Abstract
Background
Ukraine's HIV epidemic is concentrated among people who inject drugs (PWID), however, coverage with opioid agonist therapies (OATs) available mostly at specialty addiction clinics is extremely low. OAT integrated into primary healthcare clinics (PHCs) provides an opportunity for integrating comprehensive healthcare services and scaling up OAT.
Methods
A pilot study of PHC-based integrated care for drug users conducted in two Ukrainian cities between 2014 and 2016 included three sub-studies: 1) cross-sectional treatment site preference assessment among current OAT patients (N = 755); 2) observational cohort of 107 PWID who continued the standard of care versus transition of stabilized and newly enrolled PWID into PHC-based integrated care; and 3) pre/post analysis of attitudes toward PWID and HIV patients by PHC staff (N = 26).
Results
Among 755 OAT patients, 53.5% preferred receiving OAT at PHCs, which was independently correlated with convenience, trust in physician, and treatment with methadone (vs. buprenorphine). In 107 PWID observed over 6 months, retention in treatment was high: 89% in PWID continuing OAT in specialty addiction treatment settings (standard of care) vs 94% in PWID transitioning to PHCs; and 80% among PWID newly initiating OAT in PHCs. Overall, satisfaction with treatment, subjective self-perception of well-being, and trust in physician significantly increased in patients prescribed OAT in PHCs. Among PHC staff, attitudes towards PWID and HIV patients significantly improved over time.
Conclusions
OAT can be successfully integrated into primary care in low and middle-income countries and improves outcomes in both patients and clinicians while potentially scaling-up OAT for PWID.
Keywords: Methadone, Integrated care, Primary care, Patient preferences, Retention, Ukraine, HIV/AIDS
1. Introduction
Ukraine’s HIV epidemic is volatile and concentrated in people who inject drugs (PWID). PWID continue to have suboptimal access to HIV prevention and treatment services (UNAIDS, 2016a,b), which undermines the national response to HIV. Opioid agonist therapies (OATs) like methadone and buprenorphine, evidence-based interventions that reduce HIV transmission and morbidity and mortality from opioid use, first started in Ukraine in 2004 (Bruce et al., 2007), yet are under-scaled such that only 2.7% of the 310,000 PWID currently receive this treatment (Bojko et al., 2016; Wolfe et al., 2010)
Since 2004, OAT in Ukraine has primarily been provided in specialty addiction treatment clinics known as Narcology Centers. These settings are vestiges of a Soviet-style discipline of addiction treatment that traditionally did not deploy evidence-based strategies (Latypov, 2011). Soviet-style healthcare services have prioritized siloed specialty care delivery and consequently weakened primary healthcare services. OAT in Ukraine requires that methadone and buprenorphine be supervised daily through required visits to these centers, even for patients who are deemed medically stable. Moreover, Narcology Centers are often inconvenient for patients by virtue of being located in remote areas with long lines due to limited hours of operation (Bojko et al., 2015; Bojko et al., 2016). With the exception of where OAT is provided in integrated care settings (Bachireddy et al., 2014), additional services that prevent or treat other medical co-morbidities are often absent, with the exception of annual screening for tuberculosis or HIV testing.
Primary healthcare clinics (PHCs), however, provide routine medical care for non-specialty conditions and are embedded within polyclinics. Prevention and treatment services for addiction, HIV and tuberculosis have not been available in these settings. Expected international funding reductions anticipated in 2017 prompted new healthcare reform and financing efforts by Ukraine’s Ministry of Health to reduce emphasis on specialty care and strengthen primary care for medically complex and socially vulnerable patients like PWID. This is especially crucial since provision of OAT in PHCs is effective in many other international settings (Bachireddy et al., 2015). Despite international recommendations to integrate OAT and PHCs (CDC, 2012; Sylla et al., 2007; Thompson et al., 2012; WHO/UNODC/UNAIDS, 2008), there is little empirical guidance for administrators, clinicians, policy-makers and funders. Real-world demonstration projects with PWID are needed to help guide policy and delivery practices. While OAT services have been integrated into HIV and TB specialty services (Bachireddy et al., 2014; Morozova et al., 2013), until recently, integration into PHCs was not allowable. Now in the setting of a weakened economy and unbridled HIV epidemic, Ukraine’s Ministry of Health has called for sweeping healthcare reform, including strengthening of PHC-based services, which provides new opportunities for empirically testing innovative strategies. One strategy recommended to scale-up OAT services is to provide it in a number of non-specialty settings like PHCs and pharmacies, which could reduce barriers to treatment entry and promote retention (Bachireddy et al., 2015; Bojko et al., 2015). OAT integrated into PHCs has been examined in high-income settings (Carrieri et al., 2014; Parmenter et al., 2013; Weisner et al., 2001), yet has not been implemented in low or middle-income settings in Eastern Europe and Central Asia, the only UNAIDS region where HIV morbidity and mortality continue to increase (UNAIDS, 2016a).
To determine if such an integrated care strategy would work in Ukraine, we conducted a series of pilot studies of OAT integrated into PHCs in two Ukrainian cities, Mykolaiv and Poltava, to assess: 1) the feasibility of the pilot intervention in Ukrainian context; 2) retention in treatment; 3) patient satisfaction with the pilot intervention; and 4) the attitudes of primary care providers towards PWID. This paper provides a summary of key findings from this pilot.
