymic carcinoma. We surveyed ITMIG clinicians in order to identify areas of agreement and variability in current clinical practice related to management of thymic carcinomas.
Methods
A 16-question electronic survey was designed and approved by the members of the TCWG. All 565 ITMIG members were identified and invited to participate. Questions were directed at demographics and initial clinical management of thymic carcinoma (Table 1).
Table 1. Survey Questions and Answer Choices.
| Question # | Question Stem | Question Answer Choices |
|---|---|---|
| 1 | A 60 year old woman without significant past medical history presents with a 7 cm anterior mediastinal mass. She has intermittent chest pressure, but no symptoms of myasthenia. CT scan demonstrates a tumor in contact with the pericardium, but a fat plane is present. There is no evidence of distant metastatic disease, and there is no involvement of the lung, liver, bone, or pleura. What is your initial evaluation to obtain a pathologic diagnosis? |
|
| 2 | A 65 year old physically fit patient undergoes a complete thymectomy for a 3 centimeter thymic tumor. Pathology review identifies a thymic carcinoma (Masaoka stage II) with all margins negative. What do you recommend for postoperative management? |
|
| 3 | A 65 year old physically fit patient undergoes a complete thymectomy for a 3 centimeter thymic tumor. Pathology review identifies a thymic carcinoma with involvement of the pericardium (Masaoka stage III) with all margins negative. What do you recommend for postoperative management? |
|
| 4 | A physically fit 55 year old patient presents with a Masaoka stage IVA thymic carcinoma with an anterior mediastinal mass and multiple pleural nodules (>5). What is your recommended surgical management? |
|
| 5 | A physically fit 55 year old patient presents with a Masaoka stage IVA thymic carcinoma with an anterior mediastinal mass and multiple pleural nodules (>5). What is your recommended surgical management? |
|
| 6 | A 43 year old woman presents with Masaoka Stage IVB thymic carcinoma with an anterior mediastinal mass and multiple metastatic lung nodules (biopsy confirmed to represent metastatic disease). What is your preferred initial chemotherapy? |
|
| 7 | A 50 year old patient presents with a 5 × 6 centimeter anterior mediastinal mass with invasion into the mediastinal fat, but not the lungs, pericardium, heart or great vessels. On exam, two cervical (jugular and supraclavicular) lymph nodes are identified and found to be biopsy proven thymic carcinoma. What is your recommended treatment course? |
|
| 8 | A 65 year old patient presents with a 13 × 15 centimeter thymic carcinoma in the anterior mediastinum with invasion into the great vessels, pericardium and lungs bilaterally. What is your next recommended treatment step? |
|
| 9 | A 65 year old patient presents with recurrent thymic carcinoma in the anterior mediastinum measuring 8 × 6 centimeter in size and invading the right upper lobe of the lung. A staging workup does not reveal any distant metastatic disease, pleural or pulmonary nodules. He initially presented with stage II thymic carcinoma 2 years ago and underwent surgical resection without any chemotherapy or radiation therapy. What is your recommended treatment course? |
|
| 10 | A 50 year old patient is found to have unresectable thymic carcinoma due to invasion of the great vessels. What is your recommended treatment course? |
|
| 11 | A 60 year old patient presents after an R1 resection of a stage III thymic carcinoma with involvement of the adjacent lung and pericardium for adjuvant radiation therapy. The mediastinal margin is microscopically involved with malignancy. Which radiation technique would you find acceptable? |
|
| 12 | A 60 year old patient presents after an R1 resection of a stage III thymic carcinoma with involvement of the adjacent lung and pericardium for adjuvant radiation therapy. The mediastinal margin is microscopically involved with malignancy. Which radiation dose would you find acceptable? 1. 45 Gy 2. 50 Gy 3. 54 Gy 4. 60 Gy 5. 70 Gy |
|
The survey was conducted from 12/9/13 to 1/20/14. By grouping answers together, general agreement was determined by >60% concordance.
Areas of controversy were discussed with the TCWG and consensus was achieved, when possible, before the manuscript was prepared.