2. Methods
2.1. Study sites
In both Mykolaiv and Poltava, district PHCs and addiction specialty clinics were selected for participation (one PHC in Mykolaiv and two in Poltava). To assess patient preferences about where they would prefer to receive OAT, an additional specialty addiction site in Kyiv was selected.
2.2. Study participants and design
Three sub-studies to address the aims included:
2.2.1. Assessment of preferences among current
An anonymous cross-sectional survey of 755 current OAT patients at specialty addiction clinics in Mykolaiv, Poltava and Kyiv was conducted to assess patients’ preferences in terms of where they prefer to receive OAT. Eligibility included: 1) age ≥18 years; 2) prescribed OAT at a specialty addiction clinic; and 3) verbal consent. Survey items included patient preference related to type of treating physician, location (convenience), stigma and police harassment, and overall preference.
2.2.2. Assessment of PHC-based OAT among patients transitioning from specialty addiction clinics and new patients initiating OAT at the PHCs
OAT patients in the longitudinal cohort were observed for six months and included those who: 1) continued to receive OAT at the specialty addiction clinics (N = 36); 2) transitioned from specialty to PHC-based OAT (N = 31), and 3) initiated OAT in PHC (N = 40). Groups 1 and 2 were randomly selected from current OAT patients and recruited within Narcology Centers. Group 3 patients included newly recruited, opioid dependent PWID interested in receiving OAT, but were required to receive it at the PHC. Groups 1 and 2 patients must also have been on a stable dose of methadone for at least 10 days prior to enrollment, not have an outstanding police warrant, not planning to move in the next 6 months, and willing to be allocated to either condition. Participants were surveyed at baseline and after 6 months and willing to have their medical charts reviewed.
The a priori pre-specified primary outcome was retention in treatment over 6 months. Group 1 participants were only assessed for the primary outcome based on chart review of medication-administration records. Secondary outcomes included changes in the satisfaction with their methadone treatment, health-related quality of life and health well-being, illicit drug use, HIV and HCV diagnostics and treatment, use of non-addiction treatment medical services, and trust in physician. Secondary outcomes were only assessed for Groups 2 and 3, and participants from these groups provided additional self-reports within structured surveys at baseline and six months. Where needed, survey items were translated and back-translated to ensure comprehension (Brislin, 1970), and included the following validated scales: satisfaction with receiving methadone (5-point Likert); scale assessing opioid craving (10-point Likert); the 11-item trust in physician scale (Anderson and Dedrick, 1990); health-related quality of life (HRQoL) scale (12-item short-form, second version) (Ware et al., 1996), and subjective changes in physical and mental health (5-point Likert). We analyzed HRQoL by producing a single aggregate score that varies from 0 to 100, where higher scores reflect better health status. The aggregate score was calculated as an unweighted average of scores in eight standard domains of functioning and well-being.
2.2.3. Assessment of attitudes among medical providers at the PHC facilities
Medical staff at the three PHCs were assessed at baseline and after six months, including: 1) chief administrators and medical directors (N = 6); 2) primary care doctors and nurses directly (N = 11) and indirectly (N = 9) involved in providing integrated care to PWID. They answered structured surveys at baseline and after six months and completed in-depth interviews after six months. Structured surveys included 10-point feeling thermometers (Alwin, 1997) about treating general, PWID and HIV patients, which has been adapted for other contexts (Earnshaw et al., 2014; Jin et al., 2014).
2.3. Data analysis
Statistical analysis was done in R Statistical Software (Foundation for Statistical Computing, Vienna, Austria). Correlates of preference for OAT treatment site were analyzed using multivariate logistic regression, where independent variables included location (convenience), type of OAT (methadone vs buprenorphine), age and other factors that could influence preference: stigma, police harassment, and physician trust. Chi-squared testing (or Fisher’s exact test) for categorical variables and Student t-test (or ANOVA) for continuous variables assessed significance. In the observational study, a pre/post comparison was performed using McNemar’s and paired Student t-test for categorical and continuous variables, respectively.
2.4. Ethics statement
Ethical oversight for the study was provided by the institutional review board at the Ukrainian Institute on Public Health Policy.
3. Results
3.1. Treatment site preferences (N = 755)
Table 1 presents baseline participant characteristics and a summary of the treatment site preference assessment. The 755 current OAT patients had a mean age of 37.2 years (SD = 7.7) and were from three cities: Poltava (N = 201, 26.6%), Mykolaiv (N = 201; 26.6%), and Kyiv (N = 353; 46.8%). Most OAT patients were receiving methadone (N = 588; 77.9%) and 167 (22.1%) received buprenorphine. Participants were first queried about various factors that could potentially influence their ultimate preference about treatment setting. There were significant differences in preferences by city (Table 1) for all “individual” choice dimensions (e.g., location, trust, stigma). After assessing these individual preferences, participants were then asked where they would most prefer to receive OAT. For the overall site preference, there was no difference between the three cities, with 53.5% of respondents preferring OAT provided at PHC rather than in their current Narcology Center. All questions were worded as a hypothetical possibility, and did not imply that a patient would be able to make a transition based on their choice.
Table 1.
Comparison of Preferences and Expectations for Opioid Agonist Treatment in Patients Receiving Treatment in Specialty Addiction Treatment Settings in Three Ukrainian Cities (N = 755).
| Overall N = 755 |
Poltava N = 201 |
Mykolaiv N = 201 |
Kyiv N = 353 |
p-value* | |
|---|---|---|---|---|---|
| Age | 37.2 (7.7) | 36.9 (7.2) | 40.7 (7.0) | 35.3 (7.7) | <0.001 |
| Treatment medication: | |||||
| Methadone | 588 (77.9) | 176 (87.6) | 186 (92.5) | 226 (64.0) | <0.001 |
| Buprenorphine | 167 (22.1) | 25 (12.4) | 15 (7.5) | 127 (36.0) | |
| Preferred location is: | |||||
| Primary care clinic | 478 (63.6) | 112 (56.6) | 133 (66.2) | 233 (66.0) | 0.058 |
| Specialty care clinic | 274 (36.4) | 86 (43.4) | 68 (33.8) | 120 (34.0) | |
| Preferred physician is: | |||||
| Primary care physician | 420 (56.1) | 96 (48.7) | 85 (42.3) | 239 (68.1) | <0.001 |
| Specialty care physician | 329 (43.9) | 101 (51.3) | 116 (57.7) | 112 (31.9) | |
| Expected stigma is less at: | |||||
| Primary care clinic | 310 (42.0) | 70 (35.2) | 108 (54.5) | 132 (38.7) | <0.001 |
| Specialty care clinic | 428 (58.0) | 129 (64.8) | 90 (45.5) | 209 (61.3) | |
| Expected police harassment is less at: | |||||
| Primary care clinic | 483 (65.5) | 147 (73.1) | 179 (90.4) | 157 (46.4) | <0.001 |
| Specialty care clinic | 254 (34.5) | 54 (26.9) | 19 (9.6) | 181 (53.5) | |
| Trust in physician is higher at: | |||||
| Primary care clinic | 172 (23.4) | 49 (24.4) | 97 (48.7) | 26 (7.8) | <0.001 |
| Specialty care clinic | 563 (76.6) | 152 (75.6) | 102 (51.3) | 309 (92.2) | |
| Preferred treatment site is: | |||||
| Primary care clinic | 401 (53.5) | 101 (50.5) | 112 (55.7) | 188 (53.9) | 0.565 |
| Specialty care clinic | 349 (46.5) | 99 (49.5) | 89 (44.3) | 161 (46.1) |
For categorical variables data is presented in the form: N (%), and for continuous variables: mean (SD). Percentage is calculated using total non-missing responses in the denominator. Values may not sum up to totals due to missing values.
p-value for the ANOVA for continuous variables and Chi-square test for categorical variables.
In order to evaluate how various factors might influence the overall treatment site preference, multivariate logistic regression (Table 2) suggests that all covariates except age were significantly associated with preferring OAT integrated into PHC. Factors most significant for this outcome include convenience (proximity) (AOR = 30.2, 95%CI: 14.4; 63.3) and higher trust in physician (AOR = 14.9, 95%CI: 5.6; 39.3). Interestingly, patients currently prescribed buprenorphine rather than methadone, were significantly less likely to choose PHC-based treatment (AOR = 0.5, 95%CI: 0.3; 0.9).
Table 2.
Independent Correlates in Preference for Receiving Opioid Agonist Treatment in Primary Healthcare Clinics (N = 755).
| Covariate | AOR | 95% CI for AOR |
|---|---|---|
| Intercept | 0.07 | (0.02–0.27) |
| Site: | ||
| Kyiv | RC | RC |
| Poltava | 1.05 | (0.55–2.00) |
| Mykolaiv | 0.39 | (0.16–0.98) |
| Treatment medication: | ||
| Methadone | RC | RC |
| Buprenorphine | 0.50 | (0.28–0.88) |
| Age | 0.98 | (0.94–1.01) |
| Preferred location is: | ||
| Specialty care clinic | RC | RC |
| Primary care clinic | 30.16 | (14.36–63.34) |
| Preferred physician is: | ||
| Specialty care physician | RC | RC |
| Primary care physician | 2.74 | (1.43–5.25) |
| Expected stigma is less at: | ||
| Specialty care clinic | RC | RC |
| Primary care clinic | 2.00 | (1.17–3.42) |
| Expected police harassment is less at: | ||
| Specialty care clinic | RC | RC |
| Primary care clinic | 1.84 | (1.04–3.27) |
| Trust in physician is higher at: | ||
| Specialty care physician | RC | RC |
| Primary care physician | 14.87 | (5.63–39.27) |
McFadden’s pseudo r-squared for the multivariate logistic regression model = 0.59,
AOR: adjusted odds ratio; CI: confidence interval; RC: reference category
3.2. Longitudinal cohort of patients prescribed opioid agonist therapies (N = 107)
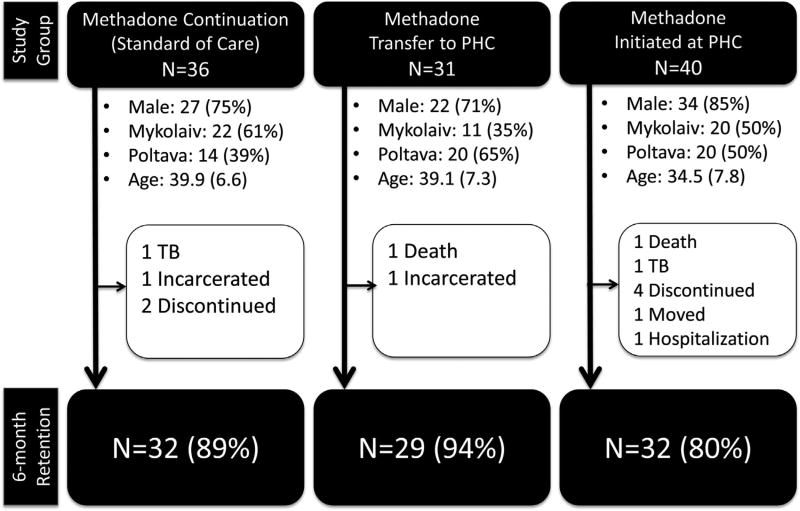