Results
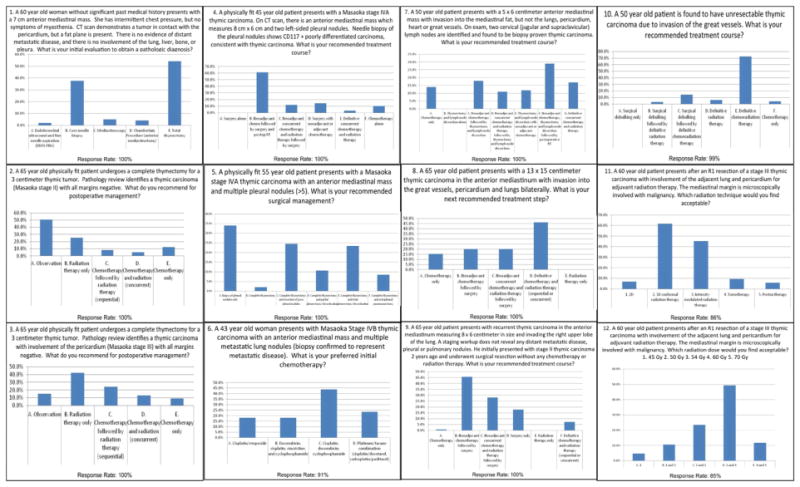
One-hundred ITMIG members responded. Table 2 lists the demographic information of the survey responders. Responses are depicted in Figure 1.
Table 2. Survey Responder Demographics.
| Profession (N) | |
|---|---|
| Surgeons | 60 |
| Medical Oncologists | 17 |
| Radiation Oncologists | 13 |
| Pathology/Pulmonology | 7 |
| Did Not Answer | 3 |
| Location of Practice (N) | |
| Europe | 39 |
| North America | 33 |
| Asia | 17 |
| Other | 7 |
| Did Not Answer | 4 |
| Experience Level (N), patients/year | |
| ≤6 | 33 |
| 7-12 | 37 |
| 12-24 | 12 |
| 25 or greater | 16 |
| Did Not Answer | 2 |
| Time Since Completing Medical Training (N) | |
| ≤5 years ago | 14 |
| 6-20 years ago | 56 |
| >20 years ago | 28 |
| Did Not Answer | 2 |
Figure 1. Survey Responses by Question.
Areas of general agreement and controversy
Areas of general agreement
-
-
The treatment course for stage IVA thymic carcinoma with limited number of left-sided pleural nodules (Question 4) with 87% of responders recommending multimodality therapy, including surgery.
-
-
The surgical management of stage IVA disease with multiple (>5) pleural nodules (Question 5) with 60% of responders recommending thymectomy with or without pleurectomy/decortication.
-
-
The treatment course for resectable disease with 2 biopsy-proven cervical lymph nodes (Question 7) with 69% of responders recommending multimodality therapy including surgery.
-
-
The treatment of locally recurrent disease (Question 9) with 75% of responders recommending multimodality therapy including surgery.
-
-
The treatment course for unresectable disease due to great vessel invasion (Question 10) with 71% recommending definitive chemoradiation.
-
-
The acceptable technique for adjuvant radiotherapy (Questions 11), with 93% of responders choosing some form of 3D planned radiation.
-
-
The acceptable dose of RT after an R1 resection (Question 12) with 73% of responders choosing 50-60 Gy.
Areas of controversy
-
-
The need for histologic confirmation of pathology prior to a total thymectomy (Question 1), with 54% of responders recommending upfront total thymectomy, 36% recommending a core biopsy and 10% recommending an alternative form of biopsy.
-
-
The role of adjuvant therapy after an R0 resection of a Masaoka Stage II thymic carcinoma (Question 2), with 51% of responders recommending observation, 25% recommending adjuvant RT alone, 13% recommending adjuvant RT and chemotherapy and 11% recommending adjuvant chemotherapy alone.
-
-
The role of adjuvant therapy after an R0 resection of a Masaoka Stage III thymic carcinoma (Question 3), with 42% recommending adjuvant RT alone, 34% recommending adjuvant RT and chemotherapy, 14% of responders recommending observation, and 10% recommending adjuvant chemotherapy alone.
-
-
The preferred first-line chemotherapy for Stage IVB thymic carcinoma (Question 6), with 42% recommending cisplatin/doxorubicin/cyclophosphamide, 23% recommending a platinum/taxane combination, 19% recommending cisplatin/etoposide and 16% recommending doxorubicin/cisplatin/vincristine/cyclophosphamide.
-
-
The recommended treatment course for disease with invasion into the great vessels, pericardium, and lungs bilaterally (Question 8) with 46% recommending definitive chemoradiation, 39% recommending multimodality therapy with surgery and 15% recommending chemotherapy alone.
Analysis by specialty
Upon further review of the results by specialty, some generalizations were noted. Surgeons were more likely to recommend surgical management for stage IVA disease with multiple (>5) pleural nodules (Question 5: 80% vs. 48% vs. 62%) or involvement of cervical lymph nodes (Question 7: 79% vs. 55% vs. 34%).
Discussion
We present the results of a questionnaire that provides a cross-sectional assessment of the management patterns of 100 ITMIG members, a group of physicians of various specialties with a particular clinical and scientific interest and expertise in these rare tumors Although there was agreement in some areas, clinical practice varies.