Fig. 1 describes basic demographics and primary outcome (treatment retention) information for OAT patients in each group. The stable OAT patients randomized to Groups 1 or 2 had, on average, received methadone for 2.4 (SD = 1.9) and 3.2 (SD = 2.0) years, respectively (p = 0.089). After six months, treatment retention remained high in both groups (89% vs. 94%, p = 0.678). No switches between Groups 1 and 2 were recorded over six months of observation. For patients newly initiating methadone in PHCs, however, retention was 80%, similar to retention in specialty addiction clinics in Ukraine (Schaub et al., 2010). Over the period of observation, none of the new OAT patients switched to the specialty care site. In addition to the proportion retained at 6 months, Fig. 1 also details the reasons for drop-out, which may or may not indicate discontinuation of treatment. For example, because OAT is not available during incarceration, such individuals would forcibly discontinue OAT, but for patients hospitalized for tuberculosis, those in Poltava and Mykolaiv could continue OAT since it is available in their regional tuberculosis hospitals.
Fig. 1.
Demographics and Treatment Retention for the Observational Cohort of Opioid Agonist Treatment Patients.
Table 3 provides a summary of the secondary analyses, which largely consists of within individual pre/post comparisons, where participants serve as their own controls. In patients transferring from addiction to PHCs, reasons stated for their willingness to transfer included: convenience or proximity (100%), the opportunity to address other medical conditions at the same site (35%), and ability to avoid large numbers of other drug users (26%). All patients reported that the transition process went very smoothly, and that social workers played a key role in facilitating the transfer. The mean pre/post satisfaction scores increased significantly (p = 0.016) from 3.8 (SD = 1.2) to 4.8 (SD = 0.8). Six months after transitioning to PHC-based treatment, participants were asked to compare their current experience with the specialty addiction clinic, with 18 (58%) reporting their health and overall care as considerably better and 9 (29%) indicated it was somewhat better. None of the respondents said that it got worse (data not shown).
Table 3.
Secondary Outcomes Among Patients Transitioning to and Newly Initiating Opioid Agonist Treatment in Primary Healthcare Clinics (N = 67).a
| Secondary outcomes | Transitioning patients N = 29 |
New patients N = 38 |
||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Baseline | After 6 months |
p-valueb | Baseline | After 6 months |
p-valueb | |
| Overall satisfaction with the program (5-point Likert scale) | 3.76 (1.15) | 4.45 (0.83) | 0.016 | – | 4.79 (0.70) | – |
| Injecting drug use during the last 30 days (number of days) | 1.31 (5.58) | 1.45 (5.80) | 0.547 | 27.87 (6.32) | 0.21 (0.62) | <0.001 |
| Opioid craving (10-point Likert scale) | 3.34 (5.59) | 3.71 (3.01) | 0.626 | 6.55 (3.33) | 3.01 (2.87) | <0.001 |
| HIV diagnosisc | 9 (29.0) | 11 (35.5) | – | 12 (30.0) | 12 (30.0) | – |
| New ART initiations (among HIV-infected) | – | 0 (0.0) | – | – | 5 (41.7) | – |
| HCV diagnosisc | 12 (38.7) | 19 (61.3) | – | 10 (25.0) | 25 (62.5) | – |
| Aggregate measure of HRQoL (0–100 scale) | 58.22 (16.59) | 53.52 (19.83) | 0.164 | 58.26 (18.59) | 65.59 (21.16) | 0.013 |
| Subjective improvement of physical health (compared to baseline) | – | 16 (55.2) | – | – | 30 (76.9) | – |
| Subjective improvement of mental health (compared to baseline) | – | 19 (65.5) | – | – | 32 (82.1) | – |
| Trust in physician (11–55 scale) | 31.07 (7.16) | 35.50 (6.66) | 0.007 | 32.39 (6.09) | 38.47 (6.55) | <0.001 |
For categorical variables data is presented in the form: N (%), and for continuous variables: mean (SD). HRQoL: health-related quality of life; ART: antiretroviral therapy.
This analysis is restricted to patients, for whom both baseline and 6-months follow-up data is available (except HIV and HCV diagnosis indicators).
p-value for continuous variables corresponds to the paired Student t-test.
HIV and HCV diagnosis indicators use the entire cohort (N = 31 transitioning patients, and N = 40 new patients) in the denominator.
Transitioning patients in both cities reported limited availability of medical services other than addiction treatment provided at the specialty addiction clinics. Analysis of charts of patients continuing care at the specialty addiction clinic (standard of care) demonstrated limited access to diagnostic and screening procedures, which mostly included required urine drug testing for opioids, chest radiographs and HIV testing. In comparison, transitioning patients made routine visits to their primary care physician about twice monthly, including complete physical examinations each quarter. While no significant changes were observed in their HRQoL (measured with an aggregate score from the 12-item short-form), transitioning patients reported subjective improvements in their physical (55%) and emotional (66%) well-being.
Eleven (36%) transitioning patients were HIV-infected, and 2 of them were diagnosed after transition to the PHC. Among 9 transitioning patients with known HIV at baseline, 5 were receiving antiretroviral therapy (ART). After six months, there were no further ART initiations, and both patients who dropped out (one death and one incarceration) were among the 5 individuals receiving ART at baseline. Chart review data for HCV found 19 (61%) patients with confirmed HCV at the follow-up assessment, yet another 3 patients reported being told by a medical provider that they had HCV in the past. One of these 3 patients was incarcerated soon after transitioning to the PHC, and was unable to be tested (data not shown).
Mean trust in physician scores increased significantly (p = 0.007) over time in transitioning OAT patients from 31.1 (SD = 7.2) to 35.5 (SD = 6.7) after 6 months, and 79% of them reported that they would not want to return to specialty addiction clinics (data not shown), with most expressing fear that they would be forced to leave the PHC if the program was stopped.
For PWID initiating OAT in PHCs, the treatment enrollment procedures differed by site, which were dictated by the regional chief addiction specialist. While PWID in Mykolaiv completed the entire induction and stabilization process within the PHC, Poltava patients were required to be inducted at the specialty addiction clinic before transitioning to the PHC-based treatment. In general, this process involved 1–4 weeks. While both strategies were feasible, both patients and primary care physicians in Poltava said that the induction procedure was inconvenient and unnecessary.
Patients newly initiating OAT in PHCs had, on average, injected opioids for 14.5 years (SD = 8.1) and had multiple previous unsuccessful attempts to quit drug use without using OAT, including detoxification (N = 35, 88%) within an inpatient addiction treatment unit, and drug-free rehabilitation with counseling (N = 15, 38%). Three patients (8%) had attempted to initiate methadone before, but were unable to do so due to limited treatment slots and long waiting lists (data not shown).
Not surprisingly, patients newly initiating OAT significantly (p < 0.001) reduced their mean number of days injecting opioids per month from 27.9 (SD = 6.3) to 0.2 (SD = 0.6) and mean opioid craving score from 6.6 (SD = 3.3) to 3.0 (SD = 2.9). Meanwhile, overall satisfaction with PHC-based OAT was high (mean score = 4.8 (SD = 0.7) on the 5-point scale) and most (N = 34, 85%) patients reported that their district PHC clinic was very convenient. Additionally, a critical minority (N = 16, 40%) of these newly induced patients said that having access to various medical services plays an important role in remaining in OAT and was driven primarily by 24 (60%) of initiating patients not having received any medical services during the previous 6 months (data not shown).
New initiates to OAT reported significant (p = 0.013) improvement in HRQoL. The mean aggregate HRQoL score increased from a mean of 58.3 (SD = 18.6) to 65.6 (SD = 21.2) over six months. The most notable improvements were observed for subscales measuring mental health and social functioning (data not shown). Similarly for the transitioning patients, new OAT initiates in PHCs reported substantial subjective improvement in their physical (77%) and emotional (82%) well-being.
While no new HIV diagnoses were observed in new OAT patients, 5 of 12 HIV infected participants started ART after initiating OAT. For this same group, besides 25 confirmed HCV diagnoses at the follow up assessment, another 6 patients reported having being told by a medical provider that they had HCV in the past; one of these 6 patients had been in treatment for less than a month, and did not have a chance to get tested.
Trust in physician among initiating patients demonstrated similar dynamics to that of transitioning patients with mean scores significantly (p < 0.001) increasing from 32.4 (SD = 6.1) to 38.5 (SD = 6.6).
3.3. Clinic staff surveys
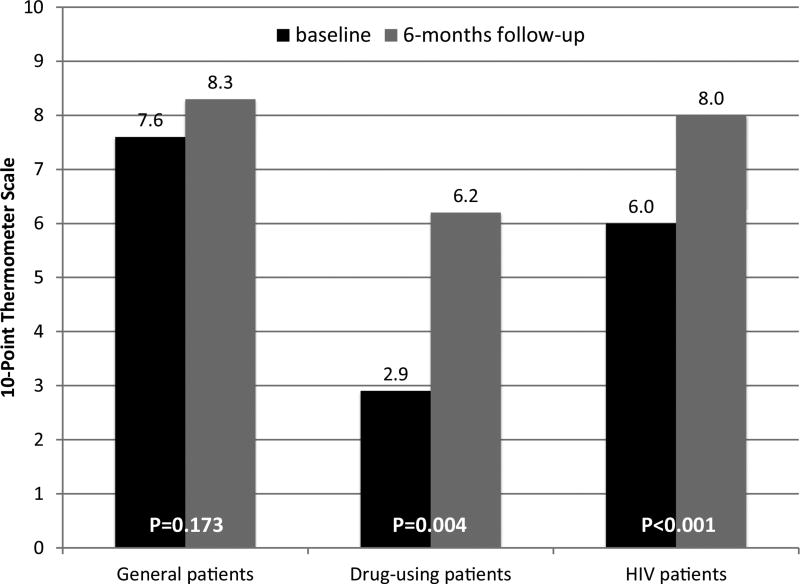
Most administrative and clinical staff members were women (88%) in their mid-40s (mean age = 43.2 years, SD = 10.2). Fig. 2 reports the mean pre/post feelings toward the three types of patients. While attitudes toward both drug-using and HIV patients significantly improved over time, these scores remained unchanged for general medical patients.