The areas of controversy highlight a clear need for collaborative research to identify optimal evaluation and treatment strategies. The areas of controversy identified from this survey were discussed by the TCWG and consensus across various disciplines was sought whenever possible.
Diagnostic Workup
The group discussed the need for pathologic diagnosis of thymic carcinoma prior to surgical resection. The consensus was that if patients require neoadjuvant therapy or if there is clinical or radiographic concern for lymphoma, germ cell tumor or other malignancy that is not typically managed with upfront surgery, then a core biopsy is indicated.
Surgical Management
Surgery is generally considered the cornerstone of treatment for patients with resectable thymic malignancies3,4. In patients with localized disease, the goal of surgery is curative. In patients with Stage IVA thymic carcinomas, however, generally the goal is prolonged disease free survival. There was general agreement on the need for multimodality therapy with surgery for patients with Stage IVA thymic carcinoma with pleural nodules, involved cervical lymph nodes or recurrent disease. It is important to note, however, that the majority of responders were surgeons. The decision regarding the role of surgical management of locally advanced thymic carcinoma has to be weighed against the risks of the invasive procedure.
The differing responses seen regarding the treatment course for patients with invasion into the great vessels, pericardium, and lungs bilaterally was thought to be related to differences in what was considered “resectable” by responders. Typically, invasion of the pericardium and lung does not preclude surgical resection and can be managed by pericardial resection and/or lung resection. Additionally, if patients have invasion of certain blood vessels, e.g. the superior vena cava or innominate vein, they may still be resectable. Since surgery is the main treatment modality in this disease, every attempt should be made to achieve an R0 resection.
A clinical vignette, which clearly stated that the patient was unresectable due to great vessel invasion, resulted in agreement that the patient should be treated with definitive chemoradiation. This topic was discussed by the group and it was mentioned that in addition to limited data suggest a potential role for debulking surgery in thymic carcinoma2,10,11, a recent large retrospective Japanese Nationwide Database study provided further support that maximal debulking surgery might be beneficial in these patients12. Due to the retrospective nature of that study, however, there is likely significant patient selection bias.
Radiation Therapy
The group discussed the role of adjuvant therapy in patients with Masaoka Stage II and III disease. Since the survey was conducted, there have been 3 publications demonstrating the benefit of adjuvant RT in large cohorts of completely resected thymic carcinoma5,7,9. Adjuvant RT demonstrated an overall survival benefit5,9,13. Because of these recent data, the group recommended the use of adjuvant RT in patients with Masaoka Stage II and III disease. The role of adjuvant RT in patients with completely resected Masaoka stage I thymic carcinoma requires further evaluation.
Chemotherapy
The role of adjuvant chemotherapy is less clear in patients with Masaoka Stage II and III disease. The options for first-line chemotherapy in patients with inoperable disease were discussed. The regimens of cisplatin/ doxorubicin/ cyclophosphamide and etoposide/cisplatin were generally considered preferred first-line regimens for malignant thymoma. In thymic carcinoma, recent data from phase II trials evaluating carboplatin/paclitaxel and capecitabine/gemcitabine have demonstrated favorable results6,8. The consensus from the TCWG was that there are insufficient data to favor one chemotherapy regimen over another and that more data are required to determine the optimal choice for first-line chemotherapy in patients with unresectable disease.
The role of molecular-targeted therapy in the treatment of unresectable thymic carcinoma has been evaluated in phase II clinical trials14,15. Further efforts are needed to identify additional molecular targets in thymic carcinoma and evaluate the role of immunotherapy.
Conclusion
In conclusion, the aforementioned results from a survey of providers specializing in thymic malignancies provide guidance for the treatment of patients with thymic carcinoma. The survey is limited by a small number of respondents, the majority being surgeons. Despite this, areas of agreement were determined, and the areas of controversy were discussed within the TCWG to derive consensus. These results highlight the need for collaborative research to identify optimal evaluation and treatment strategies, especially for management of locally advanced thymic carcinomas. The TCWG is currently working on multiple projects including prospective databases, immunotherapy trials, and genomic analyses, among others, to enhance clinical management and improve outcomes of patients with thymic carcinoma. Given the need for multimodality therapy in many cases, a multidisciplinary discussion of the management of patients with thymic carcinoma is critical.