Fig. 2.
Changes in Primary Care Medical Staff Attitudes Toward the Three Types of Patients.
4. Discussion
To the best of our knowledge, this is the first study to pilot test integrating OAT into PHCs, for opioid dependent PWID in Eastern Europe and Central Asia (EECA). This is especially important since EECA remains the only region globally where HIV incidence and mortality continue to increase (UNAIDS, 2016a), in the presence of HIV concentrated in PWID and a lack of effective prevention services (UNAIDS, 2016b). PHCs in Ukraine and elsewhere in the region provide a new strategy, yet underutilized resource to expand OAT to PWID with opioid dependence. Several important lessons were learned from this study. Over half of patients receiving OAT in specialty settings, the current standard of care, would prefer to receive it in PHC settings. PHC facilities are embedded throughout the community through a large network and more conveniently located within neighborhoods where patients live or work. This convenience reduces transportation and time burden on patients, who are required to visit OAT sites daily. Analysis of the treatment site preferences of current OAT patients shows that the most important factor influencing the decision about the preferred site is convenience or proximity of the site. This is especially important since OAT sites are often located inconveniently for patients and PHC clinics are relatively close. Interestingly and somewhat unexpectedly patients receiving buprenorphine are twice less likely to choose receiving OAT in PHC facilities, compared to those receiving methadone. Because both methadone and buprenorphine must be taken daily in clinical settings, the observed differences in preferences cannot be explained by the lower transportation burden among buprenorphine patients. Historically, because buprenorphine was introduced first and is generally preferred more since it is restricted to less than 10% of patients prescribed OAT, buprenorphine is often viewed as a superior treatment (Makarenko et al., 2016). This may, in part, explain their relative unwillingness to switch to a different treatment site due to a perception that their elevated status of receiving a restricted treatment might be undermined.
From the public health system perspective, integrating OAT into PHCs would potentially scale-up OAT coverage by making OAT more accessible and allowing patients on waiting lists and those who were not interested in logistical restrictions in Narcology Centers to receive treatment. Even for those receiving OAT in specialty addiction clinics where lines are long and dispensation limited to a few hours, over a quarter of participants transitioning to PHCs for OAT reported their motivation for changing sites was to avoid daily interactions with other PWID.
Drug injection is a known risk factor for multiple co-morbid health conditions (Altice et al., 2010). The lack of availability of non-addiction treatment at Narcology Centers complicates care for patients with multiple comorbidities. The daily visits to PHCs provide expanded opportunities for screening and treatment for a number of conditions. Although there were no improvements overall in HRQoL in patients transitioning to PHCs, the majority reported subjective improvement in their physical and mental well-being. HRQoL, however, was markedly improved in those newly initiating OAT, who demonstrated significant increase in both standard and subjective measures of health-related well-being. This finding is consistent with PWID newly initiating methadone in Ukraine (Dvoriak et al., 2014).
Although HIV testing is largely available at the specialty care addiction clinics, 2 out of 11 transitioning patients with HIV were diagnosed at the PHC. Importantly and similar to findings in the United States with HIV patients enrolling in buprenorphine treatment (Altice et al., 2011), nearly half (5 of 12) of new patients initiated ART. Similarly, a number of patients were newly diagnosed with HCV after starting OAT in PHCs. One potential reason for the low level of HCV testing at the specialty care clinics might be related to the virtual absence of affordable and tolerable HCV treatment in Ukraine.
Anecdotally, addiction treatment specialists perceive that OAT cannot be provided by anyone without extensive training, which has restricted OAT expansion to PHCs. Similar attitudes by specialists have restricted HIV treatment to specialty settings. Research from the United States suggest that primary care clinicians, if adequately supported through collaborative learning environments, can achieve the same outcomes as specialty physicians. Project ECHO (Extension for Community Health Outcomes) is one such strategy that can support primary care clinicians (Arora et al., 2011). Findings here, however, suggest that not only can non-specialists deliver care that results in optimal treatment outcomes, measured here minimally as treatment retention that is at least similar to that provided at specialty addiction care sites. In addition to the high retention rates, trust in physicians increases among patients who transition to PHCs, as does overall satisfaction with the methadone treatment program. This is especially salient as trust in physician is the second most important determinant of overall treatment site preference.
In addition to benefitting patients, provision of OAT in PHCs positively influences medical providers who developed more positive attitudes towards drug-using and HIV patients, lending support for the contact hypothesis that states that people reduce negative attitudes toward stigmatized individuals after they have real lived experiences with them (Earnshaw et al., 2016). Concerning here was the remarkably low baseline scores toward drug-using patients, which persists across many settings in Ukraine (Polonsky et al., 2015), and necessitates increasing training and contact with drug users both in medical students and primary care doctors in clinical practice.
5. Conclusions
Though this study should be interpreted by the inherent limitations in pilot studies with small sample sizes, it does provide proof-of-concept evidence that OAT integration into PHCs is feasible and acceptable in Ukraine and may provide important insights for other low to middle-income countries that seek alternative OAT delivery strategies. Importantly here, not only do patients do well in transitioning from specialty addiction clinics, but can also initiate it in PHCs. Such findings extend beyond patient-level outcomes and are supported by the markedly improved attitudes by medical personnel toward patients with substance use disorders and with HIV. Such strategies are likely to reduce the near universal stigma that these patients experience in Ukraine (Polonsky et al., 2016) and throughout Eastern Europe and Central Asia where HIV mortality and incidence are continuing to increase (UNAIDS, 2016a). Such strategies appear to be beneficial to patients, clinicians, public health and innovations in healthcare delivery and are an important next step to scaling up OAT and improving HIV outcomes in one of Europe’s most devastated countries.
Acknowledgments
We want to thank medical staff of the participating clinics, as well as interviewers and patients for their contribution to the implementation of this study.
Role of funding source
This work was supported by the USAID via Pact Inc. (grant 380A0689/P4044-47, 2014–2016). OM receives support from the National Institute of Mental Health (R01MH105203) and National Institute on Drug Abuse (R36DA042643). FLA and SD receive funding from the National Institute on Drug Abuse (K24 DA017072, R01 DA033679 and R01 DA029910). The funding sources had no role in data collection or analysis, manuscript writing or revision, or decision to submit this paper for publication.
Footnotes
Contributors
OM, SD and FLA designed the study and wrote the protocol. IP supervised the implementation of the study. OM undertook the statistical analysis and wrote the first draft of the manuscript. All authors contributed to the manuscript revision and have approved its final version.
Conflicts of interest
None.
References
- 1.Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376:367–387. doi: 10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Altice FL, Bruce RD, Lucas GM, Lum PJ, Korthuis PT, Flanigan TP, Cunningham CO, Sullivan LE, Vergara-Rodriguez P, Fiellin DA, Cajina A, Botsko M, Nandi V, Gourevitch MN, Finkelstein R Collaborative B. HIV treatment outcomes among HIV-infected, opioid-dependent patients receiving buprenorphine/naloxone treatment within HIV clinical care settings: results from a multisite study. J. Acquir. Immune Defic. Syndr. 2011;56(Suppl. 1): S22–S32. doi: 10.1097/QAI.0b013e318209751e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alwin DF. Feeling thermometers versus 7-point scales – which are better? Soc. Method Res. 1997;25:318–340. [Google Scholar]
- 4.Anderson LA, Dedrick RF. Development of the Trust in Physician scale: a measure to assess interpersonal trust in patient-physician relationships. Psychol. Rep. 1990;67:1091–1100. doi: 10.2466/pr0.1990.67.3f.1091. [DOI] [PubMed] [Google Scholar]
- 5.Arora S, Thornton K, Murata G, Deming P, Kalishman S, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N. Engl. J. Med. 2011;364(23):2199–2207. doi: 10.1056/NEJMoa1009370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bachireddy C, Soule MC, Izenberg JM, Dvoryak S, Dumchev K, Altice FL. Integration of health services improves multiple healthcare outcomes among HIV-infected people who inject drugs in Ukraine. Drug Alcohol Depend. 2014;134:106–114. doi: 10.1016/j.drugalcdep.2013.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bachireddy C, Weisberg DF, Altice FL. Balancing access and safety in prescribing opioid agonist therapy to prevent HIV transmission. Addiction. 2015;110:1869–1871. doi: 10.1111/add.13055. [DOI] [PubMed] [Google Scholar]
- 8.Bojko MJ, Mazhnaya A, Makarenko I, Marcus R, Dvoriak S, Islam Z, Altice FL. Bureaucracy & Beliefs: assessing the barriers to accessing opioid substitution therapy by people who inject drugs in Ukraine. Drugs. 2015;22:255–262. doi: 10.3109/09687637.2015.1016397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bojko MJ, Mazhnaya A, Marcus R, Makarenko I, Islam Z, Filippovych S, Dvoriak S, Altice FL. The future of opioid agonist therapies in Ukraine: a qualitative assessment of multilevel barriers and ways forward to promote retention in treatment. J. Subst. Abuse Treat. 2016;66:37–47. doi: 10.1016/j.jsat.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brislin RW. Back-translation for cross-cultural research. J. Cross Cult. Psychol. 1970;1:185–216. [Google Scholar]
- 11.Bruce RD, Dvoryak S, Sylla L, Altice FL. HIV treatment access and scale-up for delivery of opiate substitution therapy with buprenorphine for IDUs in Ukraine–programme description and policy implications. Int. J. Drug Policy. 2007;18:326–328. doi: 10.1016/j.drugpo.2006.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Report, M.R.a, editor. CDC. Integrated Prevention Services for HIV Infection, Viral Hepatitis, Sexually Transmitted Diseases, and Tuberculosis for Persons Who Use Drugs Illicitly. CDC; 2012. pp. 1–40. (Summary Guidance from CDC and the U. S. Department of Health and Human Services) [PubMed] [Google Scholar]