Acknowledgments
Anja Roden (roden.anja@mayo.edu), Alex Marx (alexandermarx@umm.de)
Footnotes
Disclosures: The following authors have disclosures, which have been noted on the ICMJE form:
Dr. Andreas Rimner reports a grant, personal fees and non-financial support from Varian Medical Systems, a grant from Boehringer Ingelheim, and personal fees and non-financial support from Bristol Myers-Squibb, outside the submitted work;
Results were presented in part at the ITMIG 2014 Annual Meeting
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Detterbeck FC. The creation of the international thymic malignancies interest group as a model for rare diseases. American Society of Clinical Oncology educational book / ASCO American Society of Clinical Oncology Meeting. 2012:471–474. doi: 10.14694/EdBook_AM.2012.32.23. [DOI] [PubMed] [Google Scholar]
- 2.Kondo K, Monden Y. Therapy for thymic epithelial tumors: a clinical study of 1,320 patients from Japan. The Annals of thoracic surgery. 2003 Sep;76(3):878–884. doi: 10.1016/s0003-4975(03)00555-1. discussion 884-875. [DOI] [PubMed] [Google Scholar]
- 3.Filosso PL, Guerrera F, Rendina AE, et al. Outcome of surgically resected thymic carcinoma: a multicenter experience. Lung cancer. 2014 Feb;83(2):205–210. doi: 10.1016/j.lungcan.2013.11.015. [DOI] [PubMed] [Google Scholar]
- 4.Weksler B, Dhupar R, Parikh V, Nason KS, Pennathur A, Ferson PF. Thymic carcinoma: a multivariate analysis of factors predictive of survival in 290 patients. The Annals of thoracic surgery. 2013 Jan;95(1):299–303. doi: 10.1016/j.athoracsur.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 5.Ahmad U, Yao X, Detterbeck F, et al. Thymic carcinoma outcomes and prognosis: results of an international analysis. The Journal of thoracic and cardiovascular surgery. 2015 Jan;149(1):95–100. doi: 10.1016/j.jtcvs.2014.09.124. [DOI] [PubMed] [Google Scholar]
- 6.Hirai F, Yamanaka T, Taguchi K, et al. A multicenter phase II study of carboplatin and paclitaxel for advanced thymic carcinoma: WJOG4207L. Annals of oncology: official journal of the European Society for Medical Oncology / ESMO. 2015 Feb;26(2):363–368. doi: 10.1093/annonc/mdu541. [DOI] [PubMed] [Google Scholar]
- 7.Omasa M, Date H, Sozu T, et al. Postoperative radiotherapy is effective for thymic carcinoma but not for thymoma in stage II and III thymic epithelial tumors: the Japanese Association for Research on the Thymus Database Study. Cancer. 2015 Apr 1;121(7):1008–1016. doi: 10.1002/cncr.29166. [DOI] [PubMed] [Google Scholar]
- 8.Palmieri G, Buonerba C, Ottaviano M, et al. Capecitabine plus gemcitabine in thymic epithelial tumors: final analysis of a Phase II trial. Future oncology. 2014 Nov;10(14):2141–2147. doi: 10.2217/fon.14.144. [DOI] [PubMed] [Google Scholar]
- 9.Ruffini E, Detterbeck F, Van Raemdonck D, et al. Thymic carcinoma: a cohort study of patients from the European society of thoracic surgeons database. Journal of thoracic oncology : official publication of the International Association for the Study of Lung Cancer. 2014 Apr;9(4):541–548. doi: 10.1097/JTO.0000000000000128. [DOI] [PubMed] [Google Scholar]
- 10.Lin JT, Wei-Shu W, Yen CC, Liu JH, Chen PM, Chiou TJ. Stage IV thymic carcinoma: a study of 20 patients. The American journal of the medical sciences. 2005 Oct;330(4):172–175. doi: 10.1097/00000441-200510000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Liu HC, Hsu WH, Chen YJ, et al. Primary thymic carcinoma. The Annals of thoracic surgery. 2002 Apr;73(4):1076–1081. doi: 10.1016/s0003-4975(01)03607-4. [DOI] [PubMed] [Google Scholar]
- 12.Hishida T, Nomura S, Yano M, et al. Long-term outcome and prognostic factors of surgically treated thymic carcinoma: results of 306 cases from a Japanese Nationwide Database Study. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2015 Jun 26; doi: 10.1093/ejcts/ezv239. [DOI] [PubMed] [Google Scholar]
- 13.Rimner A. Postoperative radiotherapy: not all thymic malignancies are created equal. Cancer. 2015 Apr 1;121(7):972–974. doi: 10.1002/cncr.29164. [DOI] [PubMed] [Google Scholar]
- 14.Thomas A, Rajan A, Berman A, et al. Sunitinib in patients with chemotherapy-refractory thymoma and thymic carcinoma: an open-label phase 2 trial. The Lancet Oncology. 2015 Feb;16(2):177–186. doi: 10.1016/S1470-2045(14)71181-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zucali P, De Pas T. Phase II study of everolimus in patients with thymoma and thymic carcinoma previously treated with cisplatin-based chemotherapy. Journal of Clinical Oncology. 2014;32(15) 7527 doi: 10.1200/JCO.2017.74.4078. [DOI] [PubMed] [Google Scholar]