- 13.Carrieri PM, Michel L, Lions C, Cohen J, Vray M, Mora M, Marcellin F, Spire B, Morel A, Roux P Methaville Study, G. Methadone induction in primary care for opioid dependence: a pragmatic randomized trial (ANRS Methaville) PLoS One. 2014;9:e112328. doi: 10.1371/journal.pone.0112328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dvoriak S, Karachevsky A, Chhatre S, Booth R, Metzger D, Schumacher J, Chychula N, Pecoraro A, Woody G. Methadone maintenance for HIV positive and HIV negative patients in Kyiv: acceptability and treatment response. Drug Alcohol Depend. 2014;137:62–67. doi: 10.1016/j.drugalcdep.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Earnshaw VA, Jin H, Wickersham J, Kamarulzaman A, John J, Altice FL. Exploring intentions to discriminate against patients living with HIV/AIDS among future healthcare providers in Malaysia. J. Trop. Med. Int. Health. 2014;19:672–679. doi: 10.1111/tmi.12306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Earnshaw VA, Jin H, Wickersham JA, Kamarulzaman A, John J, Lim SH, Altice FL. Stigma toward men who have sex with men among future healthcare providers in Malaysia: would more interpersonal contact reduce prejudice? AIDS Behav. 2016;20:98–106. doi: 10.1007/s10461-015-1168-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jin H, Earnshaw VA, Wickersham JA, Kamarulzaman A, Desai MM, John J, Altice FL. An assessment of health-care students’ attitudes toward patients with or at high risk for HIV: implications for education and cultural competency. AIDS Care. 2014;26:1223–1228. doi: 10.1080/09540121.2014.894616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Latypov AB. The Soviet doctor and the treatment of drug addiction: a difficult and most ungracious task. Harm Reduct. J. 2011;8:32. doi: 10.1186/1477-7517-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Makarenko I, Mazhnaya A, Polonsky M, Marcus R, Bojko MJ, Filippovych S, Springer S, Dvoriak S, Altice FL. Determinants of willingness to enroll in opioid agonist treatment among opioid dependent people who inject drugs in Ukraine. Drug Alcohol Depend. 2016;165:213–220. doi: 10.1016/j.drugalcdep.2016.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morozova O, Dvoryak S, Altice FL. Methadone treatment improves tuberculosis treatment among hospitalized opioid dependent patients in Ukraine. Int. J. Drug Policy. 2013;24:e91–e98. doi: 10.1016/j.drugpo.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parmenter J, Mitchell C, Keen J, Oliver P, Rowse G, Neligan I, Keil C, Mathers N. Predicting biopsychosocial outcomes for heroin users in primary care treatment: a prospective longitudinal cohort study. Brit. J. Gen. Pract. 2013;63:e499–505. doi: 10.3399/bjgp13X669220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Polonsky M, Azbel L, Wickersham JA, Taxman FS, Grishaev E, Dvoryak S, Altice FL. Challenges to implementing opioid substitution therapy in Ukrainian prisons Personnel attitudes toward addiction, treatment, and people with HIV/AIDS. Drug Alcohol Depend. 2015;148:47–55. doi: 10.1016/j.drugalcdep.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Polonsky M, Rozanova J, Azbel L, Bachireddy C, Izenberg J, Kiriazova T, Dvoryak S, Altice FL. Attitudes toward addiction, methadone treatment, and recovery among hiv-infected Ukrainian prisoners who inject drugs: incarceration effects and exploration of mediators. AIDS Behav. 2016;20:2950–2960. doi: 10.1007/s10461-016-1375-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schaub M, Chtenguelov V, Subata E, Weiler G, Uchtenhagen A. Feasibility of buprenorphine and methadone maintenance programmes among users of home made opioids in Ukraine. Int. J. Drug Policy. 2010;21:229–233. doi: 10.1016/j.drugpo.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 25.Sylla L, Bruce RD, Kamarulzaman A, Altice FL. Integration and co-location of HIV/AIDS, tuberculosis and drug treatment services. Int. J. Drug Policy. 2007;18:306–312. doi: 10.1016/j.drugpo.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thompson MA, Mugavero MJ, Amico KR, Cargill VA, Chang LW, Gross R, Orrell C, Altice FL, Bangsberg DR, Bartlett JG, Beckwith CG, Dowshen N, Gordon CM, Horn T, Kumar P, Scott JD, Stirratt MJ, Remien RH, Simoni JM, Nachega JB. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an International Association of Physicians in AIDS Care panel. Ann. Intern. Med. 2012;156:817–833. doi: 10.7326/0003-4819-156-11-201206050-00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.UNAIDS. Global AIDS Update 2016. Joint United Nations Programme on HIV/AIDS 2016a [Google Scholar]
- 28.UNAIDS. Prevention Gap Report. Joint United Nations Programme on HIV/AIDS 2016b [Google Scholar]
- 29.WHO/UNODC/UNAIDS. Policy Guidelines For Collaborative TB And HIV Services For Injecting And Other Drug Users: An Integrated Approach. Geneva: 2008. [PubMed] [Google Scholar]
- 30.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med. Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Weisner C, Mertens J, Parthasarathy S, Moore C, Lu Y. Integrating primary medical care with addiction treatment. A randomized controlled trial. JAMA. 2001;286:1715–1723. doi: 10.1001/jama.286.14.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wolfe D, Carrieri MP, Shepard D. Treatment and care for injecting drug users with HIV infection: a review of barriers and ways forward. Lancet. 2010;376:355–366. doi: 10.1016/S0140-6736(10)60832-X. [DOI] [PubMed] [Google Scholar]